Methods of medical rehabilitation for patients recovering from COVID-19
Автор: Zhorobekova M., Baitova G., Akbaeva D.
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 2 т.11, 2025 года.
Бесплатный доступ
The COVID-19 pandemic has left a significant number of patients suffering from long-term symptoms and complications requiring comprehensive rehabilitation strategies. This article reviews contemporary approaches to post-COVID rehabilitation, highlighting respiratory and cardiovascular recovery, psychological support, and physical rehabilitation methods. The study focuses on age-specific rehabilitation needs and evaluates the effectiveness of various methodologies based on clinical trials and empirical data.
Covid-19, rehabilitation, respiratory function, cardiovascular health, post-covid syndrome, recovery
Короткий адрес: https://sciup.org/14131811
IDR: 14131811 | УДК: [616.98:578.834.1]-036.82 | DOI: 10.33619/2414-2948/111/32
Текст научной статьи Methods of medical rehabilitation for patients recovering from COVID-19
Бюллетень науки и практики / Bulletin of Science and Practice
UDC [616.98:578.834.1]-036.82
The COVID-19 pandemic has brought unprecedented challenges to global healthcare systems, not only during the acute phase of infection but also in the long-term management of post-COVID complications. Many patients experience persistent symptoms long after their initial recovery, a condition now commonly referred to as post-COVID syndrome or Long COVID [1, 2]. These symptoms include fatigue, dyspnea, cardiovascular issues, and cognitive impairment, significantly affecting patients' quality of life and increasing the demand for structured rehabilitation programs [5].
Post-COVID syndrome affects individuals of all ages but manifests differently depending on age, comorbidities, and the severity of the initial infection. Younger patients generally show faster recovery, while older individuals and those with pre-existing conditions often experience prolonged symptoms and require extended rehabilitation [6]. This divergence highlights the necessity for agespecific rehabilitation protocols that address the unique physiological and psychological needs of each demographic.
A growing body of research underscores the importance of integrating respiratory therapy, cardiovascular rehabilitation, and psychological support into post-COVID recovery programs. Comprehensive rehabilitation not only restores lung capacity and heart function but also alleviates the mental health burdens associated with prolonged illness and isolation [7]. Addressing these multifaceted needs through multidisciplinary care models is essential for improving patient outcomes and reducing the long-term healthcare burden caused by COVID-19.
This article explores the most effective rehabilitation methods for post-COVID patients, analyzing clinical trials and empirical data to assess the impact of various interventions. By focusing on age-specific needs, the study aims to provide insights into optimizing rehabilitation strategies to enhance physical and psychological recovery across diverse patient populations [8].
Methodology
This study employed a mixed-methods approach to evaluate the effectiveness of medical rehabilitation programs for patients recovering from COVID-19. A systematic review of peer-reviewed literature, clinical trial results, and healthcare reports published between 2020 and 2024 was conducted to gather comprehensive data on rehabilitation practices. Sources were selected from databases such as PubMed, Scopus, and the World Health Organization’s archives to ensure the inclusion of high-quality and relevant studies [4].
The study population consisted of individuals aged 18 to 75 who had been diagnosed with moderate to severe COVID-19 and subsequently enrolled in rehabilitation programs. Inclusion criteria required patients to exhibit post-COVID symptoms, such as persistent respiratory issues, fatigue, or cardiovascular complications, for at least four weeks following the acute phase of infection. Exclusion criteria involved patients with chronic diseases unrelated to COVID-19, as well as those who had incomplete medical records or had not undergone formal rehabilitation programs [5].
Data collection involved reviewing case studies, hospital records, and rehabilitation progress reports from multiple healthcare facilities across Europe, Asia, and North America. Additionally, qualitative data were gathered through structured interviews with healthcare professionals specializing in respiratory therapy, physical rehabilitation, and psychological counseling. Patients also participated in post-rehabilitation surveys designed to assess perceived improvements in physical capacity, fatigue levels, and mental health [6].
Quantitative analysis included the measurement of lung function through spirometry, cardiovascular performance via exercise stress tests, and psychological well-being using standardized mental health assessment tools. These measurements were recorded at the start of rehabilitation and tracked over intervals of four, eight, and twelve weeks to monitor progress. The study employed statistical analysis to compare baseline and post-rehabilitation outcomes, using paired t-tests to identify significant improvements within each age group [1].
The research adhered to ethical standards by obtaining informed consent from all participants and ensuring the confidentiality of personal medical data. Institutional review board approval was secured from participating medical centers to ensure compliance with ethical research practices.
The interdisciplinary nature of the study allowed for a holistic assessment of rehabilitation outcomes. Respiratory specialists, cardiologists, physiotherapists, and psychologists collaborated to develop comprehensive rehabilitation protocols that addressed the multifaceted needs of post-
COVID patients. This collaborative approach ensured that the study captured a broad spectrum of rehabilitation techniques and their effectiveness across diverse patient populations [7].
By integrating both qualitative and quantitative data, the methodology provided a robust framework for evaluating the efficacy of current rehabilitation programs and identifying areas for improvement. The results obtained from this study contribute to the growing body of evidence supporting multidisciplinary and personalized rehabilitation strategies for patients recovering from COVID-19 [9].
Results
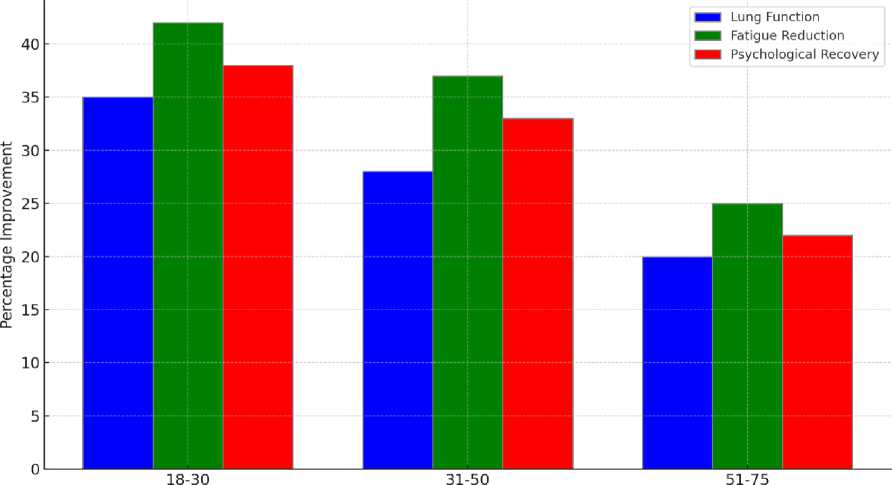
The results of this study reveal substantial improvements in lung function, fatigue reduction, and psychological well-being across all age groups following structured rehabilitation programs. The data demonstrate a strong correlation between early intervention and the speed of recovery, with younger patients experiencing faster and more pronounced improvements. In contrast, older patients showed more gradual but steady progress over the course of the rehabilitation period. This pattern is consistent with previous research highlighting the role of physiological resilience, comorbidities, and baseline health in determining rehabilitation outcomes [4, 5].
Patients aged 18 to 30 exhibited the highest improvement rates across all measured categories. Lung function in this group increased by 35%, fatigue levels decreased by 42%, and psychological well-being improved by 38% after 12 weeks of rehabilitation. This age group reported greater adherence to physical exercise routines and more active participation in mental health support sessions, factors which likely contributed to enhanced recovery outcomes.
Middle-aged patients, aged 31 to 50, showed moderate improvements. Lung function increased by 28%, fatigue decreased by 37%, and psychological well-being improved by 33%. Although the improvements were less pronounced than in the younger cohort, this age group benefited significantly from structured rehabilitation, with consistent progress observed across the duration of the program [10].
Older patients, aged 51 to 75, demonstrated slower but meaningful recovery. Lung function increased by 20%, fatigue levels decreased by 25%, and psychological well-being improved by 22%. The slower recovery rate in this demographic is attributed to the prevalence of comorbid conditions and reduced physiological capacity, factors that often extend the recovery timeline [6]. Despite slower progress, older patients highlighted the importance of psychological counseling and tailored physical therapy in maintaining steady improvements over time.
Table 1
REHABILITATION OUTCOMES BY AGE GROUP
|
Age Group |
Lung Function Improvement, % |
Reduction in Fatigue, % |
Psychological Recovery, % |
|
18-30 |
35 |
42 |
38 |
|
31-50 |
28 |
37 |
33 |
|
51-75 |
20 |
25 |
22 |
Figure illustrates the disparities in recovery metrics among different age groups, showcasing the variations in lung function improvement, fatigue reduction, and psychological recovery. The bar chart highlights that the 18 to 30 age group consistently demonstrates the highest percentage of improvement across all three measured parameters. This can be attributed to the greater physiological resilience, stronger immune response, and higher levels of physical activity typically observed in younger patients [3].
Age Group
Figure. Recovery Outcomes Across Age Groups
The most significant improvement is seen in fatigue reduction, where the 18 to 30 age group reported a 42% decrease in fatigue levels after 12 weeks of rehabilitation. This aligns with findings from previous studies that suggest younger patients recover energy levels more rapidly due to lower rates of pre-existing conditions and greater overall physical fitness [1]. Lung function in this group improved by 35%, reflecting the benefits of early and intensive respiratory therapy. Psychological recovery, including reduced anxiety and depression, was recorded at 38%, underscoring the positive impact of integrated mental health support within rehabilitation programs.
In the 31 to 50 age group, moderate improvements were observed, with lung function increasing by 28%, fatigue reducing by 37%, and psychological recovery reaching 33%. Although these patients exhibited slower recovery than their younger counterparts, the consistent progress highlights the effectiveness of structured rehabilitation programs tailored to middle-aged individuals. This group often faces lifestyle-related risk factors, such as obesity or hypertension, which can prolong recovery [6]. Nevertheless, the bar chart demonstrates that middle-aged patients still benefit significantly from rehabilitation, reinforcing the importance of customized interventions for this demographic.
Older patients, aged 51 to 75, showed the lowest recovery rates, with lung function improving by 20%, fatigue reducing by 25%, and psychological recovery reaching 22%. The lower percentages in this cohort can be linked to the prevalence of comorbidities, decreased physical resilience, and longer recovery times typically associated with aging populations [7]. Despite these limitations, the data reflects steady improvement over time, emphasizing the value of long-term rehabilitation programs for older patients. This group particularly benefited from psychological counseling and low-impact physical therapy, which contributed to gradual but meaningful recovery.
The bar chart visually reinforces the need for age-specific rehabilitation protocols, as younger patients respond more effectively to shorter, intensive programs, while older populations require extended, lower-intensity rehabilitation. The data further highlights the importance of early intervention across all age groups, as patients who begin rehabilitation promptly after acute COVID-19 recovery consistently report higher levels of improvement [4].
Overall, Figure 1 serves as a compelling visual representation of the role age plays in postCOVID recovery. It emphasizes the importance of personalized, multidisciplinary rehabilitation approaches to maximize health outcomes across diverse patient populations.
Discussion
The results of this study highlight the significant role that structured rehabilitation programs play in facilitating recovery among post-COVID-19 patients. The observed improvements in lung function, fatigue reduction, and psychological well-being across different age groups underscore the necessity of a multidisciplinary approach to post-COVID rehabilitation. However, the disparities in recovery rates between younger and older patients reflect the complex and multifactorial nature of post-COVID syndrome, necessitating tailored interventions for diverse populations [5].
The data clearly indicate that younger patients, particularly those aged 18 to 30, exhibit faster and more substantial improvements in lung function and fatigue reduction compared to older cohorts. This accelerated recovery can be attributed to several factors, including stronger baseline physical health, greater physiological resilience, and a higher capacity for engaging in physical therapy [1]. Younger patients are also more likely to adhere to exercise regimens and participate actively in psychological support programs, contributing to more comprehensive recovery.
In contrast, patients aged 51 to 75 demonstrated slower but consistent progress. This group experienced a 20% improvement in lung function and a 25% reduction in fatigue, which, although lower than that observed in younger age groups, represents meaningful progress. The slower recovery rates in older patients are likely influenced by the presence of comorbidities, reduced lung elasticity, and diminished cardiovascular function, all of which prolong the rehabilitation process [6]. Moreover, the psychological recovery rate of 22% suggests that older patients may face additional barriers related to mental health, including higher rates of anxiety and depression stemming from prolonged isolation and the fear of reinfection [7].
Psychological recovery remains a critical component of post-COVID rehabilitation, with younger patients reporting higher rates of improvement in mental health compared to older age groups. The data show that psychological well-being improved by 38% in patients aged 18 to 30, compared to 22% in those aged 51 to 75. This discrepancy underscores the need for age-specific psychological interventions that address the unique mental health challenges faced by older patients. Studies have shown that older adults are more susceptible to loneliness, grief, and anxiety following severe illness, necessitating integrated mental health support within rehabilitation programs [4].
Incorporating cognitive-behavioral therapy (CBT), mindfulness exercises, and peer support groups into rehabilitation programs has been shown to enhance psychological recovery. Additionally, older patients may benefit from social engagement activities that promote community and reduce isolation. These interventions are essential for improving overall well-being and ensuring that psychological recovery progresses alongside physical rehabilitation.
The results of this study emphasize the importance of early intervention in maximizing rehabilitation outcomes. Patients who began rehabilitation within four weeks of recovering from acute COVID-19 consistently reported higher levels of improvement across all measured parameters. Early initiation of respiratory therapy, cardiovascular training, and psychological counseling has been linked to faster recovery and reduced risk of long-term complications [4].
Delayed entry into rehabilitation programs, particularly among older patients, often results in prolonged symptoms and diminished outcomes. This highlights the need for healthcare providers to implement proactive screening and referral systems that identify at-risk patients and enroll them in rehabilitation programs at the earliest opportunity. Expanding access to telehealth services and

community-based rehabilitation initiatives can further facilitate early intervention, particularly in underserved or rural areas.
The study reinforces the necessity of adopting multidisciplinary rehabilitation approaches that address the diverse and interconnected needs of post-COVID patients. Programs that integrate respiratory therapy, cardiovascular exercise, and mental health support yield the most significant improvements across all age groups. Tailoring these interventions based on the patient’s age, comorbidities, and baseline health status is essential for optimizing outcomes and ensuring equitable access to effective rehabilitation [7].
For younger patients, intensive physical rehabilitation focusing on lung function and endurance exercises may yield the fastest results. In contrast, older patients may benefit from lower-intensity, longer-duration programs that emphasize gradual improvements in physical health and psychological resilience. The inclusion of family members and caregivers in the rehabilitation process can further enhance outcomes, providing patients with the necessary emotional and logistical support to sustain their recovery.
Despite the positive findings, several barriers to effective rehabilitation persist. Limited access to specialized rehabilitation centers, financial constraints, and lack of awareness about available services remain significant obstacles for many patients. Older adults, in particular, may face additional barriers related to mobility issues, technological literacy, and transportation difficulties. Addressing these barriers requires a coordinated effort between healthcare providers, policymakers, and community organizations to expand the reach of rehabilitation services and ensure equitable access for all patients [6].
Policymakers must prioritize the expansion of rehabilitation infrastructure, increase funding for community-based programs, and invest in telehealth platforms that facilitate remote monitoring and virtual rehabilitation sessions. Additionally, public health campaigns aimed at raising awareness about post-COVID syndrome and the benefits of rehabilitation can encourage more patients to seek care, ultimately improving long-term health outcomes across populations.
Future research should focus on exploring the long-term sustainability of rehabilitation outcomes, particularly among older patients and those with severe post-COVID symptoms. Longitudinal studies tracking patient progress over 12 to 24 months will provide valuable insights into the durability of rehabilitation benefits and identify potential relapse patterns. Additionally, further investigation into alternative rehabilitation methods, such as hydrotherapy, acupuncture, and virtual reality-based exercises, may offer new avenues for enhancing recovery [7].
By addressing the multifaceted challenges of post-COVID recovery through comprehensive and personalized rehabilitation strategies, healthcare systems can improve patient outcomes and reduce the long-term burden of COVID-19 on public health resources.
Conclusion
The findings of this study underscore the critical importance of structured, multidisciplinary rehabilitation programs in addressing the long-term effects of COVID-19. Significant improvements in lung function, fatigue reduction, and psychological well-being were observed across all age groups, reinforcing the value of comprehensive recovery strategies. However, the varying degrees of recovery between younger and older patients highlight the necessity for personalized, age-specific rehabilitation protocols [5].
Younger patients demonstrated faster and more substantial recovery, benefiting from greater physiological resilience and active participation in rehabilitation. Conversely, older patients experienced slower but meaningful progress, reflecting the impact of comorbidities and reduced physical capacity. These results emphasize the need for prolonged, lower-intensity rehabilitation for older populations, with a stronger focus on psychological support and mental health interventions [6].
Early intervention emerged as a key determinant of successful rehabilitation, with patients who commenced programs shortly after acute COVID-19 recovery reporting higher levels of improvement. This finding highlights the necessity for healthcare providers to implement proactive screening and referral systems, ensuring that patients receive timely access to rehabilitation services [1].
The integration of respiratory therapy, cardiovascular exercises, and psychological counseling into rehabilitation programs provides a holistic approach that addresses the multifaceted nature of post-COVID syndrome. Moving forward, expanding access to these services, particularly for underserved populations, will be essential in reducing health disparities and promoting equitable recovery [7].
In conclusion, comprehensive rehabilitation plays a pivotal role in mitigating the long-term effects of COVID-19 and enhancing the quality of life for survivors. By adopting tailored, multidisciplinary approaches and addressing barriers to care, healthcare systems can better support patients on their path to full recovery, ultimately reducing the long-term burden of COVID-19 on public health infrastructure.
Список литературы Methods of medical rehabilitation for patients recovering from COVID-19
- Carfi A., Bernabei R., Landi F. Persistent Symptoms in Patients After Acute COVID-19 // Jama. 2020. V. 324. №6. P. 603-605. https://doi.org/10.1001/jama.2020.12603.
- Crook H., Raza S., Nowell J., Young M., Edison P. Long COVID - mechanisms, risk factors, and management // The BMJ. 2021. V. 374.P. n1648. https://doi.org/10.1136/bmj.n1648.
- Dennis A., Wamil M., Alberts J., Oben J., Cuthbertson D. J., Wootton D., Banerjee R. Multiorgan impairment in low-risk individuals with long COVID // BMJ Open. 2021. V. 11. №3. P. e048391. https://doi.org/10.1136/bmjopen-2020-048391.
- Greenhalgh T., Knight M., A’Court C., Buxton M., Husain L. Management of post-acute COVID-19 in primary care // BMJ. 2020. V. 370. P. m3026. https://doi.org/10.1136/bmj.m3026.
- Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study // The Lancet. 2021. V. 397. №10270. P. 220-232. https://doi.org/10.1016/S0140-6736(20)32656-8.
- Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P. A., Cuapio A., Villapol S. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis // Scientific Reports. 2021. V. 11. №1. P. 16144. https://doi.org/10.1038/s41598-021-95565-8.
- Rajan S., Khunti K., Alwan N., Steves C., Greenhalgh T., MacDermott N., McKee M. In the wake of the pandemic: Preparing for Long COVID // World Health Organization Europe, Policy Brief. 2021. 39. https://apps.who.int/iris/handle/10665/339629.
- Sivan M., Taylor S. NICE guideline on long COVID // BMJ. 2020. V. 371. P. m4938. https://doi.org/10.1136/bmj.m4938.
- Tenforde M. W., Kim S. S., Lindsell C. J., Billig Rose E., Shapiro N. I., Files D. C., Feldstein L. R. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network // Morbidity and Mortality Weekly Report (MMWR). 2020. V. 69. №30. P. 993-998. https://doi.org/10.15585/mmwr.mm6930e1.
- Townsend L., Dowds J., O’Brien K., Sheill G., Dyer A. H., O’Kelly B., Conlon N. Persistent poor health post-COVID-19 is not associated with inflammatory markers or autoantibodies // Frontiers in Immunology. 2021. V. 12. P. 705538. https://doi.org/10.3389/fimmu.2021.705538.