A systematic review on the association between ovarian and prostate cancer with BRCA1 and BRCA2 gene
Автор: Veena S.C., Mohammed V., Veerabathiran R.
Журнал: Сибирский онкологический журнал @siboncoj
Рубрика: Обзоры
Статья в выпуске: 6 т.21, 2022 года.
Бесплатный доступ
Background. BRCA1 and BRCA2 were discussed as the basis of inherited adenocarcinoma and breast and ovarian malignancy. Ovarian cancer is uncommon in women below 40 years of age, and prostate cancer mainly occurs in older men cause 90 % in those above sixty-five. Objective. The main objective of this paper is to investigate the relationship between ovarian and prostate cancer with the BRCA1 and BRCA2 genes. Material and Methods. The ovarian and prostate cancer mechanism is discussed in detail, and their preventive measures with screening techniques are also demonstrated. This systematic review collected the related articles from online databases using the key terms ovarian cancer, prostate cancer, BRCA genes, mutation, polymorphism, carcinoma, sarcoma, and genetic association. Results. Based on the obtained information, it is found that the BRCA genes are highly associated with prostate cancer in men, and in women, it is significantly linked with breast cancer than ovarian cancer. Conclusion. Therefore, early diagnosis and genetic testing for BRCA1&BRCA2 genes in both men and women are necessary. in some cases, these genes might even cause different types of cancer like pancreatic cancers. identifying individuals with tumour-HRD through mutations in the homologous repair pathway and determining this gene expression is essential to improve treatment techniques developed during the previous decade and rapidly make their way into clinical trials practice. However, the safe introduction of these medicines into everyday practice will require a thorough understanding of treatment targets and associated adverse effects.
Ovarian cancer, prostate cancer, mutated allele
Короткий адрес: https://sciup.org/140296687
IDR: 140296687 | УДК: 616.681+616.65]-006.6:575.113 | DOI: 10.21294/1814-4861-2022-21-6-145-155
Текст научной статьи A systematic review on the association between ovarian and prostate cancer with BRCA1 and BRCA2 gene
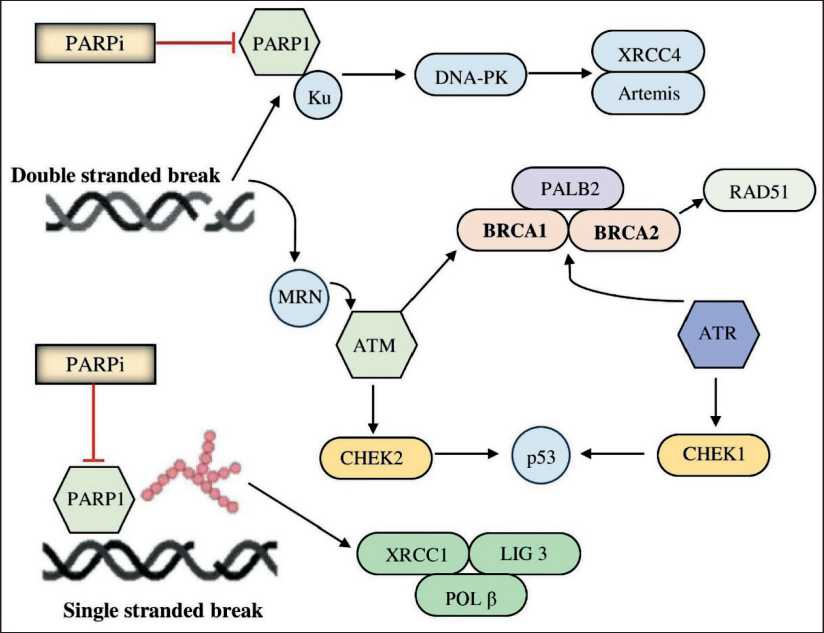
Fig. 1. Role of BRCA genes in the progression of cancer with PARP inhibitors, when a double stranded break occurs, it progresses to the MRN complex which further develops as ATM (ataxia telangiectasia mutated gene) which divides into two pathways, as BRCA genes or CHEK2 gene. When a single stranded break occurs, it progresses to XRCC1, LIG 3, and POLβ
Рис. 1. Роль генов BRCA в развитии рака при применении ингибиторов PARP, при возникновении двухцепочечного разрыва происходит активация комплекса MRN с последующим вовлечением ATM (мутированный ген атаксии телеангиэктазии), что сопровождается инициацией двух путей при участии генов BRCA и CHEK2 . В случае одноцепочечного разрыва происходит активация комплекса, состоящего из XRCC1, LIG 3 и POLβ
primarily expands mortality and morbidity. Surgery accompanied by platinum-basic chemotherapy is the normal customary treatment pathway for ovarian cancer. As of now, it results in no recognized inhibitory measures, and there has not yet been a productive screening tool for OC [5]. Most patients with progressive stages of the PC presently respond to the current treatment such as hormonal therapy, radiotherapy, or chemotherapy. However, only in the beginning cause as the PC progresses, it gets widespread and evolves to a stage where it becomes resistant to the present prostate cancer therapeutic methods. As for PC, there has still not yet been any conclusion of direct evidence that shows that early observation and remedy improve the lifespan or standard of living, the effect of PC screening remains disputable [6].
Risk Factors
It remains unrevealed how ovarian carcinoma develops, and the events are commencing it. Epidemio-logically, some evolving hazardous factors may lead to OC growth, some of which are discovered, including nulliparity, late menopause, early menarche, family ancestry, and elderliness in North America [7]. The lifetime count of menstruation cycles is also related to the chance of developing OC. The usage of fertility drugs also probability leading to ovarian cancer; however, the findings remain inconsistent. Overall, the occurrence of ovarian malignancy is excessive in perimenopause and post-menopause. Greater height and overweight were also related to the risks of OC [8]. The most significant subset risk for OC is females who bear pernicious BRCA1 or BRCA2 genes. Females who bear BRCA1 gene mutations have more risk for OC in their late thirties, and similar for females who bear BRCA2 gene mutations have more risk for OC in their late forties [9]. Approximately, about 85 % of PC cases are diagnosed only for men aged above 65 years. By the age of 65 years, the disease’s risk varies from 0.5 % to 20.0 % globally. Family inherent is now an established risk factor for PC; this was studied and confirmed by subsequent cohort and case-control studies [10]. Smoking cigarettes can also serve as a determinant condition for PC; numerous studies have found this. Vasectomy may expand the risk of attaining PC cause it has been observed that men who undergo vasectomy have more levels of circulating testosterone [11]. Differences in dietary habits can also be a risk for PC to occur, Nutrients which also comprises of carbohydrates, fats, proteins, polyphenols, and vitamins like A, B, and E, the conclusion of the mentioned nutrients may also be demonstrated by many mechanisms which also consists of swelling, the activity of sex hormones and antioxidant effects [12]. Spontaneously sequencing of all intron boundaries and codifying exons is included in BRCA1/2 gene genetic screening, and new techniques can detect broad deletions and insertions, which may even involve a single or more complete exons. A negative, positive or non-informative re- sult can be obtained from a genetic test. The NCCN Prostate Cancer Guidelines recommend that somatic and germline testing panels also give results to Lynch syndrome-linked genes like MLH2, MSH6, PMS2, and MSH1) and also homologous recombination genes (PALB2, BRCA1/2 CHEK2, ATM) [35]. This review investigates the relationship between ovarian and prostate cancer with the BRCA1 and BRCA2 genes. The ovarian and prostate cancer mechanism is discussed in detail, followed by their preventive measures with screening techniques are also demonstrated [13].
BRCA1 (Breast Cancer 1) gene
In the year 1994 BRCA1 gene was recognized and cloned based on the relation to premature onset breast carcinoma and breast-ovarian malignancy syndromes in females. About 40–45 % of inherent mutations of this gene account for hereditary cancer [14]. This tumor suppressor is also crucial for the growth of embryonic cells and expected growth. BRCA1 genes are also engaged in cell division regulation, deoxyribonucleic acid repair and damage, and differentiation of cells [15]. BRCA1 mutations are detected on the 17q12-21 of the chromosome and cipher a protein with 1863 amino acids in humans. BRCA1 mutations cause breast and ovarian carcinoma, and they also may or may not cause PC in men [16]. BRCA1 was the first breast malignancy suspected gene found; it covers around 100 kb on the long arm of chromosome 17 (17q21.3), from which a 7.8-kb mRNA is produced, which encodes an 1863-amino-acid protein, and comprises 24 exons, including a relatively significant exon 11. Another word used for the BRCA1 gene is known as the caretaker of the genome as it intricates in maintaining genome stability [17]. Control of proliferation is another significant role of the BRCA1 gene for ovarian and prostate cancer is explained in Table 1. The BRCA1 gene also inhibits estrogen receptor signaling; it is presumed that interference of estrogenic stimulant of epithelial mammary cell growth by BRCA1 may vanquish mammary tum-origenesis. However, the interaction of BRCA1 with the estrogen receptor task does not reasonably describe the relationship of BRCA1 mutations to OC. It is very noticeable that BRCA1 plays a chief role in cell-mediated response to deoxyribonucleic acid damage because BRCA1 does the transcription-coupled repair, microhomology adjoining, non-homologous end-joining and homologous recombination [18]. Women who carry a solitary mutated BRCA1 allele are exposed to ovarian and breast carcinoma, but it does not lead to cancer development; cancer development requires the destruction of allelomorphs that are wild in type that expresses itself as a carcinoma suppressor gene [19].
BRCA2 (Breast Cancer2) gene
Most commonly mutated sNps in the BRCA1 gene for ovarian and prostate cancer and explained in the location of chromosomes, alleles, function, and the clinical significance of the sNps
Наиболее часто мутирующие sNp в гене BRCA1 при раке яичников и предстательной железы с локализацией на хромосомах, обозначением аллелей, объяснением функции белков и клинической значимостью
Most commonly mutated sNps in the BRCA2 gene for ovarian and prostate cancer and explained in the location of chromosomes, alleles, function, and the clinical significance of the sNps
Наиболее часто мутирующие sNp в гене BRCA2 при раке яичников и предстательной железы с локализацией на хромосомах, обозначением аллелей, объяснением функции белков и клинической значимостью
All over the globe, more than two-thousand distinctive BRCA2 VUS have been recognized, including silent and missense substitutions, intronic variants, and small in-frame deletions and insertions [22]. BRCA2 gene is a more commonly found gene that is altered in a premature set course of PC in young men below the age of Sixty-Five. BRCA2 mutation has an excessive probability of maturing to a progressive stage of the disease, which sums up the affected to be short-lived [23]. Although BRCA2 mutations flop when it comes to repairing DNA duplex by homologous recombination, which then out turns in rising gene errors. BRCA2 plays a significant role in cell division during the S and G2 phases [24]. Double-strand break repair is the resulting purpose of the gene after the cell division. According to that, deficient cells, that is, cells that do not carry the BRCA2 gene, undergo chromosomal rearrangements such as deletions and translocations [25]. The only factor that is still left undiscovered by monitoring these BRCA2 -deficient cells is that they also have a greater prevalence in chromosome number alterations. Evidence states that the BRCA2 gene also involves itself in cytokinesis, and the chromosomal abnormalities glimpsed on the deficient cells are part of a direct reaction of BRCA2 dysfunction. BRCA2 is also profoundly called a “chromosome-instability gene” [26]. At least 2 different cancer phenotypes are exhibited by the BRCA2 germline mutation carriers, in which the first cancer phenotype are BRCA2 genes that have a perilous probability of breast or ovarian malignancy but when compared to the second cancer phenotype, which is presented by BRCA2 germline mutation carriers have no inherent chronicle of pancreatic or ovarian or breast cancer, these sorts of occurrence can also be called sporadic [27]. So, therefore, inherent mutations of the BRCA2 gene concludes to a multi carcinoma phenotype which compromises breast cancer (can occur in female and male), ovarian cancer, pancreatic carcinoma, prostate cancer, ocular cancer and other melanomas cancer, laryngeal cancer, colon malignancy, and stomach cancers. Germline mutations and Somatic mutations of the DNA Damage Response, in short, known as DDR, BRCA2 genes rise in mCRPC, which can be expanded as metastatic castration-resistant prostate cancer in contrast to primary localized prostate cancer, the aspect of BRCA2 alteration in primary confined prostate cancer is not distinguished well enough [28].
BRCA genes influence Ovarian and Prostate Cancer
Family chronology is the significant risk factor for OC [29]. WHO has reclassified OC, previously known as surface epithelial-stromal cancers, into five histotypes: low-grade serous carcinoma, high-grade serous carcinoma, clear cell carcinoma, endometrioid carcinoma, and mucinous carcinoma [30]. Spontaneous mutations cause the majority of ovarian tumors. A hereditary tendency is responsible for about 10 % of instances. The most significant category of females at danger for ovarian carcinoma is those with detrimental alterations in the BRCA1 or BRCA2 genes. Several genes have been discovered to be when altered, raise a woman’s risk of OC significantly. DNA mismatch repair genes, BRCA1&2 are among them. Familial mutations in DNA repair genes and HOXB 13 such as CHEK2 , RAD51D, BRCA2 , PALB2, BRCA1, and ATM have been discovered by genomic investigations for PC. BRCA1 -associated OC (Fig. 2) has been found that they have more rate of serous adenocarcinoma, and OC in BRCA1 -certain families mostly to be expected
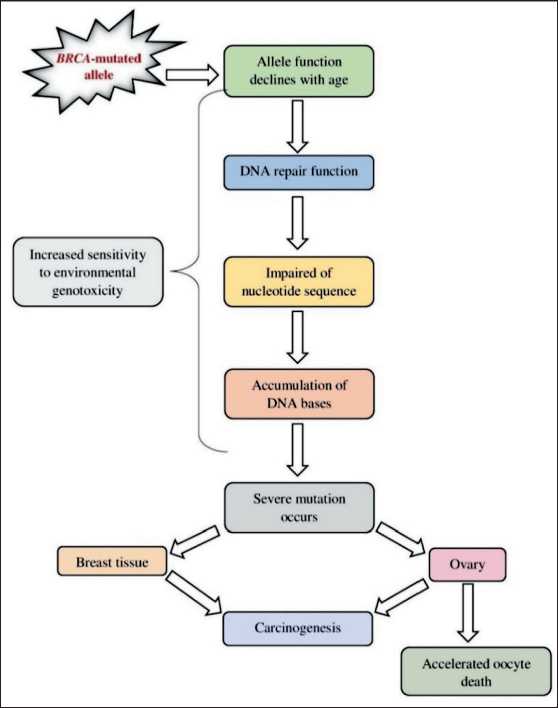
Fig. 2. Formation of ovarian cancer due to BRCA genes mutated allele, as allele function declines with age it leads to impaired nucleotide sequence and further accumulation of DNA bases under high sensitivity to environmental genotoxicity which leads to severe mutation, thus when occurred with ovary, leads to ovarian carcinoma
Рис. 2. Развитие рака яичников при наличии мутантного аллеля BRCA; поскольку репарационные возможности ДНК снижаются с возрастом, то происходит нарушение последовательности нуклеотидов, накопление оснований с высокой чувствительностью к генотоксическим факторам окружающей среды и развитие мутаций; в случае развития мутаций в клетках яичников развивается карцинома яичников of high-grade and non-mucinous than malignancies in BRCA1-uncertain families [31]. Mutations or alterations in BRCA1 are commonly seen in three domains: BRCA1 C-terminus encoded by exons 16–24 and the amino acids 1650–1863 or BRCT domain, the N-ter-minal RING domain constitutes of exons 2–7 (amino acids 1–109), the coding sections of exons 11–13, in carcinoma patients [32]. At 40 years of age, the risk of OC among BRCA1-mutation carriers was minimal.
BRCA2 mutations that occur in families with one or more incidences of OC tend to cluster in the “ovarian cancer cluster region”, a core section of the gene [33] limited by nucleotides 3059–4075 and 6503–6629. Ovarian Cancer Cluster Region mutations, in short, known as OCCR mutations, were allied to a less perilous probability of breast carcinoma as well as a significantly more perilous probability of ovarian carcinoma. Women with BRCA1 (17q21 chromosomal) alterations have a higher risk of OC with a lifespan risk of 24 % to 40 %. Women with BRCA2 (13q12 chromosomal) gene alterations have a comparatively more perilous probability of OC of 18–24 %. Other neoplasms, such as breast and colon cancer, can increase the chance of getting OC in families with a history of OC. Small deletions, insertions, or punctiform alterations in BRCA2 and BRCA1 genes result in the generation of stop codons, resulting in nonfunctional truncated proteins [34]. BRCA1 and BRCA 2 protein misregulation and altered expression aggravate sporadic types of breast carcinoma. The deficits in the gene’s function result in the deposition of genetic abnormalities, driving cancer formation. PC is the primary average noncutaneous cancer in males all over the globe, with a likely predicted 366,000 deaths and 1.600,000 cases each year [35]. Men with advanced PC and Intraductal histology in men and Men of Ashkenazi Jewish descent and men who meet the criteria for family history [36]. PC is explained by the abnormal division of cells found in the prostate gland, which concludes in atypical prostate gland growth. Malignant cells travel to furthermore regions of the body, such as the spinal cord, pelvic and retroperitoneal lymph nodes, brain, rectum, bladder, and bone resulting in demise from prostate carcinoma [37]. BRCA2 and BRCA1 increase the probability of malignancies of females’ fallopian tubes, ovary, peritoneum, and breast. Men who carry BRCA2 or BRCA1 alterations are likewise at peril probability for malignancy. BRCA2 and BRCA1 have both been suspected in PC in various investigations. In these carriers of BRCA1 mutations for men, the prostate is the highest reported region of malignancy peril. The link between BRCA2 and PC risk is more consistent.
Men younger than 65 years were more vulnerable to PC [38]. BRCA2 alteration carriers have a fivefold increased probability of PC [39]. In research, two BRCA2 alterations were recognized among patients affected and diagnosed with PC before the age of 60 years, and in a study of 38, it was pinpointed with familial clus- tering of PC (Fig. 3). No BRCA1 mutation was found, so these BRCA2 alterations were seen with patients diagnosed with PC before sixty years [40]. The Ovarian Cluster Central Region has recently been linked to a less perilous probability of PC of 19.2 % before age 80 years, compared to 33.6 % for mutations outside the Ovarian Cluster Central Region. Alterations found in the Edwards et al. study of 234 early-onset prostate cancer patients in the United Kingdom were outside of the OCCR. Recent findings show that common PC susceptibility genetic variants influence PC probability in BRCA2 and BRCA1 carriers [41].
Fallopian tube carcinoma, melanoma, endometrial, pancreatic, prostate, and colorectal carcinoma have all been linked to BRCA pathogenic mutations [42]. More than 2900 BRCA1 variants and 3400 BRCA2 variants are registered as pathogenic germline mutations. The retention rate of both the genes was 8.3–14.7 %, in which BRCA1 accounted for 3.4–9.9 % and BRCA2 accounted for 4.7–5.3 % for ovarian cancer [43]. The race that people belong to and their family history along with inherited syndromes can increase the risk of developing prostate carcinoma [44]. Ovarian carcinoma with the BRCA1 pathogenic variation has more aggressive clinical and pathological characteristics
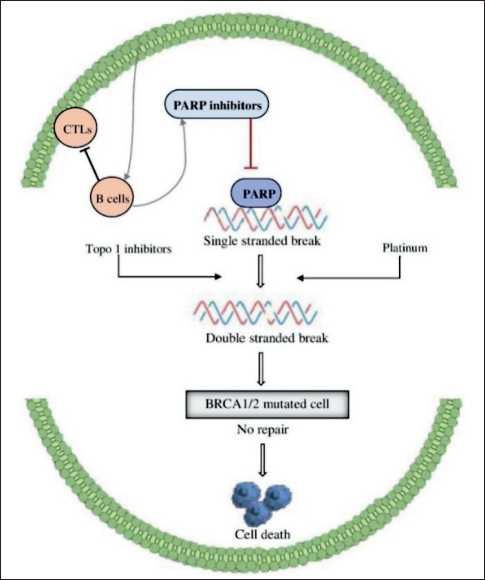
Fig. 3. BRCA mutated cells in prostate cancer with PARP inhibitors cause a single-stranded break initially followed by a double strand, which leads to BRCA1 and 2 mutated cells and ends with cell death
Рис. 3. Применение ингибиторов PARP в клетках опухоли предстательной железы с наличием мутации BRCA связано с развитием одноцепочечных разрывов ДНК, затем – двухцепочечных разрывов, с формированием мутаций в генах BRCA1 и 2, что заканчивается гибелью клеток предстательной железы than ovarian carcinoma with the BRCA2 pathogenic variant. BRCA genes are two cancer-suppressing genes that are required for DNA repair activation in response to cellular stress. Moreover in chromatin remodelling, transcription management, cell-cycle regulation, and DNA-repair mechanisms, both the BRCA genes play critical roles [45]. A recent study by Sun, et.al also states that HIV also commonly known as AIDS can develop prostate cancer [46]. In women, when affected with atypical ovarian endometriosis, even though our knowledge of considering it as an risk factor is still in study, there has been many incidence of ovarian carcinoma in people affected by endometriosis [47].
Molecular diagnosis
There has been much development in OC screening and prevention. Since the mid-1980s, researchers have established an OC screening technique to minimize disease mortality [48]. CA125 (Cancer Antigen 125) is a screening method for OC, and it was discovered in 1981, and extensive research has been done on its link to OC. To overcome the disadvantages of CA125, it is paired with transvaginal sonography. Ultrasound screening is another screening technique [49]. Erroneous positive screening results resulted in a 15 % significant complication risk (infection, direct surgical, cardiorespiratory, and other) in women undergoing surgery. Yearly ovarian cancer screening does not lower death, but it does ‘raise intrusive medical procedures and related complications,’ according to the authors [50]. To increase the sensitivity and specificity of the CA125 level, a multimodal screening algorithm was created. The ROCA algorithm is the algorithm’s name (Risk of Ovarian Carcinoma Algorithm). In the UK Collaborative Trial of Ovarian Cancer Screening, this strategy was combined with ultrasound and a systematic evaluation and follow-up [51]. PC testing is divisive. PSA-based screening has resulted in a substantial shift in disease stages ranges from mostly cannot be treated to primarily treatable.
Moreover, considering the US prostate carcinoma mortality rate, there is a peak down the reduction of 53 %. However, worries have arisen regarding too much diagnosis and therapy of screen-detected indolent tumors [52]. Serum PSA was approved for the first time in 1986 to assess PC treatment response and monitor for recurrence. However, PSA tests are inherently flawed. PSA is not produced or secreted by all PC, and an abnormal PSA level does not always indicate the presence of cancer. The ERSPC and PLCO trials produced contradictory results, with the ERSPC demonstrating a reduction in PC mortality while the PLCO demonstrated no difference in mortality between the screening and control arms [53].
Many biomarkers are used to diagnose ovarian cancer recently such as HE4, which stands for Human Epididymis Protein 4. Some of the sensitive markers include Risk of Malignancy Index (RMI) and also Risk of Ovarian Malignancy Algorithm (ROMA), these were discovered to elevate the efficiency of biomarkers [54]. CA125, a serum biomarker routinely used by physicians to estimate preoperative cancer risk, performs poorly in premenopausal women, initial cancers, and certain histological subgroups. OVA1 is a multivariate index assessment that measures the malignancy probability of an adnexal mass by combining CA125 and four other serum proteins. CA125 missed 63 % of early-stage tumours that OVA1 properly detected [55]. Amongst all the biomarkers mentioned above, HE4 is observed to be the most dependable marker for ovarian carcinoma detection, whereas ROMA is said to have greater sensitivity than other markers [56].
Molecular profiling can be shortly described as the checkup of protein, RNA and DNA from the affected person’s carcinoma through the tumor cells collected from biopsy. Molecular profiling initially started with just DNA profiling, as years went by, they have developed various other molecular profiles now for BRCA genes, PCR expanded as Polymerase Chain reaction, In situ hybridization (ISH), FISH test and is more specific to Sanger sequencing, Pyrosequencing, NGS and Fragment analysis, there are associated with RNA and DNA. For protein, Immunohistochemistry (IHC) is used [57].Individual BRCA1 and BRCA2 gene testing has mostly been substituted by multigene panel testing. DNA is extracted from formalin-fixed paraffin embedded (FFPE) tumour tissue biopsies from either old or current tumour samples for targeted cancer genomic profiling. After platinum exposure, 10–28 % of cancers when tested with homologous recombination deficiency may have a BRCA reversion mutation, restoring hormone receptor competence [58].
Cancer prevention
First, there are non-surgical alternatives to OC prevention, such as oral contraceptives, parity, multiparity, and breastfeeding. Second, reducing inflammation by medication, dietary changes, and increased physical activity. Previous research has found that parous women with BRCA1 mutations have a significantly lower incidence of OC [59]. Westernized diets have lower fiber intake and fewer fruits and vegetables compared to diets in underdeveloped nations. Compared to the general population, people who tend to have more veggies and fruits have a comparatively lesser probability of maturing carcinoma [60]. The United States Preventive Services Task Force modernized this guidance in 2005, affirming that the advantages of BRCA1 and BRCA2 testing overshadowed the risks, and “strongly recommended” that genetics services be provided to at-risk individuals. Prophylactic bilateral salpingo-oophorec-tomy lowers OC incidence in women at high risk of developing ovarian epithelial carcinoma, particularly those with BRCA2 and BRCA1 mutations [61].
Novel therapeutics
In BRCA mutation-positive patients, there are three options for lowering the risk of breast and ovarian carcinoma: monitoring, chemoprevention, and risk-reducing surgical surgery [62]. OCPs that exclusively contain progesterone has been linked to a lower incidence of OC, confirming the theory that constant menstruation contributes to ovarian carcinogenesis [63]. One of the leading reasons for mortality and morbidity in this modernized planet, PC should be a curable disease. Identifying distinct contagious pathogens like etiologic agents for PC advancement would open the door to prevention strategies based on antibiotics or vaccines. Epigenetic genome mutations, which alter gene purpose but not gene sequence, have long piqued the interest of carcinoma biologists as a potential selection for malignancy avoidance and treatment. However, significant phase 3 trials of PC prevention agents, such as vitamin E, finasteride, selenium, dutasteride, have shown and proved to be time-consuming (so many years), costly, and logistically perplexing. Till yet, there has been no clear clinical generative pathway or prostate cancer prevention drugs, from first-in-man trials to FDA registration trials [64]. Dietary guidelines for PC prevention are similar to cardiovascular and general entire health. They generally entail more vegetable and fruit consumption while lessening red meat and saturated fat consumption. Preclinical studies suggest that exercise influences tumor development by altering oxidative
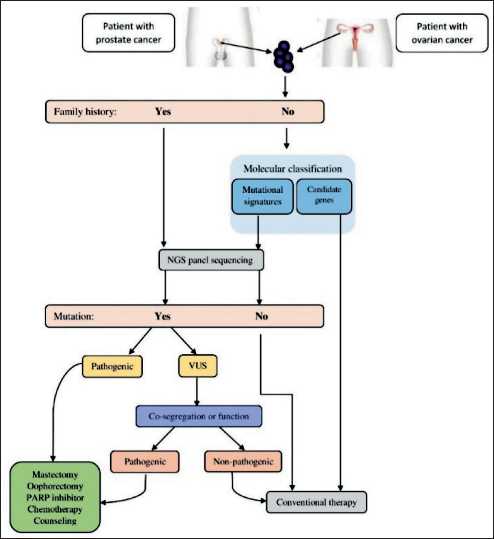
Fig. 4. Novel therapeutic strategies for ovarian and prostate cancer are available even with or without a family history, NGS panel sequencing must be done, to find out whether mutation occurs and then for further therapy
Рис. 4. Новые стратегии в лечении рака яичников и предстательной железы, в том числе и для больных без связи с семейным анамнезом; проведение секвенирования нового поколения ДНК опухолевых клеток (NGS) необходимо для детекции значимых мутации, а также для определения дальнейшей тактики лечения stress, whereas epidemiological and clinical data show that higher levels of exercise improve PC outcomes (Fig. 4) [65].
The somatic mutations accumulate in epithelial cell populations during a patient’s lifetime is thought to be substantially linked to prostate cancer. Oncogenes and tumour suppressor genes are both susceptible to these mutations. Alteration in gene transcription and/or translation, as well as functional abnormalities, result in a disruption of cell homeostasis. Genes that control cell growth, cell proliferation, and cell death are often mutated [66]. During recent years it is found that men with BRCA2 germline mutations are more likely to have much high genomic instability in lumps. These lumps generally represent a distinctive molecular profile and involvement of intraductal carcinoma of the prostate (IDCP) pathology. These IDCP originate from the similar ancestral clone, later these lump cells can withstand sensitive prostate carcinoma (castration de novo), this makes the lump escape androgen deprivation therapy [67]. For the treatment of mild prostate carcinoma, high-intensity focused ultrasound is a less intrusive approach. Focal therapy is a treatment solution for low prostate cancer that has a 75 % cancer-free survival rate, a 99 % cancer-specific survival rate, and a 96 % metastasis-free survival rate in clinical trials [68].
PARP inhibitors help in the detection of locus determined loss of heterozygosity (LOH), it is now said to be the latest stratification factor in determining the drug effects. It looks into the deterioration of the BRCA genes purpose in the lump.PARP is necessary for nucleotide excision repair, which is used to restore DNA single-strand breaks. PARP inhibition causes a buildup of single-strand breaks in DNA and, subsequently, replication fork damage. Five PARP inhibitors are now available: olaparib, talazoparib, rucaparib, niraparib, and veliparib. The US Food and Drug Administration (FDA) has authorised olaparib, rucaparib, and niraparib for the treatment of ovarian carcinoma [69]. Docetaxal, taxanes and cabazitaxel are the conventional chemotherapy drugs which are actively used in the curing of carcinoma. With taxanes, BRCA1 pathogenic variants were sort of resistant with microtubule-inhibition chemotherapies [70].
Conclusion
Список литературы A systematic review on the association between ovarian and prostate cancer with BRCA1 and BRCA2 gene
- Zaimy M.A., Saffarzadeh N., Mohammadi A., Pourghadamyari H., Izadi P., Sarli A., Moghaddam L.K., Paschepari S.R., Azizi H., Torkamandi S., Tavakkoly-Bazzaz J. New methods in the diagnosis of cancer and gene therapy of cancer based on nanoparticles. Cancer Gene Ther. 2017; 24(6): 233-43. https://doi.org/10.1038/cgt.2017.16.
- Webb P.M., Jordan S.J. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017; 41: 3-14. https://doi.org/10.1016/j.bpobgyn.2016.08.006.
- Tenke P., Horti J., Balint P., Kovacs B. Prostate cancer screening. Recent Results Cancer Res. 2007; 175: 65-81. https://doi.org/10.1007/978-3-540-40901-4_5.
- Chobanian N., Dietrich C.S. Ovarian cancer. Surg Clin North Am. 2008; 88(2): 285-99, vi. https://doi.org/10.1016/j.suc.2007.12.002.
- Rooth C. Ovarian cancer: risk factors, treatment and management. Br J Nurs. 2013; 22(17): 23-30. https://doi.org/10.12968/bjon.2013.22.Sup17.S23.
- Jaworska D., Król W., Szliszka E. Prostate Cancer Stem Cells: Research Advances. Int J Mol Sci. 2015; 16(11): 27433-49. https://doi.org/10.3390/ijms161126036.
- Daly M., Obrams G.I. Epidemiology and risk assessment for ovarian cancer. Semin Oncol. 1998; 25(3): 255-64.
- La Vecchia C. Ovarian cancer: epidemiology and risk factors. Eur J Cancer Prev. 2017; 26(1): 55-62. https://doi.org/10.1097/CEJ.0000000000000217.
- Schmeler K.M., Sun C.C., Bodurka D.C., White K.G., Soliman P.T., Uyei A.R., Erlichman J.L., Arun B.K., Daniels M.S., Rimes S.A., Peterson S.K., Slomovitz B.M., Milam M.R., Gershenson D.M., Lu K.H. Prophylactic bilateral salpingo-oophorectomy compared with surveillance in women with BRCA mutations. Obstet Gynecol. 2006; 108: 515-20. https://doi.org/10.1097/01.AOG.0000228959.30577.13.
- Patel A.R., Klein E.A. Risk factors for prostate cancer. Nat Clin Pract Urol. 2009; 6(2): 87-95. https://doi.org/10.1038/ncpuro1290.
- Pienta K.J., Esper P.S. Risk factors for prostate cancer. Ann Intern Med. 1993; 118(10): 793-803. https://doi.org/10.7326/0003-4819-118-10-199305150-00007.
- Matsushita M., Fujita K., Nonomura N. Infuence of Diet and Nutrition on Prostate Cancer. Int J Mol Sci. 2020; 21(4): 1447. https://doi.org/10.3390/ijms21041447.
- Rosen E.M., Fan S., Pestell R.G., Goldberg I.D. BRCA1 gene in breast cancer. J Cell Physiol. 2003; 196(1): 19-41. https://doi.org/10.1002/jcp.10257.
- Paterson J.W. BRCA1: a review of structure and putative functions. Dis Markers. 1998; 13(4): 261-74. https://doi.org/10.1155/1998/298530.
- Kubista M., Rosner M., Miloloza A., Hofer K., Prusa A.R., Kroiss R., Marton E., Hengstschläger M. BRCA1 and diferentiation. Mutat Res. 2002; 512(2-3): 165-72. https://doi.org/10.1016/s1383-5742(02)00063-7.
- Jhanwar-Uniyal M. BRCA1 in cancer, cell cycle and genomic stability. Front Biosci. 2003; 8: 1107-17. https://doi.org/10.2741/1131.
- Billack B., Monteiro A.N. BRCA1 in breast and ovarian cancer predisposition. Cancer Lett. 2005; 227(1): 1-7. https://doi.org/10.1016/j.canlet.2004.11.006.
- Chakraborty G., Armenia J., Mazzu Y.Z., Nandakumar S., Stopsack K.H., Atiq M.O., Komura K., Jehane L., Hirani R., Chadalavada K., Yoshikawa Y., Khan N.A., Chen Y., Abida W., Mucci L.A., Lee G.M., Nanjangud G.J., Kantoff P.W. Signifcance of BRCA2 and RB1 Co-loss in Aggressive Prostate Cancer Progression. Clin Cancer Res. 2020; 26(8): 2047-64. https://doi.org/10.1158/1078-0432.CCR-19-1570.
- Rudkin T.M., Foulkes W.D. BRCA2: breaks, mistakes and failed separations. Trends Mol Med. 2005; 11(4): 145-8. https://doi.org/10.1016/j.molmed.2005.02.003.
- Tavtigian S.V., Simard J., Rommens J., Couch F., Shattuck-Eidens D., Neuhausen S., Merajver S., Thorlacius S., Offt K., Stoppa-Lyonnet D., Belanger C., Bell R., Berry S., Bogden R., Chen Q., Davis T., Dumont M., Frye C., Hattier T., Jammulapati S., Janecki T., Jiang P., Kehrer R., Leblanc J.F., Mitchell J.T., McArthur-Morrison J., Nguyen K., Peng Y., Samson C., Schroeder M., Snyder S.C., Steele L., Stringfellow M., Stroup C., Swedlund B., Swense J., Teng D., Thomas A., Tran T., Tranchant M., Weaver-Feldhaus J., Wong A.K., Shizuya H., Eyfjord J.E., CannonAlbright L., Tranchant M., Labrie F., Skolnick M.H., Weber B., Kamb A., Goldgar D.E. The complete BRCA2 gene and mutations in chromosome 13q-linked kindreds. Nat Genet. 1996; 12(3): 333-7. https://doi.org/10.1038/ng0396-333.
- Mesman R.L.S., Calléja F.M.G.R., Hendriks G., Morolli B., Misovic B., Devilee P., van Asperen C.J., Vrieling H., Vreeswijk M.P.G. The functional impact of variants of uncertain signifcance in BRCA2. Genet Med. 2019; 21(2): 293-302. https://doi.org/10.1038/s41436-018-0052-2.
- Junejo N.N., AlKhateeb S.S. BRCA2 gene mutation and prostate cancer risk. Comprehensive review and update. Saudi Med J. 2020; 41(1): 9-17. https://doi.org/10.15537/smj.2020.1.24759.
- Kuang S., Li H., Feng J., Xu S., Le Y. Correlation of BRCA2 gene mutation and prognosis as well as variant genes in invasive urothelial carcinoma of the bladder. Cancer Biomark. 2019; 25(2): 203-12. https://doi.org/10.3233/CBM-182379.
- Kojic M., Yang H., Kostrub C.F., Pavletich N.P., Holloman W.K. The BRCA2-interacting protein DSS1 is vital for DNA repair, recombination, and genome stability in Ustilago maydis. Mol Cell. 2003; 12(4): 1043-9. https://doi.org/10.1016/s1097-2765(03)00367-8.
- Daniels M.J., Wang Y., Lee M., Venkitaraman A.R. Abnormal cytokinesis in cells defcient in the breast cancer susceptibility protein BRCA2. Science. 2004; 306(5697): 876-9. https://doi.org/10.1126/science.1102574.
- Hahn S.A., Greenhalf B., Ellis I., Sina-Frey M., Rieder H., Korte B., Gerdes B., Kress R., Ziegler A., Raeburn J.A., Campra D., Grützmann R., Rehder H., Rothmund M., Schmiegel W., Neoptolemos J.P., Bartsch D.K. BRCA2 germline mutations in familial pancreatic carcinoma. J Natl Cancer Inst. 2003; 95(3): 214-21. https://doi.org/10.1093/jnci/95.3.214.
- Lubinski J., Phelan C.M., Ghadirian P., Lynch H.T., Garber J., Weber B., Tung N., Horsman D., Isaacs C., Monteiro A.N., Sun P., Narod S.A. Cancer variation associated with the position of the mutation in the BRCA2 gene. Fam Cancer. 2004; 3(1): 1-10. https://doi.org/10.1023/B:FAME.0000026816.32400.45.
- Prat J., Ribé A., Gallardo A. Hereditary ovarian cancer. Hum Pathol. 2005; 36(8): 861-70. https://doi.org/10.1016/j.humpath.2005.06.006.
- Nakonechny Q.B., Gilks C.B. Ovarian Cancer in Hereditary Cancer Susceptibility Syndromes. Surg Pathol Clin. 2016; 9(2): 189-99. https://doi.org/10.1016/j.path.2016.01.003.
- Pharoah P.D., Ponder B.A. The genetics of ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2002; 16(4): 449-68. https://doi.org/10.1053/beog.2002.0296.
- Paul A., Paul S. The breast cancer susceptibility genes (BRCA) in breast and ovarian cancers. Front Biosci (Landmark Ed). 2014; 19(4): 605-18. https://doi.org/10.2741/4230.
- Antoniou A., Pharoah P.D., Narod S., Risch H.A., Eyfjord J.E., Hopper J.L., Loman N., Olsson H., Johannsson O., Borg A., Pasini B., Radice P., Manoukian S., Eccles D.M., Tang N., Olah E., Anton-Culver H., Warner E., Lubinski J., Gronwald J., Gorski B., Tulinius H., Thorlacius S., Eerola H., Nevanlinna H., Syrjäkoski K., Kallioniemi O.P., Thompson D., Evans C., Peto J., Lalloo F., Evans D.G., Easton D.F. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003; 72(5): 1117-30. https://doi.org/10.1086/375033. Erratum in: Am J Hum Genet. 2003; 73(3): 709.
- Russo A., Calò V., Bruno L., Rizzo S., Bazan V., Di Fede G. Hereditary ovarian cancer. Crit Rev Oncol Hematol. 2009; 69(1): 28-44. https://doi.org/10.1016/j.critrevonc.2008.06.003.
- Wang G., Zhao D., Spring D.J., DePinho R.A. Genetics and biology of prostate cancer. Genes Dev. 2018; 32(17-18): 1105-40. https://doi.org/10.1101/gad.315739.118.
- Sokolova A.O., Cheng H.H. Genetic Testing in Prostate Cancer. Curr Oncol Rep. 2020; 22(1): 5. https://doi.org/10.1007/s11912-020-0863-6.
- Schatten H. Brief Overview of Prostate Cancer Statistics, Grading, Diagnosis and Treatment Strategies. Adv Exp Med Biol. 2018; 1095: 1-14. https://doi.org/10.1007/978-3-319-95693-0_1.
- Liede A., Karlan B.Y., Narod S.A. Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol. 2004; 22(4): 735-42. https://doi.org/10.1200/JCO.2004.05.055.
- Ibrahim M., Yadav S., Ogunleye F., Zakalik D. Male BRCA mutation carriers: clinical characteristics and cancer spectrum. BMC Cancer. 2018; 18(1): 179. https://doi.org/10.1186/s12885-018-4098-y.
- Gayther S.A., de Foy K.A., Harrington P., Pharoah P., Dunsmuir W.D., Edwards S.M., Gillett C., Ardern-Jones A., Dearnaley D.P., Easton D.F., Ford D., Shearer R.J., Kirby R.S., Dowe A.L., Kelly J., Stratton M.R., Ponder B.A., Barnes D., Eeles R.A. The frequency of germ-line mutations in the breast cancer predisposition genes BRCA1 and BRCA2 in familial prostate cancer. The Cancer Research Campaign/ British Prostate Group United Kingdom Familial Prostate Cancer Study Collaborators. Cancer Res. 2000; 60(16): 4513-8. Erratum in: Cancer Res 2000; 60(24): 7185.
- Nyberg T., Frost D., Barrowdale D., Evans D.G., Bancroft E., Adlard J., Ahmed M., Barwell J., Brady A.F., Brewer C., Cook J., Davidson R., Donaldson A., Eason J., Gregory H., Henderson A., Izatt L., Kennedy M.J., Miller C., Morrison P.J., Murray A., Ong K.R., Porteous M., Pottinger C., Rogers M.T., Side L., Snape K., Walker L., Tischkowitz M., Eeles R., Easton D.F., Antoniou A.C. Prostate Cancer Risks for Male BRCA1 and BRCA2 Mutation Carriers: A Prospective Cohort Study. Eur Urol. 2020; 77(1): 24-35. https://doi.org/10.1016/j.eururo.2019.08.025.
- Eccles D.M. Hereditary cancer: guidelines in clinical practice. Breast and ovarian cancer genetics. Ann Oncol. 2004; 15(4): 133-8. https://doi.org/10.1093/annonc/mdh917.
- Lee A., Moon B.I., Kim T.H. BRCA1/BRCA2 Pathogenic Variant Breast Cancer: Treatment and Prevention Strategies. Ann Lab Med. 2020; 40(2): 114-21. https://doi.org/10.3343/alm.2020.40.2.114.
- Yoshida R. Hereditary breast and ovarian cancer (HBOC): review of its molecular characteristics, screening, treatment, and prognosis. Breast Cancer. 2021; 28(6): 1167-80. https://doi.org/10.1007/s12282-020-01148-2.
- Gandaglia G., Leni R., Bray F., Fleshner N., Freedland S.J., Kibel A., Stattin P., Van Poppel H., La Vecchia C. Epidemiology and Prevention of Prostate Cancer. Eur Urol Oncol. 2021; 4(6): 877-92. https://doi.org/10.1016/j.euo.2021.09.006.
- Orban T.I., Olah E. Emerging roles of BRCA1 alternative splicing. Mol Pathol. 2003; 56(4): 191-7. https://doi.org/10.1136/mp.56.4.191.
- Sun D., Cao M., Li H., Ren J., Shi J., Li N., Chen W. Risk of prostate cancer in men with HIV/AIDS: a systematic review and metaanalysis. Prostate Cancer Prostatic Dis. 2021; 24(1): 24-34. https://doi.org/10.1038/s41391-020-00268-2.
- Králíčková M., Laganà A.S., Ghezzi F., Vetvicka V. Endometriosis and risk of ovarian cancer: what do we know? Arch Gynecol Obstet. 2020; 301(1): 1-10. https://doi.org/10.1007/s00404-019-05358-8.
- Menon U., Karpinskyj C., Gentry-Maharaj A. Ovarian Cancer Prevention and Screening. Obstet Gynecol. 2018; 131(5): 909-27. https://doi.org/10.1097/AOG.0000000000002580.
- Gupta K.K., Gupta V.K., Naumann R.W. Ovarian cancer: screening and future directions. Int J Gynecol Cancer. 2019; 29(1): 195-200. https://doi.org/10.1136/ijgc-2018-000016.
- Buys S.S., Partridge E., Black A., Johnson C.C., Lamerato L., Isaacs C., Reding D.J., Greenlee R.T., Yokochi L.A., Kessel B., Crawford E.D., Church T.R., Andriole G.L., Weissfeld J.L., Fouad M.N., Chia D., O’Brien B., Ragard L.R., Clapp J.D., Rathmell J.M., Riley T.L., Hartge P., Pinsky P.F., Zhu C.S., Izmirlian G., Kramer B.S., Miller A.B., Xu J.L., Prorok P.C., Gohagan J.K., Berg C.D.; PLCO Project Team. Efect of screening on ovarian cancer mortality: the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial. JAMA. 2011; 305(22): 2295-303. https://doi.org/10.1001/jama.2011.766.
- Jacobs I.J., Menon U., Ryan A., Gentry-Maharaj A., Burnell M., Kalsi J.K., Amso N.N., Apostolidou S., Benjamin E., Cruickshank D., Crump D.N., Davies S.K., Dawnay A., Dobbs S., Fletcher G., Ford J., Godfrey K., Gunu R., Habib M., Hallett R., Herod J., Jenkins H., Karpinskyj C., Leeson S., Lewis S.J., Liston W.R., Lopes A., Mould T., Murdoch J., Oram D., Rabideau D.J., Reynolds K., Scott I., Seif M.W., Sharma A., Singh N., Taylor J., Warburton F., Widschwendter M., Williamson K., Woolas R., Fallowfeld L., McGuire A.J., Campbell S., Parmar M., Skates S.J. Ovarian cancer screening and mortality in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial. Lancet. 2016; 387(10022): 945-56. https://doi.org/10.1016/S0140-6736(15)01224-6. Erratum in: Lancet. 2016; 387(10022): 944.
- Catalona W.J. Prostate Cancer Screening. Med Clin North Am. 2018; 102(2): 199-214. https://doi.org/10.1016/j.mcna.2017.11.001.
- Dunn M.W. Prostate Cancer Screening. Semin Oncol Nurs. 2017; 33(2): 156-64. https://doi.org/10.1016/j.soncn.2017.02.003.
- Dochez V., Caillon H., Vaucel E., Dimet J., Winer N., Ducarme G. Biomarkers and algorithms for diagnosis of ovarian cancer: CA125, HE4, RMI and ROMA, a review. J Ovarian Res. 2019; 12(1): 28. https://doi.org/10.1186/s13048-019-0503-7.
- Lahlou N., Brun J.L. [Ovarian tumor markers of presumed benign ovarian tumors]. J Gynecol Obstet Biol Reprod (Paris). 2013; 42(8): 752-9. https://doi.org/10.1016/j.jgyn.2013.09.030.
- Dunton C.J., Hutchcraft M.L., Bullock R.G., Northrop L.E., Ueland F.R. Salvaging Detection of Early-Stage Ovarian Malignancies When CA125 Is Not Informative. Diagnostics (Basel). 2021; 11(8): 1440. https://doi.org/10.3390/diagnostics11081440.
- El-Deiry W.S., Goldberg R.M., Lenz H.J., Shields A.F., Gibney G.T., Tan A.R., Brown J., Eisenberg B., Heath E.I., Phuphanich S., Kim E., Brenner A.J., Marshall J.L. The current state of molecular testing in the treatment of patients with solid tumors, 2019. CA Cancer J Clin. 2019; 69(4): 305-43. https://doi.org/10.3322/caac.21560.
- Haunschild C.E., Tewari K.S. The current landscape of molecular profling in the treatment of epithelial ovarian cancer. Gynecol Oncol. 2021; 160(1): 333-45. https://doi.org/10.1016/j.ygyno.2020.09.043.
- Ali A.T. Towards Prevention of Ovarian Cancer. Curr Cancer Drug Targets. 2018; 18(6): 522-37. https://doi.org/10.2174/1568009618666180102103008.
- Boyle P., Maisonneuve P., Autier P. Update on cancer control in women. Int J Gynaecol Obstet. 2000; 70(2): 263-303. https://doi.org/10.1016/s0020-7292(00)00298-8.
- Temkin S.M., Bergstrom J., Samimi G., Minasian L. Ovarian Cancer Prevention in High-risk Women. Clin Obstet Gynecol. 2017; 60(4): 738-57. https://doi.org/10.1097/GRF.0000000000000318.
- Yamauchi H., Takei J. Management of hereditary breast and ovarian cancer. Int J Clin Oncol. 2018; 23(1): 45-51. https://doi.org/10.1007/s10147-017-1208-9.
- Schüler S., Ponnath M., Engel J., Ortmann O. Ovarian epithelial tumors and reproductive factors: a systematic review. Arch Gynecol Obstet. 2013; 287(6): 1187-204. https://doi.org/10.1007/s00404-013-2784-1.
- Nelson W.G., de Marzo A.M., Lippman S.M. Prostate cancer prevention. Can Chemopre. 2005; 185-203.
- Ballon-Landa E., Parsons J.K. Nutrition, physical activity, and lifestyle factors in prostate cancer prevention. Curr Opin Urol. 2018; 28(1): 55-61. https://doi.org/10.1097/MOU.0000000000000460.
- Rebello R.J., Oing C., Knudsen K.E., Loeb S., Johnson D.C., Reiter R.E., Gillessen S., Van der Kwast T., Bristow R.G. Prostate cancer. Nat Rev Dis Primers. 2021; 7(1): 9. https://doi.org/10.1038/s41572-020-00243-0.
- Taylor R.A., Fraser M., Rebello R.J., Boutros P.C., Murphy D.G., Bristow R.G., Risbridger G.P. The influence of BRCA2 mutation on localized prostate cancer. Nat Rev Urol. 2019; 16(5): 281-90. https://doi.org/10.1038/s41585-019-0164-8.
- Borja Menéndez D.A., Borja Menéndez K.A., Sánchez Núñez J.E., de la Santis García Velandria F.A. [Treatment of prostate cancer using high-intensity focused ultrasound, literature review]. Arch Esp Urol. 2021; 74(9): 815-20.
- Zimmer A.S., Gillard M., Lipkowitz S., Lee J.M. Update on PARP Inhibitors in Breast Cancer. Curr Treat Options Oncol. 2018; 19(5): 21. https://doi.org/10.1007/s11864-018-0540-2.
- Ruiz de Porras V., Font A., Aytes A. Chemotherapy in metastatic castration-resistant prostate cancer: Current scenario and future perspectives. Cancer Lett. 2021; 523: 162-9. https://doi.org/10.1016/j.canlet.2021.08.033.
- Xu G.P., Zhao Q., Wang D., Xie W.Y., Zhang L.J., Zhou H., Chen S.Z., Wu L.F. The association between BRCA1 gene polymorphism and cancer risk: a meta-analysis. Oncotarget. 2018; 9(9): 8681-94. https://doi.org/10.18632/oncotarget.24064.
- Wang S.S., Maurer M.J., Morton L.M., Habermann T.M., Davis S., Cozen W., Lynch C.F., Severson R.K., Rothman N., Chanock S.J., Hartge P., Cerhan J.R. Polymorphisms in DNA repair and one-carbon metabolism genes and overall survival in diffuse large B-cell lymphoma and follicular lymphoma. Leukemia. 2009; 23(3): 596-602. https://doi.org/10.1038/leu.2008.240.
- Solano A.R., Aceto G.M., Delettieres D., Veschi S., Neuman M.I., Alonso E., Chialina S., Chacón R.D., Renato M.C., Podestá E.J. BRCA1 And BRCA2 analysis of Argentinean breast/ovarian cancer patients selected for age and family history highlights a role for novel mutations of putative south-American origin. Springerplus. 2012; 1: 20. https://doi.org/10.1186/2193-1801-1-20.
- Ledwoń J.K., Hennig E.E., Maryan N., Goryca K., Nowakowska D., Niwińska A., Ostrowski J. Common low-penetrance risk variants associated with breast cancer in Polish women. BMC Cancer. 2013; 13: 510. https://doi.org/10.1186/1471-2407-13-510.
- Wang S.S., Maurer M.J., Morton L.M., Habermann T.M., Davis S., Cozen W., Lynch C.F., Severson R.K., Rothman N., Chanock S.J., Hartge P., Cerhan J.R. Polymorphisms in DNA repair and one-carbon metabolism genes and overall survival in difuse large B-cell lymphoma and follicular lymphoma. Leukemia. 2009; 23(3): 596-602. https://doi.org/10.1038/leu.2008.240.


