Clinical acute bulbar syndrome in a 6-month-old child with cortical brain dysplasia
Автор: Zhikhareva V., Yuldashev I., Sulaimanov Sh.
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 9 т.10, 2024 года.
Бесплатный доступ
The article presents a rare clinical case of Autoimmune brain stem encephalitis of unknown etiology in a 6-month-old girl. The manifestation of the disease began with a subacute growing bulbar syndrome, however, in the clinical picture noted hemiparesis, which was not typical for the brain stem lesions. In the series of examinations, we revealed a concomitant congenital pathology of the cerebral cortex, which was the cause of child hemiparesis. The clinical case shows the importance of differential diagnosis in limited conditions and medical alertness for the correct diagnosis and further treatment.
Congenital brain malformation, focal cortical dysplasia, autoimmune stem encephalitis, bulbar syndrome, myasthenia, guillain-barré syndrome
Короткий адрес: https://sciup.org/14130833
IDR: 14130833 | УДК: 616.831.31-008.6 | DOI: 10.33619/2414-2948/106/24
Текст научной статьи Clinical acute bulbar syndrome in a 6-month-old child with cortical brain dysplasia
Бюллетень науки и практики / Bulletin of Science and Practice
UDC 616.831.31-008.6
Autoimmune diseases of the nervous system can affect any part of the nervous system, including the brain and spinal cord (central nervous system, CNS), as well as peripheral nerves, neuromuscular junctions, and skeletal muscles (peripheral nervous system) [1]. Clinical manifestations of autoimmune encephalitis are very diverse and nonspecific [2]. The manifestation of the disease gives an ambiguous clinical picture, which can cause difficulties in making a diagnosis.
Bulbar syndrome (BS) is a peripheral paralysis that develops with bilateral damage to the nuclei or trunks of the glossopharyngeal (IX), vagus (X) and hypoglossal (XII) cranial nerves that innervate the muscles of the tongue, as well as the laryngeal-pharyngeal and respiratory muscles. Examination reveals atrophy and fibrillar twitching of the muscles of the tongue, larynx, and soft palate, and suppression of pharyngeal reflexes. Some symptoms of bulbar palsy (BP), depending on the nature of the pathomorphological substrate, may be expressed unevenly. So, the defeat of the XII pair of cranial nerve is characterized by weakness of the tongue and neck muscles lying below the hyoid bone, the IX pair only slightly weakens the muscles of the larynx, since their motor innervation is carried out mainly by the Vagus nerve. Damage to the X pair causes weakness of the vocal cords, up to aphonia, choking, pouring liquid food through the nose, and other dysphagic disorders.
BS can occur in a variety of neurological disorders such as stroke, myasthenia gravis, botulism, multiple sclerosis, and acute brain stem encephalitis. These clinical manifestations can also occur in Guillain-Barré syndrome (GBS) even in the absence of noticeable limb weakness in GBS [3].
The aim of this article to present a rare clinical case of autoimmune brain stem encephalitis in combination with a congenital brain defect in a 6-month-old child.
Materials and methods
Presented a clinical case of autoimmune brain stem encephalitis of unspecified etiology in a 6-month-old girl who admitted to the Bishkek National Center for Children and Health on the 3rd day from the onset of symptoms with complaints from the mother of the lack of swallowing when eating. The mother also noted that the day before the child sluggishly sucked the breast, and breast milk partially poured out of the mouth, and the next day the child began to experience periodic choking, which intensified during the day and led to a complete rejection of the breast. The patient underwent clinical-anamnestic and laboratory-instrumental methods of examination - ultrasound of the thyroid gland and internal organs, MRI of the brain, Proserin test for the purpose of differential diagnosis, as well as consultations of other specialists.
Results. Child A., 6 months old
From the anamnesis of the disease according to the parents:
-
- on September 18, 2022, against the background of complete well-being, the child's body temperature increased to 38.0 degrees. With an antipyretic purpose a non-steroidal antiinflammatory drug (Ibufen), was given, after which the condition improved somewhat;
-
- on September 25, 2022, the mother noticed that the baby was suckling sluggishly, and breast milk partially poured out of the mouth;
-
- the choking increased over the following days and led to complete rejection of the breast;
-
- on September 26, 2022, the parents went to a local private clinic, to an ENT doctor who recommended a throat spray.
-
- on September 27, 2022, due to the lack of effect the baby brought to National Center for Motherhood and Childhood Welfare (NCM&ChW), Bishkek.
Anamnesis vitae. Child born from III pregnancy, III birth. Previous pregnancies have been uneventful. This pregnancy registered from the 1st week of gestation. In the first trimester of pregnancy, mother received the 1-rst vaccine against COVID-19. In the last trimester, stable arterial hypertension (BP 140/100-150/100 mmHg) recorded. Mother observed on an outpatient basis. Childbirth at 36 weeks' gestation, by planned Caesarean section. The child screamed immediately, attached to the breast for 30 minutes. Jaundice appeared on the 3rd day and lasted one week. Early development: the child began to hold his head at 2 months, roll over from his abdomen to back and vice versa at 4.5 months, start to sit at 6 months. Preventive vaccinations carried out according to the vaccination calendar of the Kyrgyz Republic. Allergy anamnesis: population "A". The epidemiological environment stated as “clean”. Heredity — not burdened.
Neurological status at admission: clear consciousness. Reacts to examination with concern. The head is of a normal shape, the percussion sound is not changed. Large fontanel — 0.5 x 0.5 cm, at the level of the bones of the skull. The palpebral fissures are the same, D=S, the pupils are rounded, D=S. Pupillary reaction to light is alive, D=S. The gaze fixes and traces for a short time, D=S. The face is symmetrical, D=S. Cough, pharyngeal reflexes are absent. Feeding through a nasogastric tube. Dysphonia when crying (hoarseness). Muscle tone increased moderately spastic type, D>S. Tendon reflexes are moderately brisk, D>S. Limitation of movements in the hip joint on the right. Pathological Babinski's foot reflex on the right. Meningeal symptoms are negative. Seizures not noted.
The Investigation results:
-
- general blood test — anemia of moderate severity (Hb - 94g/l, erythrocytes 3.50 x 10^12/l, Color test - 0.81), iron level 4.8 mmol/l (reduced).
-
- Antibodies to SARS COV-2 coronavirus (COVID-19) IgG positive.
-
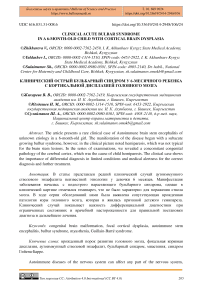
- X-ray taken to rule out injury to the cervical spine. According to radiographs of the cervical and thoracic spine in two projections: the bone structures of the vertebral bodies are within the age norm. No offsets or blocks (Figure 1, 2).
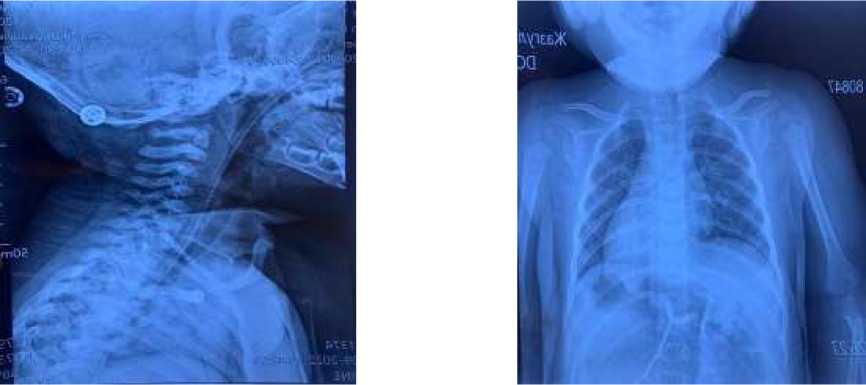
Figure 1, 2. X-ray of the cervical and thoracic spine in two projections: bone structures of the vertebral bodies within the age norm
-
- Ultrasound investigation of the brain dated 27.09.2022 — dilatation of the external cerebrospinal fluid pathways.
-
- Ultrasound investigation of the internal organs and the thyroid gland from 09/27/22 — without structural changes.
-
- MRI of the brain — data for moderately severe external hydrocephalus; hyperplasia of the rethrocerebellar cistern. Signs of focal cortical dysplasia (FCD) in the fronto-parietal regions, predominantly on the left (Figure 3).
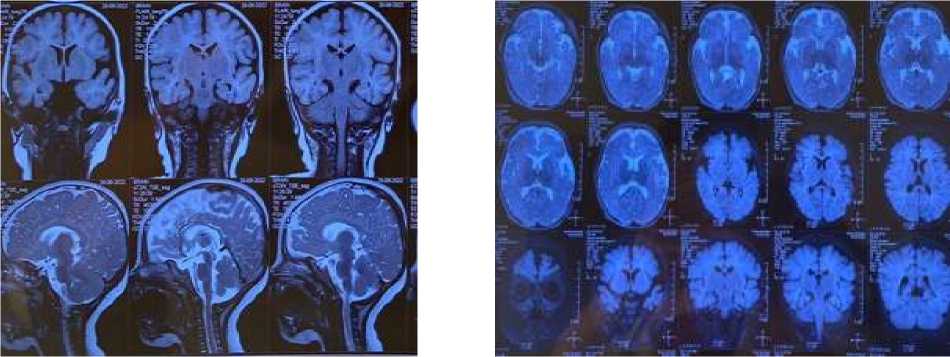
Figure 3. MRI of the brain - data for moderately severe external hydrocephalus; hyperplasia of the retrocerebellar cistern. Signs of focal cortical dysplasia in the fronto-parietal regions, predominantly on the left.
-
- Electroneuromyogram with stimulation of the digastric, deltoid, and biceps muscles - the test is negative.
-
- 03.09.2022: To exclude the local form of myasthenia gravis was performed a proserine test at the rate of 0.018 ml/kg (see Table).
-
- Consultation of narrow specialists: orthopedist, hematologist, surgeon, dentist did not reveal any specific pathology.
As follows from the table, the result of the Prozerin test gave a slightly positive effect, which indicates the exclusion of the alleged myasthenia gravis.
Table
PROSERINE TEST RESULTS
|
Time |
Blood pressure, mmHg |
Heart rate, str/min |
Saturation, % |
Pharyngeal reflex |
|
10:55 before test |
115/79 |
149 |
99 |
abc |
|
11:07 |
115/79 |
151 |
99 |
slightly positive, D>S |
|
11:14 |
116/75 |
143 |
99 |
slightly positive, D>S |
|
11:25 |
111/74 |
143 |
99 |
positive, D>S |
The child diagnosed:
Primary: Acute autoimmune encephalitis of unknown etiology.
Complication: Acute bulbar syndrome.
Concomitant: Congenital Malformation of the Central Nervous System. Focal cortical dysplasia in the frontal-temporal-parietal regions of the brain bilaterally. Right-sided pyramidal insufficiency.
The child was selected etiotropic and pathogenetic therapy:
-
1. Infusion therapy for the purpose of detoxification in the dehydration mode with the restriction of the injected fluid to 75% of the physiological need.
-
2. For anti-inflammatory purposes, hormonal therapy was used with the corticosteroid drug Dexamethasone 0.4% at a dose of 1 mg/kg intravenously every 6 hours for 3 days, then from the 3rd day at a dose of 0.6 mg/kg/day for 2 -x days
-
3. for an etiotrophic purpose, Acyclovir at a dose of 30 mg / kg for 5 days.
-
4. for immune-corrective purposes: normal human immunoglobulin at a dose of 0.3 g/kg for 6 hours No. 3 days
Three days after the start of therapy, the child's condition improved markedly: the girl began to swallow on her own, cough and pharyngeal reflexes appeared, and phonation improved when crying.
The child transferred from the intensive care unit to the general ward on the 5th day from admission, where he received a course of rehabilitation therapy and discharged home in a relatively satisfactory condition under the supervision of a group of family doctors at the place of residence.
Discussion
When conducting a differential diagnosis, it is important to be aware of a possible autoimmune process. The criteria for autoimmune encephalitis differ from those for encephalitis of any other etiology and include the following:
-
1. Subacute onset of clinical manifestations (up to 3 months).
-
2. Short-term memory loss, mental status change, or mental symptoms (in older children).
-
3. One of the following indicators: new focal cns data; seizures not explained by a previously known seizure disorder; pleocytosis of cerebrospinal fluid (leukocyte count more than 5 cells per mm3); features of MRI (However, it is worth noting that most patients with encephalitis undergo MRI of the brain on the first day of the disease, and therefore the results of neuroimaging may be normal). but sometimes they can indicate an autoimmune cause;
-
4. Exclusion of alternative causes [4].
A differential diagnosis made between the following diseases:
-
1. Myasthenia gravis - the result of a pharmacological Prozerin test was weakly positive, electroneuromyogram (ENMG) with stimulation of the digastric, deltoid, and biceps muscles without pathological changes, the clinical picture and age criteria were not characteristic of this diagnosis,
-
2. Volumetric formation in the oropharynx or pons Varolii — mass effect was excluded based on the following criteria: alkaline phosphatase and alpha-fetoprotein were slightly elevated, as a normal variant, MRI picture of the brain does not correspond to volumetric processes, specific pathology was excluded by oncologists.
-
3. Acute inflammatory demyelinating pathology of Guienne-Barre - for differential diagnosis of pharyngo-cervico-brachial forms, an electroneuromyogram performed with stimulation of the digastric, deltoid, and biceps muscles — the test did not reveal pathological changes, feces for dangerous infectious material — without features.
-
4. Acute cerebrovascular accident (no specific changes on MRI of the brain)
-
5. Encephalitis of bacterial and other etiologies (clinical and laboratory data do not meet the criteria for bacterial encephalitis), and so on.
However, when conducting a clinical and anamnestic analysis, the child was diagnosed with hemiparesis on the right (increased tone of the right arm and leg, revitalization of tendon reflexes, a pathological Babinsky foot reflex is positive on the right). Mother confirmed, indicating that the restriction in the movements of the right limbs observed almost since birth. As follows from the MRI data, the patient has a congenital malformation of the brain — Focal Cortical Dysplasia (FCD) in the fronto-temporal-parietal regions bilaterally. Characteristic features are the following:
thickening of the cortex, blurring of the border of white matter and gray matter with abnormal architecture of the subcortical layer, altered signal from white matter either with or without penetration through the cortex (transmantal sign), altered signal from gray matter, abnormal furrow or tortuous pattern and segmental and/or lobar hypoplasia/atrophy [5].
We assume an anomaly of the neural tube anlage in the period of 5-6 weeks of intrauterine development, which, as many authors believe, can subsequently lead to epileptic seizures, motor and cognitive impairments [6].
The etiology of Focal Cortical Dysplasia (FCD) is not well understood, it is believed that the causes are: a violation of the cellular structure of the cerebral cortex, perinatal and early postnatal injuries during fetal development, and the viral etiology of the disease is not excluded [7].
Taking into account the above clinical and laboratory manifestations and the differential diagnosis, the child diagnosed:
Primary: Acute autoimmune encephalitis of unknown etiology.
Complication: Acute bulbar syndrome.
Concomitant: Congenital Malformation of the Central Nervous System. Focal cortical dysplasia in the frontal-temporal-parietal regions of the brain bilaterally. Right-sided pyramidal insufficiency.
Conclusions
We described this case due to the fact that there are often certain difficulties in the timely diagnosis and, in our opinion, this is due to the peculiarities of autoimmune stem encephalitis in general, and in our case, specifically, the presence of an isolated clinical manifestation with bulbar disorders in the absence generalization of the degenerative process. By presenting clinical case, we would like to draw attention to the fact that, based solely on clinical and anamnestic data and standard diagnostic tests (such as X-ray, ENMG, MRI of the brain, Proserine test, test for specific onco-markers in the blood, etc.), it is possible in a timely manner make a diagnosis of autoimmune stem encephalitis and implement treatment in the early stages. Also in the clinical picture, in addition to the manifestations of stem encephalitis, right-sided pyramidal insufficiency noted, and MRI of the brain confirmed Congenital Malformation of the Central Nervous System. We would like to note the importance of differentiated diagnosis in limited conditions and medical alertness for the correct diagnosis and further treatment. The chosen etiotropic therapy, the first injections of which gave a positive result and allowed us to confidently dwell on the bulbar syndrome as a complication of autoimmune stem encephalitis.
Referencies:
Список литературы Clinical acute bulbar syndrome in a 6-month-old child with cortical brain dysplasia
- Bhagavati S. Autoimmune disorders of the nervous system: pathophysiology, clinical features, and therapy // Frontiers in neurology. 2021. V. 12. P. 664664. DOI: 10.3389/fneur.2021.664664 EDN: KMXUDH
- Arbizu J., Pérez-Larraya J. G., Hilario A., Grande A. G., Rubí S., Camacho V.Update on the diagnosis of encephalitis // Revista Española de Medicina Nuclear e Imagen Molecular (English Edition). 2022. V. 41. №4. P. 247-257. DOI: 10.1016/j.remnie.2022.05.003 EDN: EMOVSI
- Klimaj Z., Klein J. P., Szatmary G. Cranial Nerve Imaging and Pathology // Neurologic Clinics. 2020. V. 38. №1. P. 115-147. DOI: 10.1016/j.ncl.2019.08.005
- Leypoldt F., Armangue T., Dalmau J. Autoimmune encephalopathies // Annals of the New York Academy of Sciences. 2015. V. 1338. №1. P. 94-114. DOI: 10.1111/nyas.12553
- Kabat J., Król P. Focal cortical dysplasia-review // Polish journal of radiology. 2012. V. 77. №2. P. 35. https://doi.org/10.12659%2Fpjr.882968.
- Мухин К. Ю. Фокальные кортикальные дисплазии: клинико-электро-нейровизуализационные характеристики // Русский журнал детской неврологии. 2016. №2. С. 8-24. DOI: 10.17650/2073-8803-2016-11-2-8-24 EDN: WHUSXJ
- Najm I. M., Tassi L., Sarnat H. B., Holthausen H., Russo G. L. Epilepsies associated with focal cortical dysplasias (FCDs) // Acta neuropathologica. 2014. V. 128. P. 5-19. DOI: 10.1007/s00401-014-1304-0 EDN: VNWZDM