Comparative analysis of surgical plasty of bone defects in distal humerus fractures
Автор: Aleksey P. Davydov, Andrej G. Chibrikov, Aleksey B. Petrov, Vladimir Yu. Ulyanov
Журнал: Saratov Medical Journal @sarmj
Статья в выпуске: 2 Vol.6, 2025 года.
Бесплатный доступ
Objective: to conduct a comparative analysis of the plastic surgery outcomes of bone defects in various locations in distal humerus fractures using block and cancellous allografts. Materials and methods. The study included 56 patients with comminuted fractures of the distal humerus distributed among 3 groups depending on the bone defect location and 2 subgroups based on the bone grafting. Elbow joint function was assessed using the Broberg and Morrey rating system, pain syndrome was evaluated according to the visual analog scale. Results. The amplitude of flexion and extension movements of the elbow joint in medial area defects 1.5 months after plastic surgery with a block allograft reached 90±5º (p=0.04) and 75±6º when using cancellous allograft. Three months after surgical repair with a block allograft, the strength and pain scores for defects reached 80±2 pts in the central area, 82±3 pts in the lateral area and 88±4 pts in the medial column. For cancellous allograft, these scores were 59±5 pts (p=0.01), 62±3 pts (p=0.01) and 60±3 pts (p=0.03), respectively. Conclusion. The plasty of the bone defect with a block allograft for distal humerus fractures contributes to an increase in the multiplanar range of motion 1.5 months after surgery for a medial column defect, and also improves strength and increases range of the flexion and extension motion, and reduces pain 3 months after surgery for defects of the medial, lateral and central metaphyseal locations.
Fracture, humerus, comminuted fracture, surgical treatment, allograft, osteosynthesis
Короткий адрес: https://sciup.org/149148856
IDR: 149148856 | DOI: 10.15275/sarmj.2025.0205
Текст научной статьи Comparative analysis of surgical plasty of bone defects in distal humerus fractures
© This article is an open access publication. Russian Text. Published in Saratov Journal of Medical Scientific Research 2025; 21 (2): 149–155. ISSN 1995-0039.
Currently, despite the variety of employed surgical techniques, the treatment outcome of intra-articular fractures of distal humerus (DH) in 30% of cases is persistent disability. Frequent complications of the postoperative period are the formation of pseudoarthrosis and combined contractures of the elbow joint, occurring in 85% of cases. The comminuted nature of the fracture due to the high-energy mechanism of injury, the complex anatomical structure of the DH and the high reactivity of the elbow joint to external impact easily results in complications. To avoid a fracture nonunion, prolonged immobilization is performed. The process of a comminuted fracture fusion in the humerus requires long-term motion restriction, which contributes to the morphological transformation of the damaged articular hyaline cartilage into dense fibrous tissue and, consequently, to early progression of osteoarthritis and concomitant contracture of the elbow joint. A reduction in the amplitude of the flexion and extension movements in the elbow joint by more than 50% leads to a limitation of everyday routine household functions [1–4].
Early restoration of elbow joint movements is provided by the surgical treatment of DH fractures, the main types of which are open reduction and extramedullary fixation of fragments, closed reduction and transosseous osteosynthesis, as well as total elbow arthroplasty (TEA). Comminuted fractures of the elbow joint are often accompanied by a bone tissue defect in the metaphyseal area, which requires surgical correction. One of its options is corrective osteotomy and subsequent shortening of the bone, which can result in a deterioration in the patient’s quality of life. Another option is surgical plasty of the defect, which, in turn, limits the use of the transosseous osteosynthesis method. TEA (used in case of comminuted fractures of this localization accompanied by bone tissue defects of various etiologies) has up to 70% of unsatisfactory treatment outcomes and is recommended for use solely in elderly patients with a reduced activity. That is why in patients of working age in case of a fracture of the elbow joint with an accompanying bone defect, the method of choice is open reduction and extramedullary fixation of fragments with defect plasty [5–9].
The defect is replaced by autologous grafts (autografts) and allogeneic cadaveric grafts (allografts). An allograft does not have the disadvantages of an autograft, while rigid fixation of this graft type in an affected defect area, given the localization of the injury and the structure of the graft, is often problematic, thereby contributing to prolonged immobilization. The latter can lead to the emergence of postoperative contractures. The use of an allograft from bone
bank materials obtained from the femoral head and prepared via the 1993 Marburg Bonebank System has a number of advantages. They include the following: the native architecture of bone trabeculae, facilitating the physiological course of reparative processes; the presence of osteoconductive and osteoinductive properties of the material; and the possibility of inserting additional screws through the graft for its better fixation. The use of an allograft of various etiologies resolves multiple issues characteristic for an autograft (such as a shortage of donor zones, a limited volume of material, and the presence of undesirable effects for the patient at the site of autograft collection) [6, 10–15].
Objective: to compare surgical plasty outcomes of bone defects of various localizations in DH fractures using block vs. cancellous allografts.
Materials and methods
Our study involved 56 patients with closed DH fractures with a bone tissue defect (similar in age, location and size of the defect) but without comorbid pathology.
The inclusion criteria for the study were as follows: the period after injury (no more than 7 days); the presence of a closed isolated comminuted fracture of 13C2 and 13C3 types sensu the Association for Osteosynthesis/Orthopedic Trauma Association classification; the presence of a post-traumatic bone defect in the meta-epiphyseal area of the humerus; and no history of injuries and contractures of the elbow joint. The distribution of patients was based on the localization of the post-traumatic bone defect and the method of its plastic surgery ( Figures 1 and 2 ).
Depending on the choice of the method of bone defect plastic surgery (osteoplasty), we split each group into subgroups. In a subgroup a patients, osteoplasty was performed with a cadaveric cancellous allograft by impaction into the bone bed, while in a subgroup b, we used a block allograft obtained from the heads of resected femurs using the Marburg Bonebank System technique that involved the formation of a spike-shaped protrusion on the graft surface, insertion of locking screws through the bone plate, blocking a graft in intersecting planes, and the formation of bone canals connecting the allograft block with the bone marrow cavity ( Figure 2 ).
Comparison of the surgical treatment functional outcomes was performed using several criteria. Multiplanar range of motion in the elbow joint, including flexionextension and supination-pronation components (degree, о), was measured with a goniometer. The severity of pain syndrome was based on the subjective assessment of patients using the visual analogue scale. To assess the stability of the elbow joint, we performed valgus and varus stress tests and the elbow drawer test. The strength of the operated upper limb was estimated using a stationary tension meter. To calculate the total number of points, we employed an integral parameter that combined the above-listed aspects of the elbow joint function and converted them to a 100-point scale by M.A. Broberg and B.F. Morrey [16]. Examination was performed 1.5, 3 and 6 months after surgery: strength, pain syndrome and stability were assessed in comparison with the intact contralateral limb.
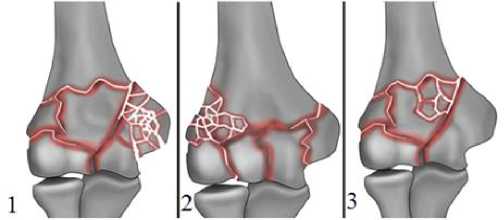
Figure 1. Distribution of patients among groups depending on the defect location: 1 – Group of patients with a medial defect (n=19); 2 – Group of patients with a lateral defect (n=19); 3 – Group of patients with a central metaphyseal defect (n=18)
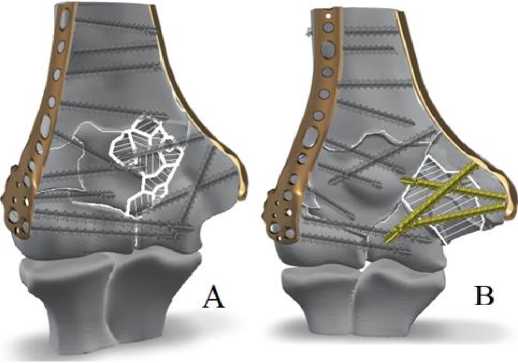
Figure 2. Methods of post-traumatic osteoplasty:
a – with a cadaveric cancellous allograft; b – with a native block allograft
Statistical processing of the obtained data was performed using the IBM SPSS Statistics v. 20 software. Due to noncompliance of the majority of collected data with the normal distribution law, we employed the nonparametric Mann-Whitney U test, the Wilcoxon test and the statistical significance (p) to compare the numerical values.
Results
In patients of subgroup 1a, 1.5 months after the surgery, the amplitude of flexion and extension movements in the elbow joint was 75±6º, i.e., 1.2 times less pronounced than in patients of subgroup 1b with 90±5º (p=0.04). Three months after the surgery, patients of subgroup 1a demonstrated an increase up to 79±9º, which was 1.3 times less pronounced than in patients of subgroup 1b with 100±5º (p=0.02). After 6 months, patients of subgroup 1a exhibited an increase up to 85±9º, which was 1.4 times less pronounced than the corresponding value in subgroup 1b with 114±4º (p=0.02). In patients of the Group 2, we found no reliable differences after 1.5 months and 3 months (p>0.05). However, after 6 months, patients in subgroup 2a had a flexion and extension range of motion of 82±8º, which was 1.3 times less pronounced than in subgroup 2b with 101±6º (p=0.01). In patients of Group 3, 1.5 months after the operation, no significant differences were noted (p>0.05). After 3 months, with an increase in median values in both groups, the values reached 72±60º in subgroup 3a and 88±5º in subgroup 3b (p=0.02). After 6 months after the surgery, the range of motion in subgroup 3a reached 82±8º, while in patients of subgroup 3b we observed the increase of this indicator up to 95±6º (p=0.01).
When assessing supination movements in the elbow joint 1.5 months after the operation, the result in patients of subgroup 1a was 36±4º, which was 1.2 times lower than in patients of subgroup 1b with 43±3º (p=0.02). Three months after the Surgery, an increase up to 32±2º and 52±4º in this indicator was noted in patients of subgroups 1a and 1b, correspondingly (i.e., we revealed 1.7-fold difference: p=0.01). Six months after the surgery, patients of subgroups 1a and 1b achieved a result of 36±4º and 60±2º, respectively, which implied 1.6-fold and 1.3-fold difference, correspondingly (p=0.01). In patients of Group 2, no differences were detected after 1.5 months (p>0.05). After 3 months, patients of subgroup 2a achieved a value of 40±4º, while patients of subgroup 2b achieved a value of 48±3º, with 1.2-fold difference (p=0.03). After 6 months, no statistically significant differences between the groups were found (p>0.05). In patients of Group 3, we observed no statistically significant difference at any checkpoints in the range of supination.
When assessing the pronation in Group 1 patients 1.5 months after surgery, no intergroup differences in the values were noted (p>0.05). Three months after surgery, patients of subgroup 1a demonstrated 40±4º, which was 1.2 times less pronounced than the values of patients in subgroup 1b with 47±3º (p=0.01). After 6 months, the range of pronation in patients of subgroup 1a increased to 45±6º, which was 1.3 times lower than in patients of subgroup 1b with 57±3º (p=0.01). In patients of Group 2, we noted no intergroup differences 1.5 months after the operation (p>0.05). Three months after the surgery, patients of subgroup 2a exhibited 42±3º, and patients of subgroup 2b showed a value 1.1 times higher: 47±2º (I=0.01). After 6 months, no intergroup difference in the values was revealed (p>0.05). Among patients of subgroups 3a and 3b, no statistically significant differences in the values were found at any checkpoints ( Figure 3 ).
When analyzing the total score on the Broberg and Morrey scale 1.5 months after the surgery, patients in subgroup 1a showed 63±5 pts, which was 1.1 times lower than in subgroup 1b with 71±2 pts (p=0.049). Three months after the operation, patients in subgroup 1a demonstrated 60±3 pts, which was 1.5 times lower than in subgroup 1b with 88±4 pts (p=0.03). After 6 months, patients in subgroup 1a demonstrated a score of 78±6 pts, while the score in subgroup 1b was 94±2 pts, demonstrating a 1.2-fold difference (p=0.02) ( Figure 4 ). In subgroup 2a, 1.5 months after the operation, a score of 54±5 pts was achieved, which was 1.1 times lower than in subgroup 2b with 62±3 pts (p=0.01). After 3 months, the score in the subgroup 2a was 62±3 pts vs. 82±3 pts in subgroup 2b (p=0.01), and after 6 months after the surgery, we observed no statistically significant differences (p>0.05) ( Figure 5 ).
In Group 3a, after 1.5 months, the score of 52±3 pts was achieved vs. 62±2 pts in group 3b, i.e., 1.1 times lower (p=0.01). Three months after surgery, in patients of group 3a, the score reached a value of 59±5 pts vs. 80±2 pts in the subgroup 3b (p=0.01), indicating a 1.35-fold difference in values . Six months after the operation, the score in subgroup 3a was 75±5 pts vs. 84±3 pts and in subgroup 3b, indicating a 1.1-fold difference between subgroups (p=0.00) ( Figure 5 ).
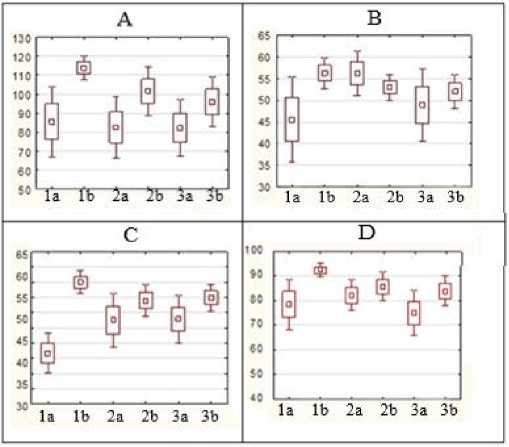
Figure 3. Diagrams depicting the range of values of elbow joint function assessment after 6 months: a – flexionextension range of motion in the elbow joint; b – range of pronation in the elbow joint; c – range of supination in the elbow joint; d – stability of the elbow joint
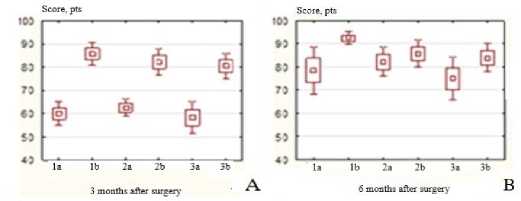
Figure 4. Diagrams depicting the range of the total score for the operated upper limb: a – 3 months after surgery; b – 6
months after surgery
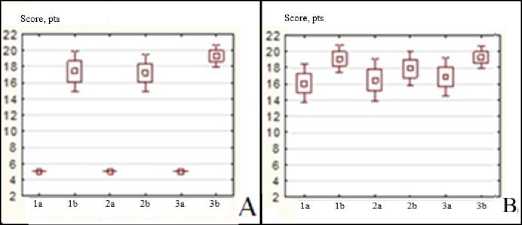
Figure 5. Diagrams of the range of strength for the operated upper limb: a – 3 months after surgery; b – 6 months after surgery
Discussion
Surgical treatment of patients with comminuted fractures of the DH, accompanied by posttraumatic bone defects, requires replacement of the defective area in addition to osteosynthesis with fixation of fragments [17]. An increase in the boundaries of the operating field, prolonged pain syndrome in the area of graft collection, and the risk of infectious complications limit the use of autograft [18]. The use of block allograft from resected femoral head, obtained according to the Marburg Bonebank System, not only removes the above limitations, but also creates the possibility of its additional fixation, thereby increasing the rigidity of the bone-graft-metal structure system. According to the plastic surgery method of posttraumatic periarticular defects of long tubular bones [10], it is possible to perform additional fixation of the graft via the formation of a groove in the affected defect area and a tenon-shaped protrusion on the top of the graft, and also by locking transplant screws in intersecting planes, thus achieving its additional fixation both in the defect area and directly to the metal structure. The formation of transosseous channels connected to the bone marrow cavity ensures an increase in the concentration of bioactive substances in the area of the defect – transplant – bone system, which contributes to the improvement of osseointegration processes [10, 13]. The rigidity of the bone – graft – metal structure system allows avoiding long-term immobilization. The pronounced difference in the magnitude of the pronation, supination, and flexion and extension movements in the elbow joint observed 1.5 months after the operation is a direct consequence of the absence of long-term immobilization of the elbow joint and a mechanically provided opportunity for an earlier start of rehabilitation measures in patients of subgroup a vs. patients of subgroup b, who underwent plastic surgery with a cadaveric cancellous allograft. Gradual leveling of differences in the values of the range of movements 3 and 6 months after the surgery is due to the onset of bone callus formation and marginal restructuring of the graft in the defect area (subgroup b). At the same time, after 6 months, the difference between groups remained, which can be explained by prolonged immobilization in patients of subgroup b and the formation of elbow joint contracture, which is consistent with the published data [12, 19, 20]. Comparing strength characteristics, elbow joint stability, and pain severity between groups via the calculation of the total number of points on the M.A. Broberg and B.F. Morrey scale, we observed a clear difference in quantitative indicators 3 months after surgery due to a reduction in pain syndrome, as well as early restoration of strength characteristics in the operated upper limb in patients of all subgroups a, along with a persistence of pain syndrome and low strength characteristics in patients of all subgroups b. The latter is a consequence of the difference in the immobilization timing and the onset of rehabilitation measures. Moreover, after 6 months, both groups demonstrated a reduction in the intergroup differences against the background of an increase in the total score due to a decrease in pain syndrome 6 months after surgery in patients of subgroups a and b, which corresponded to the mean duration of the reduction in pain syndrome described in the literature [7, 19].
For studying the functional outcomes of surgical treatment in patients with DH fractures with posttraumatic defects of bone tissue, the main role is played by the comprehensive assessment of the operated elbow joint functioning, provided by the M.A. Broberg and B.F. Morrey scale. Based on the latter, we demonstrated a favorable effect of plastic surgery of the posttraumatic defect with a block allograft in combination with open reduction osteosynthesis on the functional outcome due to the possibility of its additional fixation both in the area of the defective bone bed and to the metal structure directly by inserting screws through the graft. It is worth noting that in patients of all localizations of the posttraumatic defect, when performing plastic surgery with a block allograft, we observed an improvement in strength characteristics and a reduction in pain syndrome already 3 months after the surgery, with subsequent leveling off in intergroup values by 6 months. The latter, in our opinion, was due to the possibility of an earlier start of rehabilitation. In patients with defect localization in the area of the medial or lateral columns, an increase in the multiplanar range of motion was observed already 1.5-3 months after surgery. At the same time, the intergroup difference in the range of motion was not leveled off by 6 months after surgery, which was caused by the influence of the rehabilitation start date on the outcome. As a result, early development of movements in the operated elbow joint is critically important in terms of further restoration of the motion range. In Group 3 patients with central metaphyseal location of the post-traumatic defect, an increase in the range of flexion movements was noted 1.5 months after surgery, with this ratio maintained throughout the entire observation period. At the same time, no intergroup differences in pronation and supination movements were detected, which may be due to immense damage to the periarticular capsular ligamentous apparatus and further limitation of movements of this type of cicatricial etiology in both groups.
Conclusion
In DH fractures with a predominant localization of the bone defect in the areas of the lateral and medial columns, the use of open reduction osteosynthesis in combination with plastic surgery of the defects using a native block allograft with its additional fixation at the implantation site improves the range of multiplanar movements after 1.5-3 months, reduces pain syndrome, and increases joint stability 3 months after surgery. When the defect is localized in the central metaphyseal area in DH fractures, the use of a block graft helps increasing the range of motion performed in the elbow joint 1.5-3 months after surgery. At the same time, the use of the studied plastic surgery methods for DH fractures with a defect in the central metaphyseal area does not yield any differences in the range of rotation and pronation or improved stability in the elbow joint in the medium term and long term.
Author contributions. All authors contributed equally to the preparation of the manuscript.
Conflict of interest. The study was carried out within the framework of the initiative plan of scientific research at the Department of Traumatology and Orthopedics of V.I. Razumovsky State Medical University of Saratov, the Russian Federation Ministry of Healthcare, Outcomes of Using an Allograft as a Defect-Replacing Technology for Fractures of the Distal Humerus Metaepiphysis (state registration number: R&D 121111600047-2).


