Posterior reversible encephalopathy syndrome in children: a case report
Автор: Gulyamova Durdona Nasriddinovna, Mukhamedov Akmal Asatulla Ugli
Журнал: Re-health journal @re-health
Рубрика: Неврология
Статья в выпуске: 4 (8), 2020 года.
Бесплатный доступ
Posterior reversible encephalopathy syndrome (PRES) is a clinical and radiological entity. The article describes the clinical manifestations, radiological signs, possible mechanisms of pathogenesis, course, and outcomes of this type of encephalopathy. We present a case of a pediatric patient with posterior reversible encephalopathy syndrome. It is noted that clinical and radiological disorders in PRES are caused by vasogenic cerebral edema. Only brain MRI is an informative method for diagnosis of the PRES. It was emphasized that timely diagnosis of the PRES and adequate management lead to relief of the clinical and radiological disorders and that the first emergency aid is the estimation and elimination of the causes of the PRES [17].
Posterior reversible encephalopathy syndrome, headaches, epilepsy, heart attack, visual impairment, vasogenic edema, neuroimaging
Короткий адрес: https://sciup.org/14125607
IDR: 14125607 | DOI: 10.24411/2181-0443/2020-10161
Текст научной статьи Posterior reversible encephalopathy syndrome in children: a case report
Introduction. In recent decades, when the widespread use of MRI has come into clinical practice, a number of pathological conditions have been identified that often mimic acute disorders of cerebral circulation, among which a special role is played by posterior reversible leukoencephalopathy syndrome. Posterior Reversible Encephalopathy Syndrome (PRES) was described at the end of the 20th century. by J. Hinchey et al. [1,9,10]. Posterior reversible encephalopathy syndrome (PRES) is a clinical and radiological entity that causes reversible subcortical vasogenic edema, predominantly in the parietooccipital areas [8,15,20,22].
The clinical course of PRES develops acute or subacutely, in the period of several hours to several days [1,4,19]. Classical manifestations of PRES are severe headache, nausea, vomiting, impaired consciousness, seizure, and visual disturbances that develop on the background of increased blood pressure [12, 21]. Impaired consciousness ranges from mild confusion, stupor, or even coma. The clinical symptoms of this syndrome are often non-specific, so the diagnosis can be difficult to establish.
Numerous literature data indicate that PRES usually occurs between the ages of 20 and 50 (42–45 years) [5], although some authors consider the syndrome to appear at any age (even from early childhood to senile ages) [6].
Case Report. We present a clinical example, which for the first time in our practice was confirmed by a typical picture of changes in MRI scan, described in foreign literature as manifestations of posterior reversible encephalopathy syndrome.
A 7-year-old boy was admitted to a local hospital complaining of headache, nausea, dizziness and seizure that had progressed over 1 week. His history included until 7 years was considered healthy child. From the anamnesis, the child suffered from upper respiratory infection two weeks ago. A week ago, at school, the boy became ill: severe headache, nausea, gait disturbances and decreased visual acuity . Five days later, the child had seizure, generalized tonic convulsions with focal onset.
Upon admission to the hospital, the patient had altered consciousness and makes poor contact. His blood pressure was 130/80 mmHg. And the patient was hospitalized with a diagnosis of “Somatoform autonomic dystonia with the hypertonic type”. In the first hours of stay in the department, the condition worsened, as progressing of neurological symptoms, repeated convulsions, lethargy. In neurological status: horizontal nystagmus, flattening of the left nasolabial fold, deviation of the tongue to the right. On the left side, there was an increased tendon reflex and a positive sign of Babinski.
Laboratory investigations were without any significant abnormalities. The examination by ophthalmoscopy does not show any changes of the eye fundus. EEG report: Interhemispheric asymmetry, there are diffuse slow waves predominantly over left parietooccipital areas. Encephalopathy of the posterior left quadrants. MRI (figure1) report: Signs of pathological intensity of the cortex and subcortical sections of the fronto-parieto-occipital regions, extended intracerebral areas, of both cerebral hemispheres and left cerebellar hemisphere, high-likely PRES.
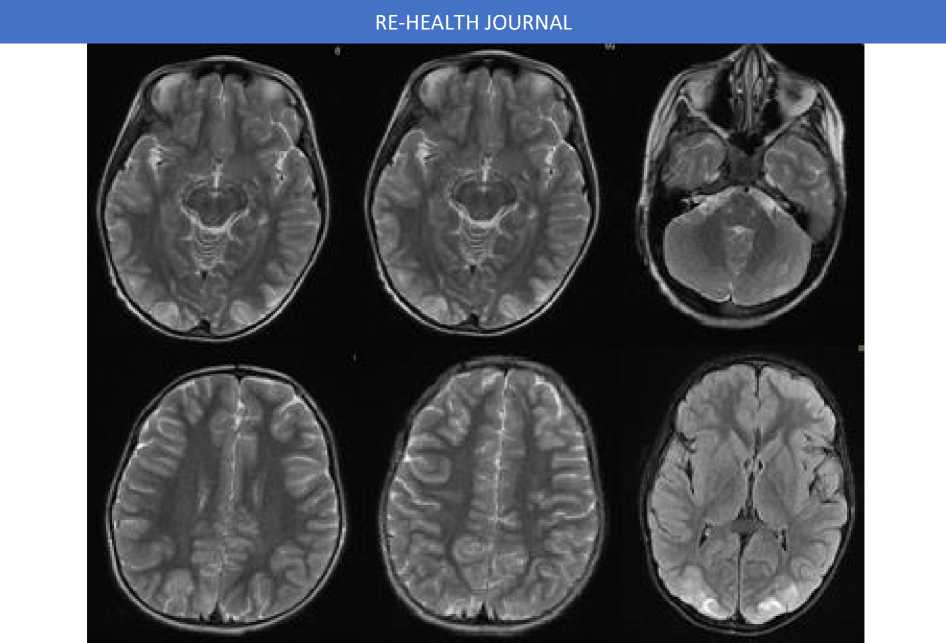
Figure1 : MRI findings of the present case (see text).
He was transferred to the intensive care unit with immediate initiation of intravenous Magnesium Sulfate (30mg/kg/day), Midazolam (0.15mg/kg/once), and antihypertensive (Enalapril 5mg/day) and diuretic (Acetazolamide 10mg/kg/day) therapy. The neurological symptoms rapidly improved by therapy, four days later. Blood pressure decreased to normal ranges and general cerebral and focal symptoms almost disappeared by the 10th day after management. He was discharged without any specific treatment.
Discussion. This complex of symptoms is called posterior reversible encephalopathy syndrome, or reversible posterior leukoencephalopathy syndrome (RPLS) in English literature. In the Russian-language literature, this name is translated as “posterior reversible encephalopathy” (PRE) [2]. Also, the terms “hypertensive encephalopathy” and “reversible posterior cerebral edema syndrome” are used to describe the syndrome [3,18].
Currently, there are two theories of the pathogenesis of radiological changes in PRES. According to the first, earlier theory, cerebral vasospasm, which occurs in response to a sudden increase in systemic blood pressure, leads to swelling of the brain substance mainly in the region of adjacent zones of blood circulation [7]. A more recent theory, second, is based on the results of studying diffusion-weighted images: increased systemic blood pressure disrupts the autoregulation of cerebral blood flow, causing brain hyperperfusion and passive stretching of cerebral arterioles with subsequent interstitial fluid extravasation and the development of local parenchymal hydrostatic edema [4,16].
The main clinical sign is a headache -bilateral and diffuse, although in some cases it can be localized in the occipital region. Headache can be combined with other symptoms - nausea, vomiting, diplopia, increased blood pressure and photosensitivity. A minority has less intense or subacute headaches, and very rarely there are no headaches.
Epileptic seizures often develop at the onset of the disease and almost always represent secondary generalized tonic-clonic seizures, which are often preceded by an aura in the form of visual hallucinations [14]. Epileptic paroxysms in PRES can be non-convulsive and therefore are often skipped by medical personal in the absence of appropriate alertness and EEG control. The presence of non-convulsive status epilepticus should be considered if the patient retains a changed consciousness for a long time, which may be mistaken for postictal drowsiness or confusion.
In some cases, focal neurological symptoms can occur up to the development of deep paresis, gross sensitive disorders, and discoordination disorders. When examining with fundoscopy, pathology is usually not detected. Repeated episodes of PRES are rare.
As we mentioned above, PRES is a reversible subcortical vasogenic edema, predominantly in the parietooccipital areas, however, it should be noted that the term “posterior” is not represented the only exact location of the process, since the cortex, frontal lobes, basal ganglia, and the brainstem may also be involved. This unique syndrome is characterized by reversible leukoencephalopathy, in the absence of significant destruction of the white matter. But PRES is a potentially lifethreatening neurological syndrome and, in the absence of timely treatment, can be complicated by the development of massive cerebral stroke, its early diagnosis, which determines the correct treatment of patients, is especially important.
In most cases, this syndrome is often mistakenly regarded as a bilateral stroke in the territory of the posterior cerebral arteries due to embolic occlusion of the distal main artery, which entails inadequate treatment and, accordingly, further an unfavorable prognosis for the patient.
PRES is not an independent nosological unit but simultaneously serves as a full clinical and radiological syndrome.
In our case, the diagnosis was more complicated and was made on the basis of clinical signs, the course of the disease, and neuroimaging. In our patient, the lesions were symmetrically in both hemispheres with the predominant involvement of the parieto-occipital region of the brain.
Neuroimaging changes in this pathology have a characteristic pattern and therefore can become the key to making a diagnosis. If its suspected that the presence of PRES, it is desirable to obtain MRI scan diffusion-weighted images, which is necessary for differential diagnosis such as cerebral edema (vasogenic or cytotoxic). An increase in the signal in diffusion-weighted images indicates the formation of cerebral stroke with PRES. As the MRI visualization of the brain becomes more accessible, PRES becomes more recognizable, and its frequency of detection increases.
Conclusion. An analysis of a neurological study conducted by this case allows us to conclude that only brain MRI is an informative method, which identifies characteristic changes in white matter and excludes diseases that resemble clinical manifestations (neoplasms, demyelinating diseases, cerebrovascular disorders).
Early and correct diagnosis of the syndrome of posterior reversible encephalopathy is important due to the fact that timely initiated antihypertensive and anti-edematous therapy contributes to the complete reverse development of clinical and radiological signs.
Список литературы Posterior reversible encephalopathy syndrome in children: a case report
- V.V. Gudkova, E.I. Kimelfeld, L.V. Stakhovskaya. A rare syndrome of posterior reversible encephalopathy requiring emergency care. Russian National Research Medical University named after N.I. Pirogova. Consilium Medicum. 2018; 20 (2): 84-89.
- O.I. Yaroshevskaya, O.E. Gurevich, I.M. Drozdova, P.S. Rogatkin. The reversible encephalopathy in children with acute post-streptococcal glomerulonephritis. N.I. Pirogov. Journal of Pediatrics, Russia, 2015/№ 3.
- V.I.Skvortsova, L.V. Gubsky, E.A. Melnikova. Syndrome of posterior reversible encephalopathy. Journal of Neurology and Psychiatry, 5, 2010 page 104-109.
- E.I. Bogdanov, I.A. Khasanov, H.I. Mamedov, D.M. Khasanova. Differential diagnosis of the syndrome of posterior reversible leukoencephalopathy and heart attacks in the territory of the posterior cerebral arteries. Actual problems of medicine. Volume 1, 2012.
- R. Miller, R. Shivashankar, M. Mossa-Basha and D. Gandhi. Reversible cerebral vasoconstrictor syndrome. Part 1: epidemiology, pathogenesis, clinical course. American Journal of Neuroradiology. August 2015.


