Investigation of the prevalence of prediabetes risk factors among rural residents of Andijan
Автор: Matkarimova M.K., Soliyeva M.I., Muhamedova V.M.
Журнал: Мировая наука @science-j
Рубрика: Основной раздел
Статья в выпуске: 2 (95), 2025 года.
Бесплатный доступ
Prediabetes is an intermediate hyperglycemic condition that often progresses to type 2 diabetes (T2D) without intervention. This study aimed to assess the prevalence of non-lipid and lipid-related risk factors for prediabetes in the rural working-age population of Andijan, Uzbekistan. A sample of 2112 individuals underwent screening, revealing that excess body weight, family history of diabetes, hypertension, and low physical activity were significant risk factors for glycemic disorders. The findings emphasize the need for early identification and preventive measures, including lifestyle changes, to reduce the progression to diabetes. Early intervention is critical to managing prediabetes and preventing complications associated with T2D.
Prediabetes, type 2 diabetes, risk factors, rural population, excess body weight, hypertension, glycemic disorders, metabolic health, lifestyle intervention, cardiovascular risk
Короткий адрес: https://sciup.org/140310820
IDR: 140310820
Текст научной статьи Investigation of the prevalence of prediabetes risk factors among rural residents of Andijan
Prediabetes is an intermediate hyperglycemic condition or a non-diabetic hyperglycemic state without symptoms or with minimal symptoms[1; С.60-67,2;
С.3-13,3; P.11–24]. In other words, it is a condition in which blood glucose levels are higher than normal but below the threshold for a clinical diagnosis of diabetes
Currently, prediabetes is increasingly recognized as an important metabolic condition, serving as a predictor of a high likelihood of future progression to manifest diabetes, with an annual conversion rate of 5-10% [4; С. 124-132, 5; P. 160–166, 6; P. 3329–3345, 7; P. 2279–2290]. Without medical intervention, prediabetes often progresses to diabetes. Even before the onset of diabetes, prediabetes is associated with an increased risk of cardiovascular diseases, cancer, kidney failure, neuropathy, and dementia. The rate of progression from prediabetes to diabetes is between 5% and 10% per year [8; P. 66–75], and 70% of people with prediabetes will develop diabetes during their lifetime, with a higher risk for individuals who are overweight or obese [9; P. 1538, 10; P. 603–613]
Several studies have examined the impact of different risk factors on the progression to type 2 diabetes (T2D). These include a family history of diabetes, obesity, low levels of high-density lipoprotein cholesterol (HDL), high systolic blood pressure (SBP), overall and abdominal obesity, tobacco smoking, gestational diabetes, and ethnicity. All of these factors are linked to an increased risk of developing T2D [11; С. 83-91, 12; P. 11–61, 13; P. 2062–2069, 14; P. 2622–31, 15; P. 67–79]
Therefore, prediabetes and diabetes should not be considered as safe conditions with regard to the acceleration of therapeutic management. Studies aimed at further uncovering the epidemiological mechanisms behind the development of these conditions and their risk factors will be invaluable for the early identification of individuals or subgroups at increased risk of developing diabetes and its complications.
The aim of this study is to investigate and evaluate the prevalence of non-lipid and lipid-related risk factors and their association with prediabetes in the adult rural male and female working-age population of Andijan.
Materials and Methods: The study was conducted in the Marhamat district of Andijan region among 2112 individuals, representing a 10% representative sample of the unorganized rural population: 1755 men and women (357). The sampling frame was based on the most recent electoral list of the studied region. A complex sampling method was used to form the sample, combining random and sequential sampling in accordance with the WHO and VNOA recommendations outlined in the 'Methodology for Organizing and Conducting Clinical Epidemiological Studies of the Adult Population for Identifying Chronic Non-Communicable Diseases' (2014; 2020), considering accumulated experience from population studies in preventive medicine. The movement of the population to the screening center followed the scheme presented in Figure 2: registration (primary examination form completed) → doctor’s office (screening questionnaire filled out, blood pressure and anthropometric measurements taken, calculation of body mass index (BMI), waist-to-hip ratio (WHR), assessment of prediabetes and diabetes risk factors, specialist recommendations)→ laboratory (blood collection for laboratory and biochemical tests) → biochemical laboratory (complete blood and urine analysis, determination of cholesterol (CH), triglycerides (TG), glucose, glycated hemoglobin, insulin in blood, HOMA-IR calculation). The examination concluded with the issuance of a final (epidemiological) diagnosis and the delivery of recommendations for the prevention of prediabetes and type 2 diabetes to the individuals involved in the study.
Epidemiological, clinical, biochemical, instrumental, and statistical methods were applied in the population study.
Blood glucose/glycemia levels are measured in the morning after fasting for 12 hours. Blood samples are collected in aseptic conditions from a vein (venous whole blood or plasma). The norms for glycemic disorders and diagnostic criteria for diabetes mellitus (DM), impaired glucose tolerance (IGT), and impaired fasting glucose (IFG) were based on WHO recommendations (1999-2013). Glycated hemoglobin (HbA1c) was also chosen as a diagnostic criterion for DM. HbA1c testing in venous blood was performed using the Mindray A88 analyzer with the reagent Max-Planck-Ring21 65205 Wiesbaden Germany, manufactured in Germany. This method of HbA1c determination is standardized according to the requirements of NGSP/DCCT and IFCC.
Results and Discussion: We studied the main risk factors for the development of prediabetes and type 2 diabetes (T2D) in the investigated rural population, including age (over 45 years), excess body weight and obesity (BMI ≥ 25 kg/m²), family history of diabetes (parents or siblings with T2D), gestational diabetes or a history of giving birth to a large baby. Other risk factors included hypertension (HTN), low physical activity, dyslipidemia, and the presence of comorbidities.
It was found that all individuals with glycemic disorders had increased body weight (Table 1).
Table 3.5
Epidemiological Characteristics of BMI in the Male and Female Population Aged 18-65 with Various Glucose Metabolism Disorders.
|
Study Participants |
BMI values, kg/m² |
||||
|
In case of IFG |
In case of IGT |
In case of IFG + IGT |
In case of T2D |
||
|
Male participants |
27,4+1,1 |
27,7+1,8 |
27,8+0,8* |
27,9+1,5 |
|
|
aged 18-65 (n=357) |
|||||
|
Female participants aged 18-65 (n=1755) |
28,2+0,8* |
28,5+0,9 |
28,7+0,5* |
28,5+2,5 |
|
|
Total participants (n=2112) |
26,5+1,2 |
26,8+2,1* |
26,8+1,2 |
27,2+1,8* |
BMI was observed in various disorders of body weight with the following indicators: in the case of IFG – 27.4 kg/m² (women – 28.2 kg/m² and men – 26.5 kg/m², P> 0.05), in the case of IGT – 27.7 kg/m² (women – 28.5 kg/m² and men – 26.8 kg/m²), in IFG+IGT – 27.8 kg/m² (women – 28.7 kg/m² and men – 26.8 kg/m², P>0.05), and in T2D – 27.9 kg/m² (women – 28.5 kg/m² and men – 27.2 kg/m², P>0.05). Overall, it is evident that BMI and obesity significantly contribute to the development of prediabetes and T2D, particularly among the rural female population.
In the representative sample of the rural population aged ≥ 18-65 years, 38.7% of participants reported having various forms of glycemic disorders related to irrational nutrition. The "irrational nutrition factor" was observed with varying prevalence among participants with glycemic disorders: in IFG – 41.5%, in IGT – 41.6%, in IFG+IGT and T2D – 41.5% and 29.9%, respectively (P<0.01).
As a risk factor, alcohol consumption was the least prevalent (1.4%) among those with carbohydrate metabolism disorders. Its prevalence was as follows: in IFG – 0.8%, in IGT – 1.1%, in IFG+IGT and T2D – 1.3% and 3.4%, respectively. Smoking prevalence was also lower (2.4%): in IFG – 2.5%, in IGT – 3.4%, in IFG+IGT and T2D – 3.1% and 9.2% (P>0.05).
Glycemic disorders were significantly more common in individuals with physical inactivity (46.9%). The prevalence of physical inactivity was as follows: in IFG – 47.7%, in IGT – 51.3%, in IFG+IGT and T2D – 47.8% and 48.3%, respectively (P<0.05).
In the case of glycemic disorders, the prevalence of hypertension (HTN) was observed in 30.3% of the participants, i.e., in every third individual. The highest prevalence of this risk factor was found among individuals with IFG – 76.5% (P<0.01), comparatively lower prevalence of hypertention(HTN) was found in impaired glucose tolerance (IGT) (19.9%), IFG+IGT and T2D (23.3% and 43.7%, respectively).
Dyslipidemia (DLP) in the studied rural population with glycemic disorders was found with a prevalence of 22.7%. As seen in Table 4.1, DLP was registered with the following prevalence in different glucose metabolism disorders: in IFG –
54.7%, in IGT – 51.3%, in IFG+IGT and T2D – 52.2% and 65.5%, respectively (P<0.05). The highest prevalence of glucose metabolism disorders was observed in individuals with excess body weight (70.0%). This risk factor was characterized by the following prevalence: in IFG – 64.2%, in IGT – 70.4%, in IFG+IGT and T2D – 71.7% and 70.1%, respectively (P<0.05).
Hyperglycemia in the medical history was identified with a prevalence of 12.7%. The prevalence of hyperglycemia in different glucose metabolism disorders was as follows: in IFG – 20.2%, in IGT – 27.0%, in IFG+IGT and T2D – 33.3% and 55.2%, respectively (P<0.05).
It was found that one in four individuals (25.9%) with glycemic disorders had coronary heart disease (CHD). The prevalence of CHD was as follows: in IFG – 48.6%, in IGT – 48.3%, in IFG+IGT and T2D – 46.5% and 49.4%, respectively (P<0.05).
It should be noted that timely identification of these risk factors can contribute to earlier active interventions and reduction of the risk of life-threatening complications of prediabetes and its "endpoints" (mortality, disability, thromboembolic and cardiovascular events). In the rural population of the studied region, non-modifiable risk factors for glycemic disorders also exhibited specific epidemiological characteristics.
As seen from the analysis presented in Table 4.2, non-modifiable risk factors (age ≥ 40 years, male and female gender, hereditary predisposition, gestational diabetes, stillbirth, giving birth to a large (>4 kg) baby) contributed to the development of glycemic disorders – IFG, IGT, IFG+IGT, and T2D.
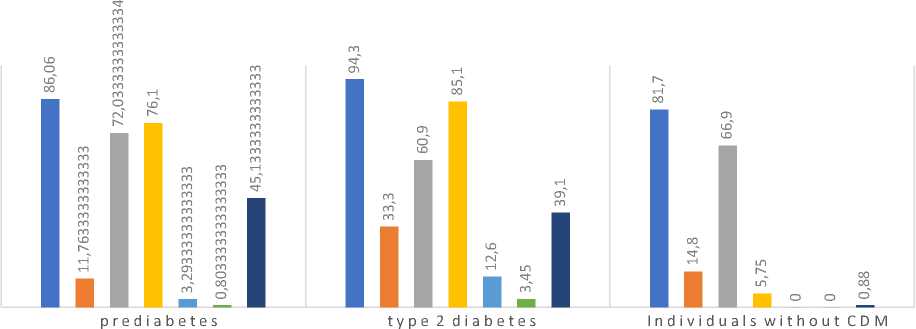
■ >40 years
■ Male
■ Female
■ Genetic predisposition
■ Gestational diabetes
■ Аbortion
Fig. 2. Development of Glycemic Disorders in the Rural Population under the Influence of Various Non-Modifiable Risk Factors
The results of our study showed that in the group of individuals aged ≥ 40 years, the prevalence of IFG was observed in 88.9%, IGT – 85.0%, IFG+IGT – 84.2%, and T2D – 94.3% (P<0.05). These glycemic disorders among the male and female populations were registered with the following prevalence rates, respectively: IFG – 14.4% and 67.8% (P<0.001), IGT – 8.9% and 76.0%, IFG+IGT – 11.9% and 72.3%, T2D – 33.3% and 60.9% (P<0.05).
The hereditary factor was associated with IFG in 65.8% of cases, with IGT in 83.9%, with IFG+IGT in 78.6%, and with T2D in 85.1% of cases (P<0.05). This risk factor was observed twice as often in individuals with T2D compared to those with prediabetes.
The prevalence of gestational diabetes in the medical history was 1.6% in individuals with IFG, 2.6% with IGT (P<0.05), 5.7% with IFG+IGT, and 12.6% with T2D (P<0.05).
The frequency of stillbirth was noted as 0.4% in IFG, 0.7% in IGT, 1.26% in IFG+IGT, and 3.45% in T2D (P<0.05).
The history of giving birth to a large baby (weighing more than 4 kg) was observed in 34.2% of cases with IFG, 52.8% with IGT, 48.4% with IFG+IGT, and 39.1% with T2D (P<0.01).