Ilizarov ring fixator for ankle fusion: a gold standard in managing complex ankle pathologies
Автор: Dhawan M., Nandan B., Guhan R.K., Dwivedi S., Prasad M.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 3 т.31, 2025 года.
Бесплатный доступ
Introduction Ankle arthrodesis is a surgical procedure for end-stage arthritis and complex ankle pathologies, offering a limb-salvaging alternative to amputation. This study aims to present clinical experience with the Ilizarov apparatus in achieving stable, painless ankle fusion in patients with varied complex ankle pathologies. Materials and Methods A retrospective study was conducted involving 27 patients who underwent ankle arthrodesis using the Ilizarov fixator between 2014 and 2024. Clinical and radiological evaluations were performed using the ASAMI scoring system. Surgical techniques, patient demographics, and outcomes were analyzed. Results All 27 patients achieved successful bone union. ASAMI Bone results were rated excellent in 23 and good in 4. Functional outcomes were rated as good in 22 patients and fair in 5. Pin tract infections were effectively managed with antibiotics. The Ilizarov technique demonstrated superior results in achieving stable, pain-free ankles, even in cases with severe osteomyelitis and destroyed ankles with deformities. Discussion The Ilizarov apparatus provides a minimally invasive, versatile approach for complex ankle pathologies, enabling dynamic axial compression, early weight-bearing, and deformity correction. Despite limitations such as high costs and skill requirements, its success rate surpasses that of internal fixation techniques. Conclusion The Ilizarov apparatus is the gold standard for ankle arthrodesis, offering stable fusion and addressing comorbidities such as osteomyelitis and limb length discrepancy, with high patient satisfaction and functional recovery.
Ankle arthrodesis, Ilizarov apparatus, bone union, limb salvage, complex ankle pathology
Короткий адрес: https://sciup.org/142244804
IDR: 142244804 | DOI: 10.18019/1028-4427-2025-31-3-279-286
Текст научной статьи Ilizarov ring fixator for ankle fusion: a gold standard in managing complex ankle pathologies
Ankle arthrodesis refers to complete fusion of the tibio-talar joint and is recommended for conditions such as secondary painful osteoarthritis, neuromotor disorders, post-septic sequelae, avascular necrosis (AVN) of the talus, Charcot neuroarthropathy, and as a salvage procedure to preserve limb functionality [1]. In patients suffering from end-stage arthritis, where amputation is considered the only option due to complexity of local pathology, ankle arthrodesis serves as the ultimate alternative for limb salvage [2].
Various techniques have been developed over time to achieve ankle fusion, including cross screws at the tibio-talar joint, ankle arthrodesis nail, and external fixators. However, no consensus has been reached regarding the most effective method for achieving good interfragmentary compression under functional weight-bearing conditions, along with sufficient foot functionality [3–7]. Unfortunately, many of the currently used methods are associated with significant complications, including deformities, non-consolidated fractures, and septic arthritis, which may further lead to severe secondary osteoarthritis [8].
In cases where bone quality is good, soft tissue coverage is adequate, and there is no associated shortening, the use of internal plate osteosynthesis for ankle joint fusion can yield good results. However, this technique is linked to a higher risk of chronic osteomyelitis (in some instances tuberculosis osteomyelitis), bone defects, neurological deficits, and soft tissue compromise. Under such circumstances, the Ilizarov apparatus provides a more effective solution for orthopedic surgeons [9, 10].
Compared to the Ilizarov technique, internal fixation methods are less complex and involve a simpler approach. However, the risk of complications such as skin necrosis, severe infections, septic arthritis, lack of fusion, and the necessity for revision arthrodesis remains significant [2, 3, 9].
The Ilizarov apparatus offers a unique advantage by enabling dynamic axial compression and providing 360-degree rigidity. Its minimally invasive approach ensures reliability with significant benefits including immediate weight-bearing and early mobilization of adjacent joints. Moreover, it serves as a definitive fixation technique in a single stage [11]. Beyond compression, the apparatus also enables distraction, allowing for effective correction of bone axis deformities.
Despite its numerous advantages, the Ilizarov apparatus has certain notable limitations including the complexity of the fixator assemblies, the skill required for its application along with temporary patient discomfort with the fixator [1, 2, 9–11].
Patients with severe osteoarthritis of the ankle often endure excruciating pain during routine daily activities. The accompanying functional loss and pain are often the driving factors leading these patients to seek surgical intervention. The success of ankle arthrodesis is highly dependent on patient compliance to postoperative protocols [8, 9, 12]. The most effective treatment outcomes are marked by reduced pain and improved functional capabilities [5, 8, 9, 12, 13].
Aim of the study is to present our clinical experience and the versatility of the Ilizarov apparatus in achieving stable, immobile, and painless ankle fusion in patients with a wide spectrum of ankle joint pathologies.
MATERIALS AND METHODS
The study was conducted at a reputed teaching institution and tertiary care hospital in New Delhi, India. It received approval from the institutional ethics committee. The analysis was based on a retrospective review of 27 patients who underwent ankle arthrodesis using the Ilizarov apparatus between 2014 and 2024, spanning a decade.
The study included all patients who underwent ankle fusion with the Ilizarov fixator. Various parameters such as gender, age, time of injury, fracture type, history of prior surgeries, indications for the procedure, and duration of fixation with the frame on were evaluated. Bone and functional outcomes were evaluated using the ASAMI scoring system [14].
Preoperative radiological assessments were performed based on individual case requirements. Full-length X-rays of the ankle and leg were taken in all patients, while MRI and CT scans were obtained for cases involving osteomyelitis or suspected nonunion to aid in diagnosis.
Medical comorbidities were documented, and any modifiable risk factors were addressed and optimized prior to surgery.
All surgical procedures were carried out by a senior orthopedic surgeon experienced in complex trauma management and an expert in the Ilizarov method.
Surgical technique
All surgeries were performed under general/spinal/epidural anesthesia depending upon the medical condition of the patient, with the patient positioned in supine position with ipsilateral sandbag elevation. Prophylactic intravenous antibiotics were administered at the time of the skin incision in accordance with standard guidelines. The ankle joint was approached laterally, medially, or anteriorly depending on the pathology, with the lateral transfibular (malleolar) approach being the most commonly used due to its advantage of providing wide access to the ankle region.
For the medial approach, a 7-cm skin incision was made starting at the tip of the medial malleolus and curving anteriorly over the distal tibia. The saphenous nerve and vein were carefully protected, and the medial malleolus was osteotomized to access the ankle joint. For the anterior approach, a 10-cm incision was centered midline between both malleoli. Superficial dissection was performed, preserving the superficial peroneal nerve. The extensor digitorum longus and extensor hallucis longus were identified, and a plane was developed between them. Deeper dissection revealed the anterior tibial artery and deep peroneal nerve, which were retracted safely, allowing anterior access to the ankle joint.
In the lateral transfibular approach, a 10-cm incision was made along the subcutaneous border of the distal fibula, with a transverse fibular osteotomy performed 8 cm proximal to the tip of the lateral malleolus. The tibio-talar joint was opened, and the distal tibial articular surface was denuded at the subchondral level, followed by preparation of the talar dome. In cases of infection, thorough debridement of the soft tissue and bone was performed, and culture swabs were taken for postoperative management.
Once fresh metaphyseal bone with the characteristic “paprika sign” was exposed, the tibia and talus were aligned under fluoroscopic guidance and fixed with a tibio-calcaneal 3-mm K-wire. Infected cases underwent meticulous debridement of necrotic tissue before fixation. The Ilizarov frame included proximal tibial rings (R1, R2) and a foot frame with 5/8 rings for the hindfoot and forefoot, if required. The hindfoot ring (R3) was secured with olive wires and half-pins to the calcaneus and connected to the tibial rings (R2) with threaded rods for controlled compression. In some cases, wires were used to secure talus considering having good bone stock in order to get good interfragmentary compression and to put less stress on subtalar joints. Intraoperatively, 1-cm compression was applied between R3 and R2, with corticotomy and distraction performed between R1 and R2 for lengthening when necessary. No primary bone grafting was performed in any of the cases, which is an important observation in this context.
Postoperatively, patients were instructed to perform weight-bearing with walker support after removal of tibio-calcaneal wire at 6 weeks postoperatively. Emphasis was placed on rigorous pin-site care at least twice daily. Follow-ups were conducted thrice monthly initially and transitioned to monthly visits after three months. Radiological evaluations monitored callus formation, alignment, and infection, while clinical assessments focused on skin and pin-tract condition and neurovascular status. Solid union was defined by continuous cortical and trabecular lines on radiographs at the tibiotalar joint, followed by one month of dynamization and CT confirmation before frame removal. Patients used protective bracing for up to six weeks upon frame removal, with the ultimate goal of achieving a pain-free, stable, plantigrade foot and restored gait.
RESULTS
This retrospective study included 27 patients who underwent ankle arthrodesis using the Ilizarov frame, comprising 8 females (29.63 %) and 19 males (70.37 %). The patient’s age ranged from 20 to 78 years, with an average of 40 years [SD: 15.48; Median (IQR) is 35 (20–56)]. Among the cases, 12 patients (44.4 %) presented with active osteomyelitis. The Ilizarov frame was used for an average duration of 33 weeks [SD: 13.9; Median (IQR) is 27 (21–43)], earliest frame removal being 19 weeks and longest being 70 weeks. The causes of ankle joint destruction in the study covered a broad spectrum, including post-traumatic cases in 16 patients (59.26 %), post-polio residual deformity in 3 patients (11.11 %), Charcot arthropathy in 6 patients (22.22 %), and cases involving a destroyed or resorbed talus in 2 patients (7.41 %). Adjacent joint arthritis was noted in 6 patients, representing 22.2 % of the sample. All patients exhibited a limb length discrepancy of less than 1.5 cm, which was effectively addressed using appropriately sized shoe lifts.
The study achieved a 100 % bone union rate across all cases. Patients reported significant comfort with the procedure and were able to ambulate independently, pain-free, and without support after frame removal.
The ASAMI scoring system (Association for the Study and Application of the Methods of Ilizarov) was utilized to evaluate bone and functional outcomes. Regarding bone results, 23 patients (85.19 %) demonstrated excellent results, while 4 patients (14.81 %) achieved a good outcome (Table 1). Functional scores revealed that 22 patients (81.48 %) had good results, and 5 patients (18.52 %) had fair results (Table 2). Since functional scoring incorporates ankle dorsiflexion, a “good” functional outcome represents the highest achievable score.
In all 27 patients, no primary bone grafting was performed, highlighting that the Ilizarov method is a definitive and less demanding technique for ankle fusion.
A few patients developed pin-tract infection during the treatment period, which was successfully managed with oral and local antibiotics.
Table 1
Table 2
ASAMI Bone result
|
Scores |
Frequency |
Percentage |
|
Excellent |
23 |
85.19 % |
|
Good |
4 |
14.81 % |
|
Total |
27 |
100 % |
Abbreviations : ASAMI — Association for the Study and Application of the Methods of Ilizarov; There were no entries in the Fair and Poor scores.
ASAMI Functional result
|
Scores |
Frequency |
Percentage |
|
Good |
22 |
81.48 % |
|
Fair |
5 |
18.52 % |
|
Total |
27 |
100 % |
Abbreviations : ASAMI — Association for the Study and Application of the Methods of Ilizarov; There were no entries in the Excellent and Poor scores.
Cases
Among 27 patients, a 38-year-old male presented with swelling and dull pain in his left ankle. Clinical andradiologicalassessmentsconfirmedadiagnosisofCharcotarthropathy.Thepatienthadpreviouslyundergone multiple unsuccessful corrective fusion surgeries. Following 44 weeks of treatment, a stable and infection-free tibio-calcaneal fusion was achieved. The ASAMI bone results were excellent, and the functional results were good. However, the patient developed a leg length discrepancy (LLD) of approximately 1.5 cm, which was successfully corrected with a customized shoe lift (Fig. 1, 2, 3).

Fig. 1. Pre-op clinical pictures of left ankle with severe septic arthritis (sequelae of Charcot arthropathy): a — lateral view; b — medial view; c — frontal view

Fig. 2. Clinical picture of stable infection-free painless fused left ankle after frame removal: a — lateral view; b — anteromedial view; c — medial view; d — frontal view
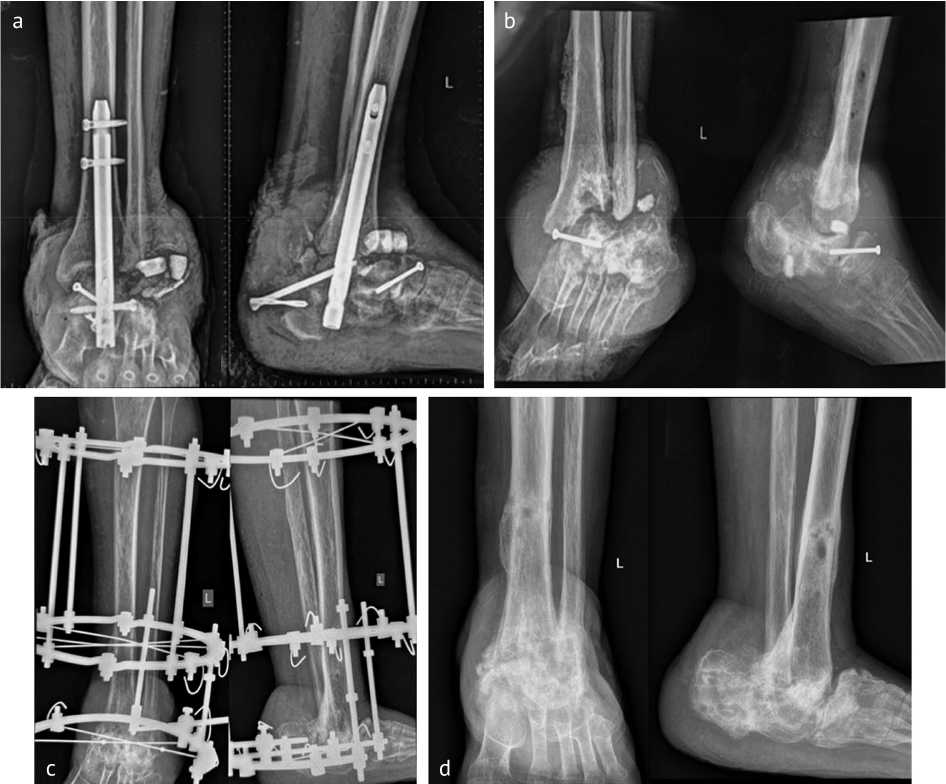
Fig. 3. Series of left ankle X-Rays during the course of treatment: a — 3-month pre-op X-ray with broken calcaneal nail; b — pre-op X-ray at time of surgery; c — at the time of frame removal; d — 6-month follow-up
DISCUSSION
Ankle arthrodesis is a definitive salvage procedure for addressing severely damaged ankle joints. As it represents patient’s final opportunity to achieve a stable and pain-free ankle, careful consideration is essential when selecting an implant for the procedure [15, 16].
The introduction of external fixators for ankle fusion by Charnley marked a significant advancement [1]. Although these devices achieved favorable fusion rates, monoplanar fixators lacked rotational stability. To address this, triangular frames enabling multiplanar compression were developed [17, 18]. Despite these advancements, challenges such as persistent instability at the fusion site remain, particularly in cases with substantial bone loss [7, 12, 19].
For patients with infections, ankle fusion provides absolute stability, thereby minimizing the risk of recurrence [13, 20].
The Ilizarov ring fixator is widely regarded as the most effective system for addressing complex ankle pathologies, outperforming all other fusion techniques [19, 21–26]. Its advantages include dynamic axial fixation, which preserves bone contact without the need for additional grafting. It also offers superior stability against bending, shear, and torsional forces, enabling early weight-bearing and reducing pin-tract infections. Its modular design allows circumferential mechanical control, facilitating postoperative adjustments that are impossible with conventional implants like screws, plates, or nails. Additionally, transfixation wires placed percutaneously provide reliable fixation even in cases with compromised bone and soft-tissue conditions.
Moreover, the Ilizarov method allows ankle arthrodesis to be performed as a single-stage procedure, even in the presence of active infection. Gradual compression at the fusion site promotes biological union, with or without proximal osteotomy and callus distraction. The device also ensures limb length equalization when required [16, 26].
Renowned for its versatility, the Ilizarov device is considered the gold standard for successful ankle arthrodesis. Unlike internal fixation methods, it minimizes damage to soft tissues, vascular structures, and the periosteum, making it suitable for managing complex conditions such as diabetes mellitus, peripheral neuropathy (Charcot), severe osteomyelitis, and peripheral vascular compromise. The Ilizarov system is often the last resort for patients at risk of amputation [16, 27–29].
Among the surgical approaches, the transfibular approach is frequently preferred because it provides access to both the tibiotalar and subtalar joints through a single incision [17, 29]. The choice of approach, however, depends on factors such as deformity type, fixation technique, soft-tissue condition, and surgeon experience [17, 18, 30]. Occasionally, the medial malleolus or anterior approach may be employed depending on casespecific requirements [18]. Thus, T. Onodera et al. demonstrated that transfibular ankle arthrodesis using the Ilizarov fixator combined with fibular onlay grafting achieved complete bone union [11]. In contrast, our cases achieved 100 % union without primary bone grafting.
The ASAMI scoring system is used in this study because it provides a standardized, objective, and comprehensive method to evaluate the success of surgical procedure. It allows for a quantitative and qualitative assessment of both bone healing (union, deformity, infection, and limb length) and functional outcomes (pain, mobility, return to daily activities), ensuring a holistic evaluation of patient recovery. Additionally, its widespread use in orthopedic and trauma research enables comparability with existing literature, facilitating evidence-based conclusions and treatment refinements [14].
Consistent with existing literature, our study also demonstrated a 100 % bone union rate using the Ilizarov apparatus for managing complex ankle pathologies. J. Li et al. concluded that the Ilizarov technique outperforms internal fixation in achieving stable and effective fusion in end-stage ankle arthritis [15].
Similarly, P. Morasiewicz et al. conducted a radiological comparison and found that the Ilizarov method provided superior outcomes compared to internal fixation. They also reported a higher rate of adjacent joint arthritis with internal fixation, whereas in our study, this was observed in 22.22 % (6 patients), lower than their reported 48 % [4].
-
C. Reinke et al. emphasized the reliability of the Ilizarov method for ankle fusion in patients with compromised conditions, highlighting its effectiveness in tibio-calcaneal fusion for severely damaged Charcot arthropathy cases [5]. A case of a tibiocalcaneal fusion for severely destroyed septic arthritis (Charcot arthropathy) is presented in a series of images (Fig. 1, 2, 3). Likewise, our study utilized this technique to achieve stable and functional feet in similar cases.
K.A. El-Gafary et al. demonstrated successful outcomes with the Ilizarov fixator in severe joint destruction due to Charcot arthropathy [6]. Similarly, we achieved stable, pain-free ankles in six patients with severe joint damage from Charcot arthropathy. In four patients, simultaneous tibial lengthening and ankle arthrodesis addressed limb length discrepancy (LLD). R. Sakurakichi et al. similarly reported successful outcomes using this approach [10]. Among our 27 cases, three patients (11.11 %) with post-polio residual paralysis and equinus deformity were successfully managed with this technique. A. Kirienko et al. reported comparable success in their study involving 27 patients [9]. The most common complication encountered in our cases was pin-tract infection, which was managed effectively with oral antibiotics and, in some cases, local antibiotic injections.
Based on our findings and a review of the literature, the Ilizarov apparatus proves to be an indispensable tool for orthopedic surgeons, providing a comprehensive solution for complex cases in a single definitive procedure.
The primary limitations of this study were the absence of preoperative scoring, a single-centre retrospective study and a small sample size due to irregular follow-ups after frame removal, largely because of patient socio-economic challenges. Conducting a larger, randomized study is necessary to relate the results more effectively to the target population.
For most patients undergoing ankle fusion, their frequent visits to doctors can be frustrating. This frustration can be mitigated through effective encouragement and early weight-bearing mobilization-benefits that are difficult to achieve with internal fixation techniques.
CONCLUSION
The Ilizarov apparatus should be regarded as the gold standard for ankle fusion in cases of complex pathology. Compared to other techniques, it offers superior axial compression for enhanced union and effectively addresses concurrent challenges such as limb length discrepancy, Charcot arthropathy, osteomyelitis, deformities (post-polio), osteoporosis, and failed ankle fusions after multiple prior surgeries. It provides a stable, pain-free ankle, enabling improved mobility.


