Allstone disease among the elderly population
Автор: Usmonov Husniddin Kutbinovich, Salahidinov Sarvarjon Zainabidinovich, Usmonov Elrbek Ilkhomovich
Журнал: Re-health journal @re-health
Статья в выпуске: 3,1 (7), 2020 года.
Бесплатный доступ
Gallstone disease is a very common digestive system disease among the population of the planet. It is especially common in the elderly population and women (Figure 1). This article discusses in detail the importance of this disease among the elderly.
Gallstone disease, digestive system, o't tosh, hazm tizimi
Короткий адрес: https://sciup.org/14125594
IDR: 14125594 | DOI: 10.24411/2181-0443/2020-10110
Текст научной статьи Allstone disease among the elderly population
Introduction: Cholelithiasis involves the presence of gallstones (see the image below), which are concretions that form in the biliary tract, usually in the gallbladder. Choledocholithiasis refers to the presence of one or more gallstones in the common bile duct (CBD). Treatment of gallstones depends on the stage of disease. This is associated with the increasing consumption of fatty food. With advances in radiological services, more patients are diagnosed with Gallstones. It is unique disease as it involves 3 organs namely the liver, gallbladder and pancreas. The clinical presentation varies depending on whether the bile flow is obstructed. Laparoscopic surgery offers a faster recovery and return to daily activities. The gallbladder is an organ located under the liver It functions as a store for bile produced by the liver. Bile is essential for the absorption and digestion of fat. When the semi-digested food passes the upper part of the small intestine called duodenum, a hormone called Cholecystokinin is released which stimulates bile release.
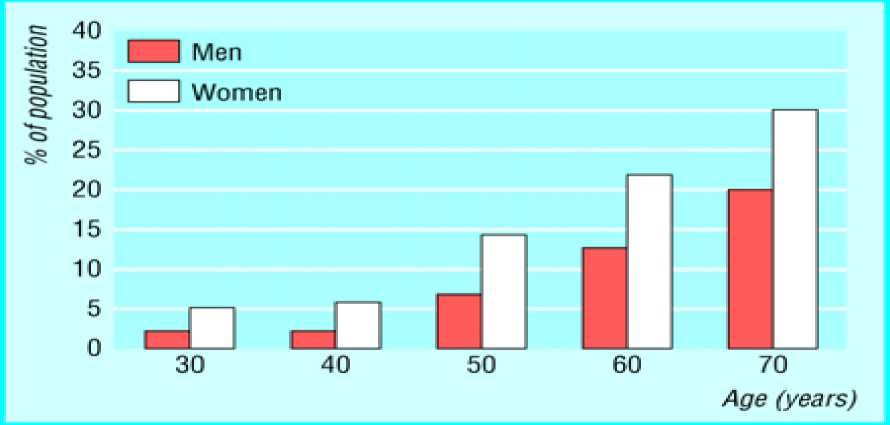
Figure 1.
This is associated with the increasing consumption of fatty food. With advances in radiological services, more patients are diagnosed with Gallstones. It is unique disease as it involves 3 organs namely the liver, gallbladder and pancreas. The clinical presentation varies depending on whether the bile flow is obstructed. Laparoscopic surgery offers a faster recovery and return to daily activities. The gallbladder is an organ located under the liver It functions as a store for bile produced by the liver. Bile is essential for the absorption and digestion of fat. When the semi-digested food passes the upper part of the small intestine called duodenum, a hormone called Cholecystokinin is released which stimulates bile release.
Gallstone disease is a very common condition in the general population. Prevalence of gallstones increases with age, from 8% in people younger than 40years old to more than 50% in people older than 70 [1]. In this last group, the incidence of symptomatic gallstone disease is around 30%, representing the most common cause of acute abdominal pain in elderly population [1, 2]. Elderly patients have been found to have higher risk of developing gallstone-related complications [3-6]. Furthermore, early recurrence of symptomatic disease in elderly population has been estimated around a third of patients on follow-up [5, 7-9], being these episodes related with increasing morbidity rates for each new episode [5, 7, 10]. Current guidelines recommend early cholecystectomy (EC) in order to prevent gallstone-related complications and recurrence in the absence of contraindication for the surgical procedure [11–13]. Although cholecystectomy has been described to be effective and safe for elderly patients [14–18], the treatment of symptomatic cholelithiasis with EC still remains a debatable issue. Elderly patients are less likely to undergo a surgical treatment, due to patient’s preference, surgeon reticence, and related comorbidities [9]. Finally, they present a higher risk of surgeryrelated complications with an increase in morbidity, mortality, costs, and recurrence rate (RR) [7, 9, 10]. Gallstone disease presents a high incidence and morbidity in elderly population. Although cholecystectomy is the most accepted treatment, a high proportion of elderly patients still undergo an NOM [8, 9]. Only a few studies have analyzed the RR after NOM of symptomatic gallstone disease in the elderly patients [5, 7–9, 11]. Previous retrospective analyses notified RR around one-third of patients after a 1-year follow-up [6, 9], increasing up to 40% in the long term [7, 8, 10]. A group of scientists came to the following conclusion from their research [12]: NOM of the first episode for symptomatic gallstone disease showed an RR of 39% after a 2-year follow-up. RR was related to the specific diagnosis and severity of the first episode at H1. If there are no contraindications for surgery, cholecystectomy should be considered during the initial admission in order to prevent relapses.
Another group of scientists conducted research on the treatment of elderly gallstone patients [13]. The aim of this study was to evaluate the differences in clinical outcomes of endoscopic retrograde cholangiopancreatography (ERCP), ERCP followed by cholecystectomy (EC) and percutaneous aspiration (PA) in the elderly population with choledocholithiasis. The results showed that, a patient’s age negatively affects the treatment outcomes of cholelithiasis with associated complications. The EC procedure appears to be the method of choice for the management of complicated gallstones in patients of all ages.
A number of other details can be cited. Cholelithiasis or gallstone disease is characterized by high prevalence ranging from 7 to 15% [15–17]. The treatment and morbidity associated with this condition constitute a significant financial burden [18, 19]. In 2012, there were almost 400 000 admissions for cholelithiasis with cholecystitis in the USA alone, and the aggregate expenses for in-hospital treatment exceeded 4 billion dollars [18]. Almost 2000 deaths (0.5%) were reported among the patients suffering from gallstone disease [18]. Moreover, although the causal mechanism is unknown, the presence of cholelithiasis is associated with a 30% higher all-cause mortality, mostly due to cardiovascular events and cancer [17]. Between 5 and 30% of cholelithiasis patients have concurrent choledocholithiasis or gallstones lodged in the common bile duct (CBD) [2022].
Endoscopic retrograde cholangiopancreatography (ERCP) is used for both diagnosis and treatment of choledocholithiasis [23–25]. It can be implemented prior to, during or after cholecystectomy and is considered to represent a low-risk intervention. Annually, 1.3 million procedures are performed and an overall complication rate is 5–10% [26,27]. Patients undergoing either ERCP or cholecystectomy have a 70% lower risk of biliary disease recurrence within 1 year [28]. In another study, ERCP alone was shown to reduce the recurrence by 37% [29]. These data are consistent with the conclusion that ERCP only is not sufficient to reach an optimal treatment outcome and that ERCP should be combined with cholecystectomy for adequate stone clearance [30]. In comparison with ERCP alone, a smaller number of stones remain in the CBD after cholecystectomy [31]. However, cholecystectomy after ERCP appears not to be necessary for patients with acalculous cholecystitis [32]. With the increase in the age of the population [33], the number of elderly patients undergoing treatment for symptomatic gallstones is expected to increase [34]. In fact, the proportion of emergency and elective surgical cases involving older patients is on the rise [35]. Of relevance, elderly surgical patients are characterized by higher indices of comorbidities than younger subjects [36–38], posing an additional challenge in the management of gallbladder stones. Although the mortality rate after cholecystectomy remains low (0.2–0.3%) [39–41], this fraction is increased in the older population and with increasing comorbidities. In fact, elderly patients were 7–10 times more likely to die post-operatively [39, 42].
Additionally, approximately 1% of patients who undergo laparoscopic cholecystectomy suffer from a procedure-related CBD injury. This adverse event is more common in the elderly and results more often in death in this age group [43]. Patients affected by diseases of the heart, lungs and kidneys, as well as type 2 diabetes—conditions more frequent in the older population—are more likely to die following cholecystectomy [40, 42, 44]. In order to lessen the risk of morbidity and mortality associated with cholecystectomy, elderly patients are recommended to undergo laparoscopic instead of open cholecystectomy [45]. Elective surgeries are preferred over emergency surgery, as they have a lower perioperative risk [46]. ERCP was found to be safe and effective for the elderly [23, 25, 47, 48]. However, combining this method with laparoscopic cholecystectomy, while improving the removal of gallbladder stones, may lead to increased complications such as bile leaks or adhesions [49, 50].
Alternatively, the reason for these complications might not be the ERCP itself, but pre-existing pathologies that prompted the use of ERCP in the first place [51]. Regardless of the underlying cause-and-effect relationships, the use of ERCP positively correlates with the necessity for conversion from laparoscopic to open surgery [52–55]. To date, only one study compared the outcomes of patients who underwent ERCP with and without cholecystectomy among the elderly and concluded that cholecystectomy after the ERCP does not provide a benefit to patients older than 80 years [56].
In view of the limited information regarding the impact of various types of treatment of gallbladder disease in the oldest patients, we have designed a study aiming at the comparison of in-hospital mortality, length of hospital stay and readmission rates after ERCP alone and ERCP followed by laparoscopic cholecystectomy in patients 60 years of age or older. Patients undergoing percutaneous aspiration (PA) were also included in the comparisons, since this protocol is considered to be a third-line option for the management of complicated gallstone disease in surgically high-risk patients [57]. Since the female gender was postulated to have a protective role against the complications of gallstone treatment [58, 59], the differences by gender were analysed as well.
According to Nassar's and Richter's average, the average age of the elderly patients included in the study was 75.6 6 8.7 years. Small but statistically significant differences in age were present among the treatment groups, with the EC patients being the youngest and the PA patients being the oldest. Males constituted a majority of EC and ERCP patients, while both genders were equally represented in the PA group. In each treatment group, the patients were predominantly Caucasian, and the proportion of Caucasian patients did not differ among the groups. Approximately half of the EC procedures were performed in a fully equipped operating room, while a significantly higher fraction, more than 90%, of ERCP and PA treatments took place outside operating rooms. Patients undergoing ERCP and PA were more likely to be affected by a chronic disease than those subjected to EC (Table 1).
|
EC (N = 20462) |
ERCP(N = 21938) |
PA(N = 938) |
|
|
Age (years, mean * SD) |
74.4 ± 8.3 |
76.7 t 8.9“ |
77.4 ± 9.1“* |
|
Gender, n (%) Male |
8925 (44.9) |
9327 (42.5)“ |
471 (50.2)“* |
|
Female |
11537 (55.1) |
12611(57.5)“ |
467 (49.8)“* |
|
Ethnicity White |
13131 (75.7) |
13902(63.3) |
599 (63.9) |
|
Black |
968 (5.6) |
1024(5.6) |
79 (9.5) |
|
Hispanic |
2135 (12.3) |
2012 (11.0) |
97 (11.7) |
|
Asian or Pacific Islander |
589 (3.4) |
844(4.6) |
21 (2.5) |
|
Native American |
67 (0.4) |
82 (0.5) |
3 (O.4) |
|
Other or unknown |
461 (2.7) |
487 (2.7) |
29 (3.5) |
|
Procedure in a major operating room Yes |
10613(51.9) |
640 (2.9)“ |
94 (10.0)“* |
|
No or unknown |
9849 (48.1) |
21298(97.1)“ |
844 (90.0)“b |
|
Chronic disease Ischemic heart disease |
4982 (24.4) |
6058 (27.6)“ |
387 (41.3)“* |
|
Heart failure |
2283 (11.2) |
3221 (14.7)“ |
302 (32.2)“* |
|
Chronic obstructive pulmonary disease |
3231 (15.8) |
3603 (16.4) |
195 (20.8)“* |
|
Cancer |
757 (3.7) |
1582 (7.2)“ |
87 (9.3)“* |
|
Any of the above |
8499 (41.5) |
10 496(47.8)“ |
628 (7.0)“* |
Table 1. Patient characteristics. ERCP, endoscopic retrograde cholangiopancreatography; EC, ERCP followed by cholecystectomy; PA, percutaneous aspiration. a,bIndicate a statistically significant difference vs EC and ERCP groups, respectively.
Conclusion: Gallstone disease is a actual disease that is common in the elderly and women and we have discussed it in detail in the article. Studies by several scientists have also been cited. We hope that this article will be the basis for great researchs on the prevention and treatment of gallstones disease among the elderly.
Список литературы Allstone disease among the elderly population
- Hendrickson M, Naparst TR.: Abdominal surgical emergencies in the elderly. Emerg Med Clin North Am 2003;21(4):937-969.
- Riall TS, Adhikari D, Parmar AD et al: The risk paradox: use of elective cholecystectomy in older patients is independent of their risk of developing complications. J Am Coll Surg 2015;220(4):682-690.
- Bedirli A, Sakrak O, Sozuer EM et al: Factors effecting the complications in the natural history of acute cholecystitis. Hepatogastroenterology 2001;48(41):1275-1278.
- Bergman S, Sourial N, Vedel I et al: Gallstone disease in the elderly: are older patients managed differently? Surg Endosc 2011;25(1):55-61.
- Lupinacci RM, Nadal LR, Rego RE et al: Surgical management of gallbladder disease in the very elderly: Are we operating them at the right time? Eur J Gastroenterol Hepatol 2013;25(3):380-384.