Постковидный синдром в виде венозных и артериальных тромбозов, осложненных COVID-19
Автор: Байсекеев Т.А., Деркембаева Ж.С., Мамышов А.Ж., Осмонбекова Н.С., Жолборсов А.А., Кочконбаев Ж.А., Эмилбеков Ф.М., Муратов К.К.
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 6 т.10, 2024 года.
Бесплатный доступ
Постковидный синдром в виде тромбозов является распространенным и опасным осложнением COVID-19.
Covid-19, постковидный синдром, тромбообразование, расслаивающаяся аневризма
Короткий адрес: https://sciup.org/14130487
IDR: 14130487 | УДК: 616.151.5 | DOI: 10.33619/2414-2948/103/30
Текст научной статьи Постковидный синдром в виде венозных и артериальных тромбозов, осложненных COVID-19
Бюллетень науки и практики / Bulletin of Science and Practice
УДК 616.151.5
С 11 марта 2020 года ВОЗ объявила о вспышке коронавирусной пандемии COVID-19 [1]. Этиологическим агентом COVID-19 является вирус SARS-CoV-2, который, в свою очередь, «опирается» на ангиотензин-превращающий фермент 2 (АПФ), являющийся рецептором входа в так называемый организм хозяина для клеточной инокуляции и повреждения органов-мишеней [2]. Во время пандемии COVID-19 наблюдались многочисленные случаи осложнения от заболевания в виде мультиорганного повреждения, в первую очередь, сердечно-сосудистого характера [3], включающего тромбообразование на микро- и макроуровнях [4]. Распространенность тромбов как осложнение среди пациентов с COVID-19 составляет 25%-50% [5].
В обзоре [6] приводятся данные про аортальное тромбообразование, которое было симптоматическим у 56% пациентов с COVID-19 с клиническим проявлением в виде острой ишемии нижних конечностей (у 46%). Общая смертность в популяции составила 30%. Тромбоэмболия среди пациентов с COVID-19 в разы выше в ОИТ, чем в общих отделениях: 48% против 10%, 50% против 18% [7, 8].
Своевременное диагностирование тромбов как осложнения при COVID-актуальная проблема современной системы здравоохранения. В одном французском исследовании [9] признак ТЭЛА был диагностирован спустя 12 дней. В метаанализе 1461 пациентов с COVID-19 у 443 была выявлена тромбоэмболия со смертностью в 25.73% (114 пациентов) [10]. Однако смертность пациентов от тромбоэмболии без COVID-19 была в два раза ниже (11.89%, 121 пациент). В другом метаанализе [11] пациентов с COVID-19 распространенность ТГВ составила 27% (95% ДИ: 21, 34%), ВТЭ 32% (95% ДИ: 25, 40%). Смертность среди пациентов с COVID-19 и тромбоэмболией была гораздо выше в 2.1 раза (95% ДИ: 1.2, 3.6), чем у пациентов без тромбоэмболии. Сохраняющаяся медико-социальная угроза и актуальность COVID-19 основаны на геномных мутациях вируса Sars-Cov-2 таких как Sars-Cov-2 B.1.1.529 омикрон, репродукционное число которого в 2 раза выше, чем дельты и составляет 11.88 (95% ДИ: 9.16-4.61) [12].
Следовательно, вопросы касательно тромбозных осложнений от COVID-19 сохраняют свою актуальность.
Цель исследования: выявить локализацию, частоту, сроки возникновения тромбозов у пациентов, перенесших COVID-19, частоту использованных методов хирургического лечения.
Материалы и методы исследования
Проведено ретроспективное обсервационное исследование на основании изучении данных историй болезней 494 пациентов, госпитализированныхв Национальный Госпиталь Министерства Здравохранения Кыргызской Республики в отделение сосудистой хирургии за период август подекабрь 2020 год, из них были отобраны 239 истории болезней больных, переболевших коронавирусной инфекцией из них 138 женщин 101 мужчин.
Результаты исследования
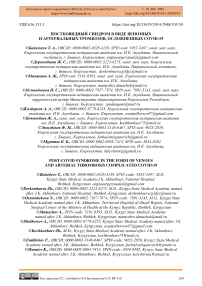
По результатам исследования, основанные на изучении 239 историй болезней пациентов с постковидным синдромом, было выяснено, что венозные тромбозы встречаются на 74% чаще, чем артериальные тромбозы (Рисунок 1).
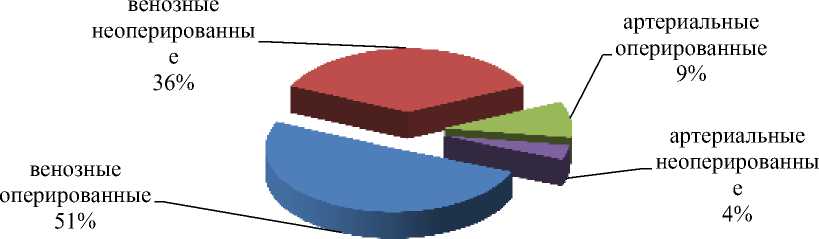
Рисунок 1. Соотношение прооперированных и не прооперированных случаев артериальных и венозных тромбозов.
Таблица 1
СООТНОШЕНИЕ ВИДОВ ТРОМБОЗОВ К ПРОВЕДЕННЫМ ОПЕРАЦИЯМ
С УЧЕТОМ ПОЛОВОЙ ПРИНАДЛЕЖНОСТИ
|
Пол |
Всего |
Артериальные прооперированные |
Артериальные не оперированные |
Венозные прооперированные |
Венозные не оперированные |
|
муж |
101 |
13 |
5 |
48 |
35 |
|
жен |
138 |
9 |
4 |
73 |
52 |
В зависимости от пола: из 239 пациентов, у которых диагностировали тромбоз: 101 мужчин, 138 женщин. Артериальные тромбозы встречались у 18мужчин от общего числа, а у женщин 13. Венозные тромбозы были диагностированы у 83 мужчин и у 125 женщин. У женщин по сравнению с мужчинами, частота заболеваемости на 15,4% выше. Эта тенденция наиболее выражена в нетрудоспособном возрасте от 61 и более лет (Таблица 2).
Таблица 2
РАСПРЕДЕЛЕНИЕ ПО ВОЗРАСТАМ
|
Возраст |
Артериальные прооперированные |
Артериальные не оперированные |
Венозные прооперированные |
Венозные не оперированные |
|
18-30 |
0 |
0 |
4 |
11 |
|
31-45 |
3 |
2 |
22 |
21 |
|
46-60 |
7 |
5 |
35 |
28 |
|
61-более |
12 |
2 |
58 |
29 |
Показано, что пациентов в возрасте:
от 18-30лет: нет по артериальным тромбозам; 15 — с венозными тромбозами, 4 — из которых были прооперированы, а 11 — получили консервативное лечение.
с 31-45лет: у 5 человек диагностирован артериальный тромбоз: 3 — прооперированы, а 2 — получили консервативное лечение; у 43 — диагностирован венозный тромбоз: у 22 — из которых была проведена операция, а 21 — получали консервативное лечение.
с 46-60 лет: у 12 человек диагностирован артериальный тромбоз: 7 — были прооперированы, а 5 — нет; у 63 — диагностирован венозный тромбоз: 35 — прооперированные, а 28 — получили консервативное лечение.
с 61 года и более: у 14 человек был диагностирован артериальный тромбоз: 12 — прооперированы, а 2 — получили консервативное лечение.
Из приведенной Таблицы 1 видно, что больные были в возрасте от 18 до 91 года, основная группа больных по возрастной категории была в пожилом нетрудоспособном возрасте от 61 года и выше (Таблица 2).
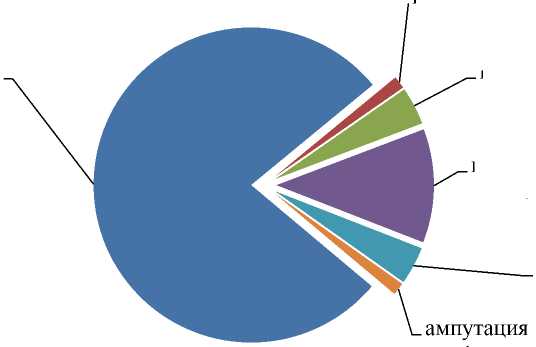
Из 239 пациентов: с г. Бишкек — 105 человек (44%), Ощской области — 3 (1%), с Иссык-Кульской области — 33(14%), с Джалал-Абадской области — 4(2%), с Таласской области — 13(6%), с Чуйской области — 65(27%), с Баткенской области — 3(1%), а с Нарынской области — 13 человек (5%) (Рисунок 2).
Нарынская обл.
Баткенскаяобл.
Чуйская обл.
Таласская обл.
Джалал-Абадская обл.
Иссык-Кульская обл.
Ошская обл.
г.Бишкек
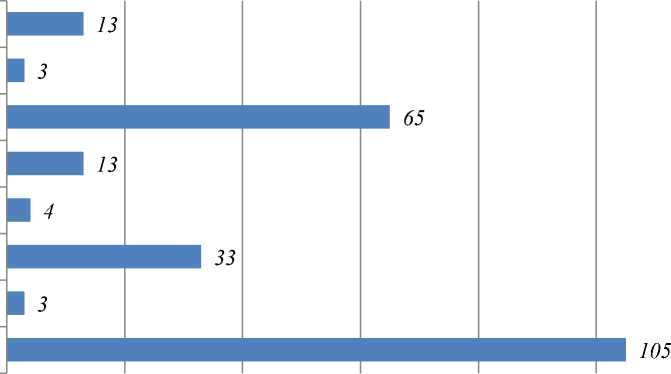
Рисунок 2. Распределение пациентов по регионам получивших лечение в Национальном госпитале(НГ МЗ КР)
Исходя из этих данных следует, что больше всего в НГ МЗ КР проходили лечение лица с пропиской в г. Бишкек и жители Чуйской области. И меньше всего людей с других регионов.
На Рисунке 3 показано количественное соотношение из 239 человек, у которых имелись сопутствующие заболевания — это 138 человек (58%) и те, у кого их не было — 101 человек, что составляет 42%.
с сопутствующими болезнями 58%
без сопутствующих болезней 42%
Рисунок 3. Соотношение сопутствующих заболеваний у пациентов.
Это может обуславливаться тем, что люди с сопутствующими заболеваниями, в частности, с заболеваниями сердечно-сосудистой системы больше подвержены к постковидным осложнениям в виде тромбозов и тромбоэмболий. На Рисунке 4 размещена информация о видах операций при артериальных тромбозахвыполненных в процентом соотношении. Из чего следует, что в 50% случаев при артериальных тромбозах проводилась — тромбоэмболэктомия, в 25% случаев проводилась ампутация, в 13% случаев — фасциотомия, в 8% случаев была операция поясничной симпатэктомии, а реже всего в 4% случаев проводилась операция подмышечно-плечевое аутовенозное шунтирование.
поясничная симпатэктомия 8% ампутация 25% тромбоэмболэкто мия 50%
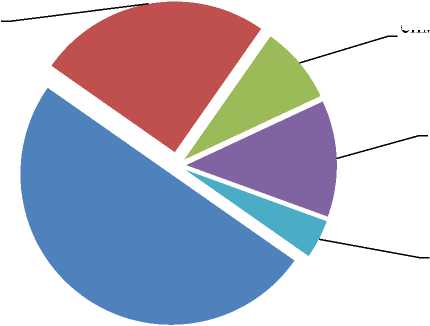
фасциотомия 13% подмышечноплечевое аутовенозное шунтирование 4%
Рисунок 4. Виды операций при артериальных тромбозах в процентом соотношении.
Причиной частого проведения тромбоэмболэктомий может быть то, что это один из первых этапов в лечении артериальных тромбозов. Также показателем опасности артериальных тромбозов может служить высокий процент операций по ампутации, что доказывает риск серьезных необратимых реакций в данной патологии.
В данном случае: перевязка большой подкожной вены(БПВ) по Троянову составляет 78% операций, перевязка по поверхностной бедренной вены(ПБВ) составляет 9%, частота ретроградной-илиокаваграфии(РИКГ) с имплантацией противоэмболического кава- фильтра в нижнюю полую вену 4% и перевязки общей бедренной вены(ОБВ) составляет по 4%, ампутации и перевязки малой подкожной вены(МПВ) составляют по 1% (Рисунок 5).
перевязка МПВ перевязка БПВ по Троянову 78%
РИКГ 4% перевязк ОБВ 4%
1%
Рисунок 5. Виды операций при венозных тромбозах
перевязка ПБВ 12%
Следует отметить, что больше всего венозные тромбозы были локализованы в венах в нижних конечностей, и чаще всего проводились операции по перевязке большой подкожной вены (БПВ) по Троянову.
По результатам исследования и анализа, основанного на конкретном клиническом случае, было выявлено, что последствия постковидного синдрома могут проявлятся после длительных сроков вследствие перенесенной инфекции.
Клинический случай. 6-ноября 2020-года в НГ МЗ КР отделение сосудистой хирургии поступил мужчина 42 лет с Джалал-Абадской области. При этом больной предъявлял жалобы на шум в ушах пульсирующего характера, головную боль и боли в животе с иррадиацией в поясничную и в подвздошную области.
Со слов больного работал на стройке в Санкт-Петербурге на протяжении двух лет. В мае 2020-года переболел коронавирусной инфекцией. А в сентябре этого же года попал в Санкт-Петербургскую «Городскую Мариновскую больницу» в отделение терапии с сильными болями в животе и с АД 240 мм ртутного столба. Питерские доктора, обследовав поступившего больного, нашли у него кучу хронических заболеваний, о которых ранее он даже не подозревал. Врачи данной больницы предположили, что обострение хронических заболеваний было тесно связано с перенесенным COVID-19, так как именно после перенесенной инфекции, появились данные осложнения. Там он получал лечение по поводу врожденная аномалия сосудов: Кинкингинфраренального отдела брюшной аорты на уровне L2 позвонка. Удвоение правой почечной артерии. Дистопия правой почки. Вторичная реноваскулярная артериальная гипертензия 3ст. Г ипертонический криз острая левожелудочковая недостаточность(ОЛЖН) KillipIII от 30.08.2020, купирован. Хроническое расслоение нисходящего отдела аорты, с распространением на Левую общую подвздошную артерию (ЛОПА), Левая Наружная Подвздошная Артерия (ЛНПА)III расслоения по M. DeBaky. Самостоятельная диссекция ЛОПА, с распространением на Левую Внутреннюю Подвздошную Артерию(ЛВПА). Окклюзия Наружной Подвздошной Артерии (НПА). Хронический гастродуоденит. Во время лечения была выявлена дистония почки с аномалией правой почечной артерии. Был консультирован хирургом, рекомендовано было оперативное лечение, от которого он отказался. По приезду в КР обратился в сосудистую хирургию НГ МЗ КР, в связи с усилениями вышеперечисленных жалоб. Был госпитализирован в экстренном порядке для стационарного лечения.
Объективно: общее состояние средней тяжести, сознание ясное, положение, вынужденное. Кожа и видимые слизистые обычной окраски, без патологических высыпаний. Дыхание жесткое, одинаково проводится с обеих сторон, в нижних отделах ослабленно, хрипов нет. Сердечный тон ритмичный, ясный. АД-180-220/120-130 мм. рт. ст. ЧСС-84 уд в мин. Язык чистый, влажный. Живот слегка вздут, умеренно болезнен в зоне правой подвздошной области. Перитонеальных явлений нет. Стул и диурез не нарушен.
Локально: Живот слегка вздут, при пальпации отмечается болезненность в левой подвздошной и поясничной области с обеих сторон. Симптом Пастернацкого справа слабо положительная.
УЗДС аорты от 03.11.2020 г. из амбулаторной карты: Осмотрсупраренального сегмента брюшной аорты ограничен. На уровне почечных артерий аорта диаметром 19мм, с уровня отхождения почечных артерий аорта С-образно изгибается кпереди и аневризматически расширяется на всем протяжении с переходом в общие подвздошные артерии. При ЦДК аневризма определяется двух-просветным (диссекция) с наибольшим переднезадним размером 39мм, поперечным размером 45 мм, стенкой толщиной до 1,4 мм. Диаметр общих подвздошных артерий расширен до 24 мм, С-образный кинкинг обеих наружных подвздошных артерий (д = 10-8 мм) и левой внутренней подвздошной артерии (д = 12 мм), ТИМ утолщен до 2,4 (вероятно давнее кровоизлияние в интиму артерий). В аневризме и подвздошных артериях магистрально измененный, монофазный и бифазный с турбулентным характером кровоток. Почечные артерии лоцировать не удается. Артерии нижних конечностей: левая ГБА тотчас после отхождения удваивается, одна ветвь окклюзирована прослеживается на всем протяжении 16 мм кровоток в остальных магистральных артериях магистрального типа, трехфазный, прослеживается на всем протяжении. НПВ и подвздошные вены проходимы, сжимаемы (Рисунок 6).

Рисунок 6. Схема кровотока пациента
КТ панаортография от 05.11.2020 г.: Данные за умеренное расширение восходящего отдела аорты. Расслоение в инфраренальном сегменте брюшной аорты с распространением на общую, наружную и внутреннюю подвздошные артерии слева. Добавочные почечные артерии справа. Правосторонний кинкинг брюшной аорты и общей подвздошной артерии слева. Незавершенная ротация и дистопия правой почки.
ОАК от 16.11.2020. Общий белок — 73 г/л., Магний — 0,92 ммоль/л, Кальций — 2,25 ммоль/л, Натрий — 141 ммоль/л, Калий — 4,9 ммоль/л., Альбумин — 70,4%, Глобулины: Альфа — 1-1,2%, Альфа — 2-5,6%; Бета — 9,5%; Гамма — 13,3%. Коэффициент альбумин\глобулин — 2,4.
От 12.11.2020 г. Креатинин — 79,5 г/л.; RW — от 06.11.2020 — отриц.; ССК 85%; Фибриноген «А» — 3996. ОАК от 10.11.2020 НВ — 131 г/л, эр. — 4,7 млн., Л — 6-4 тыс., п — 0%, с — 61%, э — 7%, л — 25%, м — 7%, Ht — 38% СОЭ — 11 мм ч.; От 08.11.2020г. — Общий билирубин — 8,3 ммоль/л; прямой — 0, креатинин — 165 ммоль/л.
ССК от 11.11.2020 г.: Тромботест — 6 ст, ПТИ — 100%; Фибриноген «А» — 2664.
Консультация уролога от 31.11.2020 г. Аномалия развития мочеполовой системы. Тазовая дистопия правой почки. Артериальная гипертензия. Хронический пиелонефрит в стадии ремиссии. ХПН интерметтирующая стадия.
Консультация нефролога от 18.11.2020 г.; от 24.11.2020 г. Заключение: Хронический пиелонефрит в стадии ремиссии. ХБПС3бАо. ХПН. Субклиническая стадия.
На основании вышеперечисленных данных выставлен клинический диагноз: Расслаивающаяся аневризма инфраренального отдела брюшной аорты. Вазоренальная гипертензия. Болевой синдром.
19.11.2020: Была проведена девятичасовая операция: Лапаратомия. Нефроэктомия справа. Ликвидация аневризмы аорты. Аорто-бедренное бифуркационное протезирование с протезом «ЭКОФЛОН». Входе длительной операции был применен эпидуральный наркоз с последующим применением комбинированного интубационного наркоза.
Обсуждение. 11 марта 2020 года ВОЗ объявила о вспышке коронавирусной пандемии COVID-19 [1]. Этиологическим агентом COVID-19 является вирус SARS-CoV-2, который, в свою очередь, «опирается» на ангиотензин-превращающий фермент 2 (АПФ), являющийся рецептором входа в так называемый организм хозяина для клеточной инокуляции и повреждения органов-мишеней [2].
Коагулопатия (как составная системного воспалительного ответного синдрома) осложнение (20-50%) при COVID-19 [13].
В датском исследовании [14] тромбозы были выявлены у 31% пациента с COVID-19, 3.7% артериального характера. В метаанализе [15] 102 обсервационных исследований (64 503 пациентов) венозные тромбозы были выявлены у 14.7% пациентов с COVID-19 (95% ДИ 12.1%-17.6%), ТЭЛА — в 7.8% случаях (95% ДИ 6.2%-9.4%), ТГВ — в 11.2% (95% ДИ 8.414.3%). Распространенность венозных тромбозов была гораздо выше в ОИТ, чем в общих отделениях: 23.2% (95% ДИ 17.5-29.6%) против 9.0% (95% ДИ 6.9-11.4%).
По результатам исследования НГ МЗ КР, основанного на изучении 239 историй болезней пациентов с постковидным синдромом, было выяснено, что венозные тромбозы встречаются на 74% чаще, чем артериальные тромбозы. Одним из осложнений COVID-19 является абдоминальный аортальный синдром, включающий в себя также аневризмы абдоминальной аорты (ААА). В литературе описано несколько клинических случаев [4, 1618]. В одном из них [19] описан клинический случай 5.3-сантиметровой ААА у 65-летнего пациента с бессимптомным COVID-19. Опасность ААА заключается в риске разрыва сосуда и смерти [2]. Смертность при остром тромбозе инфраренального отдела ААА доходит до 75% (без хирургии), от 20% до 50%-даже в случае квалифицированной хирургической помощи [20].
Своевременное диагностирование тромбов как осложнения при COVID-актуальная проблема современной системы здравоохранения. В одном французском исследовании [9] признак ТЭЛА был диагностирован спустя 12 дней. В исследовании НГ МЗ КР описан клинический случай отдаленного тромбозного осложнения в виде расслаивающейся аневризмы инфраренального отдела брюшной аорты у 42-летнего пациента с COVID-19. В мае 2020-года этот пациент переболел коронавирусной инфекцией, а в сентябре этого же года попал в Санкт-Петербургскую «Городскую Мариновскую больницу» в отделение терапии с сильными болями в животе и с АД 240 мм ртутного столба. Следовательно, перенесенная болезнь COVID-19 стало триггером осложнения уже имеющегося сопутствующего заболевания в виде аневризмы аорты. А период проявления данного тромбозного осложнения составил не 12 дней как в упомянутом исследовании [9], а 5 месяцев с мая по сентябрь.
В обзоре показано резкое снижение количества скрининга и диагностики ААА в связи с пандемией COVID-19: в районе Лондона Южный Лондон, в среднем, 271- 667 пациентов с ААА не смогли пройти скрининг и диагностику. Несмотря напредпринимаемые исследования с демонстрацией эпидемиологической распространенности ААА при COVID-19, уровень доказанности того, что ААА является тромбозным осложнением COVID-19, недостаточен [18, 21].
Cледовательно, предпринятое исследование коллективом НГ МЗ КР по итогам лечения пациентов с тромбозными осложнениями в период COVID-19 имеет актуальное значение.
Теоретические гипотезы о наличии связи между двумя явлениями основываются на понижении уровня ангиотензин-превращающего фермента 2 и активации ренин– ангиотензин–альдостероновой системы с последующим гипертоническим статусом [22] на активации макрофагов, вырабатывающих коллагеназус последующим повреждением стенки сосуда [23].
В метаанализе [2] сделана попытка обоснования патогенетического влияния COVID-19 на ААА. Показано, что влияние происходит в силу: повышенной активности рецептора АПФ-ангиотензина II-AT1 в результате снижения реципрокной активации ACE2-ангиотензина 1-7-Mas; повышенной продукции проаневризматических медиаторов, стимулируемых вирусными спайковыми белками в ACE2-негативных миелоидных клетках или ACE2-экспрессирующих сосудистых структурных клетках; повышенном локальном или системном перекрестном взаимодействии между вирусными несосудистыми, нелейкоцитарными клетками, экспрессирующими ACE2, посредством распознавания лигандов их родственных рецепторов лейкоцитов; гипоксемии и повышенном системном воспалительном тонусе, наблюдаемые во время тяжелого заболевания COVID-19. Данная гипотеза нашла свое подтверждение в одном итальянской серии [24] 4 клинических случаев ААА при COVID-19. Показано,чтоCOVID-19 дал локальное и системное инфекционное осложнение ААА с последующим цитокиновым штормом.
В период COVID-19 наблюдается резкое снижение элективных хирургических вмешательств в связи с ААА [21].
Предлагаемая идея об откладывании хирургических операций при ААА из-за пандемии выглядит спорной. Согласно Американской коллегии хирургов [25] хирургическое лечение ААА должно быть отложено при размере<6.5 cантиметрови иногда при>6.5. Однако данная идея имеет своих противников. Так, в одном исследовании [26] показано, что риск смерти 60летнего пациента с COVID-19 составляет 0.6%, а при ААА (даже в диапазоне 5.5-5.9 см) 0.8% за 3 месяца и 1.9% за 6. Нет также единого консенсуса по поводу хирургического подхода (открытого/эндоваскулярного) в случае тромбозного осложнения в виде ААА при COVID19 [21].
Выдвигаются [19, 27-29] тезисные утверждения о плюсах эндоваскулярного подхода, выраженных меньшим сроком операции и послеоперационного наблюдения пациента, а также более высокой степенью инфекционной безопасности для хирургической бригады. В одном клиническом случае [20] описано успешное применение эндоваскулярного подхода при остром тромбозе 8-сантиметровой инфраренальной ААА у 89-летнего пациента с COVID-19. После трех месяцев наблюдения в общем отделении данный пациент был выписан без признаков каких-либо васкулярных осложнений. В ретроспективном обсервационном исследовании НГ МЗ КР на основании изучения данных историй болезней 494 пациентов, госпитализированных в в отделение сосудистой хирургии за период август по декабрь 2020 год, были отобраны 239 истории болезней больных, переболевших коронавирусной инфекцией из них 138 женщин 101 мужчин. В 50% случаев при артериальных тромбозах проводилась тромбоэмболэктомия, в 25% случаев проводилась ампутация, в 13% случаев фасциотомия, в 8 % случаев была операция поясничной симпатэктомии, а реже всего в 4% случаев проводилась операция подмышечно-плечевое аутовенозное шунтирование. Кава-фильтры были установлены только в 4% случаев, в 78% случаев была проведена хирургическая перевязка по Троянову.
Результат клинического случая 42-летнего пациента , перенесшего COVID-19 в мае 2020, у которого данная инфекция в сентябре 2020 года (то есть через пять месяцев) дало осложнение уже имеющемуся заболеванию в виде аневризмы инфраренального отдела брюшной аорты. Была проведена девятичасовая операция: Лапаратомия. Нефроэктомия справа. Ликвидация аневризмы аорты. Аорто-бедренное бифуркационное протезирование с протезом «ЭКОФЛОН».
Было проведено открытое хирургическое вмешательство по нескольким причинам. Первое. КР входит в число стран с невысоким уровнем экономического дохода. Эндоваскулярные вмешательства, как правило, проводятся в современных высокотехнологических госпиталях с соответствующей подготовкой кадров. Второе. У определенной части наших пациентов (если говорить в общем про исследование), а также у нашего отдельного пациента (если говорить про конкретный клинический случай), имелись тяжелые сопутствующие заболевания, размеры тромбозных образований, аневризмы аорты (в случае отдельного пациенты) были показанием к проведению открытой хирургии.
Вывод
Венозные тромбозы в качестве постковидного синдрома встречаются гораздо чаще, чем артериальные тромбозы. Частота заболеваемости тромбозным постковидным синдромом у женщин по сравнению с мужчинами существенно выше. Больше всего постковидные венозные тромбозы локализованы в венах нижних конечностей. Люди с сопутствующими заболеваниями, в частности, с заболеваниями сердечно-сосудистой системы, гораздо больше подвержены постковидным осложнениям в виде тромбозов и тромбоэмболий. Аневризма абдоминальной аорты-редкое, но чрезвычайно опасное заболевание в связи с риском разрыва сосуда, и данное постковидное осложнение может проявляться через длительный период времени. При постковидном синдроме в виду тромбозов открытые хирургические вмешательства являются эффективными и безопасными.
Список литературы Постковидный синдром в виде венозных и артериальных тромбозов, осложненных COVID-19
- Boccia M., Aronne L., Celia B., Mazzeo G., Ceparano M., D'Agnano V., Perrotta F. COVID-19 and coagulative axis: review of emerging aspects in a novel disease // Monaldi Archives for Chest Disease. 2020. V. 90. №2. https://doi.org/10.4081/monaldi.2020.1300
- Xu B., Li G., Guo J., Ikezoe T., Kasirajan K., Zhao S., Dalman R. L. Angiotensinconverting enzyme 2, coronavirus disease 2019, and abdominal aortic aneurysms // Journal of Vascular Surgery. 2021. V. 74. №5. P. 1740-1751. https://doi.org/10.1016/j.jvs.2021.01.051
- Hu Y., Sun J., Dai Z., Deng H., Li X., Huang Q., Xu Y. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis // Journal of clinical virology. 2020. V. 127. P. 104371. https://doi.org/10.1016/j.jcv.2020.104371
- Webster W. Z., Sraow A., Morel K. C. Abdominal aortic thrombosis as initial presentation of COVID-19 infection: A case report //World Journal of Clinical Infectious Diseases. 2020. V. 10. №3. P. 42-46. https://doi.org/10.5495/wjcid.v10.i3.42
- Beun R., Kusadasi N., Sikma M., Westerink J., Huisman A.Thromboembolic events and apparent heparin resistance in patients infected with SARS‐CoV‐2 // International journal of laboratory hematology. 2020. V. 42. №Suppl 1. P. 19. https://doi.org/10.1111/ijlh.13230
- Karabulut K., Kapici A., Andronikashvili A., Morgan J. A review of aortic thrombosis in COVID-19 infection // Exploration of Medicine. 2021. V. 2. №5. P. 410-422. https://doi.org/10.37349/emed.2021.00059
- Middeldorp S., Coppens M., van Haaps T. F., Foppen M., Vlaar A. P., Müller M. C., van Es N. Incidence of venous thromboembolism in hospitalized patients with COVID‐19 // Journal of Thrombosis and Haemostasis. 2020. V. 18. №8. P. 1995-2002. https://doi.org/10.1111/jth.14888
- Bompard F., Monnier H., Saab I., Tordjman M., Abdoul H., Fournier L., Revel M. P.Pulmonary embolism in patients with COVID-19 pneumonia // European Respiratory Journal. 2020. V. 56. №1.
- Samajdar S. S., Sam P. A., Moitra S., Ray Y., Pal J., Joshi S. R., Tripathi S. K. Risk Benefit Analysis in Reference to use of LMWH in COVID-19 // J Assoc Physicians India. 2020. V. 68. №9. P. 52-61. https://doi.org/10.5495/wjcid.v10.i3.42
- Wang C., Zhang H., Zhou M., Cheng Y., Ye L., Chen J., Feng Z. Prognosis of COVID-19 in patients with vein thrombosis: a systematic review and meta-analysis // Eur Rev Med Pharmacol Sci. 2020. P. 10279-10285. https://doi.org/10.26355/eurrev_202010_23252
- Kollias A., Kyriakoulis K. G., Lagou S., Kontopantelis E., Stergiou G. S., Syrigos K. Venous thromboembolism in COVID-19: A systematic review and meta-analysis // Vascular medicine. 2021. V. 26. №4. P. 415-425. https://doi.org/10.1177/1358863X21995566
- Chen J., Wang R., Gilby N. B., Wei G. W. Omicron (B. 1.1. 529): Infectivity, vaccine breakthrough, and antibody resistance (preprint). 2021.
- Gomez-Mesa J. E., Galindo-Coral S., Montes M. C., Martin A. J. M. Thrombosis and Coagulopathy in COVID-19 // Current problems in cardiology. 2021. V. 46. №3. P. 100742. https://doi.org/10.1016/j.cpcardiol.2020.100742
- Klok F. A., Kruip M. J. H. A., Van der Meer N. J. M., Arbous M. S., Gommers D. A. M. P. J., Kant K. M., Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19 // Thrombosis research. 2020. V. 191. P. 145-147. https://doi.org/10.1016/j.thromres.2020.04.013
- Tan B. K., Mainbourg S., Friggeri A., Bertoletti L., Douplat M., Dargaud Y., Lega J. C. Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis // Thorax. 2021. V. 76. №10. P. 970-979.
- Roncati L., Manenti A., Manco G., Farinetti A. Abdominal aortic thrombosis complicating COVID-19 pneumonia // Annals of Vascular Surgery. 2020. P. 1-2. https://doi.org/10.1016/j.avsg.2020.05.033
- Yarımoglu R., Yarımoglu S., Tastan H., Erkengel H. I. Acute infrarenal abdominal aortic occlusion in a patient with COVID-19 // Annals of Saudi Medicine. 2021. V. 41. №6. P. 392-395. https://doi.org/10.5144/0256-4947.2021.392
- Riley C. J., Teixeira P. Development of symptomatic inflammatory aneurysm treated with endovascular repair in coronavirus disease 2019 infected patient // Journal of Vascular Surgery Cases, Innovations and Techniques. 2021. V. 7. №2. P. 193-196. https://doi.org/10.1016/j.jvscit.2021.03.003
- Yammine H., Ballast J. K., Poulsen N., Arko III F. R. Endovascular aortic repair in an asymptomatic COVID-19-positive patient with a symptomatic inflammatory abdominal aortic aneurysm // Journal of Vascular Surgery Cases, Innovations and Techniques. 2020. V. 6. №4. P. 531-533. https://doi.org/10.1016/j.jvscit.2020.08.016
- Robaldo A., Apostolou D., Persi F., Peano E., Maione M. EVAR Solution For Acutely Thrombosed Abdominal Aortic Aneurysm in a Patient with COVID-19 // EJVES Vascular Forum. Elsevier, 2022. V. 54. P. 41-43. https://doi.org/10.1016/j.ejvsvf.2022.01.006
- Bissacco D., Franchin M., Piffaretti G., Luzzani L., D'Oria M., Casana R., Trimarchi S. Impact of COVID-19 on aortic operations // Seminars in Vascular Surgery. WB Saunders, 2021. V. 34. №2. P. 37-42. https://doi.org/10.1053/j.semvascsurg.2021.04.002
- Sun P., Lu X., Xu C., Sun W., Pan B. Understanding of COVID‐19 based on current evidence // Journal of medical virology. 2020. V. 92. №6. P. 548-551. https://doi.org/10.1002/jmv.25722
- Nishiga M., Wang D. W., Han Y., Lewis D. B., Wu J. C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives // Nature Reviews Cardiology. 2020. V. 17. №9. P. 543-558. https://doi.org/10.1038/s41569-020-0413-9
- Bozzani A., Arici V., Franciscone M., Ticozzelli G., Sterpetti A. V., Ragni F. COVID-19 patients with abdominal aortic aneurysm may be at higher risk for sudden enlargement and rupture // Journal of Vascular Surgery. 2022. V. 75. №1. P. 387-388. https://doi.org/10.1016/j.jvs.2021.10.003
- Rusch V. W., Wexner S. D., Atala A., Atkinson J. L., Denneny III J. C., Eberlein T. J., Wood D. E. The American College of surgeons responds to COVID-19 // Journal of the American College of Surgeons. 2020. V. 231. №4. P. 490-496. https://doi.org/10.1016/j.jamcollsurg.2020.06.020
- McGuinness B., Troncone M., James L. P., Bisch S. P., Iyer V. Reassessing the operative threshold for abdominal aortic aneurysm repair in the context of COVID-19 // Journal of Vascular Surgery. 2021. V. 73. №3. P. 780-788. https://doi.org/10.1016/j.jvs.2020.08.115
- Shih M., Swearingen B., Rhee R. Ruptured abdominal aortic aneurysm treated with endovascular repair in a patient with active COVID-19 infection during the pandemic // Annals of Vascular Surgery. 2020. V. 66. P. 14-17. https://doi.org/10.1016/j.avsg.2020.05.001
- Rinaldi L. F., Marazzi G., Marone E. M. Endovascular treatment of a ruptured pararenal abdominal aortic aneurysm in a patient with coronavirus disease-2019: suggestions and case report // Annals of Vascular Surgery. 2020. V. 66. P. 18-23. https://doi.org/10.1016/j.avsg.2020.05.011
- Shih M., Swearingen B., Rhee R. Ruptured abdominal aortic aneurysm treated with endovascular repair in a patient with active COVID-19 infection during the pandemic // Annals of Vascular Surgery. 2020. V. 66. P. 14-17. https://doi.org/10.1016/j.avsg.2020.05.001