Morphological features of changes in the cardiovascular system in COVID-19
Автор: Zumrad Abdukayumovna Ergasheva, Rajabboy Isroilovich Isroilov, Alisher Kayumovich Shadmanov, Zukhriddin Salokhiddinovich Salokhiddinov, Mamazair Akhmedovich Khuzhamberdiev, Sardor Shakirov, Abdukhalim Khaliddin
Журнал: Re-health journal @re-health
Рубрика: Ковидология
Статья в выпуске: 4 (12), 2021 года.
Бесплатный доступ
Since its recognition in December 2019, COVID-19 has rapidly spread globally causing a pandemic. Pre-existing comorbidities such as hypertension, diabetes, and cardiovascular disease are associated with a greater severity and higher fatality rate of COVID-19. Furthermore, COVID-19 contributes to cardiovascular complications, including acute myocardial injury as a result of acute coronary syndrome, myocarditis, stress-cardiomyopathy, arrhythmias, cardiogenic shock, and cardiac arrest. The cardiovascular interactions of COVID-19 have similarities to that of severe acute respiratory syndrome, Middle East respiratory syndrome and influenza. Specific cardiovascular considerations are also necessary in supportive treatment with anticoagulation, the continued use of renin-angiotensin-aldosterone system inhibitors, arrhythmia monitoring, immunosuppression or modulation, and mechanical circulatory support. Thus, in this article we will discuss morphological features of changes in the cardiovascular system in COVID-19.
COVID-19, pandemic, hypertension, diabetes, cardiovascular disease, acute myocardial injury, acute coronary syndrome, myocarditis, stress-cardiomyopathy, arrhythmias, cardiogenic shock, cardiac arrest, acute respiratory syndrome, Middle East respiratory syndrome, influenza, anticoagulation, renin-angiotensin-aldosterone system inhibitors, arrhythmia monitoring, immunosuppression, modulation, mechanical circulatory, morphological features
Короткий адрес: https://sciup.org/14124621
IDR: 14124621
Текст научной статьи Morphological features of changes in the cardiovascular system in COVID-19
Introduction: The coronavirus disease of 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first appeared in Wuhan, China [1,2, 3]. It was officially declared a pandemic by the World Health Organization in March 2020 [1,3]. While much of the focus has been on the pulmonary complications, it is important for emergency clinicians to be aware of the cardiovascular complications, which can be a significant contributor to the mortality associated with this disease [4, 5, 6, 7, 8, 9]. This brief report will provide a focused overview of cardiovascular complications associated with COVID-19, including myocardial injury and myocarditis, acute myocardial infarction (AMI), heart failure, dysrhythmias, and venous thromboembolic events (VTE).
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes covid-19, was first reported to WHO as a pneumonia of unknown cause in Wuhan, China, on 31 December 2019 [10]. While the initial outbreak was mostly confined to the epicentre in China, SARS-CoV-2 quickly spreads internationally causing a global pandemic. By 15 March, the number of cases outside of China surpassed those in China, and as of 12 April 2020, over 1.8 million cases and 110 000 deaths were reported worldwide, affecting 185 countries [11]. The most common symptoms of COVID-19 include fever, dry cough, myalgia or fatigue, as is the case in many other viral infections [12,13]. According to a study by the Chinese Center for Disease Control and Prevention of 44 672 laboratory confirmed, 10 567 clinically diagnosed and 16 186 suspected cases of COVID-19, 81.4% exhibited mild illness (with no or mild symptoms of pneumonia), 13.9% had severe symptoms (dyspnoea with respiratory rate ≥30/min, SpO2 ≤93%, PaO2/FiO2<300 and/or infiltration of lung field >50% within 24– 48 hours), and 4.7% were critically ill (respiratory failure, septic shock and/or multiorgan failure) [14]. In patients with severe or critical disease, viral pneumonia can progress to acute respiratory distress syndrome (ARDS), and multisystem failure accompanied by a cytokine storm. Since patients with covid-19 with cardiovascular comorbidities have higher mortality, and the severity of COVID-19 disease correlates with cardiovascular manifestations [15], it is important to understand the interaction of COVID-19 and cardiovascular disease (CVD). This review will summarise our current understanding of the cardiovascular manifestations of covid-19, as compared with SARS (caused by SARS-CoV), the Middle East respiratory syndrome (MERS) (caused by MERS-CoV) and influenza.
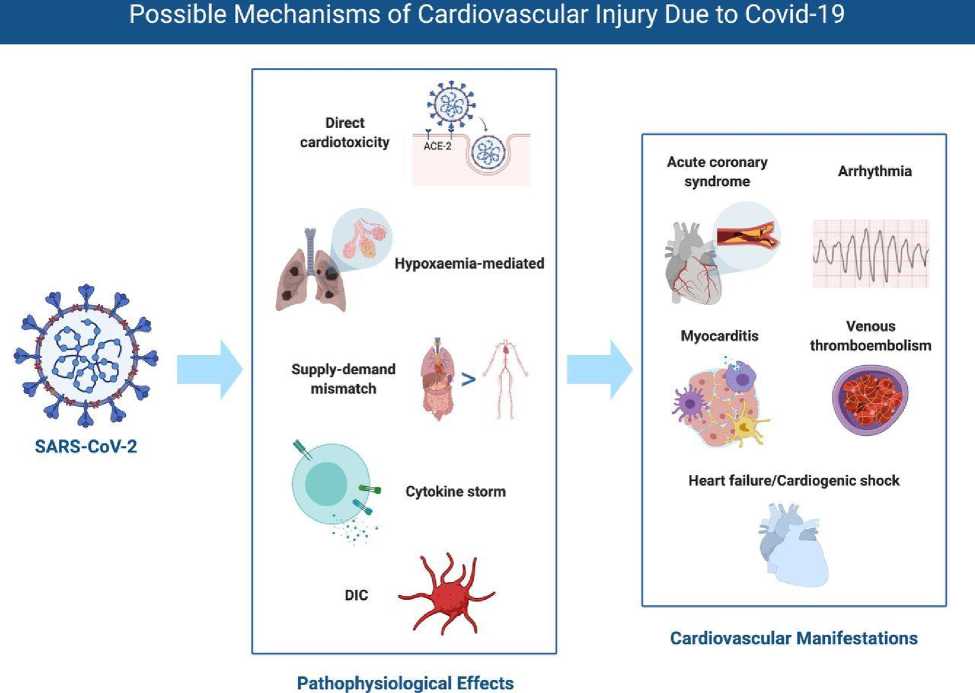
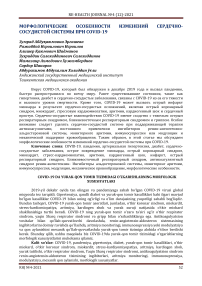
Figure 1
Possible mechanisms of cardiovascular injury due to COVID-19. DIC, disseminated intravascular coagulation; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Cardiovascular manifestations. The clinical cardiovascular manifestations of COVID-19 include elevation of cardiac biomarkers (ischaemic or non-ischaemic aetiology), cardiac arrhythmia, arterial and venous thromboembolism (VTE), and cardiogenic shock and arrest. The possible mechanisms and cardiovascular manifestations are shown in figure 1.
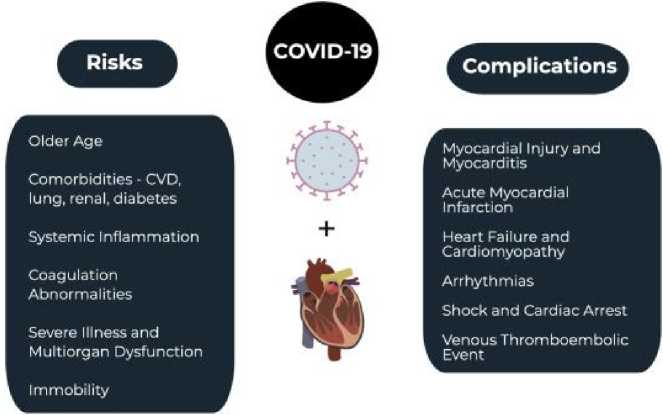
Figure 2. COVID-19
and the cardiovascular system.
As for as some group scientists go said [16] that SARS-CoV-2 is an enveloped, nonsegmented, single-stranded, positive-sense RNA virus [2, 5-9]. Angiotensin-converting enzyme 2 (ACE2) is a protein found on the surface of lung alveolar epithelial cells and enterocytes of the small intestine, which has been proposed as the entry site for SARS-CoV-2 [17]. ACE2 breaks down angiotensin II, a proinflammatory factor in the lung. Inhibition of ACE2 may be another factor in lung injury, as well as the cause of the systemic inflammation with cytokine release that can result in acute respiratory distress syndrome (ARDS) and multiorgan dysfunction [18-20]. Disruption in immune system regulation, increased metabolic demand, and procoagulant activity likely account for some of the increased risk of adverse outcomes in those with COVID-19-related cardiovascular disease (CVD) [8, 9, 21]. Specifically, systemic inflammation can destabilize vascular plaques, while the viral illness increases cytokine activity, increasing cardiac demand, similar to influenza [22, 23]. Recent research, however, has suggested that the virus may also cause direct damage to the heart utilizing ACE2 receptors located within cardiac tissue [24]. The prevalence of CVD in COVID-19 patients is unclear, but preexisting CVD may be associated with a more severe COVID-19 infection [4-6, 26]. A meta-analysis of 1527 patients with COVID-19 found that the prevalence of hypertension was 17.1% and cardiac disease was 16.4%, and that these patients were more likely to require critical care [25]. Another study of 44,672 patients with COVID-19 found that a history of CVD was associated with a nearly five-fold increase in the case fatality rate when compared with patients without CVD (10.5% vs. 2.3%) [5]. Other studies suggest similar findings with increased risk of mortality in patients with prior CVD [5-9, 19]. Severe or critical cases account for less than 20% of patients with COVID-19 [5-9, 26-30]. Patients with critical illness may present with pneumonia, ARDS, multiorgan dysfunction, and hemodynamic instability, as well as several cardiovascular complications [5-9, 26-30]. Cardiogenic shock is the most severe cardiac complication and may occur in those with critical illness [5-9, 26].
Prior viral illnesses, including Middle East respiratory syndrome coronavirus (MERS-CoV), have been associated with myocardial injury and myocarditis with troponin elevation, thought to be due to increased cardiac physiologic stress, hypoxia, or direct myocardial injury [4, 31- 40]. One of the first reports of myocardial injury associated with SARSCoV-2 was a study of 41 patients diagnosed with COVID-19 in Wuhan, China, wherein 5 patients (12%) had a high-sensitivity troponin I above the threshold of 28 pg/mL [7]. Subsequent studies have found that myocardial injury with an elevated troponin level may occur in 7-17% of patients hospitalized with COVID-19 and 22-31% of those admitted to the intensive care unit (ICU) [79]. Myocarditis has also been identified with high viral loads and mononuclear infiltrates identified on autopsy of some patients with COVID-19 [33-35]. In fact, one study suggested that up to 7% of COVID-19 related deaths were due to myocarditis [6]. Acute myocarditis presents across a variable range of clinical severity and is a significant diagnostic challenge in the COVID-19 era. Patients with COVID-19 can present with chest pain, dyspnea, dysrhythmia, and acute left ventricular dysfunction [5-9]. In patients with myocarditis and myocardial injury, serum troponin values will be abnormal. The electrocardiogram (ECG) can demonstrate a range of findings, in some cases mimicking acute coronary syndrome (ACS). The ECG abnormalities result from myocardial inflammation and include non-specific ST segment-T wave abnormalities, T wave inversion, and PR segment and ST segment deviations (depression and elevation). Echocardiography and consultation with cardiology, if either are available, is encouraged, as differentiating myocarditis and ACS is difficult. Echocardiographic evaluation is more likely to demonstrate a focal wall motion abnormality with active, significant ACS while severe forms of COVID-19-related myocarditis will show either no wall motion defects or global wall motion dysfunction [4, 39]. ECG and echocardiographic abnormalities in the setting of COVID-19 are markers of illness severity and are correlated with worse outcomes [4, 36, 37]. Moreover, troponin elevations in patients with COVID-19
infection have been directly associated with an increased risk of adverse outcome in those patients with severe infection, including mortality [32, 36, 37].
Severe systemic inflammation increases the risk of atherosclerotic plaque disruption and AMI [22, 37-40]. A 2018 study found that influenza and other select viral illnesses were associated with an increased risk of AMI within the first 7 days of disease diagnosis, with an incidence ratio of 6.1 for influenza and 2.8 for other viruses [22]. Another study of patients hospitalized for community-acquired pneumonia found an increased risk of active CVD that remained present for several years after hospitalization [38]. Due to extensive inflammation and hypercoagulability, the risk of AMI is likely present in patients with COVID-19 [4, 39]. The treatment of AMI is controversial in COVID-19 patients. In patients diagnosed with an ST elevation myocardial infarction (STEMI) and COVID-19, the American College of Cardiology (ACC) states that while fibrinolysis may be considered in those with "low risk STEMI", defined by inferior STEMI with no right ventricular involvement or lateral AMI without hemodynamic compromise, percutaneous coronary intervention (PCI) is more commonly performed at most institutions and remains the treatment of choice [39]. If PCI is pursued, staff should don appropriate personal protective equipment (PPE), and a full decontamination of the catheterization laboratory should be performed following the procedure. For suspected COVID-19 in the setting of NSTEMI, diagnostic testing prior to catheterization is recommended; the ACC note that, in properly selected patients with confirmed COVID-19, conservative therapy may be sufficient. Patients who are hemodynamically unstable in the setting of NSTEMI should be managed similarly to those with STEMI [39].
Acute heart failure can be the primary presenting manifestation of COVID-19 infection. One study found that acute heart failure may be present in 23% of patients in their initial presentation for COVID-19, with cardiomyopathy occurring in 33% of patients [8]. Another study found that heart failure was present in 24% of patients and was associated with an increased risk of mortality [40]. Among those with heart failure, nearly half did not have a known history of hypertension or CVD [40]. It is currently unknown if heart failure is due to new cardiomyopathy versus an exacerbation of previously undiagnosed heart failure [41]. It is important to be conscious of this potential cardiac dysfunction when administering intravenous fluids and avoid overaggressive fluid replacement. Importantly, right heart failure may also occur, particularly among those with ARDS and acute lung injury [4, 26].
Palpitations may be a presenting symptom in over 7% of patients with COVID-19 [33]. A range of dysrhythmias have been encountered in patients with COVID-19 infection. Most frequently, sinus tachycardia is seen in such patients, resulting from multiple, simultaneous causes (hypoperfusion, fever, hypoxia, anxiety, etc) [4]. One study found that dysrhythmias were present in 17% of hospitalized and 44% of ICU patients with COVID-19 [9]. Dysrhythmias may occur in the setting of viral illness due to hypoxia, inflammatory stress, and abnormal metabolism [4]. If dysrhythmias are associated with an elevation in serum troponin, the clinician should consider myocardial injury, acute myocarditis, and ACS in the differential diagnosis [4].
Patients with COVID-19 are also at an increased risk of VTEs [42, 43]. Systemic inflammation, abnormal coagulation status, multiorgan dysfunction, and critical illness are all potential contributing factors to the increased risk of VTE [7, 8, 42-45]. Studies suggest significant coagulation pathway abnormalities in patients with COVID-19, including elevated D-dimer [7, 8, 42-45]. One study of 25 patients with COVID-19 pneumonia found that an elevated D-dimer was present in all patients with a median of 6.06 micrograms/ml, with 10 patients having a pulmonary embolism (PE) diagnosed on computed tomography pulmonary angiography (CTPA) [44]. Patients with confirmed PE on CTPA demonstrated a median D-dimer level of 11.07 micrograms/ml [44]. D-dimer levels greater than 1 цд/mL were associated with an increased risk of death during hospitalization (odds ratio 18.4) in COVID-
19-infected patients [8]. One study suggests anticoagulation, mainly with low molecular weight heparin, may be associated with reduced mortality in severe COVID-19 infections or those with D-dimer greater than six times the upper limit of normal [46].
Many of the newly studied medications interact extensively with other cardiovascular drugs, including antihypertensives, antiarrhythmics, anticoagulants, antiplatelets, and statins [4]. Current medications under study include antivirals (e.g., remdesivir, ribavirin, lopinavir/ritonavir, favipiravir), antimalarials (e.g., chloroquine, hydroxychloroquine), azithromycin, corticosteroids, and biologics (tocilizumab) [4, 47-49]. Lopinavir/ritonavir may cause QT and PR prolongation, particularly in those with baseline QT prolongation or in those taking medications that may cause QT prolongation [50]. These medications can also affect anticoagulant medications, antiplatelet agents, and statins [50]. Chloroquine and hydroxychloroquine affect the intracellular pH, which can result in electrolyte abnormalities, cardiotoxicity, and prolonged QT intervals; they may also interact with antiarrhythmic agents [51, 52]. Methylprednisolone can cause electrolyte derangements, fluid retention, and hypertension [35].
Long, B., Brady, W. J., Koyfman, A., Gottlieb, M gave own conclusions in own article [23]: COVID-19 is associated with a number of cardiovascular complications, including myocardial injury and myocarditis, AMI, heart failure, dysrhythmias, and VTE. Some of the medications utilized to treat COVID-19 also have potential cardiac complications. It is important for the emergency clinicians to be aware of these complications when treating the COVID-19 patient.
Khawaja, S. A., Mohan, P., Jabbour, R., Bampouri, T., Bowsher, G., Hassan, A. M. M., … Mikhail, G. W gave own conclusions in own article [53]: Our study demonstrates that preexisting CVD and age predict worse outcomes in patients hospitalised with COVID-19. Furthermore, biochemical myocardial injury is associated with increased mortality. Fewer patients than expected required cardiac intervention. Further studies are needed to investigate the long-term cardiovascular outcomes of patients who have survived COVID-19.
Conclusion: COVID-19, a symptom complex of respiratory failure induced by a highly infectious pathogen, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has been classified as a pandemic. The current pandemic is evolving very rapidly and has had a profound global health impact. To mitigate the impact of COVID-19 syndrome, the scientific community has been working around the clock and new literature is being published daily. The current review is relevant and summarizes the disease as we understand it at this point in time. There are currently various ongoing clinical trials to evaluate feasibility and clinical applications of laboratory testing for rapid diagnosis, drug therapy to reduce severity of the syndrome, and development of vaccines. Every day there are new case series and retrospective reviews of patient cohorts that are published to shed light on the management and therapy of the novel virus.
In conclusion, in this article we have reviewed morphological features of changes in the cardiovascular system in COVID-19. We also discussed the treatment options for this disease. We have analyzed the opinions and conclusions of several scientists on this topic. We believe that this article can be an impetus for further in-depth research.
Список литературы Morphological features of changes in the cardiovascular system in COVID-19
- World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Available online at https://www.who.int/dg/speeches/detail/whodirector-general-s-opening-remarks-at-themedia- briefing-on-covid-19---1 march-2020, Accessed 4th Apr 2020
- Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html , Accessed 11th Apr 2020
- World Health Organization Situation report https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200403-sitrep-74-covid-19-mp.pdf?sfvrsn=4e043d03_4, Accessed 4th Apr 2020
- E. Driggin, M.V. Madhavan, B. Bikdeli, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19 pandemic
- J Am Coll Cardiol (Mar 18 2020)[pii: S0735-1097(20)34637-4, in press] Z. Wu, J.M. McGoogan Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention JAMA (Feb 24 2020), 10.1001/jama.2020.2648
- Q. Ruan, K. Yang, W. Wang, L. Jiang, J. Song Clinical predictors of mortality due to COVID- 19 based on an analysis of data of 150 patients from Wuhan, China [published online ahead of print, 2020 Mar 3] Intensive Care Med (2020), pp. 1-3, 10.1007/s00134-020-05991-x
- C. Huang, Y. Wang, X. Li, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China Lancet, 395 (2020), pp. 497-506
- F. Zhou, T. Yu, R. Du, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study Lancet, 395 (10229) (Mar 28 2020), pp. 1054-1062
- D. Wang, B. Hu, C. Hu, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China JAMA (Feb 7 2020), 10.1001/jama.2020.1585
- Novel coronavirus (2019-nCoV) situation Report-1, 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situationreports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4
- Coronavirus COVID-19 global cases by the center for systems science AD engineering (CSSE) at Johns Hopkins University. Available: https://coronavirus.jhu.edu/map.html [Accessed 12 Apr].
- Huang C , Wang Y , Li X , et al Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. doi:10.1016/S0140-6736(20)30183-5 pmid:http://www.ncbi.nlm.nih.gov/pubmed/31986264
- Wang D , Hu B , Hu C , et al Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–9.doi:10.1001/jama.2020.1585 pmid:http://www.ncbi.nlm.nih.gov/pubmed/32031570
- The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly 2020;2:113–22.
- Guo T , Fan Y , Chen M , et al Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020.doi:10.1001/jamacardio.2020.1017
- Long, B., Brady, W. J., Koyfman, A., & Gottlieb, M. (2020). Cardiovascular complications in COVID-19. The American Journal of Emergency Medicine. doi:10.1016/j.ajem.2020.04.048
- Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol Jun 2004;203(2):631–7.
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature Mar 2020;579(7798):270–3.
- Ge XY, Li JL, Yang XL, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature 2013;503:535–8.
- Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med Apr 2020;46(4):586–90.
- Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation 2001; 103:1718–20.
- Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratoryconfirmed influenza infection. N Engl J Med 2018;378:345–53.
- Davis MM, Taubert K, Benin AL, et al. Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/ American College of Cardiology. J Am Coll Cardiol 2006;48:1498–502.
- Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res Mar 30 2020. https://doi.org/10.1093/cvr/cvaa078 [pii: cvaa078, Epub ahead of print].
- Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol Mar 11 2020. https://doi.org/10.1007/ s00392-020-01626-9 [Epub ahead of print].
- Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA Mar 11 2020. https://doi.org/10.1001/jama.2020.3633 [Epub ahead of print].
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13.
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARSCoV- 2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med Feb 24 2020. https://doi.org/10.1016/S2213-2600 (20)30079-5 [pii: S2213-2600(20)30079-5, Epub ahead of print].
- Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. Lancet 2020;395(10229):1014–5. https://doi.org/10.1016/S0140-6736(20)30633-4.
- Intensive Care National Audit & Research Centre. ICNARC report on COVID-19 in critical care. March 27, 2020. Accessed March 30, 2020.
- Alhogbani T. Acute myocarditis associated with novel middle east respiratory syndrome coronavirus. Ann Saudi Med 2016;36:78–80.
- Chen C, Zhou Y, Wang DW. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz Mar 2020. https://doi.org/10.1007/s00059-020-04909-z [Epub ahead of print].
- Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) Feb 7 2020. https://doi.org/10.1097/CM9.0000000000000744 [Epub ahead of print].
- Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med Apr 2020;8(4):420–2.
- Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci 2020;63: 364–74.
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. doi:https://doi.org/10.1001/jamacardio.2020.0950.
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. doi:https://doi.org/10.1001/jamacardio.2020.1017.
- Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA 2015; 313:264–74.
- Welt FGP, Shah PB, Aronow HD, from the American College of Cardiology’s (ACC) Interventional Council and the Society of Cardiovascular Angiography and Intervention (SCAI), et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC’s Interventional Council and SCAI. JACC 2020. https://doi.org/10.1016/j.jacc.2020.03.021.
- Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ Mar 26 2020;368:m1091.
- Buzon J, Roignot O, Lemoine S, et al. Takotsubo cardiomyopathy triggered by influenza A virus. Intern Med 2015;54:2017–9.
- Xie Y, Wang X, Yang P, Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiology: Cardiothoracic Imaging 2020;2(2):e200067.
- Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J Mar 30 2020. https://doi.org/10.1093/eurheartj/ehaa254 [pii: ehaa254, Epub ahead of print].
- Chen J, Wang X, Zhang S, et al. Findings of acute pulmonary embolism in COVID-19 patients. Lancet Infectious Disease. [Available at SSRN: https://ssrn.com/abstract= 3548771 or http://dx.doi.org/10.2139/ssrn.3548771].
- Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost Apr 2020;18(4):844–7.
- Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost Mar 27 2020. https://doi.org/10.1111/jth.14817 [Epub ahead of print].
- Chavez S, Long B, Koyfman A, Liang S. Coronavirus disease (COVID-19): a primer for emergency physicians. American Journal of Emergency Medicine March 24, 2020. https://doi.org/10.1016/j.ajem.2020.03.036 Published online.
- Elfiky AA. Anti-HCV, nucleotide inhibitors, repurposing against COVID-19. Life Sci 2020;248:117477.
- Chu CM, Cheng VC, Hung IF, et al. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax 2004;59:252–6.
- KALETRA(R) oral film coated tablets, oral solution, lopinavir ritonavir oral film coated tablets, oral solution. Product insert. North Chicago, IL: AbbVie Inc. (per FDA); 2013.
- Page II RL, O’Bryant CL, Cheng D, et al. Drugs that may cause or exacerbate heart failure: a scientific statement from the American Heart Association. Circulation 2016; 134:e32–69.
- Tonnesmann E, Kandolf R, Lewalter T. Chloroquine cardiomyopathy - a review of the literature. Immunopharmacol Immunotoxicol 2013;35:434–42.
- Khawaja, S. A., Mohan, P., Jabbour, R., Bampouri, T., Bowsher, G., Hassan, A. M. M., … Mikhail, G. W. (2021). COVID-19 and its impact on the cardiovascular system. Open Heart, 8(1), e001472. doi:10.1136/openhrt-2020-001472