E-health Implementation by Private Dental Service Providers in Bulawayo, Zimbabwe
Автор: Vusumuzi Maphosa
Журнал: International Journal of Information Engineering and Electronic Business @ijieeb
Статья в выпуске: 1 vol.15, 2023 года.
Бесплатный доступ
The 2030 Agenda for Sustainable Development Goals recognises the role of Information and Communication Technologies (ICT) in accelerating human development and progress by bridging the digital divide and developing knowledge societies. Internet technologies affect every sphere of human and organisational life. The study was motivated by low e-health adoption in developing countries such as Zimbabwe. A cross-sectional quantitative survey investigated e-health implementation by private dental care service providers in Bulawayo. The research population comprised private dental service providers in Bulawayo. Data was collected using a five-point Likert scale questionnaire that was self-administered. Regression and factor analysis, Kaiser-Meyer-Olkin Measure of Sampling Adequacy, Bartlett’s sphericity test, and the Principal Component Analysis were used for data analysis. The study found that private dental service providers in Bulawayo were already implementing some rudimentary elements of e-health in their day-to-day practice. The findings also revealed that private dental care providers positively perceived the benefits of implementing e-health, such as improved quality of health service delivery, enhanced efficiency, and improved accessibility of services. Participants highlighted ICT costs, communication, lack of experience, and e-readiness as significant barriers to e-health implementation. Most participants were concerned that personal health information may fall into the wrong hands resulting in privacy violations and loss of personal data. The regression coefficient showed that combined variations in the independent variables explain at least 76.4% of the dependent variable (adoption). The study recommends the government enact policies that support private dental service providers in implementing e-health systems to improve service delivery. The study contributes to the literature on e-health adoption in developing countries.
Telemedicine, health delivery, e-health, electronic health records
Короткий адрес: https://sciup.org/15018800
IDR: 15018800 | DOI: 10.5815/ijieeb.2023.01.02
Текст научной статьи E-health Implementation by Private Dental Service Providers in Bulawayo, Zimbabwe
Published Online on February 8, 2023 by MECS Press
The technological revolution of the 21st-century fuels Internet adoption in every sphere of human and organisational life, which includes healthcare. The 2030 Agenda for Sustainable Development Goals recognises the role of Information and Communication Technologies (ICT) in fostering global interconnectedness, bridging the digital divide and developing knowledge societies which accelerate human progress [1]. The diffusion of smartphone technology has increased access to the Internet and applications (apps) among individuals once alienated from the information superhighway [2,3]. The cost of delivering medical services and patient waiting times reduce by embracing ICTs, while revenue and patient safety are improved [4]. Popovic and Maksimovic [5] conclude that the rapid development of ICT, artificial intelligence and big data facilitates the efficient transfer of healthcare information.
Healthcare outcomes improve through artificial intelligence, the Internet of Things (IoT), virtual care, big data analytics, blockchain, and smart wearables. Artificial intelligence and the IoT have led to magnificent developments in the medical fraternity, allowing surgeons to conduct procedures remotely [6]. Electronic health (e-health) is the confluence of medical informatics and public health, which delivers health services and information through Internet-supported technologies [7]. Busagala and Kawano [8] define e-health as combining the healthcare system and ICT to enable better healthcare. E-health uses electronic means to provide health-related information, resources, and services [7]. Qureshi and Shah [9] define e-health as the exchange of health information between various stakeholders. For example, Vimarlund et al. [10] define e-health as the interaction between patients and doctors using electronic devices that support well-being. The World Health Organization states that e-health is the cost-effective and secure use of ICTs to support healthcare services, health surveillance, health literature, health education, knowledge, and research [11].
E-health systems offer many benefits, such as improved communication, time-saving, improved quality of medical service, cost-saving, and reduced medical errors [4,12,13]. Furusa and Coleman [14] noted that most healthcare institutions in Zimbabwe lack the ICT infrastructure to support e-health systems. E-health strategies are necessary interventions that address many problems and challenges in healthcare service delivery. The World Health Organisation (WHO) developed its global strategy on digital health and identified priority areas related to developing ICT infrastructure for health that promotes equitable, affordable, and universal access to healthcare [15]. The strategy acknowledges the radical change in health outcomes that can be brought about by digital health and calls for investment in digital technologies, training, support, management, and governance. Zimbabwe’s 2021-2025 eHealth/Digital Health strategy empowers the Ministry of Health and Child Care (MoHCC) to plan and communicate with partners regarding digitising health service delivery, allowing the country to meet its obligation of Universal Health Coverage by 2030 [16]. The MoHCC acknowledges that adopting digital platforms will create a conducive environment to support the development, survival, and sustainability of digital health innovations from the grassroots level. Zimbabwe’s e-health strategy provides clear guidelines that can propel the transformation and growth of e-health through the effective use of ICTs.
The WHO and the International Telecommunication Union (ITU) recognise the significance of collaboration for ehealth, demanding that countries develop national e-health strategies [17,18]. The agencies developed a National ehealth Strategy Toolkit, providing a practical guide for governments and their national ministries. Electronic Health Records (EHR) benefits patients, healthcare workers, organisations, and the entire healthcare system. Patients may benefit from the improved quality of care supported by evidence-based clinical decision-making, clinician decision support, and electronic prescribing technologies.
E-health has great potential to complement traditional health delivery for rural and remote communities. The implementation of e-health in developing countries is undertaken to achieve benefits such as improved quality and continuity of healthcare, improved patient tracking and follow-up, and improved administration and monitoring of treatment programs [19]. Converting IT affordances into actual outcomes is complex and subject to numerous contextual factors. Implementers should identify typical constraints that hinder healthcare providers’ successful use of e-health.
Although components such as EHR, electronic medical record (EMR), and telemedicine can enhance the quality of life and improve the safety of patients, high costs and difficulties in implementation remain critical barriers despite the clear benefits. Inadvertently some developed countries have been slow in adopting e-health [20]. Consequently, implementing e-health systems depends on other factors, such as technical support in medical institutions and ICT skills among health practitioners. Varkey et al. [21] and Luca et al. [4] evaluated the adoption of e-health by physicians. They revealed that although its adoption has been surging globally, its uptake in developing countries has been relatively sluggish. E-health implementation is essential in developing countries due to the shortage of doctors and nurses. In response to the knowledge gap, the study seeks to identify the factors influencing the adoption of e-health in Zimbabwean private dental service providers.
2. Literature Review
Nzuki and Mugo [7] posited that e-health aims to facilitate the delivery of health services, information, and awareness campaigns through Internet-related platforms both to the locals and the people in distant places because, with the Internet, distance is not a barrier. E-health is blending medical care framework and ICT to empower better wellbeing and access to medical services. Busagala and Kawono [8] indicated that well-being includes a broad scope of activities that utilise electronic systems to give wellbeing-related data, assets, and administrations. Qureshi and Shah [9] depict well-being as any electronic trade of well-being data inside the medical care domain.
-
2.1 E-health components
-
2.2 Factors affecting the adoption of e-health
-
2.3 Benefits of implementation of e-health
According to the WHO, e-health strategy components are EMR, telehealth, telemedicine, m-Health, e-learning, continuous education for health professionals, and interoperability and standardisation [11]. EMRs are records of each patient’s health information, while telehealth and telemedicine refer to the delivery of health services using ICTs. M-Health refers to medical and public health practices supported by mobile devices and other wireless devices [10]. Telemedicine is just one cog of e-health, and according to Vimarlund et al. [13], it refers to healthcare practised at a distance. Maphosa [13] adds that telemedicine enables administering healthcare services using ICTs through the exchange of data for diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and raising awareness and education with the sole objective of improving the health of individuals and their communities.
Huston [23] asserts that most e-health technologies fail because implementers overlook the interdependencies between technology and the socioeconomic environment - resulting in technology failing to impact healthcare practices. Lack of management support and strategic level commitment, poor communication, lack of training, ineffective project management techniques, poor design of processes, and failure to handle change requirements contribute to failure [25].
Additionally, Huston [23] notes the importance of retaining experienced health workers and positive behaviour, which supports the training argument.
Kusumasari et al. [25] concluded that because of high initial costs, and migration costs, health institutions might slow the implementation of e-health strategies. In their study, Wicks et al. [26] found evidence that introducing e-health technologies may occasionally generate new risks. Patients may over-depend on clinical decision support systems such as e-prescribing or over-magnifying perceived functionality resulting in reduced performance. Another study highlighted that quality in healthcare could be improved by evaluating the adequacy of healthcare systems [22].
Poor ICT infrastructure, scarce financial resources, and lack of skilled staff slow developing countries from implementing e-health [22]. Zimbabwe’s e-health implementation is hampered by a lack of access to essential equipment for medical care, which limits the installation of advanced high-end technology [14]. Steep broadband costs constrain healthcare service providers as they rely on data to make informed decisions that enhance healthcare [23]. According to Wang et al. [24], patients may fail to utilise e-health entirely because they have become accustomed to physical interaction with healthcare personnel. In addition, they need to trust that their health data will be secure and confidential. These factors also impact the implementation of e-health in Zimbabwe.
E-health tools can also improve communication between healthcare actors through systems for messaging and audio-visual communication [27]. E-health supports people with multi-morbidity living at home by providing tools that educate and empower them in self-care and checking their coping behaviours and treatment adherence. E-health has far-reaching benefits, including improved healthcare communication, accessibility, and decision-making [6]. E-wellbeing can be utilised to work with mindfulness crusades on well-being matters and advance well-being drives. It can bring a worldview swing in customary medical care frameworks by limiting clinical blunders, extending medical care quality, lessening medical care costs, and engaging patients to deal with their clinical necessities [13,28]. E-wellbeing arrangements can expand productivity, improve patient security, and enhance well-being [7,8].
EHRs assist providers in conveniently and accurately capturing patient charges [29,30]. With an EHR framework, many charging mistakes or off-base coding might be wiped out, conceivably expanding the service provider’s income and convenience to the patient [31]. Lewis et al. [32] investigated the feasibility of using EMR for supporting antiretroviral therapy (ART) clinical guidelines in Malawi. The study concluded that EHRs positively impacted healthcare through improved performance and supervision of healthcare workers.
The use of e-health systems in developed countries has been reported to advance healthcare services [9]. There is no universal approach to implementing e-health systems, and governments are at different stages in using EHR; for example, Sweden, the Netherlands, and Australia are at 90%, 62%, and 55%, respectively [7]. Even though the diffusion of technology is high in developed countries and the economies are stable, the adoption of e-health seems significantly lower; for example, the number of physicians who use EMR/EHR systems in the US varies from 54% in New Jersey to 89% in Massachusetts [7]. Lewis et al. [32] observed few opportunities to increase knowledge through continuous learning among healthcare workers in most developing countries. Adopting e-health will achieve more meaningful results for the health sector; therefore, this research endeavours to investigate the implementation of ehealth by private dental service providers in Zimbabwe.
3. Methods
A cross-sectional quantitative study targeted private dental service providers in Bulawayo. Data was gathered using a 48-item questionnaire to evaluate the effect of e-health implementation on private dental healthcare providers. A pilot study was done to ensure the reliability and validity of each construct. The first part of the questionnaire includes information regarding the characteristics of respondents (e.g., age, gender, experience, adoption of electronic devices and services). The other sections have questions that measure other constructs, using a five-point Likert scale (1) Strongly Disagree to (5) Strongly Agree. Participants were informed about the research through a consent form containing a brief description of the study, a time frame for activities, and a statement indicating voluntary participation.
4. Results
One hundred and twenty-five questionnaires were administered to the target population of private dental clinics in Bulawayo. One hundred and one questionnaires were completed and collected, resulting in a response rate of 88.17%. The internal consistency of the scale’s items was measured using Cronbach’s Alpha. According to Barbera et al. [33], Cronbach’s Alpha is the widely accepted measure for instrument reliability.
Table 1. Reliability Statistics
|
Cronbach’s Alpha |
Cronbach’s Alpha Based on Standardised Items |
N of Items |
|
.801 |
.819 |
9 |
Barbera et al. [33] prescribed a minimum acceptable threshold of 0.7. The results presented show a high Cronbach’s Alpha of 0.819, obtained from the nine items of the questionnaire, indicating that the research instrument utilised for data collection was reliable (See Table 1.). Most (59%) of the respondents were female while 41% were male. Table 2 shows that the 31-40 age group represented most (49.5%) of the respondents, followed by the 20-30 age group, which had 37.6%. Those above 40 years constituted 12.87%. Minichiello et al. [34] found the age distribution pivotal in adopting and implementing e-health because the younger generation has a good aptitude for technological adoption.
Table 2. The age distribution of the respondents
|
Age |
Frequency |
Per cent |
|
20-30 |
38 |
37.6 |
|
31-40 |
50 |
49.5 |
|
Above 40 |
13 |
12.87 |
|
Total |
101 |
100.0 |
Experience gained by working in private dental care is one of the key variables determining the implementation of e-health services. Table 3. shows that the majority (63.37%) have 6 and 10 years of experience, followed by 24.75% with over ten years of experience. Those with 0 to 5 years of experience accounted for 11.88%. Based on the assertions of Minichiello et al. (2014), most private healthcare providers could be able to adopt and implement an e-health system.
Table 3. The experience of the respondents
|
Frequency |
Per cent |
||
|
Valid |
0-5 |
12 |
11.89 |
|
6-10 |
64 |
63.37 |
|
|
>10 |
25 |
24.75 |
|
|
Total |
101 |
100.0 |
|
Regarding qualifications, the findings reveal that the majority (38%) of the respondents had a first degree as their highest qualification, 10% had a certificate, 30% had a diploma, 19% had a master’s degree, and 3% had a PhD. Based on the assertions of Minichiello et al. [34], the respondents had a sufficient level of education to appreciate the need for implementing e-health. Toivonen and Tuominen [22] found that the educational distribution of respondents was among the top priority factors determining the adoption and implementation of e-health systems. Maphosa and Maphosa [35] noted that service providers who have been in business for a considerable number of years are more likely to adopt new technology than those who have just started. This is because they would have generated resources to meet and sustain the costs and demands of adopting new technology.
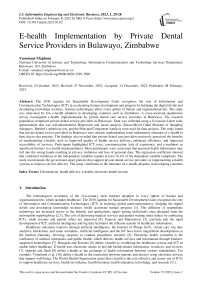
■ Agree ■ S/Agree ■ Neutral Disagree ■ S/Disagree
Fig. 1. The extent to which private dental care providers adopted e-health
The degree of e-health implementation was measured using the adoption of electronic services such as video and telephone consultation, remote monitoring, education communication, and training via the phone. Fig. 1. shows that most (70%) private dental care providers used consultation by phone to administer dental healthcare services. Regarding consultations via video, 60% of the respondents agreed, while 29% disagreed. Remote monitoring was not a popular e-health system, as indicated by 38% of the respondents who agreed, 20% were neutral, and 32% disagreed.
The finding suggests that private dental healthcare providers do not widely use remote monitoring. Training via the telephone is an e-health service that the respondents highly rated (84%), followed by education communication (78%) and e-health records (75%). The findings affirm that private dental care providers have adopted some elementary ehealth systems to align their dental care services to global trends. According to Minichiello et al. [34], this positively affects their performance because e-health enables them to provide healthcare services remotely, irrespective of distance and other barriers.
The findings show that the Internet was the most (94%) widely used tool to support e-health services and operations. Multimedia devices, including computers, smartphones, and tablets, were rated second with a score of 78%, and specialised healthcare software was rated at 66%. The finding shows that Bulawayo’s private dental care service providers are conscious of e-health services and aware of the positive impact of the delivery of dental healthcare services. COVID-19-induced lockdowns enhanced the popularity of e-health services as it became challenging for doctors and patients to have physical contact while delivering healthcare services.
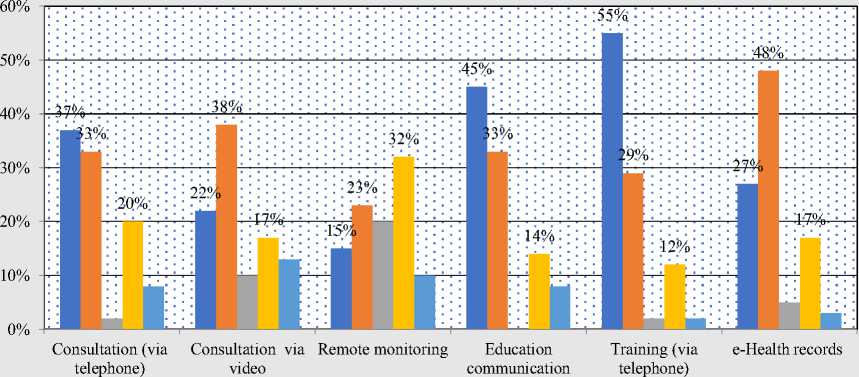
■ Agree ■ S/Agree ■ Nuetral ■ Disagree ■ S/Disagree
Fig. 2. Factors affecting the implementation of e-health services
The respondents were asked to rate four significant variables Arduini and Zanfei [36] identified as critical determinants affecting e-health implementation. These were e-readiness, effective communication, adequate experience, and ICT-related costs. Fig.2. shows that about three-quarters (74%) of the respondents agreed that good expertise was a key variable in determining the implementation of e-health. ICT-related costs were also highly rated as a variable that affects the adoption of e-health by 83% of the respondents. This is in line with Allaire et al. [17], who found that IT-related costs included project change process costs, electricity, employee remuneration, and ventilation of the systems, such as server rooms and migration costs.
Regarding e-readiness, 66% of the respondents agreed that it affects e-health implementation, while 34% disagreed. Two-thirds agreed that effective communication influences successful e-health implementation. This finding is in sync with Huston [23], who alluded that effective communication before, during, and after implementing e-health strategies is essential to success.
-
4.1 Perception and attitudes on e-health implementation
-
4.2 Factor analysis
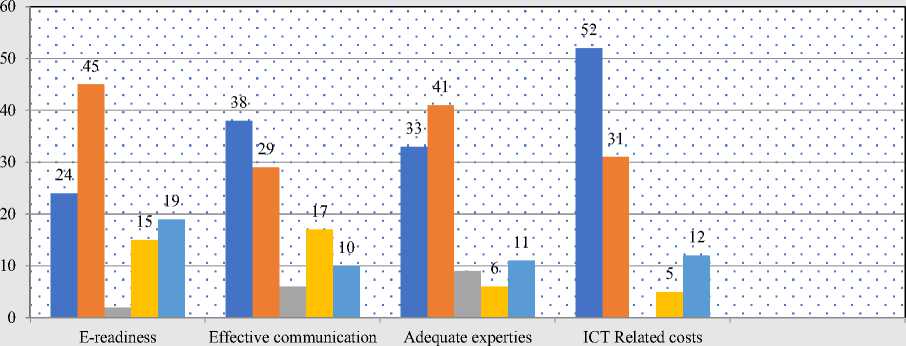
The respondents’ perceptions and attitudes on e-health were also evaluated to determine how they impacted the implementation of e-health by private dental healthcare providers in Bulawayo. Putteeraj et al. [37] observed that perceptions and attitudes of private dental providers have a bearing on the adoption of e-health. The findings presented in Fig. 3. generally show that private healthcare providers positively perceived the implementation of e-health. This view is derived from 75% of the participants who perceived e-health as an efficient healthcare delivery initiative. What makes e-health effective is that it facilitates the accessibility of medical healthcare remotely.
The findings also show that 73% of the participants rated e-health as convenient. The respondents expressed that ehealth improves the interaction between healthcare providers and patients, as demonstrated by 80% of the respondents. Minichiello et al. [34] also reported a similar finding, stating that e-health had become a burgeoning field in which health professionals and consumers create and seek information. Most respondents (86%) agreed that e-health reduces healthcare access barriers. This empowers patients to engage with information technology to enhance their dental care knowledge and quality of life. The findings reveal that private dental care providers in Zimbabwe know that the explosion of technology presents new opportunities to provide online dental health services.
■ Agree ■ S/Agree ■ Nuetral Disagree ■ S/Disagree
Fig. 3. The perception and attitude of e-health implementation
Factor analysis was conducted to extract the factors that impacted the implementation of e-health by private dental service providers in Bulawayo. To effectively perform the factor analysis, the Kaiser-Meyer-Olkin Measure of Sampling Adequacy and Bartlett’s test of Sphericity was done to determine the adequacy of the sample items for factor analysis. According to Mason [38], Kaiser Mayer Olkin (KMO) values between 0.5 and 0.7 are acceptable; values between 0.7 and 0.8 are good, while values between 0.8 and 0.9 are excellent, with superb values being 0.9 and above. Tables 4, 5, and 6 present factor analysis results.
Table 4. KMO and Bartlett’s Test
|
KMO and Bartlett’s Test |
||
|
Kaiser-Meyer-Olkin Measure of Sampling Adequacy. |
.854 |
|
|
Bartlett’s Test of Sphericity |
Approx. Chi-Square |
297.192 |
|
Df |
45 |
|
|
Sig. |
.000 |
|
Table 4. presents the KMO and Bartlett’s test statistics. The results show a KMO statistic of 0.854, more significant than 0.50. This affirms the adequacy of the sample items for factor analysis. Bartlett’s test of Sphericity was conducted, giving a Sig value of .000. The value qualifies the test as appropriate since it indicates a possibility of a relationship between the study variables.
Table 5. Factor extraction
|
Total Variance Explained |
||||||
|
Component |
Initial Eigenvalues |
Extraction Sums of Squared Loadings |
||||
|
Total |
% of variance |
Cumulative % |
Total |
% of variance |
Cumulative % |
|
|
1 |
3.544 |
35.442 |
35.442 |
3.544 |
35.442 |
35.442 |
|
2 |
2.169 |
21.690 |
57.132 |
2.169 |
21.690 |
57.132 |
|
3 |
1.230 |
12.301 |
69.433 |
1.230 |
12.301 |
69.433 |
|
4 |
.934 |
9.342 |
78.775 |
|||
|
5 |
.785 |
7.847 |
86.623 |
|||
|
6 |
.526 |
5.261 |
91.884 |
|||
|
7 |
.395 |
3.954 |
95.837 |
|||
|
8 |
.270 |
2.698 |
98.536 |
|||
|
Extraction Method: Principal Component Analysis. |
||||||
Table 5. shows that three (e-readiness, cost, and lack of expertise) of the eight factors affected the implementation of e-health by private dental care service providers as their Eigen values were greater than 1.0. The highest percentages of variance were 35.442, 21.690, and 12.301 for factors 1, 2, and 3, respectively. Hence, it was revealed that there are three significant factors.
4.3 Regression Analysis
5. Discussion
The impact of each independent variable on the dependent variable was predicted using regression analysis. After extracting some mean factors through the Principal Component Analysis, the variables were used for regression analysis, as shown in Table 6.
Table 6. Regression analysis
|
The regression in the perceptions and factors influencing e-health implementation |
||||||
|
Model |
Unstandardised Coefficients |
Standardised Coefficients |
T |
Sig. |
||
|
B |
Std. Error |
Beta |
||||
|
1 |
(Constant) |
.440 |
.074 |
1.220 |
.100 |
|
|
Perceptions |
.364 |
.035 |
.081 |
1.867 |
.063 |
|
|
Factors |
.296 |
.054 |
.290 |
5.525 |
.000 |
|
|
a. Dependent Variable: Adoption |
||||||
Table 7. Model summary
|
Model |
R |
R Square |
Adjusted R Square |
Std. Error of the Estimate |
|
1 |
.681a |
.764 |
.440 |
.31920 |
Table 7. shows the value of R–square of 0.764, which is the coefficient of determination, showing that the model can explain at least 76.4% of the variability of the response data around its mean. Perceptions and attitudes of dental care providers were found to have a statistically significant positive impact. A coefficient of 0.364 implies that a unit improvement in the perceptions will result in a 0.364 unit increase in e-health implementation. Factors influencing ehealth adoption were found to have a statistically significant positive impact on the success of private dental providers in terms of service provision. A coefficient of 0.296 implies that a unit increase in factors will result in a 0.296 increase in the adoption of e-health by private dental providers in Bulawayo.
The finding suggests that private dental care service providers are ready and willing to implement e-health. This is a significant finding which shows that private dental care providers are aware of the benefits that accrue following the implementation of e-health. This finding is consistent with Allaire et al. [17], who noted that e-health enables patients to promptly access health-related services irrespective of the distance from the physical location of the service provider. This reduces the time lost travelling to the nearby dental care service provider. E-health increases service delivery, and this has been noted by Obe and Akinloye [27], who pointed out that e-health solutions can help collect, store, and report health data to professionals and patients via EHRs and patient health records (PHRs).
The analysis shows that the three components were critical determinants of e-health implementation: e-readiness, cost, and lack of expertise. E-readiness has also been recognised by Arduini and Zanfei [36] as playing a leading role in determining the extent to which companies can adopt new technology. Technology and change management costs affect e-health implementation, as noted by Allaire et al. [17]. These costs can be very substantial for e-health implementation in developing countries. The skills gap and lack of expertise in implementing highly technical applications affect most projects in developing countries.
Given that the adoption of e-health is generally low in Zimbabwe, the study’s findings challenge healthcare practitioners to implement e-health in the entire health delivery system in Zimbabwe. The unavailability of policies and low government involvement are also significant barriers to adopting e-health. Future studies could also investigate patients’ perceptions of adopting e-health. The study’s primary limitation was that it was conducted on a small sample, limiting the generalizability of the findings.
6. Conclusion
The study contributes significant insights into private dental service delivery in Zimbabwe. This study contributes to the growing literature on e-health implementation in Zimbabwe and most developing countries, as there is a dearth of literature on e-health implementation. The findings affirm that private dental care providers have adopted some elementary e-health systems such as consultations by phone and video, communication, and education. Training and maintenance of electronic records was a popular e-health strategy. Most participants perceived e-health as an efficient healthcare delivery initiative and facilitated remote access to health services. Participants rated e-health as convenient, improved healthcare provider and patient interaction, and reduced healthcare access barriers. The Internet, multimedia devices, computers, smartphones, tablets, and specialised healthcare software were used to support e-health.
The finding also identified the factors that affected the implementation of e-health by private healthcare providers. The identified factors included IT-related costs, the readiness of private dental care providers to embrace technology, adequate expertise, and communication. Most participants were concerned about the confidentiality of personal health information, as any breach would result in privacy violations and loss of personal data. Factor analysis determined the factors that impacted the implementation of e-health. A regression analysis revealed that perceptions and attitudes of dental care providers had a statistically significant positive impact on the performance of e-health.
The study recommends that private dental service providers establish online links and dental user applications that can be uploaded on mobile devices, thereby increasing access by poor communities. Another recommendation is that policymakers in the health service sector include ICT programs for tertiary institutions offering health education, where students are exposed to real-world practical applications.
The study shows the need for the health services delivery system in Zimbabwe and private dental services providers to embrace technology and implement e-health systems. Through the finding of this study, private dental care providers in Zimbabwe have a better view through empirical evidence of the status of e-health. This will spur interest and heighten the adoption and implementation of e-health systems. This has the advantage of aligning the health services delivery in Zimbabwe with global standards. Consequently, this positively impacts the quality of health services delivery in Zimbabwe, an area in its infancy.
Список литературы E-health Implementation by Private Dental Service Providers in Bulawayo, Zimbabwe
- R. Wyber, S. Vaillancourt, W. Perry, P. Mannava, T. Folaranmi and L. Celi, “Big data in global health: improving health in low-and middle-income countries,” Bulletin of the World Health Organization, vol. 93, pp. 203-208, 2015.
- V. Maphosa, “COVID-19 and the Digital Ecosystem: Using a Mobile App to Connect a Rural Community,” Aquademia, vol. 5, no. 1, pp. ep21002, 2021. https://doi.org/10.21601/aquademia/9580
- V. Maphosa, T. Jita and B. Dube, “Students’ perception and use of Moodle as the E-Learning system implemented at a rural University in Zimbabwe,” In Proceedings of EdMedia + Innovate Learning, The Netherlands: Association for the Advancement of Computing in Education (AACE), pp. 175-182, 2020.
- M. Luca, L. Mustea, A. Taran, P. Stefea and S. Vatavu,” Challenges on radical health redesign to reconfigure the level of e-health adoption in EU countries,” Frontiers in public health, vol. 1047, pp. 1-16, 2021. doi:10.3389/fpubh.2021.728287
- B. Popovic and M. Maksimovic, M, “E-health in Bosnia and Herzegovina: exploring the challenges of widespread adoption,” CMBEBIH 2017. IFMBE Proceedings. vol. 62, pp. 388–95, 2017. doi:10.1007/978-981-10-4166-2_60
- M. Gagnon, F. Légaré, M. Labrecque, P. Frémont, P. Pluye, J. Gagnon, and K. Gravel, “Interventions for promoting information and communication technologies adoption in healthcare professionals,” Cochrane database of systematic reviews, vol. 1, pp. 1-25, 2009. doi:10.1002/14651858.CD006093.pub2.
- D. Nzuki, and D. Mugo, “Determinants of electronic health in developing countries,” International Journal of Arts and Commerce, vol. 3, no. 3, pp. 49–60, 2014.
- L.Busagala and G. Kawono, “Underlying challenges of e-health adoption in Tanzania. International Journal of Information and Communication Technology Research,” vol. 3, no. 1, pp. 34–41, 2013. doi:10.1.1.301.1188
- Q. Qureshi and B. Shah, “Infrastructural barriers to e-health implementation in developing countries,” European Journal of Sustainable Development, vol. 2, no. 1, 163–170, 2013.
- V. Vimarlund, N. Olve, I. Scandurra and S. Koch,” Organisational effects of information and communication technology (ICT) in elderly homecare: a case study,” Health Informatics Journal, vol. 14, no. 3, pp. 195-210, 2018. doi:10.1177/1081180X08092830
- G. Iyawa, M. Herselman and A. Botha, “Digital Health Innovation Ecosystems: From Systematic Literature to Conceptual Framework,” ProcediaComputerScience, vol. 100, pp. 244-252, 2016. doi:10.1016/j.procs.2016.09.149
- J. Rowley, “An analysis of the e‐service literature: towards a research agenda,” Internet research, vol. 16, no. 3, pp. 339-359, 2006. doi:10.1108/10662240610673736
- V. Maphosa, “Promoting access to COVID-19 information by underserved communities through the development of a mHealth app,” Cogent Public Health, vol. 9, no. 1, pp. 1-10, 2022. doi:10.1080/27707571.2022.2095722
- S. Furusa and A. Coleman, “Factors influencing e-health implementation by medical doctors in public hospitals in Zimbabwe, “South African Journal of Information Management, vol. 20, no. 1, pp. 1-9, 2018
- WHO, “Global strategy on digital health 2020-2025,” World Health Organization, Geneva, 2021.
- mohcc, “MoHCC Digitizing the Health Space,” 10 December 2020. [Online]. Available: http://www.mohcc.gov.zw/index.php?option=com_content&view=article&id=349:mohcc-digitizing-the-health-space&catid=84&Itemid=435.
- P. Allaire, J. Augat, J. Jose and D. Merrill, “Reducing Costs and Risks for Data Migrations”. Santa Clara, CA, USA, vol. 31, pp. 1-26, 2010. https://www.hitachivantara.com/go/virtualizetoday/pdf/white-paper-reducing-costs-and-risks-for-data-migrations.pdf
- S. Edirippulige, R. Marasinghe, V, Dissanayake, P. Abeykoon and R. Wootton, “Strategies to promote e-health and telemedicine activities in developing countries,” In telehealth in the developing world, CRC Press, pp.79-87.
- J. Blaya, H. Fraser and B. Holt, B, “eHealth technologies show promise in developing countries,” Health Affairs, vol. 29, no. 2, pp. 244-25, 2010. doi:10.1377/hlthaff.2009.0894.
- V. Omachonu and N. Einspruch, “Innovation in healthcare delivery systems: a conceptual framework,” The Innovation Journal: The Public Sector Innovation Journal, vol. 15, no. 1, pp. 1-20, 2010.
- P. Varkey, A. Horne, K. Bennet, “Innovation in health care: a primer,” American Journal of Medical Quality, vol. 23, no. 5, pp. 382-388, 2008. doi:10.1177/1062860608317695
- M. Toivonen, M and T. Tuominen, “Emergence of innovations in services,” The Service Industries Journal, vol. 29, no. 7, pp. 887-902, 2009. doi:10.1080/02642060902749492
- C. Huston, “The Impact of Emerging Technology on Nursing Care: Warp Speed Ahead. OJIN,” The Online Journal of Issues in Nursing, vol. 18, no. 2, pp. 1- 11, 2013. doi:10.3912/OJIN.Vol18No02Man01
- W. Wang, L. Sun, T. Liu and T. Lai, “The use of E-health during the COVID-19 pandemic: a case study in China’s Hubei province, “Health Sociology Review, pp. 1-17, 2021. doi:10.1080/14461242.2021.1941184
- B. Kusumasari, W. Setianto and L. Pang, “A study on digital democracy practice: Opportunities and challenges of e-Health implementation in Indonesia,” Jurnal Ilmu Sosial Dan Ilmu Politik, vol. 22, no. 1, pp 1-16, 2018. doi:10.22146/jsp.28863
- P. Wicks, J. Stamford, M. Grootenhuis, L. Haverman and S. Ahmed, “Innovations in e-health,” Quality of Life Research, vol. 2, no.1, pp. 195-203, 2014. doi:10.1007/s11136-013-0458-x
- O. Obe and F. Akinloye, “Integration of Emotional Assessment into E-Health Care Delivery: For Autism Spectrum Disorder: A Review,” Health Sciences Research Journal, vol. 4, no. 6, 45-56, 2017. .http://www.aascit.org/journal/hsr
- L. Catwell and A. Sheikh, “Evaluating eHealth interventions: The need for continuous systemic evaluation,” PLoS Medicine vol. 6, no. 8, pp. 1–6, 2009
- L. Alpay, O. Henkemans, W. Otten, T. Rovekamp and A. Dumay, “E-Health applications and services for patient empowerment: directions for best practices in The Netherlands,” Telemedicine and E-Health, vol. 16, no. 7, pp. 787-791, 2010. doi:10.1089/tmj.2009.0156
- N. Menachemi and T. Collum, “Benefits and drawbacks of electronic health record systems,” Risk management and healthcare policy, vol. 4, pp. 47-55, 2011. doi:10.2147/RMHP.S12985
- D. Balfour, S. Evans, J. Januska, H. Lee, S. Lewis, S. Nolan, M. Noga, C. Stemple and K. Thapar, “Health information technology results from a roundtable discussion. Journal of Managed Care Pharmacy, vol. 15, no. 1, pp. 10-17, 2009. doi:10.18553/jmcp.2009.15.s6-b.10.
- Z. Lewis, C. Mello-Thoms, O. Gadabu, E. Gillespie and R. Crowley, “The feasibility of automating audit and feedback for ART guideline adherence in Malawi,” J Med Inform Assoc, vol. 18, no. 6, pp. 868-874, 2011. doi:10.1136/amiajnl-2011-000097
- J. Barbera, N. Naibert, R. Komperda and T. Pentecost, “Clarity on Cronbach’s Alpha Use,” Journal of Chemical Education, vol. 98, no. 2, pp. 257-258, 2021. doi:10.1021/acs.jchemed.0c00183
- V. Minichiello, S. Rahman, A. Dune, J. Scott and G. Dowsett, G, “E-health: potential benefits and challenges in providing and accessing sexual health services,” BMC Public Health, vol. 13, no. 790, pp. 1-7, 2014. doi: 10.1186/1471-2458-13-790
- V. Maphosa and M. Maphosa, “Factors Influencing the Adoption of ICT for Remote Work Among Zimbabwean SMEs: A Case Study of Bulawayo Metropolitan Province,” International Journal of Advanced and Applied Sciences, vol. 9, no. 3, pp. 150-158, 2022. doi.org/10.21833/ijaas.2022.03.017
- D. Arduini, D and A. Zanfei, “An overview of scholarly research on public e-services? A meta-analysis of the literature,” Telecommunications Policy, vol. 38, no. 5-6), pp. 476-495, 2014. doi:10.1016/j.telpol.2013.10.007
- M. Putteeraj, N. Bhungee, J. Somanah and N. Moty, “Assessing E-Health adoption readiness using diffusion of innovation theory and the role mediated by each adopter’s category in a Mauritian context,” International Health, vol. 14, no. 3, pp. 236-249, 2022. doi:10.1093/inthealth/ihab035
- M. Mason, “Sample size and saturation in PhD studies using qualitative interviews. In Forum Qualitative Sozialforschung/Forum,” Qualitative social research, vol. 11, no. 3, pp. 1-19, 2010.