Comparative evaluation of bone defect replacement methods in revision total knee arthroplasty
Автор: Mikhail V. Girkalo, Ivan N. Shchanitsyn, Vladimir V. Ostrovskiy, Maxim N. Kozadaev, Alexander V. Derevyanov
Журнал: Saratov Medical Journal @sarmj
Статья в выпуске: 1 Vol.4, 2023 года.
Бесплатный доступ
Objective: to evaluate the immediate and long-term outcomes of revision total knee arthroplasty using porous metaphyseal sleeves and cones. Materials and Methods. The study included 134 patients who underwent revision total knee arthroplasty. The patients were distributed among two groups based on the type of metaphyseal fixator: sleeves (Group I, n=97 patients) and cones (Group II, n=37 patients). Surgical outcomes were assessed upon discharge from the hospital (after the hospital stay of 7-12 days), as well as after 6, 12 and 24 months after surgery. The survival rate of endoprostheses was analyzed using the Kaplan–Meier method. A revision with total replacement of the endoprosthesis or its components was considered a critical event. Results. The analysis of the survival rate of endoprostheses in the form of various metaphyseal fixators showed that the groups of sleeves and cones did not differ statistically significantly as suggested by the logrank test (Mantel–Cox): p=0.108. Conclusion. The midterm follow-up revealed no difference in clinical, functional, or radiological outcomes of revision total knee arthroplasty performed for types 2A, 2B, and 3 of bone defect replacement (sensu Anderson Orthopaedic Research Institute classification) using trabecular metal metaphyseal cones vs. sleeves.
Revision arthroplasty, knee joint, bone defects
Короткий адрес: https://sciup.org/149146167
IDR: 149146167 | DOI: 10.15275/sarmj.2023.0104
Текст научной статьи Comparative evaluation of bone defect replacement methods in revision total knee arthroplasty
© This article is an open access publication. Russian Text. Published in Saratov Journal of Medical Scientific Research, 2023; 19 (1): 18–25. ISSN 1995-0039.
Cite as: Girkalo MV, Shchanitsyn IN, Ostrovskiy VV, Kozadaev MN, Derevyanov AV. Features of erythrocyte electrophoretic mobility in programmed hemodialysis patients. Saratov Medical Journal 2023; 4 (1): e0104.
Background
Total knee arthroplasty (TKA) is an orthopedic surgery in high demand. Consequently, the number of revision interventions is increasing and further growth is expected in the next decade [1]. It is predicted that up to 286 thousand TKAs will be performed annually in North America by 2030, which, compared with the current number of performed procedures, implies an increase of over 600% [2].
The clinical outcome of TKA and primary survival of endoprostheses are relatively successful and predictable [3]. However, repeated revision interventions after TKA account for approximately 10% of all knee arthroplasties [4]. The leading reasons for revision TKA are aseptic loosening of endoprosthesis components and periprosthetic joint infection, which are associated with the formation of bone defects of varying severity. Substantial bone defects resulting from aseptic loosening of the components of a compromised endoprosthesis can threaten the correct orientation and fixation of the revision prosthesis. The strategy for the latter was formulated in the concept of zonal fixation, described by R. Morgan-Jones et al. [5], according to which additional fixation in the metaphyseal zone is recommended in all cases of revision TKA for types 2 and 3 defects sensu the Anderson Orthopaedic Research Institute (AORI) classification. For this purpose, metaphyseal fixators have become widespread: sleeves and cones made of trabecular metal, which have a number of advantages over bone allografts: no risk of transmitting viral or bacterial infections, elimination of the likelihood of graft material resorption, shorter duration of surgery and, possibly, more durable primary fixation (Figure 1).
Metaphyseal sleeves and cones made of trabecular metal have similar indications for use but different implantation techniques and treatment outcomes, which determines the interest in comparing results of their use in revision TKA. As clinical data accumulated, it became possible to conduct a systemic analysis to resolve the problem of choosing the optimal metaphyseal fixator.
According to 2021 systematic literature review by R.P. Roach et al., which included 12 studies on the use of sleeves and 15 studies on the use of cones in revision TKA [6], the revision rate was almost twice as high when using cones vs. sleeves: 18.7% vs. 9.7%, respectively; albeit the variability of the selected studies and the likely multifactorial nature of unsuccessful outcomes did not allow any definitive conclusions to be drawn. This review solely highlighted the need for more research examining metaphyseal prostheses in revision TKA.

Figure 1. X-ray of the knee joint after revision arthroplasty: on the left, with metaphyseal sleeves; on the right, with metaphyseal cone
In 2022, P. Byttebier et al. published the largest systematic analysis and the only meta-analysis (77 articles, 4,391 knee joints) of the early and midterm clinical outcomes of the use of sleeves and cones, compared with the use of various bone grafting options and structural grafts [7]. When comparing all porous implants and grafts, no significant differences in prosthesis survival after 5-10 years were revealed. When comparing survival of cones and sleeves, the latter had a lower risk of revision (OR 1.72, 95% CI 0.88-2.57) vs. the cones (OR 3.04, 95% CI 1.71-4.37). The authors concluded that the volume and quality of publications on metaphyseal bone defects was progressively improving. Porous prostheses (sleeves and cones) are effective in metaphyseal bone defect replacement with a good survival rate at midterm follow-up. However, the lack of clear indications for choosing one or another method of metaphyseal fixation depending on the bone defect severity leaves the issue of the optimal metaphyseal prosthesis for revision TKA debatable [8].
Objective – to evaluate the immediate and long-term outcomes of revision total knee arthroplasty using metaphyseal sleeves and cones made of trabecular metal.
Materials and Methods
Our study was conducted at the Department No. 3 of Traumatology and Orthopedics of Scientific Research Institute of Traumatology, Orthopedics and Neurosurgery of Saratov State Medical University. In 2013 – 2015, 134 patients underwent revision TKA using semiconstrained revision endoprostheses with increased frontal stability. Metaphyseal sleeves and metaphyseal cones were employed in 97 and 37 cases, respectively. A retrospective cohort trial was performed on the basis of a prospectively completed database of patients after revision arthroplasty [9]. Figure 2 presents the study design.
Inclusion criteria for the study were as follows: revision TKA for periprosthetic joint infection or aseptic loosening of the tibial, femoral, or both components of the endoprosthesis; and the presence of types 2A, 2B and 3 defects in the femur or tibia sensu the AORI classification. Exclusion criteria were as follows: uncorrected severe concomitant pathology (cardiovascular and respiratory diseases and/or other conditions that prevent surgical intervention), as well as severe dementia or other mental and physical impairments that prevented the patient from completing the questionnaire independently.
The median age of the patients was 67 years, body mass index was 34 kg/m2. Study participants included 34 men (26%) and 100 women (74%). Indications for revision TKA were aseptic loosening of the endoprosthesis in 55 cases (41%) and periprosthetic joint infection in 79 cases (59%). The study sample (134 patients) comprised of two groups based on the type of metaphyseal fixator, a sleeve (97 patients) or a cone (37 patients) ( Table 1 ). Group I included patients with sleeves (e.g., manufactured by DePuy Synthes) to replace defects; Group II consisted of patients who underwent revision TKA using tantalum cones (e.g., manufactured by Zimmer Biomet) or a revision endoprosthesis (for example, by Stryker, with a Tritanium cone).
All patients underwent a standard preoperative clinical diagnostic examination, including physical examination, laboratory tests, radiography, CT, and MRI. Clinical examination was carried out using the Knee Society Scores (KSS) scale for assessing the function of the knee joint. Scores were calculated based on patient surveys. The KSS consists of two parts: clinical assessment and knee function assessment [10, 11]. X-rays were performed in a standing position; they encompassed the hip, knee and ankle joints. A number of studies were carried out in accordance with the KSTKARE scale (Knee Society Total Knee Arthroplasty Roentgenographic Evaluation) [ 12]: (a) disorders of the lower limb axes, (b) the location of the joint and patella line, (c) assessment of the endoprosthesis loosening with identification of osteolysis signs and determination of the position of endoprosthesis components. MRI and CT have higher sensitivity and specificity but are not recommended for routine practice due to high cost and elevated radiation exposure [13, 14]. In our practice, CT of the knee joint was performed according to indications to assess bone defects and spatial orientation of the endoprosthesis components. MRI of the knee joint was conducted if ligament damage was suspected.
Bone defects identified during surgery were assessed according to the AORI [15] and J. Insall [16] classifications. The type of defect was determined preoperatively using radiographs and during surgery after removal of all endoprosthesis components. Severe osteolysis of the tibia (T2B/T3) was observed in 81% of cases (108 out of 134). A pronounced defect in the femur (F2B/F3) was rarely detected (in 11%, or 15 cases out of 134). To assess the location and extent of the defect, we used the J. Insall classification [16], according to which bone defects are categorized into central (which do not extend onto the cortical plate) and peripheral (in which the cortical plate is damaged) lesions.
2023. Volume 4. Issue 1 (March). Article CID e0104
134 patients (2013-2019) Revision total knee arthroplasty A single-center retrospective cohort open-label trial
Inclusion criteria:
Exclusion criteria:
Revision TKA for periprosthetic joint infection and aseptic loosening of the tibial, femoral, or both endoprosthesis components.
Types 2A, 2B, or 3 defects of the femur and tibia.
Uncorrected severe concomitant pathology (cardiovascular, respiratory, and/or other conditions preventing surgical intervention).
Severe dementia or other mental and physical impairments that prevented the patient from completing the questionnaire independently.
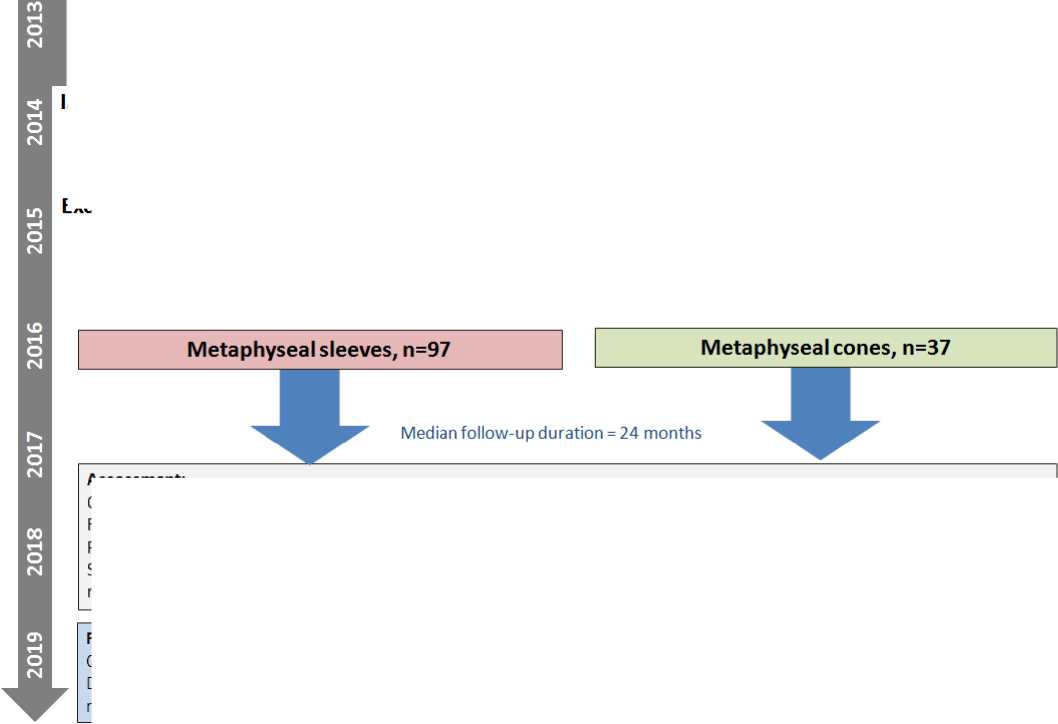
Results:
Comparison of the outcomes of using different metaphyseal fixation option (sleeves and cones)
Development of an algorithm for selecting a metaphyseal fixation option (sleeve or cone) based on the degree of bone resorption (sensu AORI scale), the limitation of the defect and the degree of primary intraoperative fixation
Figure 2. Design of the retrospective study
Assessment:
Clinical examination (KSS scale)
Radiography (bone defect classification according to the AORI scale), CT, MRT
Primary endpoints: revision arthroplasty
Secondary endpoints: revision (periprosthetic joint infection, aseptic loosening, contracture, hematoma, cumulative), bone resorption (KSTKARE scale scores), perioperative complications
Based on the results of assessing the bone defects, we identified the necessity to use a metaphyseal sleeve or cone. If it was impossible to obtain stable fixation of the sleeve, a decision was made to use a cone [17].
Metaphyseal femoral sleeves and metaphyseal tibial sleeves were used in 10% of patients (10 out of 97) and 100% of patients (97/97), correspondingly. Reconstructive cones (e.g., manufactured by Zimmer Biomet) and cones (e.g., manufactured by Stryker) were employed in 57% of cases (21 out of 37) and 43% of cases (16/37), respectively.
Postoperative management of patients was carried out according to a standard protocol. The length of hospitalization was recorded as well as adverse treatment outcomes – such as aseptic loosening, periprosthetic joint infection, bone fractures during treatment and implantation of metaphyseal fixators, hematoma, contracture, and patella baja (low-riding patella). The outcomes of the surgery were assessed in 7-12 days after the intervention and then after 6, 12, and 24 months.
The obtained data from clinical and radiological examination of all groups were subjected to statistical analyses. Statistical processing of the data was carried out using SPSS 21.0 (USA). The normality of the distribution of quantitative characteristics was assessed using the Kolmogorov–Smirnov and Shapiro–Wilk methods. Given the small sample size and non-normal distribution of most quantitative characteristics, nonparametric statistical methods were employed. To describe quantitative parameters, we used median and quartiles. Analysis of differences between different groups for quantitative characteristics was carried out using the Mann–Whitney U test. Friedman’s two-way analysis of variance by ranks was used in related groups.
For qualitative characteristics, Pearson’s χ² test was used. Logistic regression analysis was performed to identify risk factors for revision surgery. Variables included in the regression had p<0.5 on univariate analysis. A backward stepwise regression was used with an inclusion probability of 0.05 and an exclusion probability of 0.1 or greater. To identify the threshold of statistically significant values of quantitative characteristics, we constructed ROC curves with an assessment of the Youden’s index. The survival rate of the prosthesis was analyzed using the Kaplan–Meier method. A revision with total replacement of the endoprosthesis or its components was considered a critical event. A curve of the prosthesis survival function was constructed. Pairwise comparisons of survival in two different groups were performed using the logrank test (Mantel–Cox). Results were considered statistically significant at р <0.05, and two-tailed significance was assessed for all criteria.
Список литературы Comparative evaluation of bone defect replacement methods in revision total knee arthroplasty
- Belt M, Hannink G, Smolders J, et al. Reasons for revision are associated with rerevised total knee arthroplasties: An analysis of 8,978 index revisions in the Dutch Arthroplasty Register. Acta Orthop. 2021; 92 (5): 597-601. https://doi.org/10.1080/17453674.2021.1925036.
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007; 89 (4): 780-5. https://doi.org/10.2106/JBJS.F.00222.
- Khan M, Osman K, Green G, et al. The epidemiology of failure in total knee arthroplasty: Avoiding your next revision. Bone Joint J. 2016; 98-B (1 Suppl A): 105-12. https://doi.org/10.1302/0301-620X.98B1.36293.
- Yapp LZ, Walmsley PJ, Moran M, et al. The effect of hospital case volume on re-revision following revision total knee arthroplasty. Bone Joint J. 2021; 103-B (4): 602-9. https://doi.org/10.1302/0301-620X.103B4.BJJ-2020-1901.R1.
- Morgan-Jones R, Oussedik SI, Graichen H, et al. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015; 97-B (2): 147-9. https://doi.org/10.1302/0301-620X.97B2.34144.
- Roach RP, Clair AJ, Behery OA, et al. Aseptic loosening of porous metaphyseal sleeves and tantalum cones in revision total knee arthroplasty: A systematic review. J Knee Surg. 2021; 34 (10): 1033-41 https://doi.org/10.1055/s-0040-1701434.
- Byttebier P, Dhont T, Pintelon S, et al. Comparison of different strategies in revision arthroplasty of the knee with severe bone loss: A systematic review and meta-analysis of clinical outcomes. J Arthroplasty. 2022; 37 (6S): S371-S381.e4. https://doi.org/10.1016/j.arth.2022.02.103.
- Rodríguez-Merchán EC, Gómez-Cardero P, Encinas-Ullán CA. Management of bone loss in revision total knee arthroplasty: Therapeutic options and results. EFORT Open Rev. 2021; 6 (11): 1073-1086. https://doi.org/10.1302/2058-5241.6.210007.
- Girkalo MV. Database of intraoperative parameters that determine the choice of metaphyseal fixators for bone defect replacement in revision total knee arthroplasty. State R&D Registration No. RU 2021622939 of 14 December 2021. (In Russ.).
- Irzhanski AA, Kulyaba TA, Kornilov NN. Validation and cross-cultural adaptation of the WOMAC, KSS, and FJS-12 rating scales for knee disease, injury, and treatment outcome. Traumatology and Orthopedics in Russia. 2018; 24 (2): 70-9. (In Russ.). https://doi.org/10.21823/2311-2905-2018-24-2-70-79.
- Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248): 13-4.
- Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989; (248): 9-12. PMID: 2805502.
- Reish TG, Clarke HD, Scuderi GR, et al. Use of multi-detector computed tomography for the detection of periprosthetic osteolysis in total knee arthroplasty. J Knee Surg. 2006; 19 (4): 259-64. https://doi.org/10.1055/s-0030-1248116.
- Vessely MB, Frick MA, Oakes D, et al. Magnetic resonance imaging with metal suppression for evaluation of periprosthetic osteolysis after total knee arthroplasty. J Arthroplasty. 2006; 21 (6): 826-31. https://doi.org/10.1016/j.arth.2005.10.017.
- Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: Defect classification and alternatives for reconstruction. Instr Course Lect. 1999; (48): 167-75.
- Insall J. Revision of aseptic failed total knee arthroplasty. Surgery of the Knee. 2nd edition. N. Y.: Churchill, Livingstone, 1993; р. 935-57.
- Girkalo MV. A method for selecting a metaphyseal fixator for replacing extensive tibial bone defects in revision total knee arthroplasty. Invention Patent No. 2777929 of 11 August 2022. (In Russ.).
- Zagorodniy NV, Nuzhdin VI, Bukhtin KM, et al. Results of the use of bone grafting with allografts in revision hip arthroplasty. N.N. Priorov Bulletin of Traumatology and Orthopedics. 2014; (2): 33-9. (In Russ.).
- Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: A minimum 2-year follow-up. J Arthroplasty. 2009; 24 (7): 1086-92. https://doi.org/10.1016/j.arth.2008.08.011.
- Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008; 90 (1): 78-84. https://doi.org/10.2106/JBJS.F.01495


