Cryptogenic stroke in atrial fibrillation without intra-heart thrombi: possible mechanisms
Автор: Germanova O.A., Germanov A.V., Galati G., Prokhorenko I.O., Germanov V.A.
Журнал: Вестник медицинского института "РЕАВИЗ": реабилитация, врач и здоровье @vestnik-reaviz
Рубрика: Клиническая медицина
Статья в выпуске: 2 (56), 2022 года.
Бесплатный доступ
Background. Up to 45% of ischemic strokes are cryprogenic.Aim is to study which variant of permanent AF without intra-heart thrombi is the most unfavorable in appearing of stroke.Methods. We observed 202 patients with permanent AF without intra-heart thrombi and hemodynamically not significant carotid bifurcation atherosclerotic stenosis. We performed echocardiography, 24-hours monitoring of electrocardiography (ECG), ultrasound of brachiocephalic arteries, sphygmography of common carotid arteries, computer tomography of the brain, hemostasiograms, lipid profile, hemoglobin A1c. According to the 24-hours ECG monitoring data, we divided patients into two groups up to the maximum pauses between ventricular complexes in AF: patients with a pause
Cryptogenic stroke, atrial fibrillation, main arteries kinetics
Короткий адрес: https://sciup.org/143178583
IDR: 143178583 | УДК: 616-005.6
Текст научной статьи Cryptogenic stroke in atrial fibrillation without intra-heart thrombi: possible mechanisms
Nowadays stroke is still very common pathology all over the world, despite of preventive measures. So, in the USA up to 800 000 individuals have stroke each year, the majority of which (about 87 %) has ischemic pathogenesis and 23 % have recurrent stroke [1–3]. Moreover, in 240000 patients occur a transient ischemic attack (TIA) each year [4]. In the European Union (EU), stroke has the second position within the most common causes of death and the main cause of disability [5–11]. About 1,1 million inhabitants of the EU countries experience this pathology every year [12] which leads to 440000 deaths [13]. During the last decades because of preventive measures that help to reduce the predictors of stroke (for example, arterial hypertension (AH), smoking, alcohol consumption) partly slowed down the growth of cases, but not significantly [14–18]. The expected number is 1,5 million of stroke cases in 2025 in case if the 2000’s rates remained stable, and about 1,35 million in case if the rates will decline by 2 % every 5 years [19–22].
Within the structure of stroke, 88 % is the ischemic stroke (IS), 10 % – intracerebral hemorrhage and 2 % is subarachnoid hemorrhage.
In IS, 77 % of cases is non-lacunar stroke and 45 % is cryptogenic [1, 23–26]. So, despite of the diagnostic and preventive measures, in many cases of IS the reason of it remains unknown. The logical question appears – is there any unaccounted additional predictors of IS that we don’t pay attention?
Atherosclerotic hemodynamically significant lesions of carotid arteries can lead to stroke [25–27]. Surgical correction of carotid stenosis (operation of carotid endarterectomy, stenting) is currently recommended in 70 % stenosis and more [28–31]. Patients with non-significant carotid stenosis undergo medical treatment mostly oriented on prevention of the further atherosclerotic lesion growth (for example, statins). In the literature there are the publications that underline more frequent stroke in patients with non-signifi-cant carotid stenosis, but there is no clear explanation of this fact [30–32].
Atrial fibrillation (AF) is one of the most important risk factors of cardioembolic stroke [1, 33–37]. To prevent the complications, within the recommendations for patients with AF there are novel oral anticoagulants (NOACs).
In our clinical practice, we observed numerous cases of the patients with permanent AF admitted to the hospital who experience an IS despite of all recommended therapy. We decided to analyze these patients.
Aim of our investigation is to study which variant of permanent AF without intra-heart thrombi is the most unfavorable in appearing of stroke.
Methods
In our investigation we included 202 patients (99 men and 103 women) of Samara state medical university clinics, Russia.
Including criteria were: permanent AF; hemo-dynamically not significant atherosclerotic stenosis of the internal carotid artery orifice (≤ 50 %); signed agreement form for participation in the investigation. Excluding criteria were: hypercoagulation-associated hematological diseases; intraheart thrombi; atrial myxoma; left ventricle or aorta aneurysm; mechanical prosthetic valve; mitral stenosis; sick sinus syndrome; myocardial infarction (< 4 weeks); dilated cardiomyopathy. In the control group, we included 88 people without AF.
In anamnesis, we paid attention to the previous history of stroke. The laboratory analyses obligatory included hemostasiograms, lipid profile, hemoglobin A1c. Within the diagnostic methods, we used transthoracic and transesophageal echocardiography (EchoCG), 24-hours monitoring of electrocardiography (ECG), ultrasound investigation of brachiocephalic arteries, sphyg-mography (SG) of common carotid arteries, computer tomography (CT) of the brain with contrast. In EchoCG, we excluded the intra-heart thrombi in all the patients as well as the aneurisms of left ventricle apex, septum, wall aneurisms as the possible future reasons of the thrombus forming.
In ultrasound of brachiocephalic arteries, we used B-mode, Doppler, B-flow, volumetric ultrasound. We calculated the linear blood flow velocity and the blood flow volume of common carotid artery as well as in the area of maximum atherosclerotic stenosis of internal carotid artery. As all the patients had permanent AF, we calculated these parameters during the spread of the pulse wave after the minimum and after the maximum duration of the pauses between ventricular contractions. We calculated the percentage of stenosis using ECST (European Carotid Surgery Trial), NASCET (North American Symptomatic Carotid Endarterectomy Trial) and St. Mary’s ratio criteria. Moreover, in our investigation we included the patients with atherosclerotic stenosis of the orifice of the internal carotid artery less than 50 % in diameter that is hemodynamically not significant. Also, we paid attention to the type of the plaques that we found, especially the non-stability signs (heterogenic structure, calcium, uneven surface of plaque etc.). To detect the type of the plaques we used Gray-Weale– Nicolaides ultrasound classification.
In SG, we calculated the parameters of arterial vessel wall that characterized mechanical movement of outer arterial contour: speed, acceleration, power, work. This method is non-invasive, accurate and complements the data from ultrasound investigation to make the fuller evaluation of the arterial hemodynamics and wall kinetics.
We have analyzed the 24-hours ECG monitoring of all the patients. According to these data, we divided all the patients into two groups up to the maximum pauses between ventricular complexes in AF:
-
1. Patients with a pause <1,5 seconds (113 people).
-
2. Patients with a pause ≥1,5 seconds (89 people).
These two groups were identical in sex, age and comorbidities.
The patients of all groups were on the same standard therapy recommended by current ESC guidelines including NOACs to prevent the thromboembolic complications in AF. We observed the patients during 1 year from the beginning of investigation. The additional visits were made 3, 6 and 12 months after the first visit. We analyzed the appearance of verified stroke or TIA in these patients.
In statistical analyses, we analyzed ultrasound parameter (linear blood speed flow); speed, acceleration, power, work calculated by SG for all 290 patients (1 group (N = 113), 2 group (N = 89), control group (N = 88)). We performed one-way analysis of variance (ANOVA) to compare the mean values of the independent groups for each analyzing parameter to calculate the statistical significance (p < 0,05). To estimate the stroke or TIA during 1 year of investigation, we made Cox analysis. We calculated the indices of a four-field table to establish the relationship between the pause duration between ventricular complexes in AF and the development of stroke or TIA within 1 year.
Results
The characteristics of groups 1, 2 and control group are presented at the table 1.
The ultrasound characteristics of the atherosclerotic plaques in carotid bifurcation area see on the table 2. The internal carotid stenosis in diameter is calculated by ECST, NASCET and St. Mary’s ratio criteria.
Table 1. Patients of 1, 2 and control groups
|
Characteristics |
1 group (N = 113) |
2 group (N = 89) |
Control group (N = 88) |
p-value |
|
Age 60–69 – no. (%) |
52 (46,0) |
44 (49,4) |
43 (48,9) |
NS* |
|
Age 70–79 – no. (%) |
42 (37,2) |
34 (38,2) |
33 (37,5) |
NS |
|
Age 80+ – no. (%) |
19 (16,8) |
11 (12,4) |
12 (13,6) |
NS |
|
Female sex – no. (%) |
61 (54,0) |
42 (47,2) |
45 (51,3) |
NS |
|
Systolic blood pressure, mm Hg |
139 ± 12 |
141 ± 9 |
132 ± 11 |
NS |
|
Body mass index |
23,8 ± 4,2 |
22,9 ± 3,4 |
23,1 ± 5,7 |
NS |
|
NYHA I-II – no. (%) |
106 (93,8) |
84 (95,5) |
85 (96,6) |
NS |
|
NYHA III – no. (%) |
7 (6,2) |
5 (4,5) |
3 (3,4) |
NS |
|
Ejection fraction, % |
56 ± 8 |
58 ± 9 |
61 ± 7 |
NS |
|
Dyslipidaemia – no. (%) |
19 (16,8) |
11 (12,4) |
12 (13,6) |
NS |
|
Myocardial infarction in anamnesis – no. (%) |
4 (3,5) |
4 (4,5) |
3 (3,4) |
NS |
|
Stroke in anamnesis – no. (%) |
6 (5,3) |
6 (6,7) |
4 (4,5) |
NS |
|
CHA 2 DS 2 -VASc, mean |
5,5 |
5,4 |
– |
NS |
*NS – not significant (p > 0,05).
Table 2. Atherosclerotic plaques in 1, 2 and control groups
|
Characteristics |
1 group (N = 113) |
2 group (N = 89) |
Control group (N = 88) |
p-value |
|
Common carotid artery, middle part, intima-media thickness (IMT) |
1,1 ± 0,1 |
1,1 ± 0,2 |
1,1 ± 0,1 |
NS* |
|
Common carotid artery in the area of bifurcation, stenosis in diameter, % |
30 ± 13 |
35 ± 10 |
33 ± 12 |
NS |
|
Internal carotid artery stenosis in diameter, % |
45 ± 13 |
45 ± 15 |
43 ± 12 |
NS |
|
Type (class) I: uniformly echolucent plaque – no (%) |
16 (14,2) |
8 (9) |
11 (12,5) |
NS |
|
Type (class) II: predominately echolucent plaque – no (%) |
83 (73,5) |
72 (80,9) |
67 (76,2) |
NS |
|
Type (class) III: predominantly echogenic plaque – no (%) |
14 (12,3) |
9 (10,1) |
10 (11,3) |
NS |
|
Type (class) IV: uniformly echogenic plaque – no (%) |
0 (0) |
0 (0) |
0 (0) |
NS |
|
Type (class) V: heavy calcification – no (%) |
0 (0) |
0 (0) |
0 (0) |
NS |
*NS - not significant (p>0,05).
So, we see that the parameters of plaques characteristics within the groups were identical. The main factor of the difference between two main groups was the maximum duration of pauses between ventricular contractions in patients with AF. Also, very important thing was that despite hemodynamically non-significant atherosclerotic lesions in carotid arteries in both main groups there were the patients with type III plaques that potentially can be the source of the embolic events in the brain in case if there will be some conditions and predictors for that.
In AF we observed the following tendency: in ultrasound investigation, there was increase of linear blood flow speed and the volume flow in the area of carotid stenosis in the moments during the spread of the pulse wave after the long pause between ventricular contractions in group 2. The speed was rising up to 2,5 m/sec as it rises when there is the hemodynamically significant steno-sis.The parameters of SG were increasing proportionally to the linear blood flow speed measured by ultrasound, with the same tendency: the maximum growth of arterial wall kinetic parameters (speed, acceleration, power, work) was observed in group 2 after the long pause between ventricular contractions (figure 1).
Analyzing the data, we see that in general evaluation of cardiovascular events risk up to the CHA 2 DS 2 -VASc score in all two main groups was identical. So, the expected possibility of stroke and TIA was the same in these groups.
But in 1 year of investigation, we observed the statistically significant difference in stroke between the two main groups despite of anticoagulant therapy (table 3, figure 2).
SG kinetic parameters in groups (in %) in comparison with control group
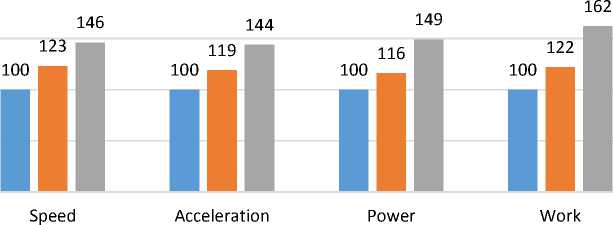
Control group Group 1 Group 2
Figure 1. SG kinetic parameters in groups (in %) in comparison with control group (p < 0,05)
Stroke and TIA in 1-year investigation
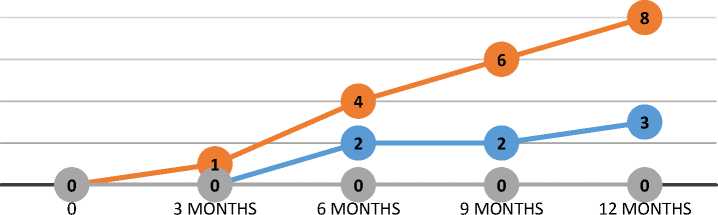
^^Group 1 ^^—Group 2 ^•— Control group
Figure 2. Stroke and TIA in 1, 2 and control groups (Cox analysis)
Table 3. Stroke in 1 year of investigation
|
1-year complications – no (%) |
1 group (N = 113) |
2 group (N = 89) |
Control group (N = 88) |
p-value |
|
Stroke |
2 (1,8) |
5 (5,6) |
0 (0) |
< 0,05 |
|
TIA |
1 (0,9) |
3 (3,4) |
0 (0) |
< 0,05 |
Discussion
Numerous investigations lead to the common opinion that hemodynamically significant carotid arteries stenosis brings the high risk of stroke. In this case the surgical treatment is strongly recommended (operation of carotid endarterectomy, carotid artery stenting). In atherosclerotic stenoses less than 50 % there are no indications for surgical correction, and only dynamic observation and medical treatment are prescribed to predict the possible growing of the plaque with further stroke complications. Multiple studies from 1978 till present time confirm the increasing of the stroke risk in patients with hemodynamically nonsignificant carotid arteries stenosis [28–32]. Despite of this fact was observed, there is still no clear opinion of the mechanism and what can be the starting torque to cause the stroke.
From the other side, the main reason of the stroke is AF. When analyzing this arrhythmia, the cardiologists for prevention of cardioembolic stroke prescribe for these patients such drugs as NOACs.
In our investigation, we also confirmed more frequent stroke in patients with hemodynamically non-significant carotid stenosis in patients with AF, that was more frequent in group 2 where the pauses between ventricular contractions in AF were 1,5 seconds and more. In all the patients we excluded intra-heart thrombi and they regularly took anticoagulant therapy. What could be the source of stroke in these cases?
We believe that the reason of the stroke could be the defragmentation of the atherosclerotic plaques in carotid bifurcation area as well as intracranial non-visualized plaques. And the starting torque for that situation was the spreading pulse wave after the long pause between ventricular contractions in AF. The increased hemodynamic characteristics (linear blood speed flow, kinetic parameters of vessel wall – speed, acceleration, power, work) cause the additional mechanical damage of the atherosclerotic plaque, additional vessel stretching that can lead to embolic stroke.
Moreover, this mechanism of the additional mechanical impact is the universal mechanism that also is observed in other arrhythmias, for example, in first post-extrasystolic wave after the compensatory pause of extrasystole, in atrioventricular blockades, the first regular wave after sinus rhythm restoration after AF or heart palpitation, in activation of the pacemaker after prolonged asystole as well as in the other situations when the pulse wave with increased hemodynamic characteristics spreads after the long pause between ventricular contractions. We described these effects in our previous publications [38, 39]. And in this case the main importance will play not only the quantity of such situations but also more the characteristics of these pulse waves. Even one of them can cause the destabilization of the plaque with further complications. Moreover, we were able to confirm our clinical observations in experimental cardiology using the original device for intra-arterial circulation modeling created by us, where we simulated all these hemodynamical situations [40, 41].
Conclusions
-
1. The more maximum duration between ventricular contractions in AF the more increasing of arterial vessel hemodynamic and kinetic parameters is observed.
-
2. The appearance of stroke and TIA in AF is higher in those patients who have 1,5 seconds and more of maximum duration pauses between ventricular contractions.
-
3. In cryptogenic stroke, the reason of it can be the atherosclerotic plaque defragmentation with further embolism, caused by the additional mechanical impact of increased hemodynamical and kinetic parameters of pulse wave after long pause between ventricular contractions in AF.
Список литературы Cryptogenic stroke in atrial fibrillation without intra-heart thrombi: possible mechanisms
- Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-e467. https://doi.org/10.1161/STR.0000000000000375. Epub 2021 May 24. Erratum in: Stroke. 2021 Jul;52(7):e483-e484. PMID: 34024117.
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139-e596. https://doi.org/10.1161/CIR.0000000000000757
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME); 2017. http://ghdx.healthdata.org/gbd-results-tool. Accessed March 15, 2018.
- Kleindorfer D, Panagos P, Pancioli A, Khoury J, Kissela B, Woo D, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. 2005;36:720-723. https://doi.org/10.1161/01 .STR.0000158917.59233.b7
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 19902017: a systematic analysis for the Global Burden of Disease Study 2017.Lancet. 2018;392:1789-1858. https://doi.org/10.1016/S0140-6736(18)32279-7
- Johnson CO, Nguyen M, Roth GA, Nichols E, Alam T, Abate D, et al. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016.Lancet Neurol. 2019; 18:439-458.
- Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al.. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151-1210. https://doi.org/10.1016/S0140-6736(17)32152-9
- Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al. European Cardiovascular Disease Statistics 2017. Brussels: European Heart Network; 2017.
- Bennett DA, Krishnamurthi RV, Barker-Collo S, Forouzanfar MH, Naghavi M, Connor M, et al.; Global Burden of Diseases, Injuries, and Risk Factors 2010 Study Stroke Expert Group. The global burden of ischemic stroke: findings of the GBD 2010 study. Glob Heart. 2014;9:107-112. https://doi.org/10.10167j.gheart.2014.01.001
- Kunst AE, Amiri M, Janssen F. The decline in stroke mortality: exploration of future trends in 7 Western European countries. Stroke. 2011;42:2126-2130. https://doi.org/10.1161/STR0KEAHA.110.599712
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010.Lancet. 2012;380:2197-2223. https://doi.org/10.1016/S0140-6736(12)61689-4
- Zahra A, Lee EW, Sun LY, Park JH. Cardiovascular disease and diabetes mortality, and their relation to socio-economical, environmental, and health behavioural factors in worldwide view. Public Health. 2015;129:385-395. https://doi.org/10.1016/j.puhe.2015.01.013
- Bejot Y, Bailly H, Durier J, Giroud M. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med. 2016;45(12 pt 2):e391-e398. https://doi.org/10.1016/jJpm.2016.10.003
- OECD. Mortality from heart disease and stroke. In: Health at a Glance: Europe 2016: State of Health in the EU Cycle. Paris: OECD Publishing; 2016.
- Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world.Lancet Neurol. 2007;6:182-187. https://doi.org/10.1016/S1474-4422(07)70031 -5
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030.PLoS Med. 2006; 3:e442. https://doi.org/10.1371 /journal.pmed.0030442
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study.Lancet. 1997;349:1498-1504. https://doi.org/10.1016/S0140-6736(96)07492-2
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Methodology of the United Nations Population Estimates and Projections, Working Paper No. ESA/P/WP.250. New York: United Nations; 2017.
- Asplund K. What MONICA told us about stroke.Lancet Neurol. 2005;4:64-68. https://doi.org/10.1016/S1474-4422(04)00967-6
- Truelsen T, Piechowski-Jozwiak B, Bonita R, Mathers C, Bogousslavsky J, Boysen G. Stroke incidence and prevalence in Europe: a review of available data.Eur J Neurol. 2006;13:581-598. https://doi.org/10.1111/j.1468-1331.2006.01138.x
- Truelsen T, Begg S, Mathers CD, Satoh T. Global burden of cerebrovascular disease in the year 2000.In: GBD 2000 Working Paper. Geneva, Switzerland: WHO; 2002.
- Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet, 2018;392:2052-2090. https://doi.org/10.1016/S0140-6736(18)31694-5
- Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001;32:2735-2740. https://doi.org/10.1161/hs1201.100209
- Gardener H, Sacco RL, Rundek T, Battistella V, Cheung YK, Elkind MSV. Race and ethnic disparities in stroke incidence in the Northern Manhattan Study. Stroke. 2020;51:1064-1069. https://doi.org/10.1161/STROKEAHA.119.028806
- Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O'Donnell MJ, et al. Cryptogenic Stroke/ESUS International Working Group. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014; 13:429-438. https://doi.org/10.1016/S1474-4422(13)70310-7
- Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2019 update: a report from the American Heart Association. Circulation 2019;139:e56-e528.
- Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke. 2008; 39:2396-2399. https://doi.org/10.1161/STROKEAHA.107.505776.
- Qureshi AI, Ziai WC, Yahia AM, Mohammad Y, Sen S, Agarwal P, et al. Stroke-free survival and its determinants in patients with symptomatic vertebrobasilar stenosis: a multicenter study. Neurosurgery. 2003;52:1033-1039; discussion 1039.
- Messas E, Goudot G, Halliday A, Sitruk J, Mirault T, Khider L, at al on behalf the ESC WG of Aorta & Peripheral Vascular Diseases, Management of carotid stenosis for primary and secondary prevention of stroke: state-of-the-art 2020: a critical review, European Heart Journal Supplements, Volume 22, Issue Supplement_M, November 2020, Pages M35-M42. https://doi.org/10.1093/eurheartj/suaa162
- Schermerhorn ML, Liang P, Dakour-Aridi H, Kashyap VS, Wang GJ, Nolan BW, et al. In-hospital outcomes of transcarotid artery revascularization and carotid endarterectomy in the Society for Vascular Surgery Vascular Quality Initiative. J Vasc Surg. 2020 Jan;71(1):87-95.
- Uno M, Takai H, Yagi K, Matsubara S. Surgical Technique for Carotid Endarterectomy: Current Methods and Problems. Neurol Med Chir (Tokyo). 2020 Sep 15;60(9):419-428. https://doi.org/10.2176/nmc.ra.2020-0111. Epub 2020 Aug 15. PMID: 32801277; PMCID: PMC7490601.
- Howard VJ, Meschia JF, Lal BK. Carotid revascularization and medical management for asymptomatic carotid stenosis: protocol of the CREST-2 clinical trials. Int J Stroke, 12 (2017), pp. 770-778.
- Ceornodolea AD, Bal R, Severens JL. Epidemiology and management of atrial fibrillation and stroke: review of data from four European countries. Stroke Res Treat 2017;2017:8593207.
- Pistoia F, Sacco S, Tiseo C, Degan D, Ornello R, Carolei A. The epidemiology of atrial fibrillation and stroke. Cardiol Clin 2016;34:255-268.
- Lin H, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke 1996;27:1760-1764.
- Overvad TF, Nielsen PB, Lip GY. Treatment thresholds for stroke prevention in atrial fibrillation: observations on the CHA2DS2-VASc score. Eur Heart J Cardiovasc Pharmacother 2017;3:37-41.
- Frost L, Engholm G, Johnsen S, Moller H, Henneberg EW, Husted S. Incident thromboembolism in the aorta and the renal, mesenteric, pelvic, and extremity arteries after discharge from the hospital with a diagnosis of atrial fibrillation. Arch Intern Med 2001;161:272-276.
- Germanova O, Shchukin Y, Germanov V, Galati G, Germanov A. Extrasystolic arrhythmia: is it an additional risk factor of atherosclerosis? Minerva Cardioangiol. 2021 Jan 11. https://doi.org/10.23736/S0026-4725.20.05490-0. Epub ahead of print. PMID: 33427426.
- Germanova O, Germanov VA, Shchukin YV, Germanov AV, Galati G. Device for modeling of intra-arterial circulation: application in experimental cardiology, European Heart Journal, Volume 42, Issue Supplement_1, October 2021, ehab724.0299. https://doi.org/10.1093/eurheartj/ehab724.0299
- Germanova OA, Germanov VA, Shchukin YuV, Germanov AV, Piskunov MV. Extrasystoles: adverse effects of the first postextrasystolic contraction. Bulletin of the Medical Institute "REAVIZ" (REHABILITATION, DOCTOR AND HEALTH). 2020;(6):89-97. (In Russ.) https://doi.org/10.20340/vmi-rvz.2020.6.11


