Effect of liraglutide dose on efficacy of correcting microcirculatory disorders in absolute insulin deficiency of albino rats
Автор: Daria D. Lagutina, Tatyana V. Stepanova, Angelina A. Savkina, Alexey N. Ivanov
Журнал: Saratov Medical Journal @sarmj
Статья в выпуске: 3 Vol.2, 2021 года.
Бесплатный доступ
The objective was to study the dose-dependent effects of glucagon-like peptide-1 receptor agonist, liraglutide, on microcirculation in white rats under the alloxan-induced insulin deficiency. Materials and Methods. Our study was carried out on 70 white rats, divided into four groups: 20 intact control animals; 20 animals of the comparison group with alloxan-induced diabetes; 10 animals with insulin deficiency, injected with liraglutide at a dose of 0.2 mg/kg per day (treatment group No. 1); and 20 animals with insulin deficiency treated with liraglutide at a dose of 0.4 mg/kg per day (treatment group No. 2). Diabetic status, skin perfusion of the posterior limb and mechanisms of blood flow modulation were assessed in all groups of animals. Results. It was established that administering liraglutide at a dose of 0.4 mg/kg per day allowed achieving complete normalization of carbohydrate metabolism in rats with alloxan-induced insulin deficiency, thereby more effectively improving the state of microcirculation, compared with a dose of 0.2 mg/kg per day. Conclusion. The efficacy of correcting the microcirculatory disorders with liraglutide correlates with correcting the carbohydrate metabolism in rats with insulin deficiency and depends on liraglutide dose. The dose-dependent effect is achieved by the endothelial mechanism of flow modulation in microcirculation. However, the restoration of the vascular tone neurogenic component is independent of liraglutide dose.
Diabetes mellitus, microcirculation, liraglutide, endothelial dysfunction, angiopathy
Короткий адрес: https://sciup.org/149139009
IDR: 149139009 | DOI: 10.15275/sarmj.2021.0304
Текст научной статьи Effect of liraglutide dose on efficacy of correcting microcirculatory disorders in absolute insulin deficiency of albino rats
Currently, an unprecedented increase in the incidence of diabetes mellitus, as well as associated vascular complications, is observed all over the world [1]. Micro- and macroangiopathy are among major causes of disability and mortality in diabetes mellitus, the development of which, as a rule, begins with damage to the vessels of the microvasculature [2]. This is due to the substantial role of diabetes mellitus in providing transcapillary exchange [3]. As a result of circulatory disorders at the level of microcirculation, trophic disorders occur with the involvement of large vessels and nerve trunks in the pathological process, which leads to impaired vascular innervation and progression of complications [4].
It is known that one of the key risk factors for the development of vascular complications in diabetes mellitus is endothelial dysfunction occurring under the influence of chronic hyperglycemia, dyslipidemia, and oxidative stress [5]. This defines the endothelium as one of the therapeutic targets in the treatment of patients with diabetes mellitus. Of particular importance is the effective correction of microcirculatory disorders in patients with type I diabetes, accompanied by absolute insulin deficiency. This is due to the fact that correction of hyperglycemia in this category of patients is carried out by insulin replacement therapy, which has a negative effect on endothelium-dependent vascular dilatation, thereby contributing to the development of endothelial dysfunction and, consequently, to the progression of microcirculatory disorders [6]. That is why it is advisable to study the vasoprotective properties of alternative hypoglycemic drugs, in particular, incretin analogs, such as glucagon-like peptide-1 (GLP-1), which have an insulinindependent mechanism of action in patients with type I diabetes mellitus.
Currently, liraglutide has been proven to be highly effective in correcting the glycemic profile in the treatment of patients with type II diabetes mellitus [7]. At the same time, some authors have shown positive effects of liraglutide in treating type I diabetes mellitus, such as a decrease in the level of glycated hemoglobin, glucose concentration, body weight, and the need for insulin in patients [8]. In addition, there is some evidence that liraglutide has a direct vasoprotective effect, preventing the development of endothelial dysfunction in type II diabetes mellitus [9].
Considering the leading positions of vascular complications in the structure of disability and mortality in patients with diabetes mellitus, the key role of microcirculatory lesions as the initial stage in the
development of diabetic angiopathy, and the prospects for using liraglutide to improve the therapeutic correction of hyperglycemia, we conducted the study of its angiotropic effects and their dose-dependency.
Objective – to investigate the dose-dependent effects of glucagon-like peptide-1 receptor agonist, liraglutide, on microcirculation in white rats under the alloxan-induced insulin deficiency.
Materials and Methods
The experiment was performed on 70 white rats randomly distributed among the following groups: 1) control group of 20 intact animals; 2) comparison group of 20 animals with alloxan-induced insulin deficiency; 3) treatment group No. 1 with 10 animals that received 0.2 mg/kg per day of liraglutide against the background of experimental diabetes; 4) treatment group No. 2 with 20 animals that received liraglutide injections at a dosage of 0.4 mg/kg per day against the background of experimental diabetes. Animals were kept under standard vivarium conditions with natural lighting and free access to water and food. The conducted studies complied with the provisions of the European Convention for the Protection of Vertebrate Animals, the requirements of the national guidelines for the maintenance and care of laboratory animals, and were approved by the Ethics Committee of Saratov State Medical University (Protocol No. 1 of February 5, 2019). Experimental insulin deficiency in animals was simulated by subcutaneous administration of a 5% solution of alloxan in a 0.9% solution of NaCl at a rate of 100 mg/kg of animal body weight [10].
An analysis of current publications shows the possibility of using two dosage options of liraglutide in rats, 0.2 and 0.4 mg/kg/ per day [11]. Hence, the correction of carbohydrate metabolism and microcirculation disorders was carried out by subcutaneous administration of liraglutide from day 21 through day 42 of the experiment in dosages of 0.2 and 0.4 mg/kg per day.
The severity of carbohydrate metabolism disorders in rats of the intact group, comparison group, and treatment groups was assessed by the blood glucose level determined on an empty stomach by the Accu-Chek Performa Nano portable glucometer (Roche Diagnostics, Switzerland), and by the concentration of HbA1c in the blood using reagents from Diagnostic Systems GmbH (Germany) on a Sapphire 400 analyzer (Hirose Electronic System, Japan).
To study the microcirculation parameters, the Laser Doppler flowmetry (LDF) method was used using the LAKK-OP analyzer (Scientific Industrial Enterprise Lazma, Russia). LDF imaging was carried out on day 42 of the experiment in all groups of animals on the foot dorsum skin. The perfusion index was calculated in perfusion units. Wavelet analysis was used to identify the normalized amplitudes of endothelial, neurogenic, myogenic, respiratory, and cardiac fluctuations.
The obtained experimental data were statistically processed using the Statistica 10 software (StatSoft, USA). The data were checked for normality of the distribution using the Shapiro-Wilk test. Most of the collected data did not comply with the law of normal distribution. Accordingly, the median (Me), along with upper and lower quartiles (Q1; Q3) were calculated, and nonparametric Mann-Whitney U test was employed for intergroup comparisons. The critical level of p when testing statistical hypotheses was considered at the level of 0.05.
Results
We established conducted a significant increase in fasting glucose and glycated hemoglobin concentrations in animals of the comparison group vs. control animals, which verified the development of alloxan-induced diabetes ( Figure 1 ).
In animals of the treatment group No. 1, liraglutide, used at a dose of 0.2 mg/kg per day for 21 days (from day 21 through day 42 of the experiment), significantly reduced the level of fasting blood glucose by 52% relative to the comparison group; however, the values remained higher than the control values. The concentration of glycated hemoglobin in the blood of the treatment group 1 rats on day 42 of the experiment was 23% lower than in the rats of the comparison group, but 28% higher than in control animals.
The level of fasting blood glucose on day 42 of the experiment in animals of the treatment group No. 2, which were administered liraglutide at a dose of 0.4 mg/kg per day, was three times lower relative to the values of the comparison group and had no statistically significant difference with the control group. The concentration of glycated hemoglobin in these animals on day 42 of the experiment was 53% lower than in rats with alloxan-induced diabetes, and did not differ statistically significantly from the control rats.
When comparing the two treatment groups against each other, we discovered that when the drug was administered at a dosage of 0.4 mg/kg per day, the fasting glucose level on day 42 day of the experiment was 30% lower than at a dosage of 0.2 mg/kg per day. At the same time, the concentration of glycated hemoglobin was also significantly lower than the values of the group with a lower dosage of liraglutide.
Hence, we conclude that the introduction of liraglutide to white rats with absolute insulin deficiency for 21 days at a dosage of 0.2 mg/kg per day led to partial normalization of carbohydrate metabolism. At the same time, an increase in the dose of liraglutide up to 0.4 mg/kg per day resulted a complete normalization of glucose and glycated hemoglobin levels in animals with alloxan-induced diabetes.
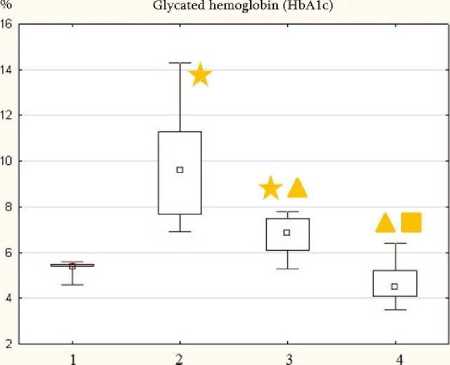
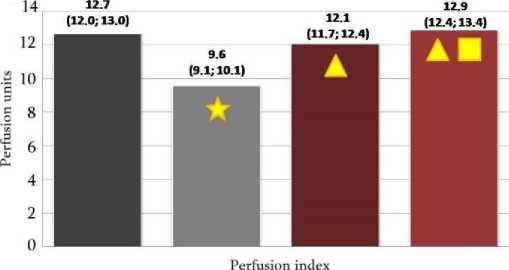
When assessing the state of the microcirculatory bed, we found that in the animals of the comparison group on day 42 of the experiment, a statistically significant decrease in perfusion index was observed, compared with the animals in the control group, indicating a reduction in tissue blood flow ( Figure 2 ).
In animals of the treatment group No. 1, with the introduction of liraglutide at a dose of 0.2 mg/kg per day against the background of insulin deficiency, an increase in perfusion index by 26% (p < 0.001) was observed relative to the comparison group by day 42 of the experiment. The perfusion index in this group did not have statistically significant differences with the values of the control group, which indicated an improvement in the state of the microcirculation.
Using the wavelet analysis of LDF images, we established that decrease in blood flow in the group of animals with alloxan-induced insulin deficiency was accompanied by redistribution of contributions on the part active mechanisms of microcirculation modulation. The normalized amplitudes of endothelial and neurogenic fluctuations on day 42 of the experiment were significantly lower than the control values. The values of myogenic fluctuation amplitude did not change statistically significantly ( Table ).
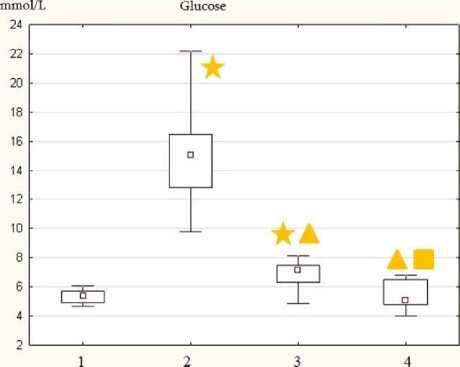
1 - Control
2 - Comparison group (DM)
3 - DM + 0.2 mg/kg per day of liraglutide
4 - DM + 0.4 mg/kg per day of liraglutide
□ Median
□ 25%-75%
"T max and min
Figure 1. Changes in the indicators of carbohydrate metabolism in rats during the course administration of liraglutide against the background of absolute insulin deficiency
Statistically significant differences are indicated as follows: a star demotes, ‘compared with the control’; a triangle denotes, ‘compared with the comparison group’; a rectangle denotes, ‘compared with a dosage of 0.2 mg/kg per day’; DM – diabetes mellitus.
-
■ Control ■ Comparison group (DM)
-
■ DM * 0.2 mg/kg per day of liraglutide В DM * 0 4 mg/kg per day of liraglutide
Figure 2. Changes in perfusion of foot dorsum skin in rats with a course of administration of liraglutide against the background of absolute insulin deficiency
Statistically significant differences are indicated as follows: a star demotes, ‘compared with the control’; a triangle denotes, ‘compared with the comparison group’; a rectangle denotes, ‘compared with a dosage of 0.2 mg/kg per day’; DM – diabetes mellitus.
It was also established that the perfusion index restoration in animals of the treatment group No. 1, in which liraglutide was used at a dosage of 0.2 mg/kg per day, occurred mainly due to an increase in the amplitudes of endothelial fluctuations by 23.2% (p=0.438) in relation to comparison group. Neurogenic fluctuations using the indicated dosage did not differ statistically from the control group. Along with this finding, we also observed that the amplitude of endothelial fluctuations in animals of the treatment group No. 2 increased relative to the comparison group by 92.6% (p=0.001) when using liraglutide dosage of 0.4 mg/kg per day.
Table. Changes in normalized amplitudes of blood flow fluctuations in rats with the introduction of liraglutide against the background of experimental diabetes: Ме (Q25; Q75)
When comparing the treatment groups with each other, we revealed that when using liraglutide at a dosage of 0.4 mg/kg per day, the perfusion index of the foot dorsum skin in rats with alloxan-induced insulin deficiency was 7% (p=0.012) higher than when using liraglutide dosage of 0.2 mg/kg per day (Figure 2). At the same time, the amplitudes of endothelial fluctuations were also statistically significantly higher in the group of animals with a higher dosage of the drug, and the amplitudes of neurogenic fluctuations did not have a significant difference between the treatment groups with different dosages of liraglutide (Table).
Thus, the obtained data confirmed that the course administration of liraglutide from day 21 of the experiment at a dosage of 0.2 mg/kg per day significantly improved the perfusion of the foot dorsum skin mainly due to stimulation of endothelium-dependent vasodilation and a decrease in the neurogenic tone of the precapillary link of the microcirculation. The course administration of liraglutide at a dosage of 0.4 mg/kg per day was the most effective for correcting the development of microcirculatory disorders in white rats with alloxan-induced diabetes, which was manifested by a greater degree of increase in the foot dorsum skin perfusion and endothelium-dependent vasodilation, compared with the course of administration of a lower dose.
Discussion
During the experiment, using LDF, we discovered that the introduction of alloxan led to a statistically significant decrease in the perfusion index, as well as the normalized amplitudes of endothelial and neurogenic fluctuations on day 42 of the experiment. This was consistent with the data of previous studies, indicating that the reduction of tissue blood flow in alloxan-induced insulin deficiency was associated with a decrease in endothelium-dependent vasodilation and an increase in neurogenic tone [12].
The integrity and function of the endothelium is critical for tonic regulation of blood flow, primarily through the release of vasoconstrictor and vasodilator factors that change the lumen of the vessels, which determines the local vascular tone in each segment. Disorder of endothelium-dependent relaxation is a characteristic clinical feature of endothelial dysfunction, which was observed in experimental models of diabetes mellitus [13].
Chronic hyperglycemia imposes an altering effect on the endothelium, an important mechanism of which is the activation of protein kinase C, which launches multiple intracellular signaling mechanisms that cause an increase in permeability of the vascular wall and disorder of endothelium-dependent vascular dilatation, suppressing the activity of soluble guanylate cyclase, an enzyme, by which nitric oxide (NO) implements its effects, in particular, vasorelaxation [14]. It is worth noting that an important role in the pathogenesis of vascular complications of diabetes mellitus is played by the activation of oxidative stress: an imbalance of prooxidants and antioxidants, leading to the accumulation of highly toxic products of free radical oxidation, which, in turn, leads to the development and progression of endothelial dysfunction [15].
The results of clinical studies of liraglutide vasoprotective effect are currently demonstrated only in patients with type 2 diabetes mellitus and are not unambiguous. For instance, an improvement in endothelium-dependent vasodilation was found in patients with type II diabetes mellitus under the influence of liraglutide [9]. Data of other authors implied that liraglutide therapy did not significantly affect either coronary or peripheral microvascular function in patients with type II diabetes mellitus [16]. The inconsistency of published data necessitates further research into the nature and mechanisms of the vasoprotective effects of liraglutide in diabetes.
In vitro experiments have demonstrated certain biological effects resulting from the impact of GLP-1 on the vascular endothelium. Thus, the effect of liraglutide on endothelial © 2021, Saratov State Medical University, Saratov, Russia © 2021, LLC Innovative Medical Technologies, Saratov, Russia © 2021, LLC Science and Innovations, Saratov, Russia cells leads to an increase in NO production and a significant decrease in the level of oxidative stress [17]. The positive effects on the vascular endothelium were confirmed by in vivo studies. In particular, intravenous administration of native GLP-1 to male rats for 2 h was accompanied by a significant improvement in microcirculation, confirmed by ultrasound examination [18], which were indicative of the presence of a direct effect of incretins on vascular tone due to the induction of endothelium-dependent vasodilation. It should be noted that in a model of arterial hypertension in mice, glucagon-like peptide analogs lowered blood pressure and exerted an endothelium-protective effect, regardless of glycemia level [18]. Therefore, the positive effects of liraglutide on microcirculation, revealed in the course of our study, may be associated with the normalization of carbohydrate metabolism, which prevents further alteration of endothelial cells [17], or else – with direct endothelium-protective effect of liraglutide [18].
According to our results, the effect of liraglutide on microvasculature perfusion is dose-dependent. The dose dependence of liraglutide is also characteristic of the process of restoring the amplitude of endothelial fluctuations and is not characteristic of neurogenic fluctuations, which indicates the sensitivity of the mechanism of endothelium-dependent dilatation to the concentration of the GGP-1 analog in the bloodstream. It should be noted that an increase in the amplitude of endothelial fluctuations indicates an increase in the production of an endogenous vasodilator, nitric oxide, by endotheliocytes [19]. This may be due to the direct effect of liraglutide on endothelium-dependent dilatation (an increase in the direct dilating effect with increasing dose); on the other hand, a greater effect of a dosage of 0.4 mg/kg per day is associated with a complete normalization of carbohydrate metabolism, which suggests a pronounced reduction of endothelial alteration by hyperglycemia. Previously demonstrated results suggest that liraglutide at two doses, 0.2 and 0.4 mg/kg per day, increases the reduced concentration of nitric oxide metabolites in diabetic rats. This can be regarded as a restoration of the production of this vasodilator [11].
It was demonstrated that liraglutide in certain dosages can have different effects on carbohydrate metabolism and lipid profile. However, the authors did not find significant differences in the intensity of the increase in the serum concentration of NO metabolites in rats with diabetes mellitus using the indicated dosages. It should be noted that the concentration of NO metabolites in serum represents the net activity of different NO synthase isoforms and does not directly correlate with endothelium-dependent vasodilation. In particular, in diseases of the cardiovascular system, developing endothelial dysfunction is associated with an increase in the level of nitrites in the bloodstream due to the activity of the inducible form of NO synthase [20]. Hence, the presented results of this study clarify the nature of the response of the nitroxidergic system to administration of liraglutide, and show the dependence of the endothelial NO synthase isoform activation on the used dosage.
Conclusion
The results of our study allow us concluding that the course of administering liraglutide has caused the restoration of microcirculation in rats with alloxan-induced diabetes in a dose-dependent manner, increasing a perfusion of the foot dorsum skin relative to the comparison group by 26% when using a dose of 0.2 mg/kg, and by 34% whenever using a dose of 0.4 mg/kg per day. Normalization of microcirculation under the action of liraglutide was carried out by stimulating endothelium-dependent vasodilation and reducing the tone of the precapillary link in the microvasculature. The dependence of this effect on liraglutide dosage was explained by different intensity of endothelium-dependent vasodilation restoration. Meanwhile, the restoration of neurogenic tone was equally pronounced when using the indicated doses.
The obtained data, characterizing the endothelium-protective effects of liraglutide, confirmed the expediency of its use in patients with diabetes mellitus with the goal to prevent the development and progression of endothelial dysfunction.
Conflict of interest: None declared.Fundings
The study was conducted within the framework of the Public Procurement of V.I. Razumovsky State Medical University of Saratov, Ministry of Healthcare of Russia, “Development of Technologies for Medicamentous and NonMedicamentous Correction of Microcirculatory Disorders in Diabetes Mellitus Accompanied by Absolute Insulin Deficiency under Experimental Conditions” (registration No. АААА-А19-119021190053-0).
Список литературы Effect of liraglutide dose on efficacy of correcting microcirculatory disorders in absolute insulin deficiency of albino rats
- Dedov II, Shestakova MV, Vikulova OK. Epidemiology of diabetes mellitus in the Russian Federation: Clinical and statistical analysis based on the Federal Registry on Diabetes Mellitus. Diabetes Mellitus 2017; 20 (1): 13-41. [In Russ.]
- Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol 2018; 17 (1): 57. https://doi.org/10.1186/s12933-018-0703-2
- Dal Canto E, Ceriello A, Rydén L, et al. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol 2019; 26 (2): 25-32. https://doi.org/10.1177/2047487319878371
- Bjerg L, Hulman A, Carstensen B, et al. Effect of duration and burden of microvascular complications on mortality rate in type 1 diabetes: An observational clinical cohort study. Diabetologia 2019; 62 (4): 633-43.
- Knapp М, Tu X, Wu R. Vascular endothelial dysfunction, a major mediator in diabetic cardiomyopathy. Acta Pharmacol Sin 2019; 40 (1): 1-8. https://doi.org/10.1038/s41401-018-0042-6
- Arcaro G, Cretti A, Balzano S, et al. Insulin causes endothelial dysfunction in humans: Sites and mechanisms. Circulation 2002; (105): 576-82. https://doi.org/10.1161/hc0502.103333
- Zhang X, Shao F, Zhu L, et al. Cardiovascular and microvascular outcomes of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A meta-analysis of randomized controlled cardiovascular outcome trials with trial sequential analysis. BMC Pharmacol Toxicol 2018; 19 (1): 58. https://doi.org/10.1186/s40360-018-0246-x
- Dimitrios P, Michael D, Vasilios K. Liraglutide as adjunct to insulin treatment in patients with type 1 diabetes: A systematic review and meta-analysis. Curr Diabetes Rev 2020; 16 (4): 313‐26. https://doi.org/10.2174/1573399815666190614141918.
- Simanenkova AV, Makarova MN, Vasina LV, et al. Glucagon-like peptide-1 receptor agonist reduces endothelial dysfunction in type 2 diabetes patients. Regional Blood Circulation and Microcirculation 2018; 17 (2): 57-63. [In Russ.] https://doi.org/10.24884/1682-6655-2018-17-2-57-63
- Bukhtiyarova IP, Drogovoz SM, Shchekina EG. Investigation of hypoglycemic properties of raleukin on an alloxan diabetes model in rats. Bulletin of Kazakh National Medical University 2014; (4): 301-4. [In Russ.]
- Zhang Q, Xiao X, Zheng J, et al. Liraglutide protects cardiac function in diabetic rats through the PPARα. Biosci Rep 2018; 38 (2): BSR20180059. https://doi.org/10.1042/BSR20180059
- Ivanov AN, Antipova ON, Savkina AA, et al. Effect of liraglutide on microcirculation in rats with experimental diabetes mellitus associated with absolute insulin deficiency. Regional Blood Circulation and Microcirculation 2020; 19 (4): 61-9. [In Russ.] https://doi.org/10.24884/1682-6655-2020-19-4-61-69
- Sukumaran V, Tsuchimochi H, Sonobe T, et al. Liraglutide treatment improves the coronary microcirculation in insulin resistant Zucker obese rats on a high salt diet. Cardiovasc Diabetol 2020; (19): 24. https://doi.org/10.1186/s12933-020-01000-z
- Popykhova EB, Stepanova TV, Lagutina DD, et al. Role of diabetes in the onset and development of endothelial dysfunction. Problems of Endocrinology 2020; 66 (1): 47-55. [In Russ.] https://doi.org/10.14341/probl12212
- Dos Santos JM, Tewari S, Mendes RH. The role of oxidative stress in the development of diabetes mellitus and its complications. J Diabetes Res 2019; (5): 4189813. https://doi.org/10.1155/2019/4189813
- Faber R, Zander M, Pena A, et al. Effect of the glucagon-like peptide-1 analogue liraglutide on coronary microvascular function in patients with type 2 diabetes – A randomized, single-blinded, cross-over pilot study. Cardiovasc Diabetol 2015; (14): 41. https://doi.org/10.1186/s12933-015-0206-3
- Ishibashi Y, Matsui T, Takeuchi M, et al. Glucagon-like peptide-1 (GLP-1) inhibits advanced glycation end product (AGE)-induced upregulation of VCAM-1. Biochem Biophys Res Commun 2010; (391): 1405-8. https://doi.org/10.1016/j.bbrc.2009.12.075
- Chai W, Dong Z, Wang N, et al. Glucagon-like peptide 1 recruits microvasculature and increases glucose use in muscle via a nitric oxide-dependent mechanism. Diabetes 2012; (62): 888-96. https://doi.org/10.2337/db11-1073
- Krupatkin AI, Sidorov VV. Laser Doppler flowmetry of blood microcirculation: A physician’s guide. Moscow: Meditsina, 2005; 256 p. [In Russ.]
- Ivanov AN, Grechikhin AA, Norkin IA, et al. Methods of endothelial dysfunction diagnosis. Regional Blood Circulation and Microcirculation 2014; 13 (4): 4-11. [In Russ.] https://doi.org/10.24884/1682-6655-2014-13-4-4-11


