Kidney damage in COVID-19 patients
Автор: Abdurahimov Abduhalim Kholiddin, Alisher Kayumovich Shadmanov, Shagazatova Barno Habibullaevna, Hegai Lyubov Nikolaevna
Журнал: Re-health journal @re-health
Рубрика: Нефрология
Статья в выпуске: 2 (14), 2022 года.
Бесплатный доступ
Signs of kidney problems in patients with COVID-19 include high levels of protein or blood in the urine and abnormal blood work. Studies indicate more than 30% of patients hospitalized with COVID-19 develop kidney injury, and more than 50% of patients in the intensive care unit with kidney injury may require dialysis. Thus, in this article we will discuss kidney damage in COVID-19 patients.
Abnormal blood work, COVID-19, protein, urine, dialysis
Короткий адрес: https://sciup.org/14124676
IDR: 14124676
Текст научной статьи Kidney damage in COVID-19 patients
Introduction. The impact of COVID-19 on the kidneys is complex. Coronavirus might target kidney cells. The virus itself infects the cells of the kidney. Kidney cells have receptors that enable the new coronavirus to attach to them, invade, and make copies of itself, potentially damaging those tissues. Similar receptors are found on cells of the lungs and heart, where the new coronavirus has been shown to cause injury. Too little oxygen can cause kidneys to malfunction. Another possibility is that kidney problems in patients with the coronavirus are due to abnormally low levels of oxygen in the blood, a result of the pneumonia commonly seen in severe cases of the disease. Cytokine storms can destroy kidney tissue. The body’s reaction to the infection may be responsible as well. The immune response to the new coronavirus can be extreme in some people, leading to what is called a cytokine storm. When that happens, the immune system sends a rush of cytokines into the body. Cytokines are small proteins that help the cells communicate as the immune system fights an infection. But this sudden, large influx of cytokines can cause severe inflammation. In trying to kill the invading virus, this inflammatory reaction can destroy healthy tissue, including that of the kidneys. COVID-19 causes blood clots that might clog the kidneys. The kidneys are like filters that screen out toxins, extra water and waste products from the body. COVID-19 can cause tiny clots to form in the bloodstream, which can clog the smallest blood vessels in the kidney and impair its function.
The initial step of SARS-CoV-2 infection is its entry into the human cells. SARS-CoV-2 and SARS-CoV share a common ancestor resembling the bat coronavirus HKU9-1 [1]. These coronaviruses have very similar spike protein 3D structures considered to have a strong binding affinity to the human cell receptor, angiotensin-converting enzyme 2 (ACE2). Therefore, cells expressing ACE2 may be target cells and are thus susceptible to SARS-CoV-2 infection; such cells include alveolar type II cells of the lungs [2]. Thus, we believe that the pattern of ACE2 expression in different organs and tissues could reveal the potential risk for SARS-CoV-2 infection because the target cells expressing ACE2 may permit the entry, multiplication, spread, and pathogenesis of coronavirus. Previously, the RNA and protein expressions of ACE2 were investigated using bulk samples from the heart, lungs, kidneys, and other organs [3]. Therefore, SARS-CoV-2 can affect not only the lungs but also other organs, as well as cause organ failure in other organs, including the kidney.
Chu et al. [4] reported that of the 536 SARS patients analyzed, 36 (6.7%) had AKI, and in a study that analyzed 30 patients with Middle East respiratory syndrome coronavirus (MERS-CoV) infection, AKI occurred in eight (26.7%) [5]. In our study, 3 (4.5%) out of 66 patients had AKI, and they all recovered to normal SCr levels. Compared with previous human coronaviruses, such as MERS-CoV and SARS-CoV, SARS-CoV-2 infections were found to have a lower incidence of AKI. This is similar to the results of the analysis of 119 patients who were recently reported to have COVID-19 infection (AKI occurred in 0 out of 116 patients) [6]. In a metaanalysis of COVID-19 patients reported by Hu et al., [7] the results were similar to those of AKI occurring in 2.1% of patients.
In 20 patients, the urine PCR increased, and in 10 patients, the urine ACR increased. When the urine ACR is normal and the urine PCR is increased, renal tubular damage can be estimated in relation to infection rather than glomerular disease or glomerular damage [8,9]. Compared with a previous study on MERS-CoV infection, [10] SARS-CoV-2 infection exhibited less proteinuria (30.3%), suggesting that AKI and renal tubular damage caused by SARS-CoV-2 is less severe compared with previous coronavirus (MERS-CoV) infections (proteinuria occurred in 60% of patients). Our study revealed results similar to those reported recently on SARS-CoV-2 infection. In a study recently published by Wang et al., [11] dipstick tests were conducted on 111 SARS-CoV-2-infected patients (except for those with CKD), and 8 (7.2%) patients had trace or + albumin. This result is similar to that of the 9 (13.6%) out of 66 patients, in our study, whose dipstick tests revealed trace or + albumin.
This study had some limitations. The study population was selected from a single institution. All three patients with AKI underwent mechanical ventilation and ECMO, and it was difficult to distinguish whether AKI was caused by SARS-CoV-2 infection or was associated with treatments, such as ECMO and vancomycin [12]. Therefore, it is possible that the incidence of AKI related to COVID-19 was overestimated. In fact, all three patients used both ECMO and vancomycin, and AKI developed after vancomycin use [13]. Therefore, it is thought that AKI is more likely to be associated with the treatment than with SARS-CoV-2 infection, and the likelihood of AKI being associated with SARS-CoV-2 infection may be lower. In addition, when tubular damage, namely, acute tubular necrosis, occurred, a follow-up of more than 2–4 weeks after improvement of infection was considered sufficient [14]; however, due to insufficient followup, it was difficult to evaluate whether there was an improvement in proteinuria. Finally, it was difficult to tell whether it was proteinuria caused by kidney damage or functional proteinuria caused by fever and infection. In this study, tests for hematuria such as RBC count and dysmorphic RBC were not performed. However, hematuria was also found in eight out of 11 patients with severely increased proteinuria. As such, it can be assumed that the possibility of the proteinuria being due to kidney damage is higher than that of its being functional proteinuria.
Some group scientists [15] say in their own conclusion that COVID-19, which is caused by SARS-CoV-2 infection, is thought to have less effect on the kidneys than the lungs, where it leads to rapidly progressing lung lesions. In our study, there was a lower percentage of patients with AKI (4.5%) and moderately to severely increased proteinuria (30.3%) than in previous human coronavirus infections. Compared with the mortality rates of MERS-CoV and SARS-CoV infections, which are 34.4% and 9.6%, respectively, the mortality rate of SARS-CoV-2 infection is lower, which may be due to the less organ dysfunction it causes overall despite its effect on the lungs. Moreover, the highly infectious nature of SARS-CoV-2 infection, compared with MERS-CoV and SARS-CoV infections, and the rapid progression of lung lesions it causes make future research on vaccines and therapeutics of utmost importance.
Another group of scientists [16] is of the opinion that the main conclusion highlights that the novel coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2, is a global pandemic which is primarily considered a respiratory illness. However, emerging reports show that the virus exhibits both pulmonary and extra-pulmonary manifestations in humans, with the kidney as a major extra-pulmonary target due to its abundant expression of angiotensin-converting enzyme 2 and transmembrane protease serine 2, which facilitate entry of the virus into cells. Acute kidney injury has become prevalent in COVID-19 patients without prior any history of kidney dysfunction. In addition, the virus also worsens kidney conditions and increases mortality of COVID-19 patients with pre-existing chronic kidney disease, renal cancer, diabetic nephropathy, end-stage kidney disease as well as dialysis and kidney transplant patients. In the search for antiviral agents for the treatment of COVID-19, hydrogen sulfide (H2S), the third established member of gasotransmitter family, is emerging as a potential candidate, possessing important therapeutic properties including antiviral, anti-inflammatory, anti-thrombotic and antioxidant properties. A recent clinical study revealed higher serum H2S levels in survivors of COVID-19 pneumonia with reduced interleukin-6 levels compared to fatal cases. In this review, we summarized the global impact of COVID-19 on kidney conditions and discuss the emerging role of H2S as a potential COVID-19 therapy.
The global outbreak of the novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) has rapidly evolved into a global pandemic with enormous consequences. It has caused significant mortality and loss of capital, with a struggling global economy to contain the pandemic. This virus, which is the third zoonotic virus next to SARS-CoV and Middle East Respiratory Syndrome (MERS-CoV), was first identified in Wuhan, Hubei Province in China in December 2019, from where it has spread to all countries and territories of the globe. The initial signs of SARS-CoV-2 infection such as pneumonia, multiple organ failure and acute respiratory distress syndrome are elicited through the actions of the immune system. Various immunopathological changes in patients with SARS-CoV-2 infection have been documented in which lymphopenia, abnormalities in granulocytes and monocytes in serum as well as increase in cytokine production have been reported. These pathological changes seen in the upper respiratory tract is due to uncontrollable viral replication, leading to influx of neutrophils, macrophages and monocytes and elevated production of pro-inflammatory cytokines, the so-called cytokine storm syndrome. Current studies have shown that the kidneys are badly affected during SARS-CoV-2 infection, leading to kidney injury especially in patients with comorbidities, and worsening kidney conditions with increased mortality of COVID-19 patients with pre-existing chronic kidney disease, renal cancer, diabetic nephropathy, end-stage kidney disease as well as dialysis and kidney transplant patients. In the search for antiviral agents for the treatment of COVID-19, hydrogen sulfide (H2S), a gas known for its distinct “rotten-egg” smell and established as the third member of a family of gaseous signaling molecules, is emerging as a potential candidate [16-21].
As far as some group scientists go said [22] that symptomatic COVID-19 patients develop renal complications and patients with pre-existing renal conditions also have a high chance of disease progression and mortality. Currently, there are no approved drugs that offer renal protection in COVID-19 patients although ritonavir-boosted nirmatrelvir and remdesivir, and a number of vaccines have been approved by United States FDA for emergency use. With a new viral pandemic which has significant renal involvement, there is a need for future studies to determine the risk factors of kidney disease among COVID-19 patients. It is important to also determine the link between genetic polymorphisms and the risk of developing kidney diseases among certain races of people including those of African ancestry, who have genetic polymorphisms to kidney diseases, and to know whether there is an association between APOL1 high-risk carriers and risk of developing COVID-19-associated nephropathy. As the search for pharmacological agents for effective treatment of COVID-19 is underway, there are studies that are suggesting the potential clinical use of H2S donors, as these agents fall under all three classifications of COVID-19 treatment - antiviral treatment, cytokine storm treatment, and thrombosis treatment. A growing body of evidence show that H2S donors interact with ACE2, TMPRSS2 and other potential SARS-CoV-2 receptors on the host cell surface, alter SARS-CoV-2 membrane, thereby inhibiting the entry of the virus into the host cell and consequently preventing its replication (assembly and release). This mechanism is thought to suppress SARS-CoV-2-induced inflammatory pathway, leading to organ protection (Fig. 1). Other studies also suggest inhibition of gene transcription by H2S donors along with antiviral immunosuppressive effect. In the light of these mechanisms of the antiviral action of H2S donors, more experimental and clinical studies with H2S donors, especially those that are already FDA-approved and are in human clinical trials such as STS, NAC, ATB-346 and zofenopril, should be considered for preventive treatment or effective therapy against COVID-19 infection, and should include their use in nebulizer for aerosol inhalation into the lungs and dissemination to extra-pulmonary organs such as the kidney.
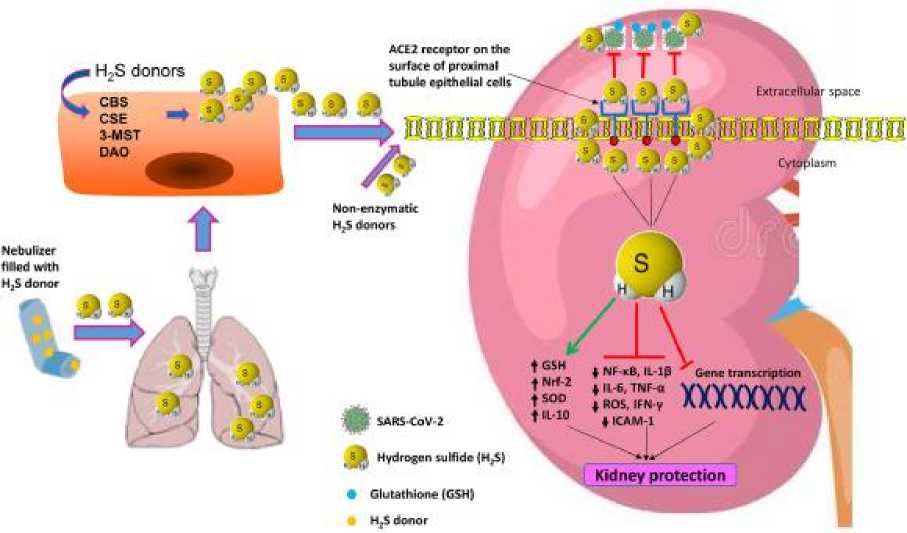
Figure 1. Possible mechanism of action of H 2 S against SARS-CoV-2.
Administration of H2S donors may increase endogenous production of H2S by cystathionine β-synthase (CBS), cystathionine γ-lyase (CSE), 3-mecaptopyruvate sulfurtransferase (3-MST) and d-amino acid oxidase (DAO) and may also activate non-enzymatic pathway. H2S interacts with angiotensin-converting enzyme 2 (ACE2) and TMPRSS2 (not shown) and may block the binding of SARS-CoV-2 to these host cell proteins, thereby inhibiting entry of the virus into the host cell. H2S may also alter SARS-CoV-2 membrane and inhibits its gene transcription including inhibiting the activation of nuclear factor-kappaB (NF-κB). In addition, H2S may activate antioxidant pathway, leading to increased levels of antioxidant enzymes such as glutathione (GSH), nuclear factor-erythroid factor 2-related factor 2 (Nrf2) and superoxide dismutase (SOD), and suppressing overproduction of reactive oxygen species (ROS). Furthermore, H2S may inhibit pro-inflammatory pathway, resulting in reduced production of pro-inflammatory mediators such as interleukin-1beta (IL-1β), IL-6, tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ) and intercellular adhesion molecule-1 (ICAM-1) while activating anti-inflammatory pathway which increases production of IL-10.
According to some [23] that COVID-19 is an emerging disease which affects various human organs including the kidneys, and the more severe the disease, the greater the risk of kidney involvement which worsens the prognosis. The exact mechanism by which SARS-CoV-2 induces acute kidney injury is unknown, but researchers believe that it directly and indirectly affects the kidney. The direct pathway is to bind the virus to ACE2 in the kidney, enter and destroy cells, disrupt the renin-angiotensin-aldosterone system balance, activate coagulation pathways, and damage the renal vascular endothelium. However, recent studies on kidney tissue biopsy specimens in the patients with COVID-19 and some autopsy have found evidence which indicates indirect pathway has a dominant role in AKI induction by SARS-CoV-2. Moreover, It was reported that ATI degree in autopsy specimens is milder compared to the degree of AKI. So it can be suggested that several factors, including ischemia, hypoxia, toxins, and other factors, may play a role in the development of AKI following COVID-19. In confirmation of this suggestion, most of the drugs used for the treatment in COVID-19 also have adverse effects on the kidneys and may have a synergistic effect with SARS-CoV-2 itself in inducing AKI. Therefore, it is better to use drugs which have the least harmful effect on the kidneys for the treatment in COVID-19. Recently, new variants of SARS-CoV-2 were identified; the most common are alpha, beta, gamma, and delta variants. All these variants have increased transmissibility and infectivity. It is not clear whether their effect on the kidneys is different from the wild type or not.
Although coronavirus primarily appears as an acute respiratory disease, it can affect other organs, including the kidneys, heart, gastrointestinal tract, blood, and central nervous system [24]. Coronavirus penetrates central nervous system through nerve cells, and it causes damage to the respiratory center, confusion, lethargy, disorientation, loss of senses of smell and taste in most patients, and other symptoms related to brain dysfunction [25]. Coronavirus in the kidney can cause AKI and other disturbances in kidney function [26]. Acute kidney injury is a condition which blood urea and creatinine concentrations increase via the retention of nitrogenous wastes, decrease GFR, as well as extracellular fluid volume and electrolyte homeostasis derangement [27]. Although AKI is an uncommon feature of SARS-CoV-2, it is known to be a fatal complication with early reports indicating 3–9% prevalence of AKI in the patients with COVID-19 [28]. However, subsequent studies reported that AKI incidence in hospitalized patients with COVID-19 is from 5% to 23%, and recent cohort studies have even reported an incidence of up to 46% which has reached 68% in ICU patients. Risk factors for AKI in COVID-19 include the need for mechanical ventilation, intubation, old age, diabetes mellitus, hypertension, severe illness, obesity, male gender, and chronic renal failure. However, some studies showed that the patients with COVID-19, in addition to AKI, also develop the glomerular disease because hematuria and proteinuria have also been detected in them [29].
The exact COVID-19 mechanism on kidney is not yet known, but researchers believe that SARS-CoV-2 directly and indirectly affects the kidney. Because SARS-CoV-2 is found in the urine, kidney damage pattern caused by the virus is limited to areas with ACE2 receptor, and the time course in which the virus appears in the urine coincides with the onset of AKI, so it was suggested that the virus directly affects the kidneys. The virus is claimed to enter the kidney cell by binding to membrane-bound ACE2 receptors in the glomerular podocyte cells and the apical membrane of proximal tubule cells, and in addition to damaging the kidney epithelial cells, it disarranges the balance of renin-angiotensin system. The angiotensinogen is primarily converted to angiotensin-I by renin and then to angiotensin-II under the influence of angiotensin-converting enzyme (ACE). Moreover, angiotensin-II is converted to angiotensin 1–7 by the ACE2 which dilates blood vessels. If SARS-CoV-2 occupies ACE2, angiotensin-II levels increase, leading to vasoconstriction, glomerular dysfunction, inflammation, and fibrosis. Recently Wang et al. and Chiu et al. found that SARS-CoV-2 also invades host cells via CD 147-spike protein pathway and this glycoprotein is highly expressed in proximal tubule. Moreover, SARS-CoV-2 causes kidney damage by activating inflammatory pathways and cytokine storm, activating coagulation pathways, damage to renal vascular endothelium, sepsis, hemodynamic instability as well as hypoxemia. Viral infection of endothelium via immune cell recruitment causes defective endothelial function and reduces the production of vasodilators, including the nitric oxide. Decreased vasodilators increase the response to vasoconstrictors and, together with ischemia-induced oxidative stress lead to AKI development [30-33]. Furthermore, there are different opinions about the timing of the onset of AKI symptoms in different studies. In a study conducted by Na et al. out of 66 patients with COVID-19, three cases showed AKI symptoms, all of which became apparent in the severe patients after the first week of hospitalization. Other studies have also reported the onset of AKI symptoms from days 5–9 after the hospitalization. However, in one case report, symptoms started on the second day of hospitalization, and in four other studies, there were symptoms at the time of admission [34,35].
Conclusion. In conclusion, in this article we have discussed kidney damage in COVID-19 patients. We have analyzed the opinions and conclusions of several scientists on this topic. We believe that this article can be an impetus for further in-depth research.
Список литературы Kidney damage in COVID-19 patients
- Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020; 63(3):457–460. PMID: 32009228.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579(7798):270–273. PMID: 32015507.
- Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020; 14(2):185–192. PMID: 32170560.
- Chu KH, Tsang WK, Tang CS, Lam MF, Lai FM, To KF, et al. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int. 2005; 67(2):698–705. PMID: 15673319.
- Cha RH, Joh JS, Jeong I, Lee JY, Shin HS, Kim G, et al. Renal complications and their prognosis in Korean patients with Middle East respiratory syndrome-coronavirus from the central MERS-CoV designated hospital. J Korean Med Sci. 2015; 30(12):1807–1814. PMID: 26713056.
- Wang L, Li X, Chen H, Yan S, Li D, Li Y, et al. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol. 2020; 51(5):343–348. PMID: 32229732.
- Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Virol. 2020; 127:104371. PMID: 32315817.
- Birn H, Christensen EI. Renal albumin absorption in physiology and pathology. Kidney Int. 2006; 69(3):440–449. PMID: 16514429.
- D'Amico G, Bazzi C. Pathophysiology of proteinuria. Kidney Int. 2003; 63(3):809–825. PMID: 12631062.
- Vinclair C, De Montmollin E, Sonneville R, Reuter J, Lebut J, Cally R, et al. Factors associated with major adverse kidney events in patients who underwent veno-arterial extracorporeal membrane oxygenation. Ann Intensive Care. 2020; 10(1):44. PMID: 32307616.
- Hsu CK, Wu IW, Chen YT, Tsai TY, Tsai FC, Fang JT, et al. Acute kidney disease stage predicts outcome of patients on extracorporeal membrane oxygenation support. PLoS One. 2020; 15(4):e0231505. PMID: 32268348.
- Sinha Ray A, Haikal A, Hammoud KA, Yu AS. Vancomycin and the risk of AKI: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2016; 11(12):2132–2140. PMID: 27895134.
- Deurdulian C, Tchelepi H. Imaging-based monitoring of the renal graft. In : Orlando G, Remuzzi G, Williams DF, editors. Kidney Transplantation, Bioengineering, and Regeneration. London: Academic Press;2017. p. 373–402.
- Cereda M, Neligan P, Shashaty MGS, Horak J. Renal diseases. In : Fleisher LA, editor. Anesthesia and Uncommon Disease. 6th ed. Philadelphia, PA: Saunders;2012. p. 225–250.
- Ki Ryang Na, Hae Ri Kim, Youngrok Ham, Dae Eun Choi, Kang Wook Lee, Jae Young Moon, Yeon-Sook Kim, Shinhye Cheon, Kyung Mok Sohn, Jungok Kim, Sungmin Kim, Hyeongseok Jeong, Jae Wan Jeon. Journal of Korean Medical Science 2020; 35(28): e257.doi.org/10.3346/jkms.2020.35.e257.
- M. Douglas, S.V. Katikireddi, M. Taulbut, et al. Mitigating the wider health effects of covid-19 pandemic response BMJ, 369 (2020), pp. 1-6.
- T.P. Velavan, C.G. Meyer. The COVID‐19 epidemic Trop. Med. Int. Health, 25 (3) (2020), pp. 278-280.
- S. Carriazo, M. Kanbay, A. Ortiz. Kidney disease and electrolytes in COVID-19: more than meets the eye Clin. Kidney J., 13 (3) (2020), pp. 274-280.
- S. Kudose, I. Batal, D. Santoriello, et al. Kidney biopsy findings in patients with COVID-
- J. Am. Soc. Nephrol., 31 (9) (2020), pp. 1959-1968.
- G. Pei, Z. Zhang, J. Peng, et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia . J. Am. Soc. Nephrol., 31 (6) (2020), pp. 1157-1165.
- R. Wald, S.M. Bagshaw. COVID-19–Associated acute kidney injury: learning from the first wave. J. Am. Soc. Nephrol., 32 (1) (2020), pp. 4-6.
- George J.Dugbartey, Karl K.Alornyo, Bright O.Ohenea, Vincent Boima Sampson, Antwic Alp Sener. Renal consequences of the novel coronavirus disease 2019 (COVID-19) and hydrogen sulfide as a potential therapy. doi.org/10.1016/j.niox.2022.01.002.
- Kidney injury in COVID-19 patients, drug development and their renal complications: Review study. Mohamadi Yarijani Z, Najafi H. DOI: 10.1016/j.biopha.2021.111966. PMID: 34333286 PMCID: PMC8313500.
- Desforges M., Le Coupanec A., Dubeau P., Bourgouin A., Lajoie L., Dubé M., Talbot P.J. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2020;12:14.
- Hossain M.F., Hasana S., Mamun A.A., Uddin M.S., Wahed M.I.I., Sarker S., Behl T., Ullah I., Begum Y., Bulbul I.J., Amran M.S., Rahman M.H., Bin-Jumah M.N., Alkahtani S., Mousa S.A., Aleya L., Abdel-Daim M.M. COVID-19 outbreak: pathogenesis, current therapies, and potentials for future management. Front. Pharm. 2020;11
- Brienza N., Puntillob F., Romagnolic S., Tritapeped L. Acute kidney injury in coronavirus disease 2019 infected patients: a meta-analytic study. Blood Purif. 2021;50:35–41. doi: 10.1159/000509274.
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062.
- Mohamadi M., Najafi H., Mohamadi Yarijani Z., Vaezi G.H., Hojati V. Protective effect of piperine in ischemia-reperfusion induced acute kidney injury through inhibition of inflammation and oxidative stress. J. Tradit. Complement Med. 2020;10:570–576.
- Najafi H., Mohamadi Yarijani Z., Changizi-Ashtiyani S., Mansouri K., Modarresi M., Madani S.H., Bastani B. Protective effect of Malva sylvestris L. extract in ischemia-reperfusion induced acute kidney and remote liver injury. PLoS One. 2017;12.
- Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., Li J., Yao Y., Ge S., Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838.
- Li Z., Wu M., Yao J., Guo J., Liao X., Song S., Li J., Duan G., Zhou Y., Wu X., Zhou Z., Wang T., Hu M., Chen X., Fu Y., Lei C., Dong H., Xu C., Hu Y., Han M., Zhou Y., Jia H., Chen X., Yan J. Caution on kidney dysfunctions of Covid-19 patients. medRxiv. 2020 doi: 10.1101/2020.02.08.20021212.
- Hirsch J.S., Ng J.H., Ross D.W., Sharma P., Shah H.H., Barnett R.L., Hazzan A.D., Fishbane S., Jhaveri K.D., C.Northwell COVID- Research, C.Northwell Nephrology COVID- Research Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218.
- Chan L., Chaudhary K., Saha A., Chauhan K., Vaid A., Zhao S., Paranjpe I., Somani S., Richter F., Miotto R., Lala A., Kia A., Timsina P., Li L., Freeman R., Chen R., Narula J., Just A.C., Horowitz C., Fayad Z., Cordon-Cardo C., Schadt E., Levin M.A., Reich D.L., Fuster V., Murphy B., He J.C., Charney A.W., Böttinger E.P., Glicksberg B.S., Coca S.G., Nadkarni G.N., (.Mount Sinai COVID Informatics Center Acute kidney injury in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 2021;32:151–160.
- Kant S., Menez S.P., Hanouneh M., Fine D.M., Crews D.C., Brennan D.C., Sperati C.J., Jaar B.G. The COVID-19 nephrology compendium: AKI, CKD, ESKD and transplantation. BMC Nephrol. 2020;21:449.
- Chu K.H., Tsang W.K., Tang C.S., Lam M.F., Lai F.M., To K.F., Fung K.S., Tang H.L., Yan W.W., Chan H.W., Lai T.S., Tong K.L., Lai K.N. Acute renal impairment in coronavirusassociated severe acute respiratory syndrome. Kidney Int. 2005;67:698–705.