Assessment of menstrual hygiene knowledge, attitudes and practice among medical students
Автор: Turusbekova A., Kudaiarova K., Manas S., Aastha
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 8 т.11, 2025 года.
Бесплатный доступ
Menstrual hygiene is an essential aspect of reproductive health, yet it remains a significant public health concern due to inadequate awareness, limited access to sanitary facilities, and persistent cultural taboos. Medical students, despite their educational background, also face challenges in managing menstrual hygiene effectively. Research objectives: this study aims to assess menstrual hygiene awareness, practices, and associated challenges among female medical students at the International Medical Faculty, Osh State University. A cross-sectional, questionnaire-based survey was conducted among 328 female medical students from first to sixth year. The self-developed, pre-validated questionnaire included questions on menstrual hygiene awareness, practices, product preferences, challenges faced, and the influence of residence and institutional support. Data were analyzed using descriptive statistics, expressed as counts and percentages. Research results: the study found that while most students had a basic understanding of menstrual hygiene, significant gaps existed in awareness, affordability, and accessibility of sanitary products. A considerable proportion of students (42.7%) reported experiencing health issues due to inadequate menstrual hygiene. Hostel residents faced more challenges related to sanitation and pad disposal compared to those living in flats. Period stigma remained prevalent, with 15.2% of students reporting experiences of period shaming. Despite being in a medical environment, only 34.8% of students reported receiving menstrual hygiene awareness from their institution. The study highlights the need for improved menstrual hygiene education, better sanitation facilities, and increased accessibility to affordable menstrual products. Institutional initiatives, such as awareness programs, infrastructure improvements, and policy changes, are crucial in addressing menstrual hygiene challenges and promoting a stigma-free environment.
Menstrual hygiene, menstrual practices, medical students, menstrual health awareness, sanitary products, period stigma, menstrual education, public health
Короткий адрес: https://sciup.org/14133523
IDR: 14133523 | УДК: 618.175 | DOI: 10.33619/2414-2948/117/37
Текст научной статьи Assessment of menstrual hygiene knowledge, attitudes and practice among medical students
Бюллетень науки и практики / Bulletin of Science and Practice
UDC 618.175
Adolescence is a critical phase of life, marked by rapid physical, emotional, and psychological changes. According to the World Health Organization (WHO), adolescents are individuals aged between 10 and 19 years. One of the most significant milestones in female puberty is menarche, the first menstrual cycle, which signifies reproductive maturity and the transition from childhood to adolescence. Another key developmental event is menarche, the onset of secondary breast development, which often occurs as an early sign of puberty in girls.
Menstruation is a natural biological process experienced by adolescent girls and premenopausal women. It plays a crucial role in reproductive health and parenthood, making it a topic of significance for both women and men. The age of menarche varies globally based on geographical, genetic, and socioeconomic factors, typically occurring between 8 and 16 years in low-income settings, with a median age of around 13 [1, 2].
Menopause, on the other hand, generally occurs around 50 years of age [3].
Based on these estimates, a woman in a low-income country is expected to menstruate for approximately 1,400 days over her lifetime. Despite being a routine part of life, menstrual hygiene management (MHM) remains a significant challenge in many low-resource settings. Women and girls rely on different methods to manage menstruation, shaped by personal preferences, cultural beliefs, economic status, and access to sanitary products. However, in many parts of Africa, South Asia, and the Middle East, inadequate MHM is common due to financial constraints, lack of awareness, and limited access to proper sanitary materials. Studies indicate that in some regions, disposable sanitary pad usage is alarmingly low. For example, only 18% of Tanzanian women regularly use sanitary pads, while in Nigeria, 31% to 56% of schoolgirls rely on alternatives like cloth or toilet paper [4-6].
In India, between 43% and 88% of girls wash and reuse cloth, often without adequate cleaning or drying in sunlight due to cultural taboos. Such practices increase the risk of infections linked to poor menstrual hygiene [7-9].
Reproductive tract infections (RTIs) remain a major public health concern in low-income settings, and poor menstrual hygiene may contribute to this burden. While sexually transmitted infections (STIs) and other endogenous infections are well-documented, the specific role of inadequate MHM in causing infections is not fully understood [10, 11].
However, conditions such as bacterial vaginosis (BV) and vulvovaginal candidiasis (VVC) are believed to be linked to poor menstrual hygiene. BV has been associated with an increased risk of HIV, human papillomavirus (HPV) infection, and adverse pregnancy outcomes. Both BV and VVC present with symptoms like vaginal discharge and irritation, although many infections remain asymptomatic, making diagnosis and treatment more challenging [12-16].
Beyond health concerns, menstruation carries deep social and cultural implications, often shaping a girl’s experience and status within her community. In certain cultures, menarche marks the transition to adulthood and marriageability, sometimes accompanied by restrictive customs. Due to menstruation-related stigma, many girls lack proper education on the subject and may experience fear or anxiety when their first period arrives. For example, in South India, a significant proportion of girls report feeling shocked or scared at menarche, with some undergoing seclusion rituals lasting up to two weeks. Cultural taboos may also lead to restrictions on daily activities, preventing menstruating women from cooking, touching water, attending religious ceremonies, or even sleeping in their usual place [17-23].
A major consequence of inadequate MHM is its impact on girls’ education. Many schoolgirls face barriers such as a lack of private, functional toilets, insufficient access to water and soap, and inadequate disposal facilities for used menstrual products. Additionally, menstrual pain, embarrassment, and fear of leakage or staining contribute to absenteeism and school dropout rates. Reports from international organizations such as Water Aid and Plan International suggest that improving MHM can lead to better school attendance and educational outcomes. Studies have shown that prolonged education for girls is linked to broader societal benefits, including lower maternal mortality rates, improved child health, higher contraceptive use, reduced fertility rates, and lower HIV infection rates [24, 25].
Despite being a natural biological process, menstruation remains a topic surrounded by cultural taboos, misconceptions, and inadequate awareness. In many societies, these barriers prevent open discussions about menstrual health, leading to negative body image, anxiety, and poor menstrual hygiene practices. Unhygienic menstrual practices can result in serious health consequences, including reproductive tract infections, pelvic inflammatory disease, and even longterm complications like infertility.
Medical students, being future healthcare professionals, are expected to have adequate knowledge and awareness regarding menstrual health and hygiene. However, studies suggest that even among medical students, there are gaps in awareness and misconceptions related to
Бюллетень науки и практики / Bulletin of Science and Practice Т. 11. №8 2025 menstruation and menstrual hygiene. Understanding these aspects among female medical students is crucial for ensuring their well-being and enabling them to educate others effectively.
This study aims to assess the knowledge, attitudes, and practices regarding menstruation among female medical students from the 1st to 6th year at the International Medical Faculty, Osh State University. By identifying gaps in awareness and hygiene practices, this research can contribute to developing educational interventions and improving menstrual health management among future healthcare professionals.
Materials and methods
This is an anonymous, questionnaire-based survey. A self-developed, pre-validated questionnaire (Annexure 1) was used. Data is expressed as counts and percentages. A crosssectional observational study was conducted among 328 girls from all years (1st to 5th year) of the International Medical Faculty, Osh State University. A pre-formed, pre-tested questionnaire was used. Some questions had multiple options to choose from; therefore, the sum total of percentages is not always 100%. To assess the knowledge, attitudes, and practices regarding menstruation and menstrual hygiene among female medical students from the 1st to 6th year at the International Medical Faculty, Osh State University.
Results and discussion
This survey on menstrual hygiene awareness and practices was conducted among 328 female medical students from 1st to 6th year at the International Medical Faculty, Osh State University. The findings provide valuable insights into the knowledge, attitudes, and challenges faced by medical students regarding menstrual health.
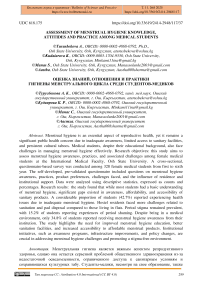
The majority of respondents were from the 2nd year (47.6%), with fewer participants from the higher years, especially the 6th year (3.7%) (Figure 1). The most common age group was 18-21 years (58.8%), while a smaller percentage were above 24 years (4.9%). When asked about their understanding of menstrual hygiene, most students associated it with changing sanitary products on time (69.3%), followed by washing undergarments (46.6%) and washing private areas (43.3%). However, some misconceptions persisted, as 32.3% believed resting was a component of menstrual hygiene. The study also explored the sources of menstrual hygiene education, revealing that 53.4% of students learned about it from their mothers, while 23.8% credited school education. A notable finding was that 8.8% of participants gained knowledge from their fathers, suggesting inclusion of parental role in menstrual health education (Figure 2).
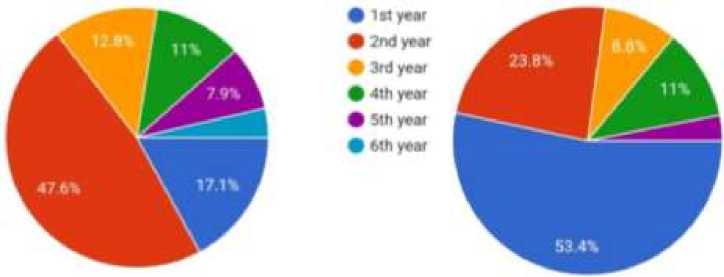
Figure 1. Survey results between respondents from the 2nd year
-
• From mother
-
• From school
-
• From fattier
9 From friends
-
• From magazine or social media
Figure 2. Survey results suggesting inclusion of parental role in menstrual health education
The age of menarche varied among students, with the most common age being 13 years (37.8%), while some reported menarche as early as 10 years (11%) or as late as 15 years (18.6%). Most students experienced a normal menstrual duration of 1-5 days (47%), though 13.7% reported prolonged bleeding lasting more than seven days.
Menstrual hygiene practices varied among participants. While 38% took showers twice daily during menstruation, 31.7% bathed only once, and 12% reported not bathing at all. Regarding their living arrangements, 66.5% resided in hostels, while 22.6% lived in flats. When asked if their place of residence influenced their menstrual hygiene, 35.4% believed it did, whereas 40.9% disagreed. When considering the most suitable residence for maintaining menstrual hygiene, 31.7% preferred flats, while 30.5% believed that all types of accommodation had their own challenges.
Students living in hostels reported several challenges related to menstrual hygiene. 47.9% cited cleanliness issues, while 45.6% found it difficult to change sanitary products on time due to shared living spaces. Additionally, 26.1% mentioned an inefficient water supply, and 18.2% struggled with the lack of dustbins for disposing of menstrual waste (Figure 3). Flat residents faced similar difficulties, with 33.9% reporting water shortages, 33.5% highlighting cleanliness issues, and 23.6% having trouble in changing pads due to shared living conditions (Figure 3).
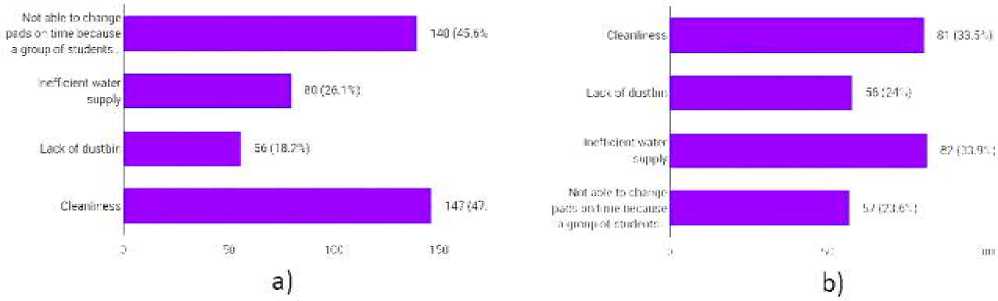
Figure 3. a) Results where 26.1% respondents mentioned an inefficient water supply, and 18.2% struggled with the lack of dustbins for disposing of menstrual waste; b) Flat residents faced similar difficulties in changing pads due to shared living conditions
Menstruation-related challenges extended beyond the home environment, as 63.3% of participants reported facing difficulties while outside their hostel or flat. The most common problems included abdominal cramps (51.8%), back pain (50%), and staining of clothes (44.5%). Additionally, 39.6% struggled to change sanitary products on time, and 39.9% found inadequate toilet facilities to be a significant challenge. Cultural and social factors played a role in shaping attitudes toward menstruation. When asked whether external influences affected their menstrual experience, 28% attributed it to age, while 21.3% cited religious beliefs, and 15.2% reported economic status as a contributing factor. Period shaming was experienced by 15.2% of students, with 6.4% stating they had always faced stigma related to menstruation (Figure 4).
Furthermore, 15.2% reported that someone had asserted menstruation to be shameful, though the majority (70.4%) did not experience such stigma. Regarding sanitary product preferences, 70.2% of students preferred commercial sanitary napkins, while 16.1% still relied on traditional methods. However, affordability remained a concern, as 26.5% found sanitary napkins expensive, and 21.6% could not always afford them (Figure 5). The majority of students changed their sanitary pads every 6-8 hours (42.4%), whereas 3.7% admitted to wearing the same pad for more than 10 hours, which poses potential health risks. When asked whether their college schedule allowed them to change napkins at appropriate intervals, only 39% found it favorable, while 35.4% disagreed, and 6.4% stated it was never possible.
Figure 4. Shaming period faced stigma related to menstruation
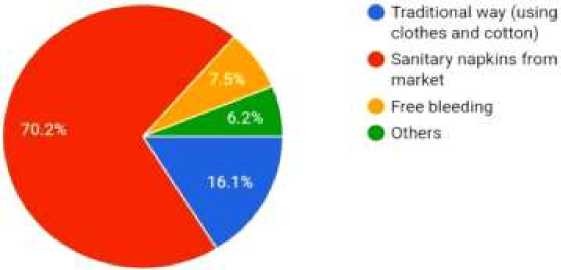
Figure 5. Sanitary product preferences
Health issues related to menstrual hygiene were frequently reported. 51.5% of students experienced itching due to napkins, 43.9% faced heavy bleeding, and 31.4% suffered from rashes or blister (Figure 6). Infections due to poor menstrual hygiene were reported by 42.7% of participants, though 47.1% had never experienced such issues. While menstrual cups are often promoted as an eco-friendly alternative, 56.7% of students rejected them, with 64.9% believing sanitary pads were the best choice. When asked if their college provided menstrual hygiene awareness programs, only 34.8% confirmed the presence of such initiatives, while 42.7% reported a lack of awareness programs.
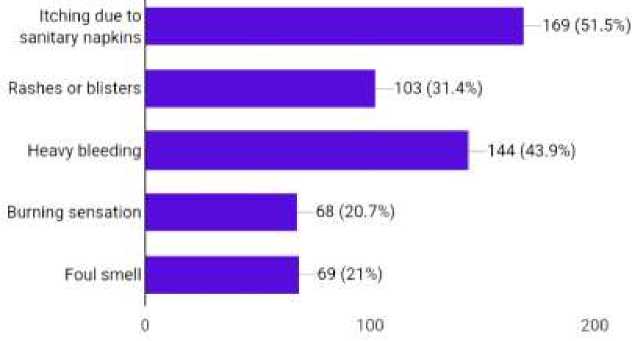
Figure 6. Health issues related to menstrual hygiene
Бюллетень науки и практики / Bulletin of Science and Practice Т. 11. №8 2025
This study highlights significant gaps in menstrual hygiene awareness and practices among female medical students. Although there is a fair understanding of basic menstrual hygiene, issues such as affordability of sanitary products, difficulties in maintaining hygiene in shared living spaces, and a lack of adequate facilities in educational institutions continue to pose challenges. Addressing these concerns through educational interventions, improved hygiene facilities, and greater access to affordable menstrual products is essential for ensuring the well-being of students and promoting menstrual health awareness.
Menstrual hygiene is a critical aspect of female reproductive health, yet it remains a topic surrounded by challenges, misconceptions, and socio-cultural restrictions. This study, conducted among 328 female medical students from the International Medical Faculty, Osh State University, provides an in-depth understanding of menstrual hygiene awareness, practices, and challenges among future healthcare professionals. Despite being medical students, the findings reveal gaps in knowledge, economic barriers, and infrastructural issues that influence menstrual hygiene management.
The mean age of menarche in this study aligns with global trends, with the majority of participants reporting the onset of menstruation at 13 years (37.8%). This is consistent with previous research indicating that menarche typically occurs between 11 and 14 years worldwide. However, a small proportion of students reported menarche as early as 10 years (11%), which could be influenced by genetic factors, nutritional status, and environmental conditions.
Despite having a medical background, misconceptions about menstrual hygiene persist. Although most students correctly identified the importance of changing sanitary products on time (69.3%), a considerable number associated menstrual hygiene with unrelated factors such as «taking rest» (32.3%). This highlights the need for stronger awareness programs to ensure that even medical students receive a well-rounded understanding of menstrual health.
The study also explored the sources of menstrual hygiene education, with mothers (53.4%) playing the most significant role, followed by schools (23.8%). The fact that 8.8% of students learned from their fathers suggests a positive shift in parental involvement in menstrual education, a subject traditionally considered as «mother’s responsibility». However, reliance on informal sources such as friends (11%) and social media/magazines (3%) underscores the need for structured education programs within academic institutions.
A significant proportion of students reported menstrual hygiene challenges linked to their place of residence. Hostel residents (66.5%) faced issues such as cleanliness concerns (47.9%), lack of privacy for timely pad changes (45.6%), and insufficient water supply (26.1%). These findings are in line with global studies indicating that communal living spaces can hinder menstrual hygiene management due to limited access to private sanitation facilities and disposal options. Similarly, flat residents reported issues with cleanliness (33.5%) and water supply (33.9%), suggesting that menstrual hygiene challenges are not restricted to hostels alone but extend to private accommodations as well.
Menstrual hygiene difficulties were also reported in public and college settings, with 63.3% of students struggling to manage menstruation while outside their hostel or flat. The most common complaints were abdominal cramps (51.8%), back pain (50%), and staining of clothes (44.5%). Additionally, 39.9% of students cited inadequate toilet facilities as a barrier to maintaining hygiene, a concern echoed in global research emphasizing the need for gender-sensitive sanitation infrastructure in educational institutions.
Cultural stigma and period shaming continue to affect students’ perception of menstruation. 15.2% reported experiencing period-related shame, while 6.4% always felt stigmatized due to
Бюллетень науки и практики / Bulletin of Science and Practice Т. 11. №8 2025 cultural beliefs. Although the majority of students (70.4%) denied facing such discrimination, the presence of a minority who still experience stigma highlights the ongoing need for social reform.
Sanitary product affordability emerged as a significant concern. While 70.2% of students preferred commercial sanitary napkins, 26.5% found them expensive, and 21.6% stated that affordability was inconsistent. This indicates that even among medical students, economic barriers limit access to essential menstrual hygiene products. The time interval for changing sanitary pads also varied, with 42.4% adhering to the recommended 6-8-hour interval, but 3.7% reported wearing the same pad for more than 10 hours, which increases the risk of infections and other health complications.
Health issues related to menstrual hygiene were commonly reported. 51.5% of students experienced itching due to sanitary products, while 43.9% faced heavy bleeding, and 31.4% reported rashes or blisters. Furthermore, 42.7% of students had experienced infections due to poor menstrual hygiene, reinforcing the need for awareness about hygiene-related health risks. Despite increasing advocacy for menstrual cups as a sustainable alternative, 56.7% of students rejected their use, with 64.9% preferring sanitary pads. The hesitancy to adopt menstrual cups could be attributed to a lack of awareness, misconceptions, and discomfort with insertion techniques.
Perhaps most concerning is the lack of institutional support for menstrual hygiene awareness. While 34.8% of students confirmed that their college provided awareness programs, 42.7% stated that no such programs were available. Given that medical students will eventually guide public health initiatives, it is crucial to incorporate menstrual hygiene education into medical curricula, ensuring that future healthcare professionals have the knowledge to educate and empower others.
Conclusion
This study highlights the critical aspects of menstrual hygiene awareness, practices, and challenges among female medical students at the International Medical Faculty, Osh State University. Despite being in a medical environment, many students still face difficulties related to hygiene management, affordability, infrastructure, and cultural stigma. The findings reveal that while most students have a basic understanding of menstrual hygiene, gaps remain in proper hygiene practices, access to sanitary facilities, and the affordability of menstrual products.
A significant proportion of students reported facing difficulties in managing menstruation, particularly those residing in hostels, where inadequate water supply, lack of privacy, and improper disposal systems pose major concerns. Additionally, a substantial number of students have experienced period-related stigma, with some reporting instances of period shaming based on cultural beliefs. These findings indicate that menstrual hygiene is not just a personal health issue but also a broader public health and social concern.
The study also emphasizes the need for institutional support in menstrual hygiene awareness programs. Given that medical students will eventually serve as healthcare providers and educators, it is crucial to ensure they receive comprehensive education on menstrual health. Addressing issues such as affordability, stigma, and infrastructure improvements will not only benefit students but also contribute to shaping a more informed and supportive healthcare system for menstrual health.
To promote better menstrual hygiene management, educational institutions must prioritize menstrual health awareness, improve sanitation facilities, and advocate for cost-effective and sustainable menstrual products. By taking proactive steps, medical institutions can play a vital role in breaking menstrual taboos, improving hygiene practices, and fostering a supportive environment for all students.
To improve menstrual hygiene awareness and management among female medical students, several steps should be taken at both institutional and societal levels. Medical institutions should integrate menstrual health education into the academic curriculum to ensure that future healthcare professionals are well-informed about menstrual hygiene management. Additionally, improving sanitation facilities within hostels and college campuses is crucial. Access to clean and private toilets, an adequate water supply, and proper disposal systems for sanitary products can significantly enhance hygiene practices, particularly for students living in hostels.
Raising awareness and reducing stigma through regular workshops and open discussions can help normalize menstruation and eliminate cultural taboos. Encouraging conversations about menstrual health among students, parents, and faculty members will create a more supportive environment. Colleges should also consider providing subsidized or free sanitary products in hostels and campus health centers to make menstrual hygiene products more accessible and affordable. Moreover, promoting the use of sustainable menstrual products such as menstrual cups and cloth pads through education on their benefits can encourage environmentally friendly practices.
Adjustments to academic schedules should also be considered to ensure that students have sufficient break times to manage their menstrual hygiene needs, including changing sanitary products. Public and institutional infrastructure improvements, such as better toilet facilities in libraries, classrooms, and university hospitals, can further support students during menstruation. Encouraging further research on menstrual health issues can provide valuable insights for policy changes at the institutional and governmental levels, ultimately leading to long-term improvements in menstrual hygiene management. By implementing these measures, educational institutions can play a vital role in breaking societal taboos, promoting better hygiene practices, and ensuring a healthier and more comfortable learning environment for female students.