Features of microcirculatory responses in experimental wound area in white rats
Автор: Darya D. Loiko, Angelina A. Savkina, Tatyana V. Stepanova, Tatyana S. Kiriyazi, Oleg V. Osnovin, Tamara A. Andronova, Ilmira I. Abdrakhmanova, Artyom N. Fedorov, Aleksey N. Ivanov
Журнал: Saratov Medical Journal @sarmj
Статья в выпуске: 3 Vol.3, 2022 года.
Бесплатный доступ
Objective: to examine changes in the microcirculatory bed parameters via laser Doppler flowmetry in the course of wound healing and the possibility of their use for upgrading the technology of evaluating the effectiveness of wound healing agents. Materials and Methods. The studies were performed on 25 white rats distributed between two groups: 10 control animals (intact rats) and 15 animals with a full-thickness experimental skin defect. The microcirculation parameters in the skin of experimental wound edges in rats were evaluated using laser Doppler flowmetry, and histological preparations of tissues in the wound area were analyzed. Results. Changes in skin microcirculation at the wound edges were characterized by inflammatory hyperemia manifested by an increase in the perfusion index by 27% and augmented normalized amplitudes of myogenic, respiratory and cardiogenic oscillations. Changes in microcirculation were verified by the morphological picture of inflammation, which reflects an increase in the number of vessels fully filled with arterial and venous blood, as well as in leukocyte infiltration of the wound edges and bottom. Conclusion. Monitoring of microcirculatory disorders occurring in the area of skin wounds allows assessing the dynamics of the reparative process, which could be used for developing and evaluating the effectiveness of existing medicamentous and non-medicamentous methods of stimulating regeneration.
Microcirculation, regeneration, full-thickness skin wound
Короткий адрес: https://sciup.org/149146156
IDR: 149146156 | DOI: 10.15275/sarmj.2022.0303
Текст научной статьи Features of microcirculatory responses in experimental wound area in white rats
At present, the worldwide prevalence of acute and chronic wounds remains high. Various complications that may accompany the wound healing process, including infection, formation of hypertrophic scars and keloids, negative impact on the quality of life in patients and economics of the healthcare system caused by an increase in treatment duration and cost [1]. An important stage in the development of new products for wound care and treatment involves their in vivo testing, which determines the relevance of improving models and tools for evaluating the effects of innovative products.
According to current concepts, the wound healing process is a complex network of physiological changes, including responses of the damaged area microvessels [2, 3].
Microcirculatory responses in the wound area have a direct impact on the dynamics and intensity of skin wound repair, correcting the metabolic phases of the wound healing process [4]. Monitoring dynamics of the latter facilitates making a timely effective therapeutic decision, which has a significant impact on the final treatment outcome.
Currently, laser Doppler flowmetry is among the best modern non-invasive techniques that allow assessing the state of the microvasculature [5]. The novelty of the methodological approach implemented in the course of our study was the possibility of using laser Doppler flowmetry parameters for assessing the dynamics of reparative regeneration in skin wounds.
Consequently, the objective of our study was to examine the changes in the microcirculatory bed parameters via laser Doppler flowmetry during the wound healing and the possibility of their application for updating the technologies of evaluating the effectiveness of wound healing agents.
Materials and Methods
The experiment was performed on 25 white rats weighing 250–320 g distributed between two groups: the control group of 10 intact rats and the experimental group of 15 animals with a full-thickness experimental skin wound.
Throughout the experiment, the animals were kept in individual cages under standard vivarium conditions. For general anesthesia, they were administered Telazol (Zoetis Inc., Spain) at a dose of 0.1 mL/kg and Xylanit (Nita-Pharm LLC, Russia) at a dose of 1 mg/kg intramuscularly. All studies were performed in compliance with the European Convention for the Protection of Vertebrate Animals Used for
Experimental and Other Scientific Purposes (1986), national guidelines, and rules of the institution regarding the maintenance and use of laboratory animals. The studies were approved by the Ethics Committee of V.I. Razumovsky Saratov State Medical University (Protocol No. 1 of 5 February 2019).
The control group was formed to record the initial parameters of skin microcirculation in rats that were not treated with antiseptics.
Modeling of a full-thickness skin wound was performed by a surgical method [6]. To do so, after depilation and antiseptic treatment of the skin in the interscapular region, the contours of the future wound were drawn with 5% iodine on the experimental group animals using a square stencil. Then, using scalpel, a full-thickness wound 10×10 mm was formed.
To examine the state of microcirculation in the wound area, we employed the method of laser Doppler flowmetry, the implementation of which was performed using the LAKK-OP device (Russia). Measurement of microcirculation parameters in experimental animals was carried out on Day 14 of the experiment by placing the analyzer sensor at a distance of 1 mm from the upper edge of experimental wound. The perfusion index and normalized amplitudes of endothelial, neurogenic, myogenic, respiratory, and cardiogenic oscillations were assessed [7].
The withdrawal of animals from the experiment was conducted by an overdose of anesthetic agents. To evaluate the morphological changes occurring in the area of experimental full-thickness wound, the soft tissues of the wound were sampled on Day 14 of the experiment and fixed in a 10% formalin solution for further histological examination. Histological sections 5 µm thick were stained with hematoxylin and eosin (Biovitrum LLC, Russia). Microscopy of the wound area preparations was performed via a transmitted light microvisor of the μVizo-103 series (LOMO PHOTONIKA LLC, Russia). We then assessed the condition and blood filling of the microvasculature, along with the infiltration of the wound bottom and its perifocal zone with cellular elements involved in the implementation of the wound healing process, such as fibroblasts, lymphocytes, and macrophages.
Statistical processing of collected data was carried out using the Statistica version 10 software. Our data did not comply with the laws of normal distribution; hence, they are presented in the Table as a median (Me) and an interquartile range (Q25; Q75). Intergroup comparisons were performed using the Mann-Whitney test. Statistical significance was assumed at p<0.05.
Results
On Day 14 of the experiment, the experimental group rats exhibited a reduction in the wound area to 6.3 (5; 30) mm2 (i.e., 95% decrease from the initial value).
When assessing microcirculatory disorders in the fullthickness skin wound area on Day 14 of the experiment, we established that the perfusion index of the skin at the wound edge was statistically significantly higher in experimental group rats vs. the control animals by 27%. An increase in perfusion in this group was accompanied by a redistribution of contributions of active and passive mechanisms of microcirculation modulation. When evaluating the active mechanisms of modulation, we revealed a statistically significant decline in the normalized amplitudes of endothelial oscillations by 65% relative to the control and 58% increase in the normalized amplitudes of myogenic oscillations vs. the control. After two weeks, we did not detect statistically significant changes in the normalized amplitudes of neurogenic fluctuations in skin perfusion at the wound edge in experimental rats. It was established that large contribution to the change in microcirculatory responses of the skin at the wound edge was made by passive mechanisms of blood flow modulation. This was manifested by statistically significant 61% increase in the normalized amplitudes of respiratory oscillations and 4.9-fold increase in the normalized amplitudes of cardiogenic oscillations vs. the control values (Table).
A morphological study of the wound area preparations showed that the connective tissue of the perifocal zone was rich in blood vessels of both arterial and venous bed ( Figure A, B ). Their plethora was noted ( Figure B ), along with sludge and blood separation in some vessels ( Figure C ). When analyzing the cell populations of the skin wound area, we established that the predominant cell population was fibroblasts. We also observed a pronounced lymphocytic infiltration and single siderophages. The wound edges and bottom were infiltrated with neutrophils (Figure D ).
Discussion
Our experimental results on regeneration rate of a fullthickness skin wound were consistent with the published data on the matter indicating that the skin wound in rats was epithelialized by more than 90% by Day 14 of the experiment [8]. At the same time, the results of our study confirmed that the skin wound healing in rats of the experimental group was accompanied by pronounced changes in microcirculation, manifested by an increase in perfusion at the wound edges, as well as by the change in contributions of active and passive mechanisms to the regulation of circulation. The outcome matched the data of other authors who demonstrated the activation of collateral circulation in the full-layer skin wound model [3].
The revealed features of microcirculatory responses corresponded to the morphological changes occurring in the wound area. For instance, an increase in perfusion at the edges of the skin wound was consistent with the presence of a large number of blood vessels along the periphery of the wound. Besides, we observed their pronounced blood filling, which led directly to an increase in the perfusion index.
Enlarged contribution of passive mechanisms to the microcirculation modulation at the wound edges in experimental rats on Day 14, manifested by an increase in both cardiogenic and respiratory oscillations detected by laser Doppler imaging, implied a blood inflow surge and outflow obstruction in the microvasculature [9]. This confirms the visualized plethora of blood vessels in both arterial and venous beds. The presence of sludge and separation of blood in individual venules pointed to a sharp reduction in blood outflow, which was probably one of the causes of a pronounced increase in the contribution of respiratory oscillations to the modulation of blood flow in the skin microvasculature at the wound edges.
Table. Changes in microcirculation parameters in the skin wound area , Ме (Q 25 ; Q 75 )
|
Parameters |
Groups |
|
|
Control ( n =10) |
Experimental ( n =15) |
|
|
Perfusion index, perfusion units |
10.4 (9.6; 12.3) |
13.2 (11.3; 14.1) р =0.015 |
|
Oscillation amplitude, procedure defined units (p.d.u.) |
||
|
endothelial |
15.2 (11.5; 17.7) |
5.3 (4.04; 6.1) р <0.001 |
|
neurogenic |
6.8 (6.7; 8.2) |
6.7 (5.4; 7.5) р =0.157 |
|
myogenic |
6.7 (5.9; 7.9) |
10.6 (7.3; 11.6) р <0.001 |
|
respiratory |
9.1 (7.9; 11.6) |
14.7 (12.5; 18.8) р <0.001 |
|
cardiogenic |
3.8 (3.3; 4.7) |
18.6 (16.4; 20.1) р <0.001 |
In each case, the median and interquartile range are given; p -values for comparisons vs. the control
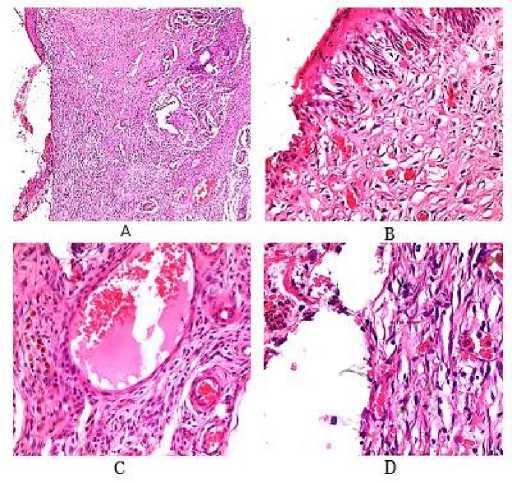
Figure. Morphological changes in the skin wound area (stained with hematoxylin and eosin): A – wound area of the skin (magnification ×5); B – vascular plethora in the perifocal zone, lymphocytic infiltration (magnification ×20); C – blood sludging and separation, lymphocytic infiltration, and siderophages in the perifocal zone (magnification ×40); D – neutrophil infiltration of the wound edge (magnification ×40)
Effective wound healing and formation of granulation tissue is impossible without angiogenesis. Under specific physiological and pathological conditions, the process of new blood vessel formation is regulated by various biologically active substances, among which a special role is given to cytokines and growth factors. According to the published data, neutrophils are the first to migrate to the wound area. They are capable of synthesizing and releasing a wide range of cytokines and pro-angiogenic factors, such as VEGF,
TNFα, IL-1β and IL-8, directly or indirectly promoting the growth and migration of endothelial cells, thereby helping the formation of new blood vessels [10]. At the same time, other cells of the leukocyte series, in particular, lymphocytes, as well as tissue macrophages and proliferating fibroblasts, can also be sources of cytokines and growth factors affecting angiogenic reactions [11]. The presence of previously mentioned cell populations, including neutrophils, macrophages, lymphocytes, and fibroblasts, in the experimental wound area and their production of regulatory molecules could explain the revealed changes in microcirculation. In particular, the decrease in myogenic vascular tone found in our study, accompanied by an increase in the normalized amplitudes of myogenic fluctuations, may be associated with the production of various pro-inflammatory cytokines by leukocytes present in large numbers in the tissues of the wound area. In addition, local acidosis and tissue hypoxia develop in the inflammatory focus, which, in turn, leads to a decrease in myogenic tone and dilatation of precapillary sphincters, resulting in increased amplitudes of myogenic fluctuations [9].
Conclusion
Features of microcirculation in the experimental wound area identified via laser Doppler flowmetry corresponds to the morphological characteristics of the wound healing process dynamics. Monitoring of microcirculatory disorders occurring in the skin wound area allows non-invasive assessment of the reparative process dynamics, which could be used for the pathogenetic development and evaluation of the effectiveness of existing medicamentous and nonmedicamentous methods of stimulating regeneration.
Conflict of interest: None declared by the authors. The study was carried out within the framework of the Public Procurement to V.I. Razumovsky Saratov State Medical University of the Russian Federation Ministry of Healthcare, “Development of Microchamber Wound Dressings Providing Local Modulation of Oxidative Homeostasis in Tissues.”
Список литературы Features of microcirculatory responses in experimental wound area in white rats
- Sen CK. Human wound and its burden: Updated 2020 compendium of estimates. Adv Wound Care (New Rochelle) 2021; 10 (5): 281–92. https://doi.org/10.1089/wound.2021.0026
- Haller HL, Sander F, Popp D, et al. Oxygen, pH, lactate, and metabolism—How old knowledge and new insights might be combined for new wound treatment. Medicina (Kaunas) 2021; 57 (11): 1190. https://doi.org/10.3390/medicina57111190
- Yousefi S, Qin J, Dziennis S, et al. Assessment of microcirculation dynamics during cutaneous wound healing phases in vivo using optical microangiography. J Biomed Opt 2014; 19 (7): 76015. https://doi.org/10.1117/1.JBO.19.7.076015
- Sоrensen MA, Petersen LJ, Bundgaard L, et al. Regional disturbances in blood flow and metabolism in equine limb wound healing with formation of exuberant granulation tissue. Wound Repair Regen 2014; 22 (5): 647–53. https://doi.org/10.1111/wrr.12207
- Kulikov DA, Glazkov AA, Kovaleva YuA. et al. Prospects for the use of laser Doppler flowmetry application in assessment of skin microcirculation in diabetes mellitus. Diabetes Mellitus 2017; 20 (4): 279–85. [In Russ.] https://doi.org/10.14341/DM8014
- Smotrin SM, Dovnar RI, Vasilkov AYu, et al. Effect of a dressing containing gold or silver nanoparticles on experimental wound healing. Journal of Grodno State Medical University 2012; 1 (37): 75–80. [In Russ.]
- Humeau A, Koïtka A, Abraham P, et al. Time-frequency analysis of laser Doppler flowmetry signals recorded in response to a progressive pressure applied locally on anaesthetized healthy rats. Phys Med Biol 2004; 49 (5): 843–57. https://doi.org/10.1088/0031-9155/49/5/014
- Bi H, Feng T, Li B, et al. In vitro and in vivo comparison study of electrospun pla and pla/pva/sa fiber membranes for wound healing. Polymers (Basel) 2020; 12 (4): 839. https://doi.org/10.3390/polym12040839
- Krupatkin AI. Blood flow oscillations as a new diagnostic language in the study of microcirculation. Regional Blood Circulation and Microcirculation 2014; 13 (1): 83–99. Russian https://doi.org/10.24884/1682-6655-2014-13-1-83-99
- Tecchio C, Cassatella MA. Neutrophil-derived cytokines involved in physiological and pathological angiogenesis. Chem Immunol Allergy 2014; (99): 123–37. https://doi.org/10.1159/000353358
- Wang Z, Qi F, Luo H, Xu G, et al. Inflammatory microenvironment of skin wounds. Front Immunol 2022; (13): 789274. https://doi.org/10.3389/fimmu.2022.789274


