Malnutrition in hospitalized children
Автор: Samanci S., Akdeniz O.
Журнал: Саратовский научно-медицинский журнал @ssmj
Рубрика: Педиатрия
Статья в выпуске: 2 т.18, 2022 года.
Бесплатный доступ
Objective: our study aimed to determine the prevalence and grade of malnutrition in patients hospitalized for various indications and to examine its relationship with comorbidities and socio-demographic factors. Material and methods. This study enrolled children aged 1 month to 15 years with a median (Q25; Q75) age of 1.8 (1.27-3.47) who were hospitalized in our hospital with various diagnoses between 1 January 2019 and 31 December 2019. Our study included 498 patients, 286 (57.4%) of which were male and 212 (42.6%) were female. Results. Forty (19.7%) patients with a median (Q25; Q75) age of 2.25 (1.27-3.48) years had a weight z-score of less than -2SD. According to the Waterlow classification, 47.2% (n=235) of the patients had malnutrition. There were significant differences between the groups regarding socioeconomic level and C-reactive protein (CRP) level. Conclusion. Malnutrition is associated with low socio-economic status. It plays an important role in hospitalizations for different reasons.
Children, malnutrition, waterlow and gomez classification
Короткий адрес: https://sciup.org/149141148
IDR: 149141148 | УДК: 616.39-008.46-071.3
Текст научной статьи Malnutrition in hospitalized children
1 Introduction. Nutrition is the bodily uptake and use of nutrients by humans in the amount necessary to achieve growth and development and to lead a healthy life cycle. The signs of malnutrition appears in humans with inadequate nutritional status. Malnutrition is defined as a ‘nutritional state that has measurable adverse effects on body shape, function, and clinical course as a result of a lack of energy, protein, or other nutrients’ [1]. Nutritional status directly affects a child’s growth and development, physical activity, intelligence, and social skills [2].
Although healthy nutrition is important at any age, it is known to determine the risk of disease and death and to affect quality of life. Malnutrition maintains its place at the top ranks of serious public health issues especially in underdeveloped and developing countries. According to the data of the World Health Organization (WHO) and the United Nations International Children’s Emergency Fund (UNICEF), one out of every four children worldwide is affected by malnutrition and approximately half of child deaths under the age of 5 are directly or indirectly related to malnutrition [3, 4]. While nutritional problems and infectious diseases have been pointed as the cause of malnutrition in developing countries like ours, trauma, surgical interventions, and chronic diseases are the primary causes in developed countries [5].
The signs of malnutrition in children may vary by the duration and severity of nutritional deficiency, dietary content and quality, and personal factors. Whereas malnutrition is easily diagnosed in severe/serious malnutrition, this task may be difficult in patients with mild-to-moderate malnutrition. In order to diagnose malnutrition, nutritional status should be checked, daily energy requirement should be calculated, and biochemical parameters should be measured [6, 7].
Preliminary planning for the early identification, correction and prevention of nutritional disorders in children can dramatically lower morbidity and mortality rates. Although domestic studies performed in different years have reported that the prevalence of malnutrition has been reducing, malnutrition currently maintains its importance [8].
Our study aimed to determine the prevalence and grade of malnutrition in patients hospitalized for various indications and to examine its relationship with comorbidities and socio-demographic factors.
Material and methods. This study enrolled 498 children aged 1 month to 15 years with a median (Q25; Q75)
age of 1.8 (1.27–3.47) who were hospitalized in our hospital with various diagnoses between 1 January 2019 and 31 December 2019. Patients younger than 1-month, intensive care patients, and patients under 2 years of age who had a history of low birth weight and prematurity were excluded.
The medical records of the patients were retrospectively examined to record personal data such as body weight, height, parental educational level, familial financial income, maternal number of gravida and parity, history and duration of breastfeeding, hospitalization diagnosis, length of hospitalization, and laboratory results. For body weight and height measurements, the reference values used in our country were taken as the reference. Age-adjusted z -scores were calculated for body weight and height measurements. For body weight and height z -scores, the reference standard deviation values for the same age and sex were used [9]. Patients with Z scores of –2SD or below were considered to have malnutrition. Antropometric, demographic, and laboratory values were compared by malnutrition status.
Malnutrition was evaluated using the Gomez and Waterlow classifications. According to the Gomez classification, patients with an age-adjusted body weight of 90-110% are considered normal; those with 75-89% mildly malnourished; those with 60-74% moderately malnourished; and those with < 60% severely malnourished [7]. According to the Waterlow classification, patients with a height-adjusted weight below 90% and those with age-adjusted height above 95% are considered to have acute malnutrition; those with height-adjusted weight above 90% and age-adjusted height below 95% are considered to have chronic malnutrition; and those with height-adjusted weight below 90% and age-adjusted height below 95% were considered to have acute on chronic malnutrition [6].
This study complied with the principles of the Helsinki Declaration. It was approved by SBU Diyarbakır Gazi Yaşargil Training and Research Hospital Ethics Committee (2019/390).
Statistical analysis. SPSS version 23.0 (software package for Windows) was used for the statistical analyses of the study data. Parametric continuous variables were presented as mean± standard deviation (SD), and the non-parametric ones as median (minimum-maximum). Conformity of the data to the normal distribution was assessed with histograms and skewness and kurtosis values between –1.5 and +1.5. Chi-square test was used for the comparison of categoric variables between paired groups and independent samples Student’s t test for the comparison of normally distributed variables. Mann — Whitney U test was used for non-normally distributed continuous variables. Multiple groups were compared using one-sided ANOVA test, and Tukey test as the post-hoc test. P<0.05 was considered statistically significant.
Results. Our study included 498 patients with a median (Q25 — Q75) age of 1.8 (1.27-3.47), 286 (57.4%) of which were male and 212 (42.6%) were female. Forty (19.7%) patients with a median (Q25 — Q75) age of 2.25 (1.27–3.48) years had a weight z -score of less than -2SD. According to the Waterlow classification, 47.2% ( n =235) of the patients had malnutrition; similarly, according to the Gomez classification, 47.2% ( n =235) of the patients had malnutrition. Among patients who were found to have malnutrition, the mean maternal age was 27.6±5.6 years. The comparison of the demographic and laboratory data of the patients were shown according to the Z score (Tabl. 1) and Waterlow classification (Tabl. 2). According to a correlation analysis, there was a negative correlation between parity and maternal education status, paternal education status, and socioeconomic level, and a positive correlation between parity and duration of breastfeeding ( p and r values, <0,001, <0,001, 0,007, <0,001, and –0,35, –0,25, –0,12, 0,23, respectively).
The patients were most commonly followed for acute gastroenteritis (40%) and respiratory tract infections (51.5%) (Fig. 1). The mean length of hospital stay was 4 (1–11) days (Fig. 2). The length of hospitalization was longer in those with respiratory tract infection compared with those who had AGE (5.1±2.2 days, 3.7±1.8 days; p<0,001), while there was no significant difference between the other groups. A weak negative correlation was found between the length of hospitalization and maternal educational level (p=0,049, r= –0,11).
According to the Gomez classification, 160 (32.1 %) patients had mild malnutrition, 53 (10.7%) moderate malnutrition, and 22 (4.4%) severe malnutrition. Severe malnutrition was most commonly seen in patients aged 1 month to 6 years (19 (3.8%) patients) (Tabl. 3). According to the Waterlow classification, 263 (52.8%) patients were normal, 156 (31.3%) had acute malnutrition, 22 (4.4%) had chronic malnutrition, and 57 (11.5%) had acute on chronic malnutrition (Tabl. 2). When the patients were divided into normal, acute malnutrition, chronic malnutrition, and acute on chronic malnutrition groups according to the Waterlow classification, it was found that the chronic malnutrition group had a greater mean age compared with the other groups. There was no significant difference between the groups in terms of length of hospitalization, duration of breastfeeding, gravida, and parity ( p >0.05). There was significant differences between the groups regarding socioeconomic level and CRP level ( p =0.09 ve p =0.07, respectively). In post-hoc Tukey test, the economic income of the acute on chronic malnutrition group was significantly lower than those without malnutrition ( p =0.011); CRP level was significantly higher in the patients with acute on chronic malnutrition than the normal and acute malnutrition
Table 1
Demographic data and malnutrition rates
|
Parameter |
Malnutrition patients |
Normal patients |
P value |
|
Age, years, median (min-max) |
2.25 (1.1–13.5) |
1.67 (1 ay–13 yıl) |
0.02¥ |
|
Sex, M/F |
21/19 |
265/193 |
0.5π |
|
Weight z -score, median (min-max) |
–2.29 ( (–5.4)–(–2.0)) |
–0.12 ( (–1.93)–(3.2)) |
0.001¥ |
|
Height z -score, median (min-max) |
–0.97 ((–6.7)–(0.83)) |
0 ( (–7.8)–(3.76)) |
0.001¥ |
|
Parity, mean±SD |
3 (1–9) |
3 (1–11) |
0.74¥ |
|
Gravida, mean±SD |
0.57¥ |
||
|
Maternal educational level, primary school or below/secondary school or above |
36/4 |
372/86 |
0.16 π |
|
Paternal educational level, primary school or below/secondary school or above |
31/9 |
304/154 |
0.15 π |
|
Income level, minimum wage or below/above minimum wage |
36/4 |
362/96 |
0.097 π |
|
Duration of breastfeeding, months, mean±SD |
14.6±8.1 |
14.3±7.3 |
0.8 t |
|
Length of hospitalization, days, median (minmax) |
4 (1–11) |
4 (1–15) |
0.72¥ |
|
Total protein, median (min-max) |
6.9 (1.4–9.5) |
6.9 (5.5–8) |
0.08¥ |
|
Albumin, median (min-max) |
3.9 (3–5) |
3.9 (2–9) |
0.55¥ |
|
Creatinine median (min-max) |
0.46 (0.33–0.74) |
0.43 (0.18–1.5) |
0.51¥ |
|
Uric acid, median (min-max) |
3.6 (2–11) |
4.2 (1–11) |
|
|
Hemoglobin, mean±SD |
11.6±1.3 |
11.4±1.4 |
0.46f |
|
CRP, median (min-max) |
40.8±61.7 |
25.5±48.5 |
0.2¥ |
|
Calcium, median (min-max) |
9.7 (8.8–11) |
9.7 (4–11.9) |
0.42¥ |
|
Phosphorus, mean±SD |
4.6±1.0 |
4.6±0.8 |
0.850f |
|
Iron, median (min-max) |
29 (9–94) |
23 (3–100) |
0.26¥ |
|
Total iron binding capacity, mean±SD |
278.8±81.8 |
317.8±63.9 |
0.006f |
N o t e s : n — Chisquare,f — Student’s t test,¥ — Mann-Whitney U test.
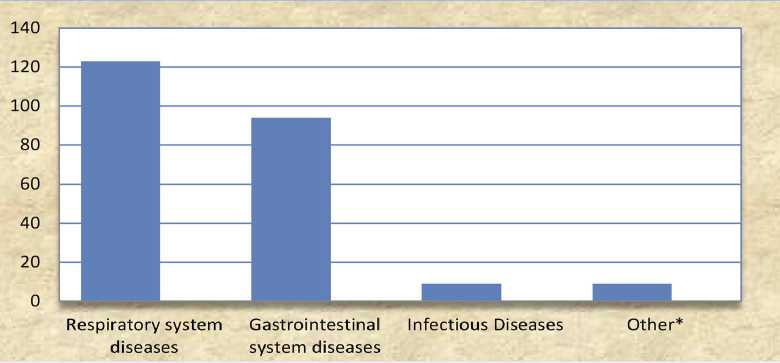
Fig. 1. Reasons for hospitalization: Respiratory System Diseases: Pneumonia, Bronchitis, Asthma, Upper Respiratory Diseases; Gastrointestinal diseases: Acute gastroenteritis, cow’s milk protein allergy, liver toxicity; infectious diseases: urinary tract infection, fever etiology; Other: Convulsion, Anemia
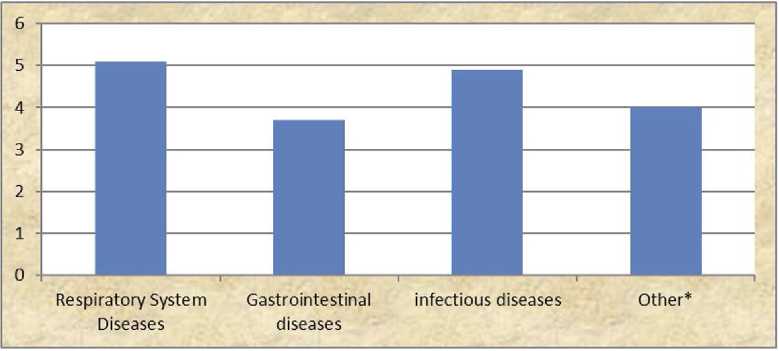
Fig. 2. Hospital stay (days): Respiratory System Diseases: Pneumonia, Bronchitis, Asthma, Upper Respiratory Diseases; Gastrointestinal diseases: Acute gastroenteritis, cow’s milk protein allergy, liver toxicity; infectious diseases: urinary tract infection, fever etiology; Other: Convulsion, Anemia
Table 2
Malnutrition and demographic parameters according to the Waterlow classification
|
Parameter |
Normal patients |
Acute Malnutrition |
Chronic Malnutrition |
Acute on chronic Malnutrition |
P value |
|
Age, years, median (min-max) |
1.68 (0.08–10.2) |
1.45 (1–10.6) |
2.29 (1.24–12.9) |
2.1 (0.1–13.5) |
0.001£ |
|
Sex, M/F |
168/95 |
80/76 |
12/10 |
26/31 |
0.017 € (a. b) |
|
Weight z -score, median (min-max) |
–0.12 ((–1.93) –(3.2)) |
–1.1 ((–176) –(1.3)) |
0.0 ((–1.6)–(0.9)) |
–1.6 ((–5.4)– (0.4)) |
0.001£ |
|
Height z -score, median (min-max) |
0 ((–7.8)–(3.76)) |
0.0 ((–1.8)–(1.7)) |
–0.4 ((–2.2)– (0.0)) |
–1.3 ((–7.9)– (0.0)) |
0.001£ |
|
Parity, mean±SD |
2.9±1.7 |
3.2±1.9 |
3.1±1.6 |
3.1±1.7 |
0.4 0 |
|
Gravida, mean±SD |
3.0±1.7 |
3.3±1.9 |
3.2±1.8 |
3.2±1.8 |
0.25 Ø |
|
Maternal educational level, primary school or below/secondary school or above |
208/55 |
133/23 |
18/4 |
49/8 |
0.35 € |
|
Paternal educational level, primary school or below/secondary school or above |
158/105 |
113/43 |
16/6 |
45/12 |
0.006 € (a. b) |
|
Income level, minimum wage or below/above minimum wage |
197/66 |
129/27 |
19/3 |
53/4 |
0.009 € (b) |
|
Duration of breastfeeding, months, mean±SD |
14.7±7.0 |
13.3±7.5 |
15.7±10.4 |
15.0±7.5 |
0.180 |
|
Length of hospitalization, days, median (min-max) |
4.0 (1–15) |
4.0 (1–10) |
4.0 (3–10) |
4.0 (1–11) |
0.77£ |
|
Total protein, median (min-max) |
6.9 (5.5–8) |
6.9 (6–8) |
6.8 (6–8) |
7 (6–8) |
0.29£ |
|
Albumin, median (min-max) |
3.9 (2–9) |
3.9 (3–9) |
4.0 (3–4) |
3.9 (3–5) |
0.29£ |
|
Creatinine median (min-max) |
0.43 (0.18–1.5) |
0.43 (0.33–1.1) |
0.45 (0.39–0.59) |
0.45 (0.18–1.5) |
0.19£ |
|
Uric acid, median (min-max) |
4.2 (1–11) |
4.1 (1–11) |
4.1 (1–7) |
3.9 (1–11) |
0.20£ |
End of tabl. 2
|
Parameter |
Normal patients |
Acute Malnutrition |
Chronic Malnutrition |
Acute on chronic Malnutrition |
P value |
|
Hemoglobin, mean±SD |
11.4±1.4 |
11.3±1.5 |
12.0±1.4 |
11.3±1.4 |
0.270 |
|
CRP, median (min-max) |
6.1 (0.0–284) |
5.6 (0.0–320) |
12.4 (0.7–161.3) |
10.0 (0.2–232.9) |
0.008£ |
|
Calcium, median (min-max) |
9.7 (4–11.9) |
9.7 (4–11.9) |
9.8 (9.2–10.2) |
9.7 (8–10.9) |
0.44£ |
|
Phosphorus, mean±SD |
4.6±0.8 |
4.5±0.7 |
4.7±0.8 |
4.6±0.8 |
0.80 |
|
Iron, median (min-max) |
23 (3–100) |
24 (5–100) |
24.5 (6–40) |
20 (5–94) |
0.28£ |
|
Total iron binding capacity, mean±SD |
319.3±67.4 |
305.6±68.6 |
331.2±66.3 |
312.1±50.5 |
0.330 |
Notes : € — Chi-square bonferroni correction, £ — Kruskal — Wallis test, 0 — One Way Anova test, a — significant between normal and acute malnutrition.
Table 3
Distribution of nutritional grades according to age and Gomez classification of cases
A weak negative correlation was found between weight Z score and gravida, parity, and a weak positive correlation with maternal educational status, paternal educational status, and socioeconomic level ( p and r values, 0.002, 0.005, <0.001, <0.001, 0.044 and –0.14, –0.12, 0.16, 0.19, 0.1, respectively). There was a negative correlation between duration of breastfeeding and maternal educational status, paternal educational status, and a positive correlation was found between the age at hospitalization and weight ( p and r values, 0.01, 0.009, <0.001, <0.001 and r values –0.11, –0.12, 0.22, 0.18, respectively).
Discussion. Malnutrition is responsible for more than half of all child deaths worldwide. It is the leading risk factor leading to morbidity and mortality especially among children under 5 years of age. Nearly 13 million children under the age of 5 die each year due to malnutrition [10]. Congenital developmental anomalies, malformations, persistent infections, and low socioeconomic level are important risk factors for developing malnutrition [11]. Among other important risk factors, parental educational level is the leading one. Since the mother assumes a greater role in the nutrition of children in our region, maternal educational level is particularly important. In our study, the correlation analysis between weight Z score and parental educational level revealed that as parental educational level is decreased, the malnutrition prevalence increased. This shows that malnutrition is a social problem beyond being a medical problem. The socioeconomic status of the family, access to food stuff, and hygienic conditions are important factors in the occurrence of malnutrition [12]. A study conducted in Malaysia reported that children who died in the region with the highest number of child deaths under the age of 5 were the children of mothers who did not have any income source, and malnutrition prevalence was higher in children of low-income mothers [13]. Our study re- vealed that the familial income was lower in patients with malnutrition tahn those without, although the difference was not statistically significant (p=0.09). The lack of statistical significance may have stemmed from our small sample size. Hence, an analysis between the malnutrition groups indicated that patients with acute on chronic malnutrition had a significantly lower income than the normal patients. This indicates the effect of income on the access to nutritional sources.
Malnutrition significantly increases morbidity and mortality among hospitalized children with malnutrition. In a study conducted on children under 3 years of age in 2011, S. G. Güleç et al. reported a malnutrition prevalence of 47.3%, and N. Ozer et al. found a malnutrition prevalence of 55.1 % among children aged 1-6 years [11]. A study by Genel et al. from Izmir revealed a malnutrition prevalence of 56.6%; among these, 21.3% had acute malnutrition, 24.2% chronic malnutrition, and 11.9% acute on chronic malnutrition [14]. According to our analysis of the status in different countries, R. J. Merrit, R. M. Suskind from the United States of America reported acute malnutrition in 26% of hospitalized children, chronic malnutrition in 38%, and acute on chronic malnutrition in 10.2% [15]. Looking at other countries, 16.5% acute malnutrition and 38.2% chronic malnutrition were reported in North Korea; 7.4% acute malnutrition and 60% chronic malnutrition were reported in Nigeria; and 31% mild malnutrition, 9% moderate malnutrition, and 1.6% severe malnutrition were reported in Jamaica [16]. In a malnutrition evaluation study on hospitalized children in Malaysia, nutritional deficiency was detected in 46% of children [13]. In a study dated 2017, which comprised all states of India, malnutrition was reported as the predominant risk factor for death among children under the age of 5, and the cause of death at a rate of 68.2% [17]. Similar to those studies, we detected a malnutrition prevalence of 47.2% among children hospitalized for various reasons. According to the Gomez classification, 10.7% of our patients had moderate mal- nutrition and 4.4% had severe malnutrition. According to the Waterlow classification, 156 (31.3%) patients found to have malnutrition were classified as acute malnutrition, 22 (4.4%) as chronic malnutrition, and 57 (11.5%) as acute on chronic malnutrition. In the light of the above data, it can be stated that the global malnutrition prevalence remains high among hospitalized patients, particularly among children under the age of 5, it may show regional variations, and the level of socioeconomic development of the country and the region is its underlying determinant.
It is known that lifestyle variability between countries, socioeconomic indicators, distribution of food stuffs, food quality, nutritional habits, and the educational and cultural level play important role in malnutrition development rates. Intervening infections are another factor that can aggravate the malnutrition process. As malnutrition affects many systems, it also causes impaired cellular and humoral immunity, phagocyte dysfunction, dysfunctional complement system, reduced cytokine production, protein production and destruction, and especially a decrease in secretory immunoglobin A antibody level in the immune system [18]. The longer the process, the more severe the immune system is affected. It is known that chronic malnutrition increases the susceptibility of children to infections and causes a more serious disease course. In our study, a more prominent increase in CRP level was observed in children with acute on chronic malnutrition; we believe that this finding can be explained by increased susceptibility to infections in the chronic process.
Infections, especially acute gastroenteritis, respiratory infections, recurrent infections, and chronic disorders can cause malnutrition by impairing a child’s nutrition and causing catabolism. S. G. Güleç et al. reported that they detected infection in 74.7% of cases with malnutrition. In our study, infections existed in 68.1% of our malnourished patients. At the same time, most frequent hospital admissions were due to respiratory system infections with a rate of 51.5%, which can be explained by suppressed immunity and reduced secretory IgA levels [8].
The length of hospitalization appears to be longer in patients with malnutrition than those without. In a study conducted in the United States of America in 2010, the length of hospitalization was 2.5 times longer and hospital costs 3 times higher in children with malnutrition [19]. In our study, the mean length of hospitalization was 4 days, with patients hospitalized for respiratory system diseases having the longest hospitalization (5.1 days).
A comparison of maternal educational level showed that as maternal educational level decreased, the length of hospitalization increased. The number of pregnancies also plays an important role in the development of malnutrition. M. Aykut et al. reported that the rate of malnutrition was higher in regions where the socioeconomic level was lower and the number of previous pregnancies was higher compared with other regions [20]. Our study yielded similar results, so that the number of parity and gravida were higher in the groups having malnutrition. It was shown that the cases with higher numbers of gravida and parity were fed with breast milk for a longer period of time. Here emerges a paradox of having more children and longer breastfeeding as education levels drop and families become poorer. When the number of children is high and the parents are uneducated and poor, breastfeeding for a long time seems to be a necessity due to economic reasons rather than a conscious approach. A positive correlation was found between the duration of breastfeeding and the age, weight, and hemoglobin level at hospitalization. The facts that patients who are breastfed for a long time suffer malnutrition at a later age, have higher hemoglobin levels, are overweight, and get ill later, highlight the protective effect of breastfeeding.
Conclusion. Malnutrition is associated with low socio-economic status. It plays an important role in hospitalizations for different reasons. Parental educational level, breastfeeding status, gravida and parity play important role in its development. It is necessary to raise awareness of families about nutrition, to encourage breast milk intake, to ensure the transition to complementary foods at the right time and with the right foods, and to inform people about the hygiene rules. Anthropometric measurements should be made and evaluated periodically in family medicine offices and pediatric outpatient clinics. Early recognition and treatment of malnutrition will reduce morbidity and mortality as well as hospitalization rates and patient costs.
Conflict of ınterest. The authors have no conflicts of interest to declare.
Список литературы Malnutrition in hospitalized children
- Joosten KF, Hulst JM. Malnutrition in pediatric hospital patients: currentis sues. Nutrition 2011; (27): 133–7.
- King C, Davis T. Nutritional treatment of infants and children withf altering growth. Eur J Clin Nutr 2002; (64): 11–3.
- WHO, World health statistics 2018: monitoring health fort the SDGs. Geneva: WHO, 2018.
- UNICEF. Malnutrition in chidren. URL: http://data.unicef.org / topic / nutrition / malnutrition (3 Sep 2019).
- Meakins JL, Pietsch JB, Bubenick O, et al. Delayed hypersensitivity: Indicator of acquired failure of host defenses sissepsis and trauma. Ann Surg 1997; (186): 241–6.
- Waterlow JL. The presentation and use of height and weight data for companing the nutritional status of groups of children under the age of 10 years. Bull WHO 1977; (5): 489.
- Gomez SF, Ramos GR, Frenk S, et al. Mortality in second and third degree malnutrition. J Trop Pediatr 1956; (2): 77–87.
- Güleç S. G, Urgancı N, Polat S, et al. Hastanede yatan üç yaş altı çocuklarda malnütrisyon durumunun değerlendirilmesi. Şişli Etfal Hastanesi Tıp Bülteni Cilt 2011; 45: sayı: 4.
- Neyzi O, Günöz H, Furman A, et al. Türk Çocuklarında vücut ağırlığı, boy uzunluğu, baş çevresi ve vücut kitle indeksi referans değerleri. Çocuk Sağlığı ve Hastalıkları Dergisi 2008; (51): 1–14.
- Blossner M, de Onis M. Malnutrition: quantifying the health impactat national and local levels. Geneva, Switzerland: World Health Organization, 2005; 43 p.
- Özer N, Urgancı N, Usta A, Kayaalp N. Hastanede yatan çocuklarda malnütrisyon durumunun değerlendirilmesi. T Klin J Pediatr 2001; (10): 133–8.
- Oztürk Y, Büyükgebiz B, Arslan N, Ellidokuz H. Effects of hospitalstay on nutritional anthropometric data in Turkish children. J Trop Pediatr 2003; (49): 189–90.
- Ong SH, Chee WSS, Lapchmanan LM, et al. Validation of the Subjective Global Nutrition Assessment (SGNA) and Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP) to Iden tify malnutrition in hospitalized Malaysian children. J Trop Pediatr 2019; 65 (1): 39–45. DOI: 10.1093 / tropej / fmy009.
- Genel F, Atlıhan F, Bak M. Hastanede yatan olgularda malnütrisyon ve anemi prevalansı. T Klin Pediatr 1997; (6): 173–7.
- Merritt RJ, Suskind RM. Nutritional survery of hospitalized pediatric patients. Am J Clin Nutr 1979; (32): 1320–5.
- Katana-Apte J, Mokdad A. Malnutrition of children in the Democratic People’s Repuplic of Nort Korea. J Nutr 1998; (128): 1315–9.
- Dandona L. Public Health Foundation of India. The burden of child and maternal malnutrition and trends in its indicators in thestates of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Health 2019; 3 (12): 855–70.
- Savino W, Dardenne M. Nutritional imbalances and infections affect the thymus: consequences on T-cell-mediated immune responses. ProcNutrSoc 2010; (69): 636–43.
- Abdelhadi RA, Bouma S, Bairdain S, et al. Characteristics of hospitalized children with a diagnosis of malnutrition: United States, 2010.
- Aykut M, Ceyhan O, Öztürk Y, Günay O. Kayseri sağlık grup başkanlığı bölgesinde 3–36 aylık çocuklarda malnütrisyon durumu. Türk Hijyen ve Deneysel Biyoloji Dergisi 1987; 44 (2): 223–39.


