Alzheimer's disease: a threat to mankind
Автор: Pandey Poorti, Singh Mritunjai, Gambhir I.S.
Журнал: Журнал стресс-физиологии и биохимии @jspb
Статья в выпуске: 4 т.7, 2011 года.
Бесплатный доступ
Alzheimer's disease (AD) is neurodegenerative disorder common among elderly involving deficits in memory and cognition. There has been a long history of research and medical practice in AD worldwide, during which different facts came into light. During recent decades with new technologies being integrated, progress has been made in finding new genes responsible for AD, but diagnosis and treatment. In this review we will focus on molecular, genetic and other evidence underlying the known AD pathology.
Alzheimer, cholinesterase, dementia, neuritic plaques, neurofibrillary tangles
Короткий адрес: https://sciup.org/14323547
IDR: 14323547
Текст обзорной статьи Alzheimer's disease: a threat to mankind
Dementia is a serious loss of cognitive ability, is far more common in the geriatric population, it may occur before the age of 65 (Fadil et al, 2009). Dementia is not merely a problem of memory. It reduces the ability to learn, reason, retain or recall past experience and there is also loss of patterns of thoughts, feelings and activities. It is caused by various diseases that result in damaged brain cells, or connections between brain cells as listed in table 1. For diagnosing dementia, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) is preferred. (American Psychiatric Association, 1994)
-
• Early-onset Alzheimer's: This is a rare form (less than 10% cases) of AD in which people are diagnosed before age of 65. (Alzheimer’s Association, 2006)
-
• Late-onset Alzheimer's: This is the most common form of AD, accounting for about 90% of cases and usually occurring after age 65. Late-onset Alzheimer's disease strikes almost half of all people over the age of 85 and may or may not be hereditary. Late-onset dementia is also called sporadic AD. (Scott et al, 2008)
-
• Familial Alzheimer's disease (FAD ): This is a form of AD that is known to be entirely
inherited. In affected families, members of at least two generations have had AD. FAD is extremely rare, accounting for less than 1% of all cases of AD. It has a much earlier onset (often in the 40s) (Scott et al, 2008).
On average, AD patients live about 8 years after initial diagnosis, although the disease can last for as long as 20 years. The areas of the brain that control memory and thinking skills are affected first but, as the disease progresses, neurons in other regions of the brain are also affected. Eventually, the patient with AD will need complete care, adding further emotional, physical, and financial costs to the family (Vitaliano et al, 2003).
Amyloid Cascade hypothesis Missense mutations in APP, PS1or PS2 genes ▼
Subtle effects of Aβ oligomers on synapses ▼
Altered neuronal ionic homeostasis : Oxidative injury ▼
Altered kinase/phosphatase activities ►Tangles ▼
Dementia
Flowdiagram 1 T he sequence of pathogenic events leading to AD proposed by the amyloid cascade hypothesis. The curved arrow indicates that Aβ oligomers may directly injure the synapses and neurites of brain neurons, in addition to activating microglia and astrocytes. (Adopted from Hardy , et al, 2002 )
Table 1: Common Types of Dementia and Their Typical Characteristics
|
Type of Dementia |
Characteristics |
References |
|
Alzheimer’s disease |
Most common & severe type of dementia; 60 - 80 % cases fall under this category. Early symptoms involve memory loss, apathy, depression, mitochondrial damage and proteasome inhibition. Later symptoms include impaired judgment, disorientation, confusion, behavior changes and difficulty speaking, swallowing and walking. p-amyloid deposits (plaques) and twisted strands of the protein tail (tangles) are hallmarks. |
Yarikner BA 1991; Selkoe DJ et al 1994 |
|
Vascular dementia |
Second most common type of dementia. It is caused by lowering of blood flow to parts of the brain, often due to a series of small strokes that block arteries. Symptoms similar to those of Alzheimer’s, although memory may not be as seriously affected. |
Viswanathan A. et al., 2009 |
|
Mixed dementia |
Characterized by the hallmarks of Alzheimer’s and other type of dementia — mostly vascular dementia and dementia with Lewy bodies. Recent studies suggest that mixed dementia is more common than previously thought. |
Jellinger, K.A. 2007 |
|
Dementia with Lewy bodies |
Share decline patterns with Alzheimer’s, including problems with memory and judgment as well as behavior changes, fluctuation in alertness and severity of cognitive symptoms Visual hallucinations, muscle rigidity and tremors are common. Abnormal deposits of a-synuclein, leading to Lewy bodies formation |
Iseki E. et al,2003 |
|
Frontotemporal dementia |
Nerve cells in the front and side regions of the brain are especially affected. Changes in personality and behavior. No distinguishing microscopic abnormality. Pick’s disease, characterized by Pick’s bodies (nerve cells containing an abnormal accumulation of fibers of tau protein), is one type of frontotemporal dementia. |
Haberland C. 2010 |
|
Creutzfeldt- Jakob disease |
First symptom involve rapid progressive dementia, leading to memory loss, personality changes and hallucinations. Caused by the misfolding of prion protein throughout the brain. Variant Creutzfeldt-Jakob disease is believed to be caused by consumption of products from cattle affected by mad cow disease. |
Chakraborty C et al,2005 |
|
Normal pressure hydrocephalus |
Caused by the buildup of fluid in the brain. Symptoms include gait disturbance, urinary incontinence, and dementia or mental decline Can sometimes be corrected with surgical installation of a shunt in the brain to drain excess fluid. |
Adams R D. et al. (1965). Vanneste J et al 1992 |
|
Parkinson's disease |
Many people who have Parkinson’s disease (a disorder that usually involves movement problems) also develop dementia in the later stages of tire disease. The hallmark abnormality is Lewy bodies (a-synuclein-immunoreactive inclusions) made up of a number of neurofilament proteins together with proteins responsible for proteolysis . |
Miyasaki JM et al.,2006 Davie C. A. 2008 |
|
Huntington's disease. |
Characterized by a triad of symptoms: personality changes, dementia, and choreiform movements. Affected individuals may display problems with impulsive behavior,substance abuse, criminal activity, and sexual promiscuity. Depression is common early in the illness." Irritability and apathy are extremely common. The hallmark of HD is the loss of medium spiny GABAergic projection neurons |
Went L.N. et. al. 1975; Mayeux R 1984; Folstein S. et al.1983; Wexler N.S. 1979 |
Neurofibrillary tangles and senile plaques are the two characteristic hallmarks of disease, observed in alzheimer’s brain (Scott et al, 2008; Tiraboschi et al, 2004). Both amyloid plaques and neurofibrillary tangles can be visalised by microscopy in brains of those afflicted by AD. Plaques are dense, mostly insoluble deposits of amyloid-beta peptide and cellular material (dystrophic axons & dendrites) primarily. Activated microglia & reactive astrocytes outside and around neurons as well as α-synuclein, ubiquitin, apolipoprotein E, presenilins and alpha antichymotrypsin,are also observed (Yankner, 1991; Hardy, 1991; Joachim, 1992 Selkoe, 1994; Dewji, 1996; Wang, 1991; Kudo, 1994). A recent study has shown that Lewy bodies are present in the brains of about 60% of AD cases (Hamilton, 2000). Tangles (neurofibrillary tangles) are aggregates of the microtubule-associated protein tau which has become hyperphosphorylated and accumulate inside the cells themselves. Although many older individuals develop some plaques and tangles as a consequence of aging, the brains of AD patients have a greater number of them in specific brain regions such as the temporal lobe.
Molecular and Genetic aspect of AD
APP is an integral membrane protein as shown in figure 1, expressed in many tissues and concentrated in the synapses of neurons . In humans, the gene for APP is located on chromosome 21 (Table 3) and contains at least 18 exons in 240 kilobases (Thomas et al, 2007) Several alternative splicing isoforms of APP have been observed in humans, ranging in length from 695 to 770 amino acids with certain isoforms preferentially expressed in neurons; Mutations in this gene cause excessive cleavage by the β- and γ-secretase enzymes, instead of normal cleavage by the α-secretase enzyme (shown in flowdiagram 2). The result is increased production of toxic β-amyloid fragments a 39- to 42- amino acid peptide, which are converted into insoluble aggregates that form senile plaques in brain tissue associated with Alzheimer's disease
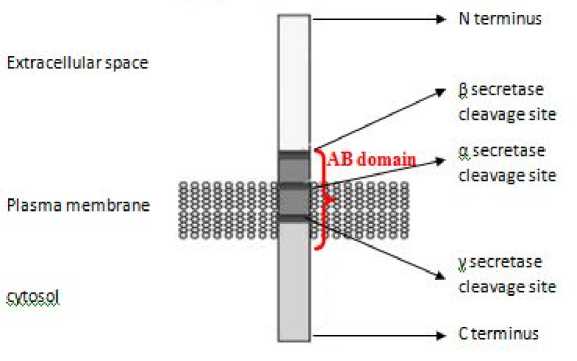
Figure 1: Structure of Amyloid precursor protein.
Table 2: Various methods of diagnosis
Diagnostic tool Types References Brain scan Computed tomography (CT)/Magnetic resonance imaging (MRI)/ Single photon emission computed tomography (SPECT)/ Positron emission tomography (PET) Abella 2009; Dougall, 2004 Cognitive assessment Abbreviated mental test score (AMTS)/Mini mental state examination (MMSE)/Modified Mini-Mental State Examination (3MS)/Cognitive Abilities Screening Instrument (CASI)/clock drawing test. Teng et al 1987 ; Teng et al 1994; Royall et al 1998 Laboratory test Vitamin B12, folic acid, thyroid-stimulating hormone (TSH), C-reactive protein, full blood count, electrolytes, calcium, renal function, and liver enzymes etc. to rule out treatable causes.
Table 3: Various genes responsible in AD pathology are summarized below:
|
Gene |
Chromosomal Location |
Pathological Significance |
References |
|
APP |
21q21.2 |
Senile Plaques formation |
Schellenberg (1995) |
|
PSI |
14q24.3 |
Enhance γ secretase activity |
Hardy (2001); Nishimura et al,(1999) |
|
PSII |
1q31.42 |
Enhance γ secretase activity |
Hardy (2001); Nishimura et al, (1999) |
|
Tau |
17q21.1 |
Neurofibrillary tangles formation |
Iqbal et al (1989) |
|
ApoE |
19q13.2 |
Not clear |
Roses (1997) |
Amyloid Precursor Protein (APP)
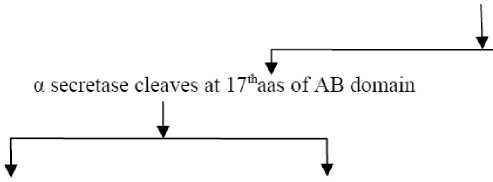
AB domain cleaved thus no Ap Peptide form
No AD pathology seen
Release large amino terminal fragment sAPPa
Cytosolic fragment subjected to cleavage by у secretase (cleaves at C terminal of AB domain)
P3 harmless fragment is released
P secretase cleaves at
N terminal of AB domain
Release amino terminal fragment sAPPp
Cytosolic fragment subjected to cleavage by у secretase
Release AB domain (Amyloid p peptide 40/42) oligomerisation^
Amyloid plaques
Flowdiagram 2: Cascade of APP cleavage in normal (left) and diseased state (right)
Two other genes that cause familial early-onset Alzheimer’s disease are presenilin-1, located on chromosome 14 (Shellenberg et al, 1992; Hardy 2001), and presenilin-2, located on chromosome 1 (Nishimura et al, 1999) (Table 3). Presenilins are a family of related multi-pass transmembrane proteins that function as a part of the gamma-secretase intramembrane protease complex and mutations lead to excessive cleavage by the γ- secretase enzyme. Aβ 42 is more likely to aggregate to form plaques in the brain than Aβ 40. Presenilin mutations lead to an increase in the ratio of Aβ 42 produced compared to Aβ 40, although the total quantity of Aβ produced remains constant. (Citron et al,1997)
Tau protein located on chromosome 17 (Table 3), are known to stabilize microtubules. They are abundant in neurons in the central nervous system and are less common elsewhere. Six tau isoforms exist in brain tissue, and they are distinguished by their number of binding domains. Three isoforms have three binding domains and the other three have four binding domains. The binding domains are located in the carboxy-terminus of the protein and are positively-charged (allowing it to bind to the negatively-charged microtubule). The isoforms with four binding domains are better at stabilizing microtubules than those with three binding domains. The isoforms are a result of alternative splicing in exons 2, 3, and 10 of the tau gene.
Hyperphosphorylation of the tau protein (tau inclusions, p-Tau) can result in the self-assembly of tangles of paired helical filaments and straight filaments, which are involved in the pathogenesis of AD and other tauopathies (Kosik, 1994). Abnormal hyperphosphorylation of the microtubule- associated tau protein and its incorporation into neurofibrillary tangles are major hallmarks of AD (Flament et al, 1989).
Until recently, only total tau protein (t-tau) as a marker of neuronal damage was detectable in cerebrospinal fluid (CSF). Elevated levels of CSF t-tau have been observed in patients with AD, even in those with mild dementia, compared with healthy elderly controls. However, CSF t-tau levels are of limited value in the differential diagnosis of AD, because they can be increased in other dementia disorders. Therefore, it appears likely that t-tau levels reflect neuronal degeneration rather than AD-specific pathophysiology. Detection of phosphorylated tau (p-tau) protein in the CSF therefore may provide a useful biomarker.
The protein, ApoE, is mapped to chromosome 19, (Table 3) and is known play fundamental role in maintenance and repair of neurons (Mahley, 1998; Mahley et al, 2000). The APOE gene consists of four exons and three introns, totaling 3597 base pairs. ApoE is polymorphic with three major isoforms, ApoE2 (5-10%), ApoE3 (60-70%), ApoE4 (15-20%), which translate into three alleles of the gene: Higher frequency of the ApoE4 allele is found in patients with AD than in the general population (Corder et al, 1993). However, the pathogenetic mechanism of ApoE4 in AD is unknown, there are few proposed mode of action . ApoE4 is known to inhibit neurite outgrowth, (Nathan et al, 1994; Bellosta et al, 1995) disrupt neuronal cytoskeleton (Nathan et al, 1994; Bellosta et al, 1995; Holtzman et al, 1995), stimulate tau phosphorylation (Tesseur et al, 2000; Huang et al, 2001) & causes neurodegeneration (Buttini et al, 1999). In vitro studies have shown that ApoE3 binds to the microtubule associated protein tau with high avidity, whereas ApoE4 does not bind tau, suggesting that
ApoE3, but not ApoE4, by binding to tau, slows the degree of tau phosphorylation and self assembly into paired helical filaments (Strittmatter al, 1994). It has also been suggested that intraneuronal ApoE, by interaction with tau protein, may influence the neuronal pathology in AD, from early in the disease (Han et al, 1994).
These allelic forms differ from each other only by amino acid substitutions at positions 112 and 158. E3 has Cys-112 and Arg-158 whereas E2 has Cys at both positions and E4 has Arg (Mahley et al, 1999). People who inherit one or two APOE ε4 alleles tend to develop AD at an earlier age than those who do not have any. APOE ε4 is called a risk-factor allele because it increases a person’s risk of developing AD with exceptions.
Besides these genes with technological advancement in genetic analysis over last few years lead to the discovery of new genes associated with late onset of AD. With the help of genome wide association study (GWAS) it is easy to screen several genes at a time which led to the discovery of novel genes, few among them are
-
1. CLU gene present on chromosome 8 (8p21), which is another apolipoprotein , like Apo E, may play a role in clearing β- amyloid out of brain (Harold et al, 2009).
-
2. PICALM (phosphatidyl inositol binding clathrin assembly protein), present on chromosome 11 (11q14) which seems to be involved in recycling of cell membrane protein at synapses (Harold et al, 2009).
-
3. CR1 (complement receptor 1) present on chromosome 1 (1q32) is an immunoprotein, responsible for inflammatory response may be involved in clearing β- amyloid from brain ( Jun et al, 2010).
-
4. ADAM 10 present on chromosome 15 (15q22.1) is an α- secretase, cleaves APP in a way leading to P3 formation thus ceases the Aβ peptide formation by β- secretase (Kim et al, 2009).
These 4 genes mentioned above are responsible for late onset of AD; mutation in any of them will increase the risk of AD.
In addition to aging & genetic factor there are many other risk factors like head injury (traumatic brain injury) (Lye et al, 2000), strokes & ministrokes, unhealthy habits (Anstey et al, 2007), high cholesterol (Sjogren et al, 2005), low level of formal education & low social-economic status. Cardiovascular and cerebrovascular and vascular risk factors (Korf et al, 2005; Decarli, 2004) cardiovascular disease and subgroups of patients with peripherial arterial disease (Newman et al, 2005) and elevated plasma total homocysteine concentrations and low serum folate concentrations (Ravaglia et al, 2005). Zinc metabolism (Mocchegiani et al, 2005), loss of microglial cell function (Streit, 2005); and decreased melatonin (Srinivasan et al, 2005). Environmental factors, such as heavy metal exposure (Treiber, 2005), have been investigated for many years.
Nutrition and lifestyle factors, such as midlife obesity (Kivipelto et al, 2005), lack of exercise (Kiraly et al, 2005) and watching too much television in middle-adulthood (Lindstrom et al, 2005), have been associated with an increased risk for AD. Even a man’s height has been associated with risk. Researchers have reported that short men are at increased risk (presumably due to its association with childhood nutrition and other risk factors) for dementia (Beeri et al, 2005).
Down’s syndrome results in trisomy of chromosome 21. Those suffering from this disease
& survive beyond 40s are at high risk of developing abnormal brain changes that characterize AD but not all of them develop dementia (Lott et al, 2005; Nistor et al, 2007), this led to the discovery of the APP gene on chromosome 21 (Goldgaber et al, 1987). People with Down syndrome are particularly at risk for a form of early onset Alzheimer's disease (Alzheimer’s Association, 2006).
Diabetes mellitus (DM) and AD are the two most devastating health problems in elderly. Diabetes is associated with cognitive decline and dementia. Indeed, individuals with diabetes are nearly 1.5 times more likely to experience cognitive decline and frank dementia than individuals without diabetes (Cukierman et al, 2005). Multiple possible mechanisms for this association have been proposed, including direct effects of hyperglycemia, insulin resistance, and insulin- induced amyloid-β peptide (Aβ) amyloidosis in the brain as well as indirect ischemic effects of DM-promoted cerebrovascular disease (Biessels et al, 2005). Diabetes increases the risk of Alzheimer disease and vascular dementia. The risk is stronger when diabetes occurs at mid-life than in late life (Xu et al, 2009).
Oxidative and Nitrosylative Damage Hypothesis states that, reactive oxygen species (ROS) and reactive nitrogen species (RNS) are important in the initiation and promotion of neurodegeneration in the brains of patients with AD (Anderton B). Some of these free radicals are released during inflammatory reactions, whereas others are formed during normal oxidative metabolism and auto-oxidation of certain neurotransmitters and by β-amyloid. Thus, the role of free radicals in the pathogenesis of AD should be considered, at least in part, independent of inflammatory reactions. Clinical studies showing the beneficial effects of high dose antioxidants such as vitamin E (Sano et al, 1997) and NADH (Birkmayer, 1996) in the treatment of AD support the role of free radicals in progressive degeneration of neurons.
There are currently no means for reversing the pathological processes of AD. Normal physiology of brain deals in transmitting messages (impulses) along nerve fibre by electrical mechanism. This electricity is insufficient to cross junction, thus impulse release neurotransmitter acetylcholine (ACh) which diffuses across junction to stimulate next cell, after purpose is solved these are eliminated by cholinesterase, otherwise disastrous stimulating downstream cell. In diseased state, as nerve endings become sick so the concentration of ACh released get progressively smaller, hence unable to transmit message across junction Thus cholinesterase inhibitors are used to prevent cholinesterase from destructing ACh. Few drugs in this category are Galantamine, Rivastigamine and Donepezil (Doody et al, 2001)
Another is Memantine (NMDA receptor antagonist) responsible for blocking glutamate receptors (involved in recycling of glutamate another neurotransmitter) (Reisberg et al, 2003). Few others may include secretase inhibitors, or one interacting with Aβ thus preventing its accumulation. Thus therapy stresses on preserving cognitive and functional ability and delay progression rather treating AD.
Abella, H.A. (2009) Report from SNM: PET imaging of brain chemistry bolsters characterization of dementias. Diagnostic Imaging, June 16, 2009.
Adams, R.D., Fisher, C.M., Haskim, S. et al. (1965) Symptomatic occult hydrocephalus with "normal" cerebrospinal fluid pressure. A treatable syndrome. Journal of Medicine, 273, 117-126.
Alzheimer’s Association. (2006) Early-Onset Dementia: A National Challenge, A Future Crisis . Alzheimer’s Association.
Washington, D.C.
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), Fourth Edition. Washington, D.C.: American Psychiatric Press 47-62.
Anderton, B Free radicals on the mind. Hydrogen peroxide mediates amyloid beta protein toxicity. Human Exp Toxicol 13 : 719,
Anstey, K.J., von Sanden, C., Salim, A., O’Kearney, R. (2007) Smoking as a risk factor for dementia and cognitive decline: A metaanalysis of prospective studies. American Journal of Epidemiology ; 166(4) : 367–378
Beeri, M.S., Davidson, M., Silverman, J.M., Noy, S., Schmeidler, J., Goldbourt, U. (2005) Relationship between body height and dementia. Am J Geriatr Psychiatry ; 13 : 116-123.
Biessels, G.J., Kappelle, L.J., (2005) Increased risk of Alzheimer’s disease in type II diabetes: insulin resistance of the brain or insulin-induced amyloid pathology? Biochem Soc Trans . 33 , 1041-1044.
Birkmayer, J.G., (1996) Coenzyme nicotinamide adenine dinucleotide: new therapeutic approach for improving dementia of the Alzheimer type. Ann Clin Lab Sci 26: 1–9.
Buttini, M., Orth, M., Bellosta, S., Akeefe, H. ,Pitas, R.E., Wyss- Coray, T., Mahley, R.W. (1999) Expression ofhuman apolipoprotein E3 or E4 in the APOE -/-mice : Isoforms specific effects on neurodegeneration J. Neuroscience 19 , 4867-4880
Calabrese, V., Butterfield, D.A., Stella, AM. (2003) Nutritional antioxidants and the heme oxygenase pathway of stress tolerance: novel targets for neuroprotection in Alzheimer's disease. Ital J Biochem ; 52 : 177-181.
Calabrese, V., Scapagnini, G., Colombrita, C., Ravagna, A., Pennisi, G., Giuffrida, Stella, A.M., Galli, F., Butterfield, D.A. (2003) Redox regulation of heat shock protein expression in aging and neurodegenerative disorders associated with oxidative stress: a nutritional approach. Amino Acids ; 25 : 437444.
Chakraborty, C., Nandi, S., Jana, S. (2005) "Prion disease: a deadly disease for protein misfolding". C urrent Pharmaceutical Biotechnology 6 (2) : 167–77.
Citron, M., Westaway, D., Xia, W., Carlson, G., Diehl, T., Levesque, G., Johnson-Wood K., Lee M. et al (1997) "Mutant presenilins of Alzheimer's disease increase production of 42-residue amyloid beta-protein in both transfected cells and transgenic mice". Nat. Med. 3 (1) : 67–72
Corder, E.H., Saunders, A.M., Strittmatter, W.J. et al . (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science ; 261 : 921–30.
Cukierman, T., Gerstein, H.C., Williamson, J.D., (2005) Cognitive decline and dementia in diabetes— a systematic overview of prospective observationalstudies.
Diabetologia 42 : 2460– 2469.
Davie, C. A. (2008) A review of Parkinson’s disease British Medical Bulletin ; 86 : 109–127
Decarli, C. (2004) Vascular factors in dementia: an overview. J Neurol Sci, 226 : 19-23.
Dewji, N.N., Singer, S.J. (1996) Genetic clues to Alzheimer’s disease. Science 271 : 159–160.
Doody, R.S., Stevens, J.C., Beck, C. et al. (2001) Practice parameter: management of dementia American Academy of Neurology. Neurology 56 . 1154–1166
Dougall, N.J., Bruggink, S., Ebmeier, K.P., (2004) "Systematic review of the diagnostic accuracy of 99mTc-HMPAO-SPECT in dementia". The American Journal of Geriatric Psychiatry 12 (6) : 554–70.
Fadil, H., Borazanci, A., Haddou, E. A. B.,Yahyaoui, M., Korniychuk, E., Jaffe, S. L., Minagar, A. (2009). "Early Onset Dementia". International Review of Neurobiology 84 : 245-262
Flament, S., Delacourte, A., Hemon, B., Defossez (1989) Direct biochemical evidence for an abnormal phosphorylation of tau proteins during Alzheimer disease. C.R. Acad. Sci. Paris 308 , 77-82.
Folstein, S., Abbott, M.H., Chase, G.A., Jenses, B.A., Folstein. M.F. (1983) The association of affective disorder with Huntington's disease in a case series and in families. Psychol Med ; 13 : 537-542.
Frank, R.A., Galasko, D. et al. (2003) Biological markers for therapeutic trails in
Alzheimer’s disease proceedings of the biological markers working groups ; NIA initiative on neuroimaging in Alzheimer’s disease. Neurobiology of Aging 24 : 521536
Goldgaber, D., Lerman, M.I., McBride, O.W. et al: (1987) Characterization and chromosomal localization of a cDNA encoding brain amyloid of Alzheimer’s disease. Science 235 : 877–880
Haberland, C. (2010) "Frontotemporal dementia or frontotemporal lobar degeneration- overview of a group of proteinopathies". Ideggyogyaszati szemle 63 (3-4): 87–93
Hamilton, R.L. (2000) Lewy bodies in Alzheimer’s disease: a neuropathological review of 145 cases using alpha-synuclein immunohistochemistry. Brain Pathol 10 : 378–384.
Han, S.H., Hulette, C., Saunders, A.M., et al. (1994) Apolipoprotein E is present in hippocampal neurons without neurofibrillary tangles in Alzheimer’s disease and age-matched controls. Exp Neurol ; 128 : 13–26
Hardy, J., Allsop, D. (1991) Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends in Pharmacological Sciences 12 : 383–388.
Hardy, J. (2001) The genetic causes of neurodegenerative diseases. J. Alzheimer’s Dis., 3 , 109–116.
Harold, D., Abraham, R., Hollingworth, P., Sims, R., Gerrish, A., et al (2009) Genome-wide association study identifies variants in CLU and PCALM associated with Alzheimer’s disease. Nature Genetics ; 41(10) : 10881093.
Holtzman, D.M., Pitas, R.E., Kilbridge, J., Nathan, B.P., Mahley, R.W., Bu, G. Schwartz, A.L. (1995) Low Density Lipoprotein Receptor-Related Protein Mediates Apolipoprotein EDependent Neurite Outgrowth in a Central Nervous System-Derived Neuronal Cell Line. Proc. Natl. Acad. Sci . USA 92 , 94809484
Huang, Y., Liu, X.Q., Wyss- Coray, T., Brecht, W.J., Sanan, D.A., Mahley, R.W. (2001) Apolipoprotein E fragments present in Alzheimer's disease brains induce neurofibrillary tangle-like intracellular inclusions in neurons. Proc Natl. Acad. Sci. USA 98 , 8838-8843.
Iseki, E., Togo, T., Suzuki, K., Katsuse, O., Marui, W., de Silva, R., Lees, A., Yamamoto, T., Kosaka, K. (2003) "Dementia with Lewy bodies from the perspective of tauopathy". Acta Neuropathol. 105 (3) : 265–70
Jellinger, K.A. (2007) The enigma of mixed dementia. Alzheimer’s & Dementia ; 3(1) : 40–53.
Jellinger, K.A., Attems, J. (2007) Neuropathological evaluation of mixed dementia. Journal of Neurological Sciences 257(1–2) : 80–87.
Joachim, C.L., Selkoe, D.J. (1992) The seminal role of beta-amyloid in the pathogenesis of Alzheimer disease. Alzheimer Dis Assoc Disord 6 : 7–34,
Jun, G, Naj, A.C., Beecham, G.W., Wang, L.S., Buros, J., Gallins, P.J., Buxbaum, J.D. et al (2010) Meta-analysis confirm.s CR1, CLU, and PICALM as Alzheimer disease risk loci and reveals interactions with APOE genotypes. Archives of Neurology. 67(12): 1473-1484
Kim, M., Suh, J., Romano, D., Truong, M.H., Mullin, K. et al. (2009) Potential late-onset Alzheimer’s disease-associated mutations in the ADAM10 gene attenuate α-secretase activity. Human Molecular Genetics 18(20) : 3987-3996.
Kiraly, M.A., Kiraly, S.J. (2005) The effect of exercise on hippocampal integrity: review of recent research. Int J Psychiatry Med, 35 : 75-89.
Kivipelto, M., Ngandu, T, Fratiglioni, L., Viitanen, M., Kareholt, I., Winblad, B., Helkala, E.L., Tuomilehto, J., Soininen, H., Nissinen, A. (2005) Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol, 62 : 15561560.
Korf, E.S., Scheltens, P., Barkhof, F., de Leeuw, F.E. (2005) Blood Pressure, White Matter Lesions and Medial Temporal Lobe Atrophy: Closing the Gap between Vascular Pathology and Alzheimer's Disease? Dement Geriatr Cogn Disord, 20 : 331-337.
Kosik, K., Greenberg, S. (1994) Tau protein and Alzheimer's disease. In Alzheimer's Disease. Raven Press, New York. 335-344.
Kudo, T., Iqbal, K., Ravid, R., Swaab, D.F., Grundke-Iqbal I. (1994) Alzheimer disease: correlation of cerebro-spinal fluid and brain ubiquitin levels. Brain Res 639 : 1–7.
Lindstrom, H.A., Fritsch, T., Petot, G., Smyth, K.A., Chen, C.H., Debanne, S.M., Lerner, A.J., Friedland, R.P. (2005) The relationships between television viewing in midlife and the development of Alzheimer's disease in a case-control study. Brain Cogn, 58: 157165.
Lott, I.T., Head, E. (2005) "Alzheimer disease and Down syndrome: factors in pathogenesis". Neurobiol Aging 26 (3) : 383–89.
Lye, T.C., Shores, EA. (2000) Traumatic brain injury as a risk factor for Alzheimer’s disease: A review. Neuropsychology Review, 10 : 115–129.
Mahley, R.W. (1998) Apolipoprotein E: cholesterol transport protein with expanding role in cell biology. Science 240 , 622-630
Mahley, R.W., Huang, Y., Rall, S.C., Jr., (1999) Pathogenesis of type III hyperlipoproteinemia (dysbetalipoproteinemia): questions, quandaries, and paradoxes J. lipid Res. 40, 1933-1949
Mahley, R.W., Rall, S.C., Jr., (2000) Apolipoprotein E: far more than a lipid transport protein. Annu. Rev. Genomics Hum. Genet. 1 , 507537
Mayeux, R., (1984) Behavioral manifestations of movement disorders:Parkinson's and Huntington's disease. Neurol Clin, 2 : 527540
Miyasaki JM, Shannon K, Voon V, Ravina B, Kleiner-Fisman G, Anderson K, et al. 2006 Practice parameter: evaluation and treatment of depression, psychosis, and dementia in Parkinson disease Neurology, 66 : 996-1002.
Mocchegiani, E., Bertoni-Freddari, C., Marcellini, F., Malavolta, M. (2005) Brain, aging and neurodegeneration: role of zinc ion availability. Prog Neurobiol, 75 : 367-390
Nathan, B.P., Bellosta, S., Sanan, D.A., Weisgraber, K.H., Mahley, R.W., Pitas, R.E. (1994) Differential effects of apolipoproteins E3 and E4 on neuronal growth in vitro. Science 264 , 850-852
Newman, A.B., Fitzpatrick, A.L., Lopez, O., Jackson, S., Lyketsos, C., Jagust, W., Ives, D., Dekosky, S.T., Kuller, L.H. (2005) Dementia and Alzheimer's disease incidence in relationship to cardiovascular disease. J Am Geriatr Soc, 53 : 1101-1107
Nishimura, M., Yu, G. and St George-Hyslop, P.H. (1999) Biology of presenilins as causative molecules for Alzheimer disease. Clin. Genet., 55 , 219–225
Nistor, M., Don, M., Parekh, M. et al. (2007) Alpha-and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain. Neurobiol Aging 28 (10) : 1493–1506
Plassman, B.L., Langa, K.M., Fisher, G.G., Heeringa, S.G., Weir, D.R. et al. (2007) Prevalence of dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology, 29 (12) : 125–132.
Ravaglia, G., Forti, P., Maioli, F., Martelli, M., Servadei, L., Brunetti, N., Porcellini, E., Licastro, F. (2005) Homocysteine and folate as risk factors for dementia and Alzheimer disease. Am J Clin Nutr, 82 : 636-643
Reisberg, B., Doody, R., Stoffler, A. et al. (2003) Memantine in moderate-to-severe Alzheimer's disease. N Engl J Med . 348 : 1333–1341.
Roses, A.D. (1997) A model for susceptibility polymorphisms for complex diseases:apolipoprotein E and Alzheimer’s disease. Neurogenetics, 1, 1–3.
Royall, D., Cordes, J., Polk, M. (1998) "CLOX: an executive clock drawing task". J Neurol Neurosurg Psychiatry 64 (5) : 588–594.
Sano, M., Ernesto, C., Thomas, R.G., Klauber, M.R., Schafer, K., Grundman, M., Woodbury, P., Growdon, J., Cotman, C.W., Pfeiffer, E., Schneider, L.S., Thal, L.J. (1997) A controlled trial of selegiline, alphatocopherol, or both as treatment for Alzheimer’s disease. N Engl J Med 336 : 1216–1222.
Schellenberg, G.D. (1995) Genetic dissection of Alzheimer disease, a heterogeneous disorder. Proc. Natl Acad. Sci. USA 92 , 8552–8559
Scott, A., Small, Duff, K. (2008) Linking Aβ and Tau in Late-Onset Alzheimer’s Disease: A Dual Pathway Hypothesis . Neuron 60 , Elsevier Inc
Selkoe, D.J. (1994) Cell biology of the amyloid beta-protein precursor and the mechanism of Alzheimer’s disease. Annu Rev Cell Biol 10 : 373–403,
Seshadri, S., Wolf, P.A., Beiser, A., Au, R., McNulty, K. et al. (1997) Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham Study. Neurology 49(6) : 1498–1504
Shellenberg, G.D., Bird, T.D., Wijsman, E.M. et al: (1992) Genetic linkage evidence for a familial Alzheimer’s disease locus on chromosome 14. Science ; 258 : 668–671
Sjogren, M., Blennow, K. (2005) The link between cholesterol and Alzheimer's disease. World J Biol Psychiatry; 6 : 85-97.
Sohal, R.S., Weindruch, R. (1996) Oxidative stress, caloric restriction, and aging. Science, 273 : 59–63
Srinivasan, V., Pandi-Perumal, S.R., Maestroni, G.J., Esquifino, A.I., Hardeland, R., Cardinali, D.P. (2005) Role of melatonin in neurodegenerative diseases. Neurotox Res, 7: 293-318.
Streit, W.J. (2005) Microglia and neuroprotection: implications for Alzheimer's disease. Brain Res Brain Res Rev, 48 : 234-239.
Strittmatter, W.J., Weisgraber, K.H., Goedert, M. et al. (1994) Hypothesis: microtubule instability and paired helical filaments formation in the Alzheimers disease brain are related to apolipoprotein E genotype. Exp Neurol, 125 : 163–171.
Teng, E.L., Chui, H.C. (1987) "The Modified MiniMental State (3MS) examination". The Journal of Clinical Psychiatry 48 (8) : 314– 318.
Teng, E.L., Hasegawa, K., Homma, A. et al. (1994) The Cognitive Abilities Screening Instrument (CASI): a practical test for cross-cultural epidemiological studies of dementia. International Psychogeriatrics / IPA 6 (1) : 45–58.
Tesseur, I., Van Dorpe, J., Bruynseels, K. Bronfman, F. Sciot, R., Van Lommel, A., Van Leuven. F. (2000) The Role of ApoE in Alzheimer's Disease: An Alternative View Am. J. Pathol. 157 , 1495-1510
Tesseur, I., Van Dorpe, J., Spittaels, K., Van den Haute, C., Moechars, D. Van Leuven, F. (2000) Expression of human apolipoprotein E4 in neurons causes hyperphosphorylation of protein tau in the brains of transgenic mice. Am. J. Pathol. 156 , 951-964
Thomas, P., Fenech, M. (2007) A review of genome mutation and Alzheimer’s disease. Mutagenesis 22(1) . 15–33.
Tiraboschi, P., Hansen, L.A., Thal, L.J., Corey-Bloom J. (2004) The importance of neuritic plaques and tangles to the development and evolution of AD. Neurology 62 (11) : 1984– 1989
Treiber, C. (2005) Metals on the brain. Sci Aging Knowledge Environ 36 pe27
Vanneste, J., Augustijn, P., Dirven, C., Tan, W.F., Goedhart, Z.D. (1992) Shunting normalpressure hydrocephalus: do the benefits outweigh the risks? Neurology, 42(1) : 5459
Viswanathan, A., Rocca, W.A., Tzourio, C. (2009) Vascular risk factors and dementia: How to move forward? Neurology 72 : 368–374
Vitaliano, P.P., Zhang, J., Scanlan, J.M. (2003) Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin 129(6) : 946–972.
Wang, G.P., Khatoon, S., Iqbal, K., Grundke-Iqbal I. (1991) Brain ubiquitin is markedly elevated in Alzheimer disease. Brain 566 : 146–151.
Went, L.N., Vester-Van der Vlis, M., Volkers, W. et al: (1975) Early Diagnosis and Prevention of Genetic Diseases. The Netherlands: Leiden University Press ; 13-25.
Wexler, N.S. (1979) Perceptual-motor, cognitive, and emotional characteristics of persons at risk for Huntington's disease. Adv Neurol, 23 : 257-271.
Xu ,W., Qiu, C., Gatz, M., Pedersen, N. L., Johansson, B., Fratiglioni, L. (2009) Mid- and Late-Life Diabetes in Relation to the Risk of Dementia Diabetes 58, 71-77
Yankner, B.A., Mesulam, M.M. (1991) Seminars in medicine of the Beth Israel Hospital,
Boston. beta-Amyloid and the pathogenesis of Alzheimer’s disease. N Engl J Med 325 : 1849–1857
Список литературы Alzheimer's disease: a threat to mankind
- Abella, H.A. (2009) Report from SNM: PET imaging of brain chemistry bolsters characterization of dementias. Diagnostic Imaging, June 16, 2009.
- Adams, R.D., Fisher, C.M., Haskim, S. et al. (1965) Symptomatic occult hydrocephalus with "normal" cerebrospinal fluid pressure. A treatable syndrome. Journal of Medicine, 273, 117-126.
- Alzheimer's Association. (2006) Early-Onset Dementia: A National Challenge, A Future Crisis. Alzheimer's Association. Washington, D.C.
- American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), Fourth Edition. Washington, D.C.: American Psychiatric Press 47-62.
- Anderton, B Free radicals on the mind. Hydrogen peroxide mediates amyloid beta protein toxicity. Human Exp Toxicol 13: 719,
- Anstey, K.J., von Sanden, C., Salim, A., O'Kearney, R. (2007) Smoking as a risk factor for dementia and cognitive decline: A meta-analysis of prospective studies. American Journal of Epidemiology; 166(4): 367-378
- Beeri, M.S., Davidson, M., Silverman, J.M., Noy, S., Schmeidler, J., Goldbourt, U. (2005) Relationship between body height and dementia. Am J Geriatr Psychiatry; 13: 116-123.
- Bellosta, S., Nathan, B.P., Orth, M., Dong, L.M., Mahley, R.W. Pitas, R.E. (1995) Stable expression and secretion of apolipoproteins E3 and E4 in mouse neuroblastoma cells produces differential effects on neurite outgrowth. J.Biol.Chem, 270, 27063-27071
- Biessels, G.J., Kappelle, L.J., (2005) Increased risk of Alzheimer's disease in type II diabetes: insulin resistance of the brain or insulin-induced amyloid pathology? Biochem Soc Trans. 33, 1041-1044.
- Birkmayer, J.G., (1996) Coenzyme nicotinamide adenine dinucleotide: new therapeutic approach for improving dementia of the Alzheimer type. Ann Clin Lab Sci 26: 1-9.
- Buttini, M., Orth, M., Bellosta, S., Akeefe, H.,Pitas, R.E., Wyss-Coray, T., Mahley, R.W.(1999) Expression ofhuman apolipoprotein E3 or E4 in the APOE -/-mice: Isoforms specific effects on neurodegeneration J. Neuroscience 19, 4867-4880
- Calabrese, V., Butterfield, D.A., Stella, AM. (2003) Nutritional antioxidants and the heme oxygenase pathway of stress tolerance: novel targets for neuroprotection in Alzheimer's disease. Ital J Biochem; 52: 177-181.
- Calabrese, V., Scapagnini, G., Colombrita, C., Ravagna, A., Pennisi, G., Giuffrida, Stella, A.M., Galli, F., Butterfield, D.A. (2003) Redox regulation of heat shock protein expression in aging and neurodegenerative disorders associated with oxidative stress: a nutritional approach. Amino Acids; 25: 437-444.
- Chakraborty, C., Nandi, S., Jana, S. (2005) "Prion disease: a deadly disease for protein misfolding". C urrent Pharmaceutical Biotechnology 6 (2): 167-77.
- Citron, M., Westaway, D., Xia, W., Carlson, G., Diehl, T., Levesque, G., Johnson-Wood K., Lee M. et al (1997) "Mutant presenilins of Alzheimer's disease increase production of 42-residue amyloid beta-protein in both transfected cells and transgenic mice". Nat. Med. 3 (1): 67-72
- Corder, E.H., Saunders, A.M., Strittmatter, W.J. et al. (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science; 261: 921-30.
- Cukierman, T., Gerstein, H.C., Williamson, J.D., (2005) Cognitive decline and dementia in diabetes-a systematic overview of prospective observationalstudies. Diabetologia 42: 2460-2469.
- Davie, C. A. (2008) A review of Parkinson's disease British Medical Bulletin; 86: 109-127
- Decarli, C. (2004) Vascular factors in dementia: an overview. J Neurol Sci, 226: 19-23.
- Dewji, N.N., Singer, S.J. (1996) Genetic clues to Alzheimer's disease. Science 271: 159-160.
- Doody, R.S., Stevens, J.C., Beck, C. et al. (2001) Practice parameter: management of dementia American Academy of Neurology. Neurology 56. 1154-1166
- Dougall, N.J., Bruggink, S., Ebmeier, K.P., (2004) "Systematic review of the diagnostic accuracy of 99mTc-HMPAO-SPECT in dementia". The American Journal of Geriatric Psychiatry 12 (6): 554-70.
- Fadil, H., Borazanci, A., Haddou, E. A. B.,Yahyaoui, M., Korniychuk, E., Jaffe, S. L., Minagar, A. (2009). "Early Onset Dementia". International Review of Neurobiology 84: 245-262
- Flament, S., Delacourte, A., Hemon, B., Defossez (1989) Direct biochemical evidence for an abnormal phosphorylation of tau proteins during Alzheimer disease. C.R. Acad. Sci. Paris 308, 77-82.
- Folstein, S., Abbott, M.H., Chase, G.A., Jenses, B.A., Folstein. M.F. (1983) The association of affective disorder with Huntington's disease in a case series and in families. Psychol Med; 13: 537-542.
- Frank, R.A., Galasko, D. et al. (2003) Biological markers for therapeutic trails in Alzheimer's disease proceedings of the biological markers working groups; NIA initiative on neuroimaging in Alzheimer's disease. Neurobiology of Aging 24: 521-536
- Goldgaber, D., Lerman, M.I., McBride, O.W. et al: (1987) Characterization and chromosomal localization of a cDNA encoding brain amyloid of Alzheimer's disease. Science 235: 877-880
- Haberland, C. (2010) "Frontotemporal dementia or frontotemporal lobar degeneration-overview of a group of proteinopathies". Ideggyogyaszati szemle 63 (3-4): 87-93
- Hamilton, R.L. (2000) Lewy bodies in Alzheimer's disease: a neuropathological review of 145 cases using alpha-synuclein immunohistochemistry. Brain Pathol 10: 378-384.
- Han, S.H., Hulette, C., Saunders, A.M., et al. (1994) Apolipoprotein E is present in hippocampal neurons without neurofibrillary tangles in Alzheimer's disease and age-matched controls. Exp Neurol; 128: 13-26
- Hardy, J., Allsop, D. (1991) Amyloid deposition as the central event in the aetiology of Alzheimer's disease. Trends in Pharmacological Sciences 12: 383-388.
- Hardy, J. (2001) The genetic causes of neurodegenerative diseases. J. Alzheimer's Dis., 3, 109-116.
- Harold, D., Abraham, R., Hollingworth, P., Sims, R., Gerrish, A., et al (2009) Genome-wide association study identifies variants in CLU and PCALM associated with Alzheimer's disease. Nature Genetics; 41(10): 1088-1093.
- Holtzman, D.M., Pitas, R.E., Kilbridge, J., Nathan, B.P., Mahley, R.W., Bu, G. Schwartz, A.L. (1995) Low Density Lipoprotein Receptor-Related Protein Mediates Apolipoprotein E-Dependent Neurite Outgrowth in a Central Nervous System-Derived Neuronal Cell Line. Proc. Natl. Acad. Sci. USA 92, 9480-9484
- Huang, Y., Liu, X.Q., Wyss-Coray, T., Brecht, W.J., Sanan, D.A., Mahley, R.W. (2001) Apolipoprotein E fragments present in Alzheimer's disease brains induce neurofibrillary tangle-like intracellular inclusions in neurons. Proc Natl. Acad. Sci. USA 98, 8838-8843.
- Iqbal, K., Grundke-Iqbal, I., Smith, A.J., George, L., Tung, Y.C., Zaidi, T. (1989) Identification and localization of a tau peptide to paired helical filaments of Alzheimer disease. Proc. Natl Acad. Sci.USA, 86, 5646-5650
- Iseki, E., Togo, T., Suzuki, K., Katsuse, O., Marui, W., de Silva, R., Lees, A., Yamamoto, T., Kosaka, K. (2003) "Dementia with Lewy bodies from the perspective of tauopathy". Acta Neuropathol. 105 (3): 265-70
- Jellinger, K.A. (2007) The enigma of mixed dementia. Alzheimer's & Dementia; 3(1): 40-53.
- Jellinger, K.A., Attems, J. (2007) Neuropathological evaluation of mixed dementia. Journal of Neurological Sciences 257(1-2): 80-87.
- Joachim, C.L., Selkoe, D.J. (1992) The seminal role of beta-amyloid in the pathogenesis of Alzheimer disease. Alzheimer Dis Assoc Disord 6: 7-34,
- Jun, G, Naj, A.C., Beecham, G.W., Wang, L.S., Buros, J., Gallins, P.J., Buxbaum, J.D. et al (2010) Meta-analysis confirm.s CR1, CLU, and PICALM as Alzheimer disease risk loci and reveals interactions with APOE genotypes. Archives of Neurology. 67(12): 1473-1484
- Kim, M., Suh, J., Romano, D., Truong, M.H., Mullin, K. et al. (2009) Potential late-onset Alzheimer's disease-associated mutations in the ADAM10 gene attenuate ?-secretase activity. Human Molecular Genetics 18(20): 3987-3996.
- Kiraly, M.A., Kiraly, S.J. (2005) The effect of exercise on hippocampal integrity: review of recent research. Int J Psychiatry Med, 35: 75-89.
- Kivipelto, M., Ngandu, T, Fratiglioni, L., Viitanen, M., Kareholt, I., Winblad, B., Helkala, E.L., Tuomilehto, J., Soininen, H., Nissinen, A. (2005) Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol, 62: 1556-1560.
- Korf, E.S., Scheltens, P., Barkhof, F., de Leeuw, F.E. (2005) Blood Pressure, White Matter Lesions and Medial Temporal Lobe Atrophy: Closing the Gap between Vascular Pathology and Alzheimer's Disease? Dement Geriatr Cogn Disord, 20: 331-337.
- Kosik, K., Greenberg, S. (1994) Tau protein and Alzheimer's disease. In Alzheimer's Disease. Raven Press, New York. 335-344.
- Kudo, T., Iqbal, K., Ravid, R., Swaab, D.F., Grundke-Iqbal I. (1994) Alzheimer disease: correlation of cerebro-spinal fluid and brain ubiquitin levels. Brain Res 639: 1-7.
- Lindstrom, H.A., Fritsch, T., Petot, G., Smyth, K.A., Chen, C.H., Debanne, S.M., Lerner, A.J., Friedland, R.P. (2005) The relationships between television viewing in midlife and the development of Alzheimer's disease in a case-control study. Brain Cogn, 58: 157-165.
- Lott, I.T., Head, E. (2005) "Alzheimer disease and Down syndrome: factors in pathogenesis". Neurobiol Aging 26 (3): 383-89.
- Lye, T.C., Shores, EA. (2000) Traumatic brain injury as a risk factor for Alzheimer's disease: A review. Neuropsychology Review, 10: 115-129.
- Mahley, R.W. (1998) Apolipoprotein E: cholesterol transport protein with expanding role in cell biology. Science 240, 622-630
- Mahley, R.W., Huang, Y., Rall, S.C., Jr., (1999) Pathogenesis of type III hyperlipoproteinemia (dysbetalipoproteinemia): questions, quandaries, and paradoxes J. lipid Res. 40, 1933-1949
- Mahley, R.W., Rall, S.C., Jr., (2000) Apolipoprotein E: far more than a lipid transport protein. Annu. Rev. Genomics Hum. Genet. 1, 507-537
- Mayeux, R., (1984) Behavioral manifestations of movement disorders:Parkinson's and Huntington's disease. Neurol Clin, 2: 527-540
- Miyasaki JM, Shannon K, Voon V, Ravina B, Kleiner-Fisman G, Anderson K, et al. 2006 Practice parameter: evaluation and treatment of depression, psychosis, and dementia in Parkinson disease Neurology, 66: 996-1002.
- Mocchegiani, E., Bertoni-Freddari, C., Marcellini, F., Malavolta, M. (2005) Brain, aging and neurodegeneration: role of zinc ion availability. Prog Neurobiol, 75: 367-390
- Nathan, B.P., Bellosta, S., Sanan, D.A., Weisgraber, K.H., Mahley, R.W., Pitas, R.E. (1994) Differential effects of apolipoproteins E3 and E4 on neuronal growth in vitro. Science 264, 850-852
- Newman, A.B., Fitzpatrick, A.L., Lopez, O., Jackson, S., Lyketsos, C., Jagust, W., Ives, D., Dekosky, S.T., Kuller, L.H. (2005) Dementia and Alzheimer's disease incidence in relationship to cardiovascular disease. J Am Geriatr Soc, 53: 1101-1107
- Nishimura, M., Yu, G. and St George-Hyslop, P.H. (1999) Biology of presenilins as causative molecules for Alzheimer disease. Clin. Genet., 55, 219-225
- Nistor, M., Don, M., Parekh, M. et al. (2007) Alpha-and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain. Neurobiol Aging 28 (10): 1493-1506
- Plassman, B.L., Langa, K.M., Fisher, G.G., Heeringa, S.G., Weir, D.R. et al. (2007) Prevalence of dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology, 29 (1-2): 125-132.
- Ravaglia, G., Forti, P., Maioli, F., Martelli, M., Servadei, L., Brunetti, N., Porcellini, E., Licastro, F. (2005) Homocysteine and folate as risk factors for dementia and Alzheimer disease. Am J Clin Nutr, 82: 636-643
- Reisberg, B., Doody, R., Stoffler, A. et al. (2003) Memantine in moderate-to-severe Alzheimer's disease. N Engl J Med. 348: 1333-1341.
- Roses, A.D. (1997) A model for susceptibility polymorphisms for complex diseases:apolipoprotein E and Alzheimer's disease. Neurogenetics, 1, 1-3.
- Royall, D., Cordes, J., Polk, M. (1998) "CLOX: an executive clock drawing task". J Neurol Neurosurg Psychiatry 64 (5): 588-594.
- Sano, M., Ernesto, C., Thomas, R.G., Klauber, M.R., Schafer, K., Grundman, M., Woodbury, P., Growdon, J., Cotman, C.W., Pfeiffer, E., Schneider, L.S., Thal, L.J. (1997) A controlled trial of selegiline, alphatocopherol, or both as treatment for Alzheimer's disease. N Engl J Med 336: 1216-1222.
- Schellenberg, G.D. (1995) Genetic dissection of Alzheimer disease, a heterogeneous disorder. Proc. Natl Acad. Sci. USA 92, 8552-8559
- Scott, A., Small, Duff, K. (2008) Linking A? and Tau in Late-Onset Alzheimer's Disease: A Dual Pathway Hypothesis. Neuron 60, Elsevier Inc
- Selkoe, D.J. (1994) Cell biology of the amyloid beta-protein precursor and the mechanism of Alzheimer's disease. Annu Rev Cell Biol 10: 373-403,
- Seshadri, S., Wolf, P.A., Beiser, A., Au, R., McNulty, K. et al. (1997) Lifetime risk of dementia and Alzheimer's disease. The impact of mortality on risk estimates in the Framingham Study. Neurology 49(6): 1498-1504
- Shellenberg, G.D., Bird, T.D., Wijsman, E.M. et al: (1992) Genetic linkage evidence for a familial Alzheimer's disease locus on chromosome 14. Science; 258: 668-671
- Sjogren, M., Blennow, K. (2005) The link between cholesterol and Alzheimer's disease. World J Biol Psychiatry; 6: 85-97.
- Sohal, R.S., Weindruch, R. (1996) Oxidative stress, caloric restriction, and aging. Science, 273: 59-63
- Srinivasan, V., Pandi-Perumal, S.R., Maestroni, G.J., Esquifino, A.I., Hardeland, R., Cardinali, D.P. (2005) Role of melatonin in neurodegenerative diseases. Neurotox Res, 7: 293-318.
- Streit, W.J. (2005) Microglia and neuroprotection: implications for Alzheimer's disease. Brain Res Brain Res Rev, 48: 234-239.
- Strittmatter, W.J., Weisgraber, K.H., Goedert, M. et al. (1994) Hypothesis: microtubule instability and paired helical filaments formation in the Alzheimers disease brain are related to apolipoprotein E genotype. Exp Neurol, 125: 163-171.
- Teng, E.L., Chui, H.C. (1987) "The Modified Mini-Mental State (3MS) examination". The Journal of Clinical Psychiatry 48 (8): 314-318.
- Teng, E.L., Hasegawa, K., Homma, A. et al. (1994) The Cognitive Abilities Screening Instrument (CASI): a practical test for cross-cultural epidemiological studies of dementia. International Psychogeriatrics/IPA 6 (1): 45-58.
- Tesseur, I., Van Dorpe, J., Bruynseels, K. Bronfman, F. Sciot, R., Van Lommel, A., Van Leuven. F. (2000) The Role of ApoE in Alzheimer's Disease: An Alternative View Am. J. Pathol. 157, 1495-1510
- Tesseur, I., Van Dorpe, J., Spittaels, K., Van den Haute, C., Moechars, D. Van Leuven, F. (2000) Expression of human apolipoprotein E4 in neurons causes hyperphosphorylation of protein tau in the brains of transgenic mice. Am. J. Pathol. 156, 951-964
- Thomas, P., Fenech, M. (2007) A review of genome mutation and Alzheimer's disease. Mutagenesis 22(1). 15-33.
- Tiraboschi, P., Hansen, L.A., Thal, L.J., Corey-Bloom J. (2004) The importance of neuritic plaques and tangles to the development and evolution of AD. Neurology 62 (11): 1984-1989
- Treiber, C. (2005) Metals on the brain. Sci Aging Knowledge Environ 36 pe27
- Vanneste, J., Augustijn, P., Dirven, C., Tan, W.F., Goedhart, Z.D. (1992) Shunting normal-pressure hydrocephalus: do the benefits outweigh the risks? Neurology, 42(1): 54-59
- Viswanathan, A., Rocca, W.A., Tzourio, C. (2009) Vascular risk factors and dementia: How to move forward? Neurology 72: 368-374
- Vitaliano, P.P., Zhang, J., Scanlan, J.M. (2003) Is caregiving hazardous to one's physical health? A meta-analysis. Psychological Bulletin 129(6): 946-972.
- Wang, G.P., Khatoon, S., Iqbal, K., Grundke-Iqbal I. (1991) Brain ubiquitin is markedly elevated in Alzheimer disease. Brain 566: 146-151.
- Went, L.N., Vester-Van der Vlis, M., Volkers, W. et al: (1975) Early Diagnosis and Prevention of Genetic Diseases. The Netherlands: Leiden University Press; 13-25.
- Wexler, N.S. (1979) Perceptual-motor, cognitive, and emotional characteristics of persons at risk for Huntington's disease. Adv Neurol, 23: 257-271.
- Xu,W., Qiu, C., Gatz, M., Pedersen, N. L., Johansson, B., Fratiglioni, L. (2009) Mid-and Late-Life Diabetes in Relation to the Risk of Dementia Diabetes 58, 71-77
- Yankner, B.A., Mesulam, M.M. (1991) Seminars in medicine of the Beth Israel Hospital, Boston. beta-Amyloid and the pathogenesis of Alzheimer's disease. N Engl J Med 325: 1849-1857


