N. Moiseev and the return to the principles of epidemic hygiene in pandemics
Автор: Kofler W.W.
Журнал: Вестник Международной академии наук (Русская секция) @vestnik-rsias
Рубрика: Экологическая антропология: здоровье, среда и качество жизни
Статья в выпуске: S1, 2022 года.
Бесплатный доступ
Academician N.Moiseev recognized that the survival of mankind can only be ensured if the biological principles of the habitats necessary for this are sustainably taken into account. Therefore, he promoted the education of as many people as possible, so that each individual is enabled to direct his behavior in such a way that the ecological requirements are not left out for lack of appropriate knowledge. This leads to two conclusions, e. g. for epidemics: To take into account the roots of the emergence of new pathogens and to disseminate the principles of biological relationships as generally as possible. Therefore, the principles of epidemic hygiene and their psycho-socio-cultural interdependencies were presented. It becomes clear that a distinction must be made between the fight against the epidemic - and thus against the pathogen - and the fight against the consequences of the penetration of the pathogen into the organism, i. e. against the infectious disease and its indirect consequences. The transition of these two process areas ALWAYS takes place in individual persons, thus is always decided by the individual process. In a pandemic, a large number of people around the world go through this process individually at the same time. A pandemic is not a tsunami that hits everyone just because he is there. The individual characteristics, which can be strengthened and weakened in a variety of ways, even in the short term, are decisive for whether contact with a carrier leads to contamination of the mucous cells of the respiratory tract or not, whether the pathogens are destroyed thanks to the resistance of the non-specific defenses or can still penetrate the body (infection in the real sense), and whether others can already be infected in this phase. Even a fight against contact between infected and infectious persons, no matter how differentiated, therefore only leads to a temporary reduction in new cases, but neither lowers susceptibility nor contributes to the destruction of the pathogens. Antibodies can only act where they are, i. e., only when the pathogens have entered the organism, but not in the extracorporeal space of the respiratory tract. Therefore, intramuscularly vaccinated persons and persons recovered from COVID-19 can be re-infected, pass the germs on to third parties and thus contribute to the spread of the epidemic. If one wants to limit the spread of the pathogens, one must strive to lower the susceptibility, e.g. by strengthening and supporting the natural extracorporeal defense and to kill the pathogens and thus to lower their chance to penetrate the organism. This is also the method of choice in the fight against new mutants. The possibilities of fighting against the spread of pathogens have been largely neglected so far. It is pretended that the fight against the consequences of the epidemic is identical to the fight against the epidemic.
Pandemic, environmental education, pathogens, individual and epidemic hygiene
Короткий адрес: https://sciup.org/143179422
IDR: 143179422
Текст научной статьи N. Moiseev and the return to the principles of epidemic hygiene in pandemics
Introduction to Key Concepts of Epidemic Hygiene
For this purpose, it is necessary to know key concepts of epidemic hygiene and to grasp their dynamics. They have stood the test of time for more than 100 years, but seem to have been virtually forgotten in the present. They include virulence and pathogenicity (of the pathogen), susceptibility, tolerance, nonspecific and specific defense, in particular antibodies and their formation (of the host), and the microbiome including the virobiome, i.e. the colonization of the respiratory tract by other germs. Virulence determines how easy it is for the pathogen to adhere to and penetrate the cell of the mucous membrane, e.g. of the respiratory tract (contamination), and how successfully the pathogens thus multiplied can overcome the external cell barrier and penetrate the organism (infection in the real sense). The mucosa cells resist this process, for example, by releasing an oxidizing agent (N-chlorotaurine) into the volume of the respiratory tract. Given sufficient exposure time, this can destroy the structures of very many bacteria, viruses (such as SARS-CoV-2), fungi, and protozoa without damaging the mucosa cells[9] (The well-tolerated NCT can also be produced artificially [10]). How the microbiome, along with the virobiome, intervenes in the mucosa cells' fight against the onrushing pathogens is still largely unknown. This process is mostly (e.g., in the case of SARS-CoV-2) independent of specific immunity, since only the so-called secretory IgA is released into the respiratory tract. Intramuscular vaccination and disease, however, result (in the case of COVID-19) in virtually no sIgA formation whereas intranasally administered vaccination would. A surprising and strategically significant result for many, but one that is supported by the current literature in leading journals [e. g. 18, 19]. The process that occurs following contact of an infectious person with a germ carrier is characterized in disease hygiene by the terms — contagion index and manifestation index. The contagion index indicates the proportion of unvaccinated persons who come into contact with the pathogen for the first time, where the pathogen can adhere/contaminate. The manifestation index indicates how many become demonstrably ill after passing through the incubation period. The manifestation index is therefore always smaller than the contagion index: The people whose non-specific defenses were able to destroy the pathogens despite contamination («inactivation period») are omitted.
Without non-specific defenses, mankind would therefore have died out long ago.
The comparison with the different contact indices between marginalized groups and the standard population shows how significant syndemic, non-therapeutic influences on defense are. This is why, for example, tuberculosis and COVID-
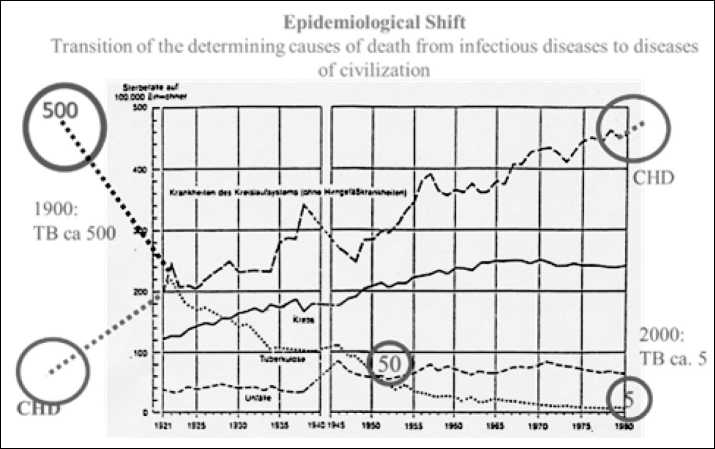
Fig. 3. Epidemiological shift in Austria: deaths from tuberculosis, cancer, CHD and accidents, Data: 1921–90 (Central Statistical Office, Vienna), supplemented by data from Mosse-Tugendreich (1913 [11]) for 1900 and our (now confirmed) forecast for 2000. (Kofler W., Lercher P. et al., 1995 [12]).
19 are also considered syndemics, epidemics that can only be adequately understood and permanently controlled if social, economic, cultural and educational influences are taken into account [4]. Graph 3 illustrates this using the example of the transition from the dominance of infectious diseases to (behavioral) civilization diseases as the determining causes of death in Austria between 1900 and 2000 (epidemiological shift).
For tuberculosis the rule of thumb is: 500 — 50 — 5. In 1900 about 500 of 100,000 Austrians died per year, in 1950 only 50 and in 2000 5 (mortality). The decrease from 500 to 50 was — contrary to the widespread opinion even in medical circles — neither due to vaccination nor due to antibiotics. For political reasons, the (French) vaccine was not used in Germany (and thus in Austria until 1945). Streptomycin was too expensive to have an impact on mortality (Mortality related to a mathematically precisely defined collective). The decrease is due to improved living, nutritional, and working conditions, social security, and education. None of these influencing variables changes specific immunity. Therefore, mortality increases among marginalized groups, migrants, and the immunocompromised (HIV). Lethality (fatality) refers to the risk to the diseased, not to the population (mortality).
It is therefore essential to distinguish between contact with an infectious agent, contamination, of the incubation period, infection in the actual sense (=penetration of the pathogen into the organism) and infectious disease. Unfortunately, the same term is currently often used for these five different stages. As a result, decisive possibilities in the fight against the pathogen remain unnoticed.
The number of newly infected persons in relation to a mathematically defined representative collective (inci- dence) therefore depends not only on the different influences on the relevance of contacts (distance, duration, intensity of speaking, mask, etc.) and thus on lock downs, school closures, testing, segregation, etc., and also not only from the effects of a protection against the infection DISEASE (vaccination, recovery). A multitude of additional promoting and inhibiting influences are also decisive. Without taking ALL influencing variables into account, a scientifically correct prognosis of the jointly caused result, but also the prognosis of the effectiveness of a special measure is not possible.
In the case of diseases in which contaminated persons can infect others even though they themselves do not (yet) have any symptoms, as is the case for COVID-19 patients, it must therefore be expected that recovered persons can also become contaminated and infect others. As early as 2020, it was demonstrated in WUHAN that about 50% of infections of third parties occur in the phase before the onset of symptom [13]. Contrary to the view held at the time, symptom-free germ carriers are potential vectors from the first day of infection, not just two days before the onset of their own symptoms [14, 15]. This is decisive for the meaningfulness of systematic testing and segregation of even the still symptom-free germ carriers [16]. If one were to systematically combine repeated testing of symptom-free individuals with antiseptic measures, a significant increase in effectiveness in the fight against the pathogen could be expected.
It is important to distinguish between individual hygiene and epidemic hygiene. The aim of individual hygiene is to avoid the individual risk of falling ill. Epidemic hygiene is aimed at reducing the risk to the community. However, a measure that makes sense in terms of individual hygiene can be counterproductive in terms of epidemic hygiene. For example, vaccination against cholera makes sense in terms of individual hygiene, but is highly problematic in terms of epidemic hygiene. This is because infection with cholera vibrions has different subjective courses, ranging from practically symptom-free to mild diarrhea to the characteristic rice-water-like diarrhea and death. However, the excretions of all ill persons are highly infectious. Inconspicuous ill persons remain undetected, while conspicuous ones are quarantined. Their excretions are disinfected, thus destroying the pathogens and stopping their spread. The cholera vaccination has no significant influence on the susceptibility = infectability, only on the course of the disease. Therefore, vaccinated individuals can become infected and pass on the germs. Cholera vaccination radically reduces the lethality (frequency of fatal outcome in patients) and the severe forms of the disease. Inconspicuous forms of progression increase sharply. Therefore, the regulation at the time that vaccinated persons were allowed to visit areas cordoned off because of cholera led to the spread of cholera.
The formation of the specific defense, i.e. one that is directed at the immunological characteristics of the specific pathogen, begins AFTER the pathogen enters the organism through special cells. The specific defense therefore takes place — apart from sIgA and IgM — ONLY in the body. Therefore, the level of the specific immunity does not affect whether the person can be contaminated and infected again, but it does affect the course of the disease.
It takes several days before the first antibodies can be detected. Until then, the intracorporeal nonspecific defense determines the course of the process and thus also the importance of the infected person for the spread of the disease. Therefore, it would also be important for the spread of the disease to support this defense. In this regard, the preventive and rehabilitative use of hypoxic -hyperoxic inhalations techniques gives hope. In this way, the person acquires the ability to absorb and use oxygen more efficiently and, as a result, to increase overall adaptive potential, antioxidant defense, nonspecific immunity, metabolic efficiency [17].
The (specific) antibodies play a crucial role in the destruction of the pathogens in the organism.
Whether her/his vaccination not only reduces the risk of severe disease progression, but also to a relevant extent the risk of transmission to third parties and the risk of renewed contamination of the vaccinated person depends on the type of vaccination. The decisive factor is whether or not the vaccination also leads to the formation of secretory IgA against the pathogen. In the case of intranasally administered vaccines, this has been used against influenza for many years. Intranasal vaccines against SARS-CoV-2 also form sIgA, but the intramuscularly administered vaccines currently in use do not [18]. To date, no intranasal vaccine against SARS-CoV-2 is on the market. The disease also does not lead to relevant sIgA formation [19.]
Whether a person becomes ill with the same pathogen at the same time as many others (epidemic), whether this occurs simultaneously worldwide (pandemic), whether he or she is one of the few who fall ill all the time because of this pathogen (endemic) or a sporadic isolated case is irrelevant to her/his biological processes. The distinction between pandemic, epidemic, endemic and sporadic occurrence is therefore essential for the necessary organizational measures, but not, for example, for therapy. With each infection, one must reckon with the different courses that have occurred in the past. This also concerns the question of whether and for how long how many of the diseased can continue to excrete germs. One and the same pathogen can trigger quite different courses. For example, some people can destroy all pathogens in the course of the healing process. Then they cannot infect anyone else after recovery. Others develop a tolerance to the pathogen. Then the persons with a good immune system can permanently spread germs without any symptoms, as in the case of so-called «infectious hospitalism». In this case, the healthy hospital staff transmit the germs to the immunocompromised patients, who can become seriously ill. Or the pathogens may also remain in a symptom-free person for a very long time without being able to be spread. Who does not know this from the fever blister as a result of an infection years in the past, which suddenly reappears after a disgusting event, a heavy other load or a recalcitrant beard hair irritating the lip? It is impossible to trace the starting point of the infection chain by retracing contacts.
So if there are people who never show symptoms but can pass on pathogens, they can also transmit the germs to people who do not fall ill themselves but pass on the germs, and so on, until finally a person is infected who becomes classically ill or who does show symptoms after an additional stress, such as stress in the family. Thus a «viral dark net» can develop, whose carrier 0/patient 0 (= the initial person of the infection chain) can no longer be determined. No wonder, then, when an epidemic turns into an endemic.
Limits of Calculability
Average values are worthless when it comes to individual cases such as the triggering of an epidemic by the carrier 0. In individual cases, infectivity can begin on the day of one's own contamination and can also be present months later, regardless of whether person 0 himself is symptomatically conspicuous or not and whether new mutants have formed in him or not.
But measures that only delay contact between germ carriers and infectibles do not kill germs or create specific immunity or unspecific defense. They do, however, flatten the curve of new cases so that hospitals are not overburdened. Therefore, they should actually be counted among the measures against the consequences of the disease and not among those against the spread of the pathogens.
Forecasts are necessary for decision-making processes. However, the considerable differences that have emerged in simulation models using the same baseline data have led to the call for the establishment of a new federal facility in the U.S., which should be associated with a fundamental rethinking of strategy [21].
Precautionary Principle and the Creation of Evidence
Which course forms a pathogen appearing for the first time — like SARS-CoV-2 — in the course of an epidemic and thus the biological «learning processes» of the cells and the organism as well as the pathogen, cannot be known at the beginning of the epidemic. Nevertheless, for legal and ethical reasons, physicians and responsible politicians are entitled and obliged to avert damage to health. In accordance with the precautionary principle, he or she must be able to justify his inaction just as conclusively as his action [22.] However, at the beginning of an epidemic of a newly emerging pathogen, no one can know what forms of progression, etc., will occur currently and in the course of the epidemic. So-called «evidence» must first be created, i.e. a proven procedure that does not even have to be able to be causally justified. Ignaz Semmelweis, who introduced disinfection in 1847 and thus also antiseptics against childbed fever, and Dr. Snow, who stopped the cholera epidemic in London in 1852 by shutting down the Broad Street pump, could not yet have known about the existence of pathogens. Pasteur and Koch did not prove it until the 1870s.
But we are in a more favorable situation today. We accept the unique, not predetermined evolutionary process. This has practically limited the theoretical possibilities that were given in a prior state. We also accept that all pathogens must have appeared for the first time at some point. The possibility that one and the same pathogen can lead to different courses, which can have different consequences with regard to the spread of the pathogen, indicates what one has to take into account as a precaution until there is evidence that certain courses do not have to be taken into account. This can be used to proceed in a scientifically justified manner even in the case of an emerging pathogen. Details will appear in the Herald in the near future [7].
Mutants
Not only can the characteristics of the individual change in a beneficial or adverse way from an epidemic hygiene perspective, but so can the pathogen. It is nice when it loses its virulence and pathogenicity and therefore there is an end to an epidemic. But unfortunately, it is much more common that mutations and recombinations of the genetic material lead to adverse consequences and thus to more dangerous mutants. In the case of viruses, it should be noted that they cannot reproduce themselves. To do so, they must invade cells and force them to produce them. Therefore, the formation of mutants is possible only in the phase when viruses are in cells. The best protection against the formation of mutants is therefore to prevent viruses from entering cells. Therefore, the longer a person has been a germ carrier, the more likely mutant formation is. A study is available of a person who shed SARS-CoV-2 virus for 8 months ]23]. During this time, the emergence of 11 epidemic-hygienical-ly relevant mutants was detected. The number of germ carriers is also significant. Therefore, the fight against a pandemic is not successful until it is over worldwide, i.e. also in the Low and Medium Income Countries (LMIC).
Primary, Secondary, Tertiary Prevention, Health Promotion and the Fight Against the Emergence of New Pathogens
The sword of Damocles of the consequences of infections is not eliminated until the pathogen that can trigger an epidemic is eradicated. It would be even more forward-looking to inhibit that such germs emerge. The IPBES has proposed extensive measures against new formation. Preventive action can be taken against the spread of a pathogen. Measures that are intended to prevent people from becoming contaminated or, in the case of contamination, to prevent penetration and thus infection in the true sense, fall into the so-called «primary preven-tion» category. Measures aimed at early detection of the disease and measures against the occurrence of serious consequences fall under secondary prevention
This therefore includes, for example, testing and intramuscular immunization. Rehabilitation after successful therapy is tertiary prevention. Secondary and tertiary prevention are thus directed against the consequences of the disease and less against the spread of the pathogens. Health promotion aims to improve the performance of the organism as a whole and the well-being of the individual. This includes all measures against the syn-demic aspects of an infectious disease. It promotes the non-specific extracorporeal and intracorporeal defenses.
Conclusions
A distinction must be made between cause and effect: The cause of a pandemic is the worldwide spread of a pathogen, the effect is the worldwide occurrence of the consequences of the disease triggered by it and its secondary and tertiary consequences.
The epidemic hygiene goal of epidemic control is to prevent the emergence of new pathogens, prevent the formation of mutants, and ultimately to eradicate the pathogen.
Measures that do not lead to the destruction of the pathogens can lead to relief for hospitals (flattening of the curve), but only temporarily reduce the incidence of new cases. Therefore, if possible, they should be combined with measures that lead to the destruction of the pathogens. This is most easily achieved in the acute phase of an epidemic by strengthening extracorporeal nonspecific defenses, e.g., administration of natural NCT and other antiseptics, and intranasally administered vaccines.
Possibly because of the misleading multiplicity of meanings of the term «infection» as a synonym for (a) contamination with a pathogen, (b) infection (occurring after the incubation period) in the true sense (penetration of the pathogen into the organism), and (c) infectious disease, these possibilities have been neglected until now. (d) In simulation models, contact with an infected person is sometimes equated with the (probability of an) infectious disease. As a result, decisive influences of the «adjusting screw» are overlooked
Only vaccinations that lead to the formation of secretory IgA (respiratory, digestive tract) or to the formation of IgM (also in digestive tract) can be expected to have a significant impact on the spread of the pathogens.
Therefore, one should not assume that healthy persons and (intramuscularly) vaccinated persons acquire «sterile immunity», i.e., can never be infected again, do not become ill again, and can be neglected as carriers. A «herd immunity», by which non-vaccinated individuals are pro
Список литературы N. Moiseev and the return to the principles of epidemic hygiene in pandemics
- BrainardJ. 'COVID-ization' of research levels off. Science. 2022; 376 (6595): 782-783. DOI: 10.1126/science.add0532.
- Johns Hopkins University of Medicine, Coronavirus Research center https://coronavirus.jhu.edu/
- IPBES: Workshop Report on Biodiversity and Pandemics of the Intergovernmental Platform on Biodiversity and Ecosystem, IPBES secretariat, Bonn, Germany, 2020. DOI: 10.5281/zenodo.4147317sogenannten Syndemien.
- Horton R. Offline: Convid-19 is not a pandemic. Lancet, 2020, DOI: 10.1016/S0140-6736(20)32000-6.
- Kofler W., Glazachev O. et al. A Guide through the COVID-19 Jungle. Herald of the international Academy of Science (Russian Section), 2021; Special Edition: 6-77.
- Kofler W., Glazachev O. et al. COVID-19, John Snow, and the quest for psychosocial integrity: Part 1: What was actually the question? Herald ofthe international Academy ofScience (Russian Section), 2022; Special Edition 2 (in press).
- Kofler W., Glazachev O. et al. COVID-19, Ignaz Semmelweis, and the struggle for psychosocial integrity: an extended approach in the fight against the spread of novel pathogens. Herald of the international Academy of Science (Russian Section), 2022; Special Edition 2 (in press).
- Kofler W., Glazachev O. et al. COVID-19, J. Snow, Ignaz Semmelweis and the quest for psychosocial integrity: Part 3: addressing causes before they lead to effects. Herald of the international Academy of Science (Russian Section), 2022; Special Edition 2 (in press).
- Gottardi W., Nagl M. Thoughts and Questions Arising upon the Recognition of the broadly bioactive and very well tolerated Antiseptic N-Chlorotaureine as a highly useful medicant for prophylaxis and therapy, Herald of the international Academy ofScience (Russian Section), 2021; Special Edition: 78-81.
- Gottardi W., Nagl M. N-chlorotaurine, a natural antiseptic with outstanding tolerability. J. Antimicrob. Chemother. 2010; 65: 399-409.
- Mosse M., Tugendreich G. Krankheit und Soziale Lage. Facsimile reprint of the edition Munich, Lehmann, 1913. Ed. Jürgen Cromm, Göttingen, self-published by the editor, 1977.
- Kofler W, Lercher P, Hortnagl J. et al. Sozialmed Werkstattbericht 7.1.2. Basisunterlagen Spezieller Teil, 5/1995 Vernetztes Ausbildungsmodell, Sozialmedizin Uni Innsbruck, School ofPublic Health ASPHER, Eigenverlag, Innsbruck 1995.
- He X, Lau E.H.Y., Wu P. et al. Temporal dynamics in viral shedding and trans-missibility of COVID-19: Nature Medicine. DOI: 10.1038/s41591-020-0869-5, published online 15 April 2020.
- Ashcroft P. et al. COVID-19 infectivity profile correction, Swiss Med Wkly, 2020; 150: w20336.
- He X, Lau E.H.Y., Wu P. et al. Author Correction: temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020; 26: 1491-1493.
- Larremore D.B. et al. Test sensitivity is secondary to frequency and turnaround time for COVID19 screening. Sci Adv. 2021. DOI: 10.1126/sciadv.abd5393.
- Bayer U., Glazachev O.S., Likar, R. et al. Adaptation to intermittent hypoxia-hyperoxia improves cognitive performance and exercise tolerance in the elderly. Adv. Gerontol. 2017; 7: 214-220.
- Lund F.E, Randall T.D. Scent ofVaccine. Intranasal vaccination should block SARS-CoV-2 transmission at the source. Science, 2021. DOI: 10.1126/scienceabg9857.
- Oh J. E. et al. Intranasal priming induces local lung-resident B cell populations that secrete protective mucosal antiviral IgA. Sci. Imm., 2021. DOI: 10.1126/ sciimmunol.abj5129.
- Kermack W.O., McKendrick A.G. A Contribution to the Mathematical Theory of Epidemics. Proc.Royal Society A, Mathematical, Physical and Engineering sciences, 1927. DOI: 10.1098/rspa.1927.0118.
- Kofler W, Nagl M. The whole strategy has to be extended now — beyond modeling. eLetter to Press WH, RC Levin: Modeling, post COVID-19. Science 2021; 370: 1015, DOI: 10.1126/science.abf7914.
- Kofler W. The environmental medical expertise in legal administrative procedures. Janauer G.A., Kerschner F., Oberleitner F. (eds.). The expert in environmental procedures, Vienna: Manz, 1999: 152-215 (in German).
- Sonnleitner S.T., Prelog M, Sonnleitner S. et al. Cumulative SARS-CoV-2 mutations and corresponding changes in immunity in an immunocompromised patient indicate viral evolution within the host. Nat. Commun., 2022; 13: 2560.


