Healthcare Access and Quality for Older Adults as a Special Socio-demographic Group
Автор: Kalashnikov K.N.
Журнал: Economic and Social Changes: Facts, Trends, Forecast @volnc-esc-en
Рубрика: Social and economic development
Статья в выпуске: 2 т.18, 2025 года.
Бесплатный доступ
The article considers healthcare access and quality for older adults in modern Russia. Based on literature sources and sociological research data, we substantiate the high level and special nature of the needs of older people in medical care. The aim of the work is to assess healthcare access and quality for older adults in the Vologda Region in comparison with other age groups, as well as in the context of the private and public health sectors. The information base includes data from sociological surveys of Vologda Region population collected during 2018-2024, which provided an opportunity to track the dynamics of respondents’ opinions, including in the context of the COVID-19 pandemic. Healthcare access and quality are assessed by appropriate indices, which helps to interpret the data using graphical visualization of results in a two-dimensional assessment field. Based on the analysis, we identify the conjugation and dichotomy between the parameters of healthcare access and quality, reflecting common features, as well as significant differences, for various age groups. The practical value and special relevance of the results obtained is due to their correlation with the practices of healthcare commercialization, the division of respondents’ assessments between public and private medical organizations. The novelty of the study consists in testing an alternative methodological approach to assessing healthcare access and quality, identifying age differences and the specifics of elderly patients’ response to changes in healthcare in the context of the COVID-19 pandemic.
Older adults, healthcare access, healthcare quality, healthcare, public sector, private sector, vologda region
Короткий адрес: https://sciup.org/147251356
IDR: 147251356 | УДК: 614.2 | DOI: 10.15838/esc.2025.2.98.10
Текст научной статьи Healthcare Access and Quality for Older Adults as a Special Socio-demographic Group
The research was supported by Russian Science Foundation grant 23-78-10128, project/23-78-10128/.
In the first quarter of the 21st century, many of the concerns expressed earlier and related to the dynamics of the world’s population were confirmed, but new major epidemiological challenges emerged, and humanity will have to respond to them in the coming decades (Fulmer et al., 2021). Thus, the predicted trend of population aging may lead to even greater than expected negative implications for society and the economy if it is accompanied by the emergence of such serious threats as the COVID-19 pandemic (Grigoryeva, Bogdanova, 2020).
The problems of the older generation are becoming particularly relevant in this context. Although the rights of the elderly population to decent living conditions do not differ from those of other socio-demographic groups, older adults require careful and sensitive treatment due to their physiological, psychological and other characteristics (Fedin et al., 2020). This is especially true in the field of healthcare. In one of the recently published papers on this issue, barriers to healthcare access care have been identified, which can be divided into common ones for all age categories (lack of necessary specialists, inconvenient opening hours, the need to pay for individual procedures) and specific ones that create difficulties in visiting medical institutions specifically for the elderly and people with disabilities. (lack of facilities in the polyclinic for people with walkers and wheelchairs) (Chukavina et al., 2024).
Older age is characterized by an increased risk of developing diseases of the cardiovascular system, neoplasms, decreased body resistance to infections, and other related limitations. Physical and psychological vulnerability are specific characteristics of this age group, and the organization of wide access to adequate medical care for its representatives is an important point in the system of achieving a healthy or prosperous old age (Zemlyanova, 2024; Belekhova et al., 2024). In this regard, both medical care as a social resource and the material objects that are the source of its receiving (for example, polyclinic buildings) are considered from the standpoint of material gerontology as important attributes of everyday life and the environment (Galkin, 2021). Currently, all countries face serious challenges in ensuring a timely and proportionate response to the growing needs of the elderly population for medical care and long-term care. There should be two basic indicators of the effectiveness of healthcare systems: healthcare access, reflecting the very possibility of receiving it, and healthcare quality, characterizing the qualifications of medical personnel and the effectiveness of the care provided, its compliance with the advanced achievements of medical science.
At the same time, monitoring healthcare access and quality at the level of organizations and territories faces a number of difficult methodological and instrumental problems. The most important of them concerns the ambiguity of the content and understanding of the categories under discussion. These terms are often accepted as synonymous, but it is not uncommon for them to be considered as elements of each other. Moreover, there is reason to assume that an approach to interpreting healthcare access and quality based on their opposition will have the greatest analytical value. It was used in this article. For this purpose, a toolkit for assessing healthcare access and quality in the regional dimension has been developed and tested. The aim of the work is to analyze subjective assessments of healthcare access and quality by elderly residents of the region as a social group characterized by a high need for these benefits and a particular sensitivity to their scarcity.
Theoretical aspects
The present study focuses on two important theoretical assumptions: first, the methodological and instrumental possibilities and limitations of assessing healthcare access and quality at the level of population and territory; second, the specifics of the needs, values and, probably, the special perception of medical care by representatives of the elderly population as a socio-demographic group. As an individual grows older, there increases a likelihood of acquiring a chronic pathology or some form of functional disability, such as lack of mobility and strength, loss of vision or hearing, loss of the ability to communicate or cognitive decline, disability. Impaired coordination of movements increases the risk of other injuries, such as falls or road accidents, while becoming an obstacle to recovery. This shows the specificity of older adults as a socio-demographic group that requires additional attention from society, the state and medical services. It for a reason that the concepts related to the responsiveness of healthcare systems to the problems and special needs of the elderly are becoming more widespread in modern management practice1 (Lehning, De Biasi, 2018).
This specificity is expressed in the need for an integrated approach to providing services to the elderly, especially in cases of dysfunctional disorders, when providing care in medical institutions (Melkonyan et al., 2021; Isaev et al., 2022). The publication issued by the Nordic Medico-Statistical Committee (NOMESCO) proposes and tests, as part of a comparative analysis of the Nordic countries, indicators of the quality of medical care that take into account the specifics of older adults as a special category of patients2. However, the authors of the report focus on a narrow category of diagnoses and types of medical services provided in hospital settings, which adds specificity to the assessment, but limits its informative value in relation to the entire elderly population, whose health characteristics and needs for medical care are, naturally, various.
The problem of interpreting the concepts of “access” and “quality” requires special attention. It becomes obvious already at the level of the review of the Russian federal legislation in the field of public health protection. Thus, in the text of RF Federal Law 323-FZ, the components of healthcare access are not strictly separated from the criteria of helathcare quality (Article 10. “Healthcare access and quality”)3. When analyzing the regulatory framework for assessing healthcare access and quality, a number of inherent contradictions and limitations are also revealed, which makes it difficult to develop and effectively implement measures to ensure these important criteria (Kolomiychenko, 2020). The possibilities and limitations of measuring healthcare access and quality have some differences. Thus, it is generally assumed that access can be measured more effectively than quality, especially when it comes to sociological surveys, which assume subjectivity of perception and, consequently, evaluation. Healthcare access is quite successfully formalized in a number of components identified by D. Peters (Peters et al., 2008). For example, geographical access to medical care can be assessed based on the distance separating the consumer and the provider, as well as the quality of transport and a number of contextual nuances, financial access – based on the willingness and ability of users to pay for the services provided, the availability of insurance tools to protect against the economic consequences of healthcare costs (Lokosov et al., 2024). Financial access is becoming particularly relevant due to the widespread commercialization of the healthcare sector, as well as taking into account the link established by Russian researchers between financial welfare and medical activity (Kislitsyna, Chubarova, 2023). Older adults in this regard fall into the category of increased risk (Mukharyamova, Savelyeva, 2019). With the development of information technology, access has also acquired a “digital” dimension. Thus, the availability of telemedicine technologies and remote consultation options are already adding to the list of aspects of healthcare access (Medvedeva et al., 2022). However, the elaboration of the structure of healthcare access does not negate the difficulty of setting boundaries when conducting appropriate assessments.
The quality of medical care or services as an object of measurement has some fundamental limitations. In most cases, they are due to asymmetric information described as an economic phenomenon by K. Arrow and G. Akerlof (Arrow, 1963; Akerlof, 1970). In the case of mixed healthcare systems, which are typical for most countries, the situation is aggravated by the lack of separation of medical services markets, which makes it difficult to find and analyze information about different treatment alternatives for patients. As a result, quality assessment goes beyond the cognitive capabilities of the consumer. In order to offset information asymmetry, administrative measures are applied, primarily standardization and licensing. The quality assessment is carried out in the context of analyzing the adequacy of routing and following treatment protocols. Informal components of control may also be included, such as moral attitudes and guidelines. However, subjective assessments, if the above-mentioned limitations of interpretation are specified, may also occur with appropriate methodological and technique-related reservations. Thus, the survey on satisfaction with healthcare quality is applied not only at the population level, but also at the micro level. For example, L.V. Mammadova describes the practice of assessing the quality of medical care after surgical interventions in hospital departments of otosurgery. The assessment is carried out by both staff and patients through the dynamics of their quality of life and the psychoemotional state of patients (Mammadova, 2012). We note that in this case, it would be reasonable to assess healthcare access by answering the question about the length of waiting for a planned operation, the distance from the home to the hospital, etc.
However, it is particularly important how the categories “access” and “quality” can and should relate to each other in the context of policy analysis and quality management in healthcare. The analysis of the sources revealed three alternative approaches to the interpretation of the links between healthcare access and quality.
-
1. Access and quality are accepted, if not as synonymous concepts, then at least adjacent and mutually communicating ones (Tsarik et al., 2017).
-
2. Access is considered as an element and criterion of quality (Sharabchiev, Dudina, 2013).
-
3. The categories of “quality” and “access” are separated, but they are analyzed in parallel, and a search is underway for ways to pair them or dichotomize them, which is especially important in the context of the coexistence of the public and private sectors in healthcare. It is this approach that has the greatest analytical value. One of the most striking examples of its successful testing is a study of subjective assessments of healthcare access and quality by citizens of three English-speaking countries – the USA, Canada and the UK, which revealed the nuances of a systems dichotomy4. Clear hints of the advantages of this approach can be found, albeit infrequently, in the works of Russian and foreign scientists. For example, Canadian researchers S. Haddad and P. Fournier talk about
the danger of absolutizing the principle of universal access to medical care in developing countries to the detriment of compliance with quality requirements (Haddad, Fournier, 1995). In the works of a number of researchers (Kochkina et al., 2014; Shishkin et al., 2019) the dichotomy between quality and access is read “between the lines” in the description of the findings of a sociological survey, according to which a significant part of respondents speak in favor of the quality of medical care even with limited access to it. However, one cannot fail to note the gap inherent in such surveys between motives and attitudes on the one hand and actions on the other (LaPiere effect). In other words, verbalized attitudes are not necessarily implemented, and respondents’ answers that do not capture objective experience may not reflect their behavior in real life. One of the objectives of our research was to overcome this omission by appealing to the actual experience of the respondents.
The comparison of criteria for healthcare access and quality provided in commercial and public sector organizations carried out in the article is due to the increasing prevalence among Russia’s residents of the practice of paying for medical services from their own funds and also due to the interesting results of this approach to research already found in the periodical press (Ivanov et al., 2023). Access and quality as features of medical care should be considered as universal categories, and the choice of criteria for distinguishing groups within the framework of comparative analysis should be dictated by the specific task of the study. For example, it may be of interest to compare estimates of healthcare access and quality in the light of gender, territorial, property, and other differences. In the context of the abovementioned urgent problems, first of all, the steady trend of aging and the contradictory development of modern Russian healthcare, the analysis of the ratio of the “access” and “quality” parameters in relation to the age categories of respondents deserves special attention.
Materials and methods
The information base of the work includes the results of sociological surveys representing the opinions and assessments of the adult population of the Vologda Region. Field sociological studies were conducted in the region in 2018, 2020, 2022 and 2024, which makes it possible to assess the situation in dynamics and taking into account changing epidemiological conditions, for example, in the context of the COVID-19 pandemic. The survey was conducted through a handout questionnaire and covered the region’s major cities of Vologda and Cherepovets, as well as eight municipal districts, including small cities. The sample size was 1,500 people. The sample was proportional and quota-based, its error was 4%. In the questionnaire, questions about healthcare access and quality are contained in the section on medical activity. First of all, respondents were asked to assess healthcare access (“Please assess the level of healthcare access provided in public and private medical institutions for you”) by choosing an answer option from the suggested ones: 1) “high”, 2) “medium”, 3) “low” and 4) “medical services are completely inaccessible”. The question about quality is formulated as follows: “How would you generally assess the level of quality of medical care provided in public institutions (polyclinics, hospitals, etc.) and private medical organizations?” It was suggested to choose one response among the following: “high”, “medium”, “low”, “quality is very poor”. The corresponding estimates for two types of organizations – “state polyclinics and hospitals” and “private medical organizations” – were initially divided.
The study was based on the answers of respondents with actual experience of visiting medical organizations during the 12 months preceding the survey. Since the study was focused on identifying the opinions of the region’s elderly population, the analysis considers the results concerning this particular category of respondents. To determine the characteristics of the analyzed population category, data are provided for other age groups (the sample is divided into three age groups: 1) young residents of the region aged 18 to 30; 2) middle-aged, from 30 to 60 (55); 3) older adults aged over 60 (55)), as well as in general for all respondents, regardless of age. Based on the results of the survey, healthcare access (AI) and healthcare quality (QI) indices were calculated. The calculation method in both cases involves calculating the difference between the sums of the specific weights of positive and negative ratings in the total pool of respondents’ answers. To exclude negative index values, 100 is added to the resulting difference. The indices are compared in the context of age-specific identification by assessing the depth of differences – through the ratio of the minimum index value to the maximum and through the ratio of the index calculated for the group of older adults to the average value for the entire sample. The parallel analysis of the quality and access parameters is carried out both by calculation, through the ratio of the coefficients corresponding to them, and graphically. The placement of age groups as points in the “access – quality” coordinate system provides analytical value due to its clarity.
Taking into account the rapid development of the private healthcare sector in the region, the analysis of healthcare access and quality was carried out in the context of the public and private sectors. Since in modern conditions the boundary between them is being blurred (for example, in public institutions there are paid departments of medical care, and in private institutions there is a rare practice of paying for medical services through the compulsory medical insurance system), it is necessary to determine the criterion for their separation in order to solve the research tasks. The “form of ownership” criterion was chosen as the basic one. According to it, the healthcare sectors are represented by institutions of the appropriate list of organizational and legal forms.
Results
The elderly in the region demonstrate the greatest need for medical care among all age groups. Although health is the highest value for representatives of the three analyzed population categories, older adults more often than others tend to put it at the highest level of the hierarchical structure of personal values. Thus, while 70 and 67% of young and middle-aged people, respectively, say that health is their main value, the proportion of such responses among the elderly reaches 84%. These differences between age groups are due to a decrease in the subjective importance of material wealth, work and social recognition for the elderly. An increasing demand for medical care in older adults is due not only to the dynamics of value stereotypes, but also to objective requirements (increased risks of diseases and, consequently, the need for regular medical check-ups) and deterioration of physical health: 39% of the older group admit that they suffer from long-term chronic diseases (among young people and the middle-aged category, this indicator amounts to 5 and 10%, respectively).
The absolute majority of representatives of all three age groups, namely 82% of young, 86% of middle-aged and 90% of elderly respondents, recognize personal responsibility for their health. The roles of the state and the family are ranked 3rd and 4th, and there are practically no age differences here. At the same time, with age, there is a slight but nevertheless noticeable transformation of the radius of responsibility for health. Older people place more responsibility for their own health on medical professionals than younger people (58% of the elderly chose this response, while among young people it was 39%, and among middle-aged respondents it was 49%). This is largely due to an increase in their medical activity. The region’s elderly residents are more likely than others to become consumers of medical services. While 57% of young people aged 18 to 30 have applied to medical organizations in the last twelve months, among middle-aged respondents the proportion of applicants has already reached 69%, and for the elderly population it has reached 84% (Tab. 1).
Older adults are more likely than representatives of the young and middle-aged categories of respondents to visit public medical institutions (in 2024, 55% of the elderly visited them exclusively, while this proportion was 34% among young people and 39% among middle-aged people). At the same time, the elderly population insignificantly, but still more often than young people and middle-aged people, show mixed medical activity, alternating or combining appeals to organizations in both health sectors.
It is of interest to analyze the dynamics of the indices showing healthcare access and quality in the context of the COVID-19 pandemic. In the precrisis period (we have data for 2018), there was a high level of satisfaction with healthcare access (AI=153.6) and especially with its quality (QI=164.1) among the elderly residents of the region who visited public medical institutions. In 2020, when the pandemic reached its peak, the satisfaction ratings of the discussed category of respondents reached the highest level for the period under consideration (QI=181.4; AI=165.8). In subsequent years, respondents’ satisfaction with healthcare access and quality decreased significantly. The situation was particularly negative in 2022 (QI = 104.4; AI = 111.6). At the same time, in contrast to the situation in 2018 and 2020, in the post-COVID period, assessments of healthcare access began to prevail over quality assessments.
Elderly residents’ assessments of healthcare access and quality provided in private medical organizations in the Vologda Region have significantly exceeded those in the public sector over the years and have varied in a similar way. In the post-COVID-19 period, there was a decrease in the indices, but these changes were moderate. During the entire period, the quality indices of medical services in private organizations exceeded the accessibility indices.
Representatives of different age groups (in this case older respondents do not show noticeable differences from younger and middle-aged groups) tend to rate healthcare quality higher than healthcare access, regardless of the health sector. These differences can be judged by the ratio of coefficients (QI/AI; Tab. 2 ). Several cases have been recorded when the AI exceeded the QI. The most significant exception was in 2024: estimates of healthcare access provided by government agencies were significantly lower than the quality parameters (QI/AI = 0.882). In the assessments of the elderly, quality indices are higher than access indices, which corresponds to the measurements carried out among representatives of the young and middle-aged groups. The only exception to this rule was young respondents’ assessments of the quality of services in private organizations, which in 2020 were not significantly inferior to
Table 1. Distribution of responses to the question “Have you visited medical institutions for the last 12 months?” (Vologda Region, 2024), %
|
Response |
18–30 years old |
30–60 (55) years old |
60 (55) years old and > |
Average for all groups |
|
Yes, I have, including: |
57.4 |
68.7 |
83.5 |
72.5 |
|
public |
46.4 |
56.7 |
76.5 |
62.4 |
|
private |
23.4 |
29.4 |
28.1 |
28.1 |
|
Only public |
34.0 |
39.3 |
55.4 |
44.3 |
|
Only private |
11.0 |
12.0 |
7.0 |
10.1 |
|
Both public and private |
12.4 |
17.4 |
21.1 |
18.1 |
|
No, I have not. |
42.6 |
31.3 |
16.5 |
27.5 |
|
Source: sociological survey of the Vologda Region population. |
||||
access parameters (QI/AI = 0.881). The differences between the estimates of the elderly population of the region and those of representatives of other age groups relate not to the fundamental ratio of quality and access parameters, but to the size of the gap between them in favor of the former. In 2024, the prevalence of assessments of healthcare quality received by respondents in private organizations in the region over its access, recorded in the elderly population, reached its maximum value for the entire measurement period for all age groups (QI/AI was 1.275).
Table 2. Indices of healthcare access and quality for older adults in comparison with other age groups
|
Index |
Age group |
Average for groups |
Difference (min / max) |
Deviation of the values for the older adults category from the average |
||
|
18–30 years old |
30–60 (55) years old |
60 (55) years old and > |
||||
|
2018 |
||||||
|
Public clinics and hospitals |
||||||
|
QI* |
166.6 |
165.1 |
164.1 |
164.8 |
0.985 |
0.996 |
|
AI** |
152.4 |
146.0 |
153.6 |
150.1 |
0.951 |
1.023 |
|
QI/AI |
1.093 |
1.131 |
1.068 |
1.098 |
0.966 |
0.973 |
|
Private healthcare organizations |
||||||
|
QI |
200.0 |
193.6 |
196.0 |
195.6 |
0.968 |
1.002 |
|
AI |
178.9 |
163.2 |
164.8 |
166.6 |
0.912 |
0.989 |
|
QI/AI |
1.118 |
1.186 |
1.189 |
0.989 |
0.940 |
1.202 |
|
2020 |
||||||
|
Public clinics and hospitals |
||||||
|
QI |
178.3 |
177.9 |
181.4 |
179.6 |
0.981 |
1.010 |
|
AI |
164.4 |
160.8 |
165.8 |
163.4 |
0.970 |
1.015 |
|
QI/AI |
1.085 |
1.106 |
1.094 |
1.099 |
0.981 |
0.995 |
|
Private healthcare organizations |
||||||
|
QI |
169.4 |
187.6 |
193.6 |
187.2 |
0.875 |
1.034 |
|
AI |
192.3 |
177.8 |
177.4 |
179.6 |
0.923 |
0.988 |
|
QI/AI |
0.881 |
1.055 |
1.091 |
1.042 |
0.808 |
1.047 |
|
2022 |
||||||
|
Public clinics and hospitals |
||||||
|
QI |
109.2 |
106.8 |
104.4 |
106.2 |
0.956 |
0.983 |
|
AI |
111.6 |
113.1 |
111.6 |
112.3 |
0.987 |
0.994 |
|
QI/AI |
0.978 |
0.944 |
0.935 |
0.946 |
0.956 |
0.988 |
|
Private healthcare organizations |
||||||
|
QI |
176.2 |
170.6 |
177.0 |
173.8 |
0.964 |
1.018 |
|
AI |
152.6 |
162.9 |
151.4 |
157.4 |
0.929 |
0.962 |
|
QI/AI |
1.155 |
1.047 |
1.169 |
1.104 |
0.896 |
1.059 |
|
2024 |
||||||
|
Public clinics and hospitals |
||||||
|
QI |
130.4 |
133.1 |
115.0 |
124.9 |
0.864 |
0.921 |
|
AI |
153.6 |
147.8 |
132.5 |
141.6 |
0.863 |
0.936 |
|
QI/AI |
0.849 |
0.901 |
0.868 |
0.882 |
0.942 |
0.984 |
|
Private healthcare organizations |
||||||
|
QI |
175.5 |
182.8 |
182.9 |
182.0 |
0.960 |
1.005 |
|
AI |
167.2 |
168.3 |
143.5 |
156.9 |
0.853 |
0.915 |
|
QI/AI |
1.050 |
1.086 |
1.275 |
1.160 |
0.824 |
1.099 |
|
*QI – quality index; **AI – access index. Source: calculated according to the sociological survey of the Vologda Region population. |
||||||
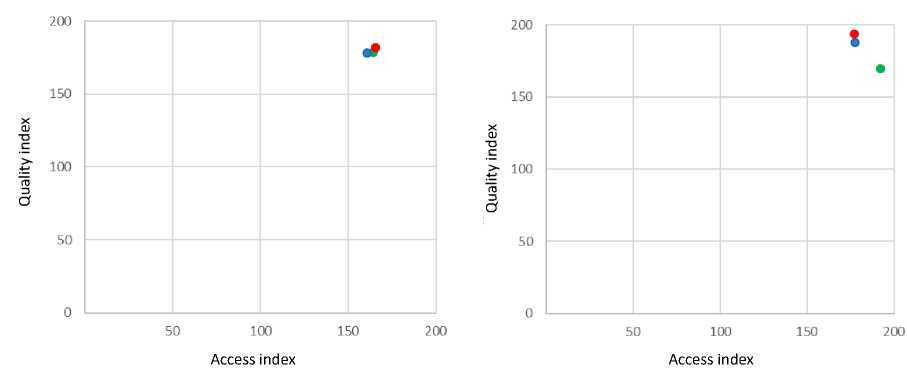
Healthcare quality/access parameters ratio provided by public sector institutions in the context of age groups is formed in such a way that the corresponding points on the graph are located as close to each other as possible, and the range of values for both indices is minimal (Fig. 1).
The exception was the assessment of medical care in the public sector in 2024: the older age group was located on the graph in isolation from the young and middle-aged groups compactly located next to each other, and according to both criteria under consideration (Fig. 2).
When it comes to assessing healthcare access and quality within the private sector, the ranges of indices’ values are significantly expanded, and this is due to the gap between different age groups. In the estimates for 2018 and 2020, there is a noticeable gap between the elderly and middle-aged groups from the younger ones, whereas in 2022, the opposition to each other is already made up of, on the
Figure 1. Dichotomous scales of healthcare access and quality indices in the public (left) and private (right) healthcare sectors for age groups: 1) from 18 to 30 ( ), 2) from 30 to 60 (55) (•), 3) over 60 (55) (•)
2018 (pre-COVID period)
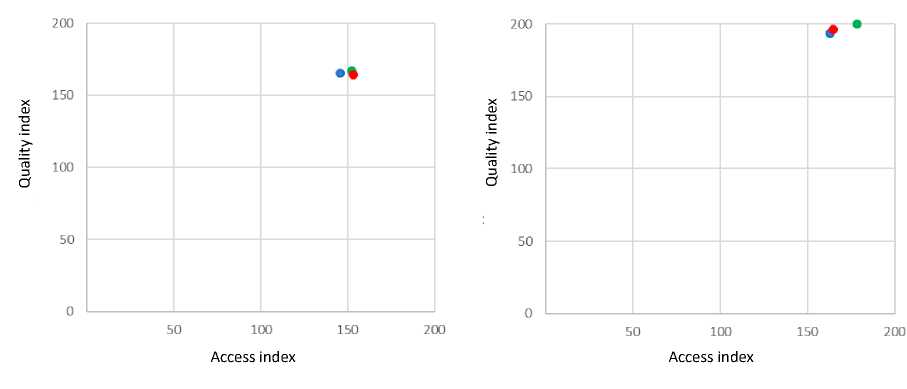
2020 (peak of the COVID-19 pandemic)
Source: sociological survey of the Vologda Region population.
one hand, the pair “youth and the elderly” located closely in the evaluation field and, on the other hand, the category of middle-aged residents of the region.
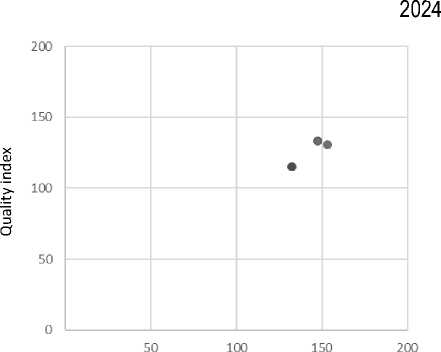
In 2024, the maximum variation in the values of healthcare access and quality indices between the elderly and other age groups in relation to public health institutions is recorded for the entire measurement period. The category of the region’s elderly residents significantly differed from the young and middle-aged groups on the scale of healthcare care access in the private sector (due to the low ratings given by older adults: the AI for the elderly was 115.0, for the young – 130.4 and for the middle-aged group – 133.1), while in the “quality” parameter there was no significant variation in the indices’ values. We note that in 2022, the access index for older adults took on an even lower value – 104.4 (the minimum value of the parameter for the entire measurement period), but the gap from other groups eventually turned out to be insignificant, since the index values for the other two age groups were extremely low (in the group of youth under 30 – 109.2, in the middle-aged group – 106.8; Fig. 2).
Figure 2. Dichotomous scales of healthcare access and quality indices in the public (left) and private (right) healthcare sectors for age groups: 1) from 18 to 30 ( ), 2) from 30 to 60 (55) (•), 3) over 60 (55) (•)
2022 (post-pandemic period)
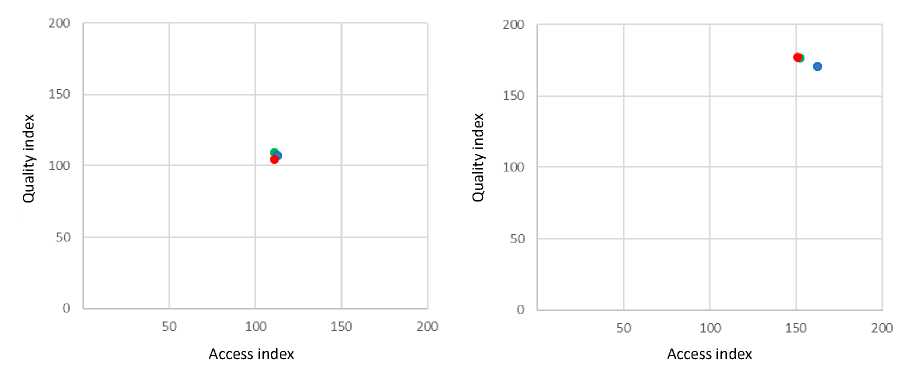
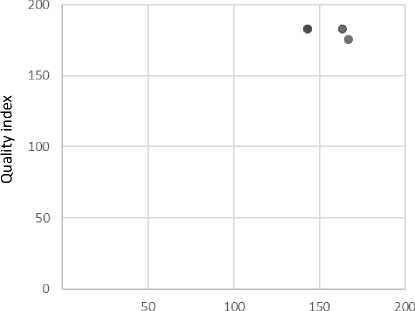
Access index Access index
Source: sociological survey of the Vologda Region population.
Discussion
Respondents’ greater satisfaction with healthcare quality rather than access is evidence that the main problem for respondents is the difficulty of obtaining medical care and services. Meanwhile, we can assume that the inverse ratio of the indices, the predominance of the access index over the quality index, would characterize the situation as particularly unfavorable – open access to services of mediocre quality.
The research results for 2024 indicate negative changes in healthcare access and quality provided by government agencies in general across all three age categories of respondents. The gap between the senior group and the other two in the assessments of public sector medical care on both scales, which has appeared for the first time in the history of the measurements, is particularly telling. Since the assessments are based on the respondents’ opinions, the reasons for the identified negative changes can be considered as an objective decrease in healthcare access and quality in the public sector, as well as an increased level of expectations and claims of older people, as well as the fact that their lower health characteristics compared to those of other groups force older adults to perceive all existing flaws in the work of medical services more acutely and painfully. At the same time, the fact that in earlier periods, including in the pandemic year, the spread between age groups in quality and access assessments was minimal, gives grounds to look for objective reasons for the differences identified. In recent years, especially in 2024, there has been a significant increase in the cost of living in Russia. Since pension indexation does not make up for the increase in prices for essential goods (food and medicines), inflation is hitting socially vulnerable population groups, including the elderly. Accordingly, it is becoming increasingly difficult for them to find the means to purchase paid services, while access to free services is not improving.
The minimum ratio of healthcare access and quality indices provided by private organizations in the group of young respondents under 30 years of age should be interpreted by recording high estimates of the level of access and modest estimates of quality, which indicates the high expectations and requests of this category of respondents and their available opportunities, primarily informational and financial. An analysis of the proportions of specific respondents’ answers allows us to note only one detail that is offset when calculating the indices: the contribution of positive ratings to the overall pool of ratings for government agencies is formed with a noticeable advantage of the “satisfactory” response, while positive ratings for commercial organizations are combined with the prevalence of high ratings, which is especially noticeable in opinions regarding the quality of care. Consequently, respondents perceive medical care provided by the public sector as a kind of minimum guaranteed by the state, while private healthcare providers strive to go beyond these boundaries, claiming to achieve high quality standards.
Comparing the indicators of healthcare access in public and private medical institutions, it is necessary to make a reservation that the accessibility of care in the private and public sectors is fundamentally different in nature. In the public sector, access is primarily related to the very possibility of getting an appointment with a specialist of interest for free, which is determined by a number of spatial conditions (territorial remoteness of the institution, availability of transport, etc.) and organizational (staffing of full-time positions, availability of specialists, and waiting times for an appointment), or to undergo the necessary examination within a reasonable time. In a private clinic, despite a number of similar restrictions (for example, the need to wait for an appointment, the territorial remoteness of organizations, which may be especially relevant for residents of rural areas, etc.), the cost of services is the main factor limiting access.
The proposed index approach to the interpretation of subjective assessments of healthcare access and quality has both important instrumental advantages and limitations. On the one hand, it is characterized by simplicity of calculation and functionality (due to these qualities, it is applicable in the comparative analysis of territorial and sociodemographic units). On the other hand, it hides a number of nuances in the estimates. The positive answers of the respondents included in the index structure latently combine both high and satisfactory ratings, and it is in these responses that the difference in assessments of the public and private sectors manifests itself, the differences between them are leveled, in particular, the overall ratings of public clinics and hospitals are increased. The most difficult problem of interpreting the results is the subjectivity of respondents’ understanding of the categories “access” and “quality” embedded in the methodology. And if access as a characteristic of medical care has a certain right to the intuitive nature of its perception and interpretation, then quality is most often accepted as an attribute, the assessment of which should be based on a high level of expertise of the actor who makes the assessment.
Conclusion
Thus, older adults demonstrate a higher level of need for medical care than representatives of other age groups due to the natural deterioration of their health status. In the post-pandemic period, there have been important and mostly negative changes in the assessments of healthcare access and quality by elderly residents in the Vologda Region. This is reflected both in a significant decrease in assessments of the quality of medical care provided in public health institutions (in 2022, the QI was 104.4, which is the minimum index value for the entire measurement period, in 2024 – 115.0), and an increase in 2024 in the gap between the index values for both parameters of medical care provided by the public sector, compared to younger age groups. In 2024, the estimates of the representatives of the older age group regarding healthcare access provided by private medical organizations decreased, which formed a gap in this parameter with the younger age groups in the region. The assessments of the elderly population regarding quality parameters demonstrated stability. As a result, the index of differences in quality and access parameters for the group under discussion reached its maximum value (1.275) for the entire period in question.
The results obtained suggest that older adults find themselves in a special risk group: having a more tangible need for high-quality medical care than other population groups, they are forced to overcome a significant number of barriers to receive it, which is complicated by natural limitations such as health conditions, movement problems, etc. The need to pay for a number of diagnostic and therapeutic procedures, as well as access to an alternative, commercial, channel for obtaining medical services, is complicated by the low level of effective demand. This is reflected in the significant separation of representatives of the older generation from other age groups in assessing healthcare access provided by private organizations.
In general, the index approach we use to assess healthcare access and quality in parallel has prospects for practical application, being characterized by the simplicity of data collection and analysis tools and the clarity of the results.


