Preserving children's health: search for the ways of solving relevant issues
Автор: Shabunova Alexandra A., Korolenko Alexandra V., Natsun Leila N., Razvarina Irina N.
Журнал: Economic and Social Changes: Facts, Trends, Forecast @volnc-esc-en
Рубрика: Social and economic development
Статья в выпуске: 2 т.14, 2021 года.
Бесплатный доступ
Changed social reality, caused by the coronavirus pandemic (COVID-19), made attention to population’s health, its risks, and defining factors relevant. Nowadays, an individual’s personal responsibility for own health and coherence of various social institutions’ activities in the formation of children’s health are of particular importance. The article is devoted to an analysis of children’s health and search for the ways of its improvement. The authors explore the issues of availability and quality of medical services, safeguard of children’s health and discuss the barriers to inter-institutional cooperation in this field, as well as ways of overcoming them. To achieve these objectives, we used quantitative and qualitative sociological methods: a sociological survey of families with children aged 3-17 years, monitoring observation of cohorts of families with children, focus group studies of parents of children aged 3-17 years, an expert survey of specialists of the regional health system and members of government authorities. The authors reveal several issues: decline of children’s health potential in growing; insufficient awareness of parents about the state, forms, and methods of preserving and strengthening children’s health, discrepancy between parents’ ideas about their own competence in this matter with reality; lack of narrow-profile specialists in children’s medical institutions; absence of medical workers among full-time staff of educational organizations; queues and complexity of making appointments with specialists; low availability of free and high cost of paid medical services; insufficient information interaction between medical, educational organizations and parents in the prevention of diseases; lack of parents’ knowledge of full information about objectives of professional examinations and insufficient awareness of the importance of further actions to restore and strengthen health of children. Based on the analysis, we stated the areas of solving these problems. They may include the development and implementation of specific management tools to preserve children’s health potential.
Health, child population, institutes of healthcare, children's health, medical services
Короткий адрес: https://sciup.org/147234731
IDR: 147234731 | УДК: 613.95+614.2 | DOI: 10.15838/esc.2021.2.74.8
Текст научной статьи Preserving children's health: search for the ways of solving relevant issues
Health is a basic component of population’s human potential [1, p. 96]. It is considered the main component of the child population’s well-being [2; 3; 4]. Individually, the state of health in childhood determines subsequent stages of human development. Qualities acquired by an individual at that time, including the basics of healthpreservation behavior [5], are kept throughout life [6, p. 94]. Along with a family, education, and child healthcare play an important role in protecting health of younger generation. Considering the priority of investments in human potential, the topic of children’s well-being has been actively developed in foreign studies. This is a broad concept, the content of which remains the subject of scientific discussions [7]. Indicators of well-being (as applied to a child) include assessments of physical health, development and safety, psychological and emotional development, social development and behavior, cognitive development, and educational achievement [8]. As a case study of European countries shows, the GDP indicator explains less than half (47%) of the Child Well-Being Index variations. In order to assess the relationship between economic development and investment in the well-being of children, it is also necessary to take into account, in addition to economic parameters, social norms, institutions or indicators of the socio-political situation in the country [9]. Global research community is focused on a comprehensive study of children’s well-being [10; 11], development of relevant methods for measuring it, allowing for cross-country comparisons [12; 13; 14]. Some progress has been made in the field of children’s opinions about what well-being means for them [15; 16]. Meanwhile, some aspects in this field remain insufficiently developed. For example, there is a lack of longitudinal studies of the impact of child well-being on the academic performance of schoolage children [17].
Child population takes less than 25% in the structure of the current Russian population, which is a consequence of a low birth rate, which is insufficient to ensure simple population’s reproduction [18], and the increase in life expectancy [19; 20]. As of January 1, 2019, a number of children, aged 0–17 years, was about 30.2 million people1. The implementation of an active federal and regional socio-demographic policy contributed to an increase in the birth rate [21; 22], which was observed until 2016 [23]. Thanks to these measures, the increase in the number of children in 2009–2019 amounted to 16 p.p. Maximum values of the indicator appeared in 2012–2015, and then it began to decline. Researchers attribute this trend to the “demographic waves” effect [24; 25] and to the postponement of births due to the 2015–2016 economic crisis [26]. To overcome the demographic crisis, additional measures of state support are needed, aimed at stimulating high-priority births [27]. The implementation of such a policy should be accompanied by further improvement of the health system, including measures to reduce infant and child mortality rates [21].
On the background of a decrease in the share of children among population, the picture that characterizes their physical well-being – health – is adverse. According to Russian studies, the health potential of children decreases as they grow older [28–32]. Considering these trends, more attention is paid to activities of institutions involved in preserving health of the younger generation: health, education, family, and social protection.
Healthcare is a specialized institution in this list, creation of favorable infrastructure conditions for the prevention of violations of children’s health, its restoration, and preservation depend on its activities. One of the priorities of such specialists is the solution of problems of preventive medicine: in particular, work with population to increase their commitment to a healthy lifestyle and organization of regular preventive checkups and medical examinations2. Among other priorities, experts mention health of adolescents, reduction of disabilities, improvement of medical rehabilitation, optimization of a system of medical and social care for children [33].
Improvement of the child health care and increase of its accessibility are priorities of the WHO Global Strategy for Women’s, Children’s and Adolescent’s Health3. In the Russian state social policy, ensuring the availability of high-quality child health services is also a priority. This is shown in the federal project “Development of child health care, including the creation of a modern infrastructure for providing medical care to children” 4, in the National Strategy for Action on Children for 2012– 20175, and in the action plan for 2018–2020 during the Decade of Childhood (2018–2027)6.
Russian researchers have repeatedly discussed the best organization of the system of continuous monitoring and protection of children’s health. Thus, specialists of the Research Center for Children’s Health of the Russian Academy of Medical Sciences (A.A. Baranov et al., 2008) mentioned a necessity to develop a national classification of avoidable health losses among child population to determine priority goals and objectives in its protection. As an example, the researchers cite the European Classification of Preventable Deaths, based on three levels of prevention. The first level primarily covers factors of conditions and lifestyle of population, the second one – timely detection and early diagnosis of diseases, the third one – adequate treatment and organization of high-quality medical care for patients. The authors call disability an important indicator of health among child population, pointing out that the rehabilitation potential of a family plays a significant role in preventing its aggravation among sick children [34]. In later works, the idea of preventable health losses of child population was revealed in more detail [35]. As part of its approbation, measures to prevent risk factors for the development of mental disorders among children are proposed. This was based on the guidelines of the European Strategy for Child and Adolescent Health and Development (2005), one of which is all stages of the life cycle approach . Its meaning is that “strategies and programs should be focused on solving problems related to child health at each development stage: from a prenatal period to adolescence, according to the most vulnerable age groups and risk factors associated with the economic situation in a region” [36].
The need for joint efforts of a family, education, and medicine in the preservation of child health throughout an entire growing up period was also pointed out by other domestic authors. Specialists of the Ministry of Health of the Republic of Tatarstan revealed a positive regional experience of the work of health centers for children in terms of increasing medical activity of families, improving interest in an independent healthcare of adolescents. The priority of expanding the interaction of specialists of these centers with educational organizations in the region to improve the effectiveness of preventive work was noted. An important result of this cooperation was the implementation of a special screening among schoolchildren. As a result, risk factors for the development of myopia were identified among 72% of students. Most of them were high school students with signs of Internet addiction (who spend a lot of time using social networks, playing videogames, and other entertainment) [37]. According to research data, the procedure for conducting preventive examinations of child population requires significant improvement. So, using a case-study of the Sverdlovsk Oblast, it was shown that a lack of narrowly focused specialists in first-level healthcare organizations leads to a noticeable decrease in the quality of preventive examinations. On the background of a high level of pathologies spread among child population, a number of medical recommendations, issued to children with identified health and physical development disorders, is insufficient. There is an inconsistency in the definition of the health group of schoolchildren and the group for physical education, as well as the problem of poor-quality informing of children’s parents about examinations results. In some cases, parents themselves do not comply with issued medical prescriptions for their children’s treatment [38].
A significant decrease in children’s health occurs during the school period. Based on a nine-year clinical observation of health of 426 Moscow schoolchildren, the researchers proved a necessity for a number of health-preserving measures in educational organizations: improvement of the quality of children’s nutrition in canteens, teaching children and their parents the rules of healthy eating, annual in-depth examination of obese schoolchildren by an endocrinologist, dispensary observation by an allergist and otolaryngologist of schoolchildren with allergic respiratory diseases. Throughout all the years of studying in educational institutions, it is recommended to conduct therapeutic and correctional work with students who have disorders of the musculoskeletal system. In relation to children with neurotic and asthenic reactions, it is advisable to conduct psychological correction and optimization of educational and emotional load in 1–2nd, 7–8th, and, in particular, in 9th grades in preparation for GIA (State Final Examination) [39].
An overview of healthcare policy documents and the works of domestic specialists suggest that, despite a high interest of the government and society in ensuring the reproduction of healthy generations, the following problems are still relevant for Russia:
-
1) decrease in the share of children among population;
-
2) low child health potential;
-
3) insufficient coordination of activities in healthcare, education and family institutions for the protection and promotion of child health.
With this in mind, the purpose of this study was formulated: it is an analysis of child population’s health status and assessment of individual institutional factors of its formation. The study period covered 2005–2019, which is substantiated by a need to study a current state of the problem and trends over the last 15 years (the period of popularization of the country’s socio-demographic policy).
Research methodology
The study was based on quantitative and qualitative sociological and medical-sociological methods.
-
1) Sociological survey of families with children aged 3–17 years , conducted in 2018 in the Vologda Oblast among 1,500 families in Vologda and
Cherepovets and 8 municipal districts of the Oblast. The sample is representative; the sampling error did not exceed 3% with a confidence interval of 4–5%. The survey used four types of questionnaires, depending on a child’s age: for parents of preschool children (3–6 years), younger (7–10 years), middle (11–14 years), and senior school (15–17 years) ages.
-
2) Prospective monitoring of cohorts of families with children. Since 1995, the Vologda Research Center of RAS has been conducting a medical and sociological monitoring study “Studying the conditions for the formation of a healthy generation”. The sample consists of families with children born during a certain period. The health of children is monitored until they reach the age of 18. The study involves large towns of the region (Vologda, Cherepovets), towns-district centers (Veliky Ustyug, Kirillov), and Vozhega – an urban-type settlement. During the period of longitudinal observation, five cohorts of families with children born in 1995, 1998, 2001 and 2004, 2014 were examined7. In 2020, a new cohort of participants was recruited.
-
3) Focus group studies of parents with children aged 3–17 years . In 2019, 5 focus groups were taken into account: 3 in Vologda, 1 in Cherepovets, and 1 in the Oblast’s municipal region. 36 people were examined, different in age, presence and age of children, level of education, marital status. An idea of real problems of families with children in the region was obtained, the expectations of parents regarding their solutions (including children’s health sphere) were revealed.
-
4) Expert survey of specialists of the regional healthcare system, representatives of the authorities responsible for the protection of children’s health. In 2019, 10 expert interviews were conducted with
specialists whose activities include work with families and children. The experts outlined their vision of possible ways to increase the potential of children’s health.
The rich empirical base of the study, collected through a combination of qualitative and quantitative methods, allows us to give a comprehensive assessment of a current situation in the field of children’s health and healthcare, as well as to formulate directions for solving problems related to the preservation of child health, taking into account opinions of parents, medical professionals, and government representatives.
Research results
Child health status
Despite notable healthcare achievements in the Russian Federation, which have reduced infant mortality by 55%, from 11.0 cases per 1,000 live births in 2005 to 4.9 per 1,000 live births in 20198, it is too early to talk about improving child health in general. The primary morbidity rate of children aged 0–14 years increased by 2% over 13 years (from 1708.78 cases per 1000 children aged 0–14 years in 2005 to 1746.94 cases in 20189). The incidence of adolescents increased by 22% (from 1114.52 cases in 2005 to 1360.20 cases in 201810).
There were also significant changes in the structure of primary morbidity among children aged 0–14 years in 2005–2018. Unfavorable trends include a slight increase in the spread of eye diseases (by 2% – from 5,577 to 5,700), injuries and consequences of external influences (by 3% – from 10,352 to 10,618 cases per 100 thousand people), and a significant increase in the incidence of malignant neoplasms (by 38% – from 341 to 469 cases per 100 thousand people), obesity (by 47% – from 256 to 375), diabetes mellitus (by 65% – from 13 to 21)11. The number of children aged 0–14 years with malignant neoplasms has increased by 71% over 10 years (from 2008 to 2018), and the number of adolescents with such diagnoses has increased by 37% over the same period12 [40].
A high level of morbidity among Russian child population in 2005–2018 was followed by an increase in its chronicity for certain classes of causes [41], as well as an increase in the detection of congenital pathologies [42]. In 2015–2018, the share of children aged 0–14 years with chronic diseases remained high and basically unchanged – nearly 15%. Among children under one year of age, this figure was slightly lower – about 8%13.
Relevant issues of health among child population also include high child disability14 [43]. During the specified period, absolute and relative disability indices among Russian child population increased by 1.2 times and 1.08 times, respectively. In 2019, these values were 670 thousand people and 222 people per 1000 children, respectively15.
These problems are actualized by studies aimed at identifying factors that preserve health of child population and searching for its management tools.
The solution of these problems can be practically used in the area of improving the coordination of the work of the institutes of health, education, and family in the field of protecting and promoting health of child population.
Data of the cohort monitoring allows not only tracking current health parameters of child population in the region (cross-sections of data), but also getting a picture of their changes over time for the same participants (longitudinal cross-sections of data). During this prospective observation, a number of patterns were identified that characterize health of the participants. In the development of children, critical ages are identified, which account for maximum “declines” of health. These are the periods of the first year of life, 6–7 years (entry into primary school), and 9–10 years (transition to secondary school, when the decline of health is determined by the increase in study load) [5]. At the previous stages of the study, the age-specific factors of children’s health formation were shown. Thus, it was revealed that the combination of biomedical and social factors most significantly affects newborns [44]. Behavioral factors are beginning to play a significant role in shaping health of school-age children. In particular, the lack of formation of health-preserving skills among children has a negative impact. For example, according to responses of parents in 2019, 40% of 15-year-olds did not adhere to a correct sitting at the desk when writing and reading, 49% – to a work regime at a computer (they did not take necessary breaks for the prevention of visual impairment). At the same time, visual disturbances, involving the wearing of glasses or contact lenses, were detected among 32% of adolescents, but 13% of them did not use glasses, despite a doctor’s recommendations.
Unfavorable factors in the formation of health of younger generation also include the lack of awareness of parents about the health status of their children . This is evidenced by the discrepancy between parental assessments of children’s
Figure 1. Distribution of parental health assessments in the cohort of children born in 2004 (% of a number of respondents in a corresponding year) and the share of children with the first health group according to pediatricians’ assessments (% of a number of children in the cohort)
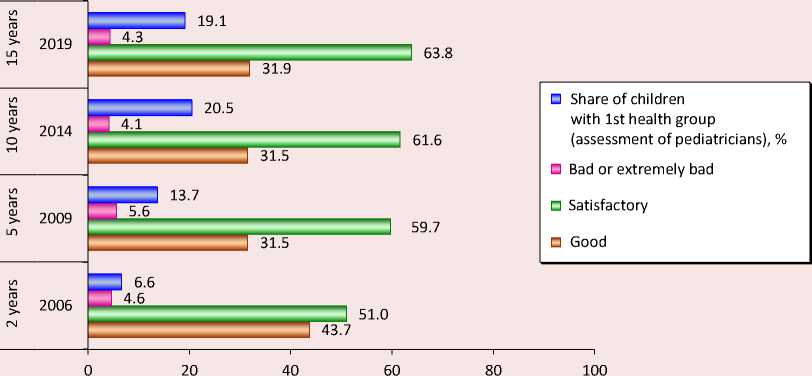
Source: cohort monitoring data “Studying the conditions for the formation of a healthy generation”, 2006–2019.
health and those made by pediatricians, observed throughout the study period. Thus, in 2019, 32% of parents of children born in 2004 described their child’s health as “good”, while, according to pediatricians, only 19% of children in this cohort were completely healthy (Fig. 1) . Among most children whose health was considered good by their parents, pediatricians noted either frequent infectious diseases during the year, or functional and morphofunctional disorders, which corresponds to the health group II. For children whose health was described as satisfactory by their parents, pediatricians’ assessments were also divided: most of the children did have the health group II, while 20% had no health disorders, and another 20% had chronic diseases (which corresponds to the health group III). Only two children had parents who reported poor health (one child actually had chronic diseases).
Inconsistency of the health assessment by medical professionals and parents, revealed in the monitoring, is also confirmed by other data. Thus, according to the results of a sociological study of the health of schoolchildren in Vologda and Cherepovets16, 43% of families rated health of their children as very good, while in fact (according to school medical offices) the share of completely healthy children was only 11.5%. The health assessments of 11th grade students differed the most: 35% of parents considered their children’s health as very good, and only 1% of them actually were like this according to medical records. The most common diseases among schoolchildren at the end of high school (grade 11) were diseases of the musculoskeletal system (60% of children), cardiovascular system (37%), visual organs (34%), nervous system (33%), respiratory system (15%), and digestive system (14% of children).
The reasons for the discrepancy between parental and medical assessments of the current state of children’s health are the lack of appropriate competencies and lack of awareness among parents. On the other hand, when assessing child health, parents look at whether it allows him to socialize normally. If there are no complaints from a child and serious functioning limitations, then health is assessed as “good”. Based on available information, understanding the degree of its importance, awareness of the responsibility of a family for preserving children’s health, appropriate behavioral practices of health conservation are formed. It can be assumed that inaccurate information of parents and incorrect behaviors can be among possible reasons for the chronization of untreated diseases among children as they grow up. Medical professionals are more accurate in their assessments, as they are guided by the presence or absence of diseases and developmental disorders, so it is very important to establish information interaction between medical professionals and families using modern capabilities and information transmission channels.
According to the monitoring data, the majority of parents of 15-year-olds (72%) considered themselves sufficiently informed about their child’s health. The main sources of information for the respondents were conversations with a child’s attending physician and nurse (this option was selected by 87 and 21% of respondents, respectively), as well as the mass media (26%; Tab. 1 ).
Full awareness of parents, being the most important prerequisite for an objective assessment of health, is not yet a sufficient condition for its preservation and strengthening. Medical activity
Table 1. Distribution of parents’ responses to the question “What is your primary source for receiving information about health and organization of care for your child?” (2019, case study of a cohort of families with children born in 2004)
|
Response |
Share of respondents who chose this response option, % |
|
Doctor |
87.2 |
|
Television, radio, Internet |
25.5 |
|
Nurse |
21.3 |
|
Literature |
6.4 |
|
Child’s medical record |
6.4 |
|
Relatives, friends, acquaintances |
6.4 |
|
Other |
2.1 |
|
Source: cohort monitoring data “Studying the conditions for the formation of a healthy generation”, 2019. |
|
of a family and disciplined adherence to doctor’s recommendations play a major role in this regard. A common mistake of parents is a refusal to timely consult a doctor in case of a child’s acute illness. According to the cohort monitoring, in 2019, nearly 23% of teenagers’ parents did so. Another problem is a failure to fulfill prescriptions of a treating doctor. In 2019, 15% of teenagers’ parents revealed that they do not always strictly obey doctor’s recommendations and follow a prescribed course for treatment or improvement of a child.
Considering the aforementioned health problems of the younger generation, it is particularly important to strengthen information and educational work with parents in the system of medical prevention. At the same time, the issues of quality and accessibility of health services for families with children come to the fore.
Issues and factors of the child health formation
When discussing medical activity of families, it is important to consider the aspects of the availability of medical care, convenience of receiving it, which mostly limit receipt of high-quality and timely medical care. Based on the results of a sociological survey of families with children in the Vologda Oblast conducted in 2018, it was revealed that, when applying for medical care in state institutions, parents with children most often noted the presence of such problems as the lack of necessary specialists (30% of respondents), queues (30%), and an inconvenient schedule for specialists’ appointments (24%).
The lack of qualified medical personnel, especially narrowly focused specialists, is noticeable across the whole country, which is confirmed by medical statistics. In Russia, the number of child pediatricians decreases and the ratio of part-time work in this specialty increases [45].
In several regions of the Northwestern Federal District in 2005–2018, there was a decrease in the number of registered pediatricians17. As of 2018, in the federal district as a whole, there were 9.75
Table 2. Availability of doctors of various specialties, per 10,000 children, the Vologda Oblast
Specialty 2017 2018 For reference: standard for polyclinics per 10,000 children (2018) Pediatric cardiologist 0.40 0.44 0.5 Pediatric oncologist 0.04 0.04 0.1 Precinct pediatrician 8.33 8.17 12.5 Pediatric psychiatrist 0.37 0.42 – Adolescent psychiatrist 0.00 0.00 – Pediatric dentist 0.84 0.84 – Urologist-andrologist for children 0.04 0.04 1 Pediatric surgeon 0.88 0.84 1 Pediatric endocrinologist 0.40 0.40 0.5 Source: Resources and activities of healthcare organizations. Medical Employees: Stat. Coll. Department of Health Monitoring, Analysis, and Strategic Development of the Ministry of Health of the Russian Federation, Federal Research Institute for Health Organization and Informatics of Ministry of Health of the Russian Federation. Ministry of Health of the Russian Federation. Moscow, 2019. 281 p.; On approval of the regulations on the organization of primary health care for children: Order of the Ministry of Health of the Russian Federation no. 92n, dated March 7, 2018. Available at:
district pediatricians per 10,000 children, while in the Vologda Region – 8. To compare, in accordance with the order of the Ministry of Health, which was in effect in 2018, a recommended staff standard for providing child polyclinics with precinct pediatricians was 12.5 units per 10,000 attached children18. Therefore, it is possible to talk about the shortage of such doctors in the region and the district. Among medical specialists, the best provision of child population in the Vologda Oblast is with surgeons and dentists, the worst – with adolescent psychiatrists (who are absent in the region), pediatric oncologists, and urologists-andrologists (Tab. 2) .
All parents are concerned with the lack of medical personnel and queues, while worries about inability to get an appointment at the right time, lack of free medicines, and poor organization of registration offices is more pronounced among parents of preschool children (27, 23, and 13%, respectively).
Issues related to the quality of medical staff are less relevant. 6.5% of parents of preschool children, 5.4% of parents of primary school children and 8% of parents of middle and high school age children reported systematic disrespect in medical institutions. The problem of tardiness and irregular breaks in the work of medical staff was most often mentioned by parents of children aged 11–14 years (9.2%; Tab. 3 ).
In case of private medical organizations, the listed problems barely bothered parents. However, an in-depth study, conducted earlier, revealed a contradiction: despite existing problems of state medical institutions, according to parents, efficiency of services is higher in these places. Moreover, most services are free, and it is very important for families with children [46].
The results of the mass survey were confirmed during a focus group study . Among the key medical care problems for families with children, parents most often mentioned the lack of narrowly focused specialists in children’s clinics, inability to make an appointment and individual procedures (for example, ultrasound). The discussion also raised the issue of a low availability of free medical services
Table 3. Issues that arise in families with children when seeking medical care (according to a sociological survey, 2018)*
|
Issues |
Share of respondents who reported a persistent nature of the issue, % |
|||
|
Parents of 3–6 years old children |
Parents of 7–10 years old schoolchildren |
Parents of 11–14 years old schoolchildren |
Parents of 15–17 years old schoolchildren |
|
|
Lack of necessary specialists |
30.8 |
27.4 |
30.7 |
30.0 |
|
Queues |
31.2 |
29.6 |
29.1 |
30.5 |
|
Inconvenient schedule for specialists’ appointments |
27.3 |
20.1 |
25.9 |
23.7 |
|
Lack of free medicines |
22.7 |
19.3 |
21.5 |
20.7 |
|
Poor organization of registry offices |
12.6 |
8.2 |
8.4 |
10.8 |
|
Tardiness, irregular breaks in the work of medical staff |
7.9 |
6.2 |
9.2 |
7.4 |
|
The need to pay for medical services that should be free |
18.2 |
13.1 |
18.5 |
18.2 |
|
Lack of information about work of specialists and who you can contact in case of certain diseases |
14.8 |
12.6 |
14.7 |
14.9 |
|
Inattentive attitude of medical workers |
12.7 |
10.3 |
13.9 |
11.7 |
|
Rudeness, disrespectful attitude of medical workers to patient |
6.5 |
5.4 |
8.9 |
8.3 |
* Distribution of respondents’ answers to the question “What problems, related to your child’s health care, do you face in public healthcare institutions?”
Source: results of a mass survey of parents of children aged 3–17, 2018.
– Lack of specialists. They are impossible to find. First, an epidemic occurs: you do not go to a clinic, because you do not want to infect a child. Then doctors themselves are on sick leave or on vacation (fem., Vologda, 36, married, 1 child, higher ed., employed).
– It is problematic to make an appointment for ultrasound even three months in advance. It happens sometimes. Maybe the clinic is quarantined, which is why schedule shifts. Parents also have an option – to go to a private clinic, but money is sometimes an issue. We once took the child to a hematologist, and he says: “Why did you come for payment? You could sign up in three days”. And we had to register him for rehabilitation, some comments were given about his blood test. Until the specialist approves... So I had to go for a fee (male., Vologda, 49, married, 3 children, higher ed., retired).
– There is a shortage of specialists here and in Vologda. When do they have checkups? In spring? Coupons are given, then it is all lost by fall, in summer you cannot get to a specialist at all, only for a fee. But for a fee, you know, not everyone can… I have a surdologist assigned to my child. We have 2 surdologists: both are paid ones. (fem., Cherepovets, 43, not married, 2 children, higher ed., employed).
– We need to visit an allergist. There is only one allergist in the town. I do not know how to get to him?! “Go to him for a paid appointment for 700 rubles”. I have three children. I have to pay 2100 for three of them, and then what? (fem., Vologda, 32, married, 3 children, higher ed., employed).
– The orthopedist works every other day. When he does not work, he is in another clinic. Well, it happens all the time... you go to a paid appointment – you snatch money from the family. While there is free medicine (male., Vologda, 39, married, 2 children, higher ed., employed).
– I have a situation. The child is 8 years old. We were sent to a surgeon, because of an umbilical hernia. There was no specialist in the clinic, I came to the clinic three times before 8 am. When there was the specialist, there were no coupons. I thought that it was not so terrible – an umbilical hernia, so we just did not go to either paid or free doctor (fem., Cherepovets, 32, not married, 3 children, higher ed., employed).
– For children, we would like medical services to be “more free”. This is our society. Medicines are very expensive. Even in villages: if someone had a serious disease, others donated ( for reference – to cure a child) . After all, this problem can be solved by the government (male, municipality, 46, non-official marriage, 3 children, full secondary education).
– The nurse is always absent (for reference – in the kindergarten). She currently comes and leaves... When it is necessary, they come – like for vaccinations … In Soviet times, a nurse went around and checked health of children. If someone had signs ( for reference – of diseases), then they were withdrawn. And now no one does this, children are brought, and that is all. A teacher cannot examine 30 people. A teacher is not a doctor. Maybe a child had a lack of sleep. A disease may be invisible. A teacher and a parent may miss some signs. I speak of my child’s experience. I can tell the difference only when he has a 40-degree temperature. There is no medical worker, so there is no one to check the group (fem., Vologda, 39, married, 1 child, higher ed., employed).
– The government does not organize the control of admission to kindergartens. A doctor must meet a child when he/she is brought there. But now, until evening, a child with fever sits in the group and does not play. I went through this: they called, I came back in an hour. The child had a fever, and we took a sick leave. We recently had a medical examination and passed only tests, and, for some specialists, we have a problem with vision for example, you get registered, receive a referral, and confirm whether the child can sit at this desk. There are professional checkups of children, but they are superficial. (fem., Vologda, 27, not married, 1 child, sec. sp. ed., employed).
-
– In the kindergarten, there is a medical worker with a medical education. But in some places kids are examined, and in another – they are not. And they are looking at it while it is happening (for reference. – a disease of a children) : 2–3 weeks. They begin the examination, and then everything is fine. (male, Cherepovets, 40, unofficial marriage, 2 children, sec.sp.ed., employed).
-
– One medic for a large kindergarten, 12 groups of 25 people, he is physically unable to examine all of them . (fem., Vologda, 36, married, 1 child, higher ed., employed).
to parents’ unwillingness to initiate the prevention of children’s health disorders, their low medical activity and lack of competence in healthcare issues. This attitude may be a consequence of the fact that, with a lack of their own resources, parents expect support from the government. The objective factor limiting parents’ capability to preserve children’s health is a bad financial situation. Its improvement is a fundamental task of regional economic policy; its solution will reduce the severity of social problems of medicines provision and access of families with children to paid medical services by increasing efficient demand. The appeal to paid medicine keeps the relevance of the potential development of the state health system: it is technically free for population, but, in fact, it is partially funded by the Compulsory Medical Insurance Fund – parents also contribute to it.
Some parents consider social government support a necessary condition for raising their children. Other people strive for taking an independent position: they say that if they had a decent job that would have allowed them to maintain a high standard of living, financial assistance from the government, benefits, allowances, and free medical services would not be critically important for them, since they could purchase all the necessary benefits themselves. Their only expectation from the government in this area would be the construction and maintenance of child infrastructure (sports fields, bike paths, stadiums, etc.).
In general, conducted sociological studies allow identifying three most relevant issues in the area of child health protection: insufficient awareness of parents and teachers about an actual state of children’s health, the increase in the number of children with chronic diseases during school education, and the lack of a coordinated work system in educational organizations and among the parent community.
As for my family, I need nothing from the government. If only they would build bike paths. Infrastructure. If they had provided parents with an opportunity to work and earn money. I would do everything myself. Buy the books and everything else... Let me earn money, and that would be it! It is not necessary to introduce benefits for large families – it seems a humiliation! Give a man a job, so his wife could take care of three children, and they both could avoid unnecessary headaches caused by questions like “what to eat and wear, how to solve household issues and move into a bigger apartment”. If he can find a job, then he can buy everything himself (male, Vologda, 30–39, married, 2 children, higher ed., employed).
Experts’ evaluations usually coincide with findings of mass surveys and focus groups. Experts unanimously classified the problem of reduced potential of children’s health in the growing up process as strategically important. According to data provided during the interview on the results of professional checkups and medical examinations of child population, the number of children with chronic diseases increases every year. Individually, physical, mental, and reproductive health of children deteriorates with age. Experts say that one of the main factors of these problems is the lack of information on child health issues among parents, and their incompetence in cultivating health-preserving skills among children . Moreover, experts confirmed that, as a child grows up, parents become less concerned about his/her health. Maximum attention is paid to children’s health in infancy, preschool and primary school age: it is when parents have an interest and time, and medical workers constantly supervise a child. In addition, during this period, the interaction of parents with medical specialists is closely established (through the work of foster nurses, district pediatricians). Besides, parents establish a close interaction with medical specialists in this period (through the work of foster nurses and district pediatricians).
The interaction between parents, children, and medical workers starts to gradually weaken in a middle school. Insufficient medical activity of parents intersects with one of the key healthcare personnel issues – the lack of permanently employed medical workers in educational organizations. Each educational organization has an attached medical worker, who frequently organizes examinations and vaccinations of children. However, according to experts, the problem is the absence of these specialists among an organization’s staff. The reasons are uncertain. A primary explanation is an unfavorable position of medical workers under the jurisdiction of the education system, compared to those who work in the healthcare sphere – it is about the qualification and financial losses. Medical workers were removed from kindergartens and schools, because they had lower wages and benefits in case of being among an educational organization’s staff. In addition, a general shortage of medical personnel contributes to the solution of the issue.
Experts have various explanations for the lack of narrowly focused specialists in child medical institutions: some think that the problem is being solved, and others still regard it as the most relevant and unresolved issue. The current mechanism for training medical students in targeted areas is being approved. It allows returning qualified specialists to the region despite the absence of a medical university in the Vologda Oblast. Experts believe that the reasons for the current personnel shortage are the demographic crisis of the 1990s, which led to a numerical reduction of applicants to medical universities and, as a result, future specialists. There also was the discretization of the medical profession that led to a massive outflow of employees from the healthcare sector.
The health problems, the perception of which is radically different in the parent and medical community, were the issues of a low availability of free medical services, a high cost of medicines, and quality of professional examinations among children . Parents criticized educational organizations and the healthcare system, and the experts, on the contrary, pointed out the lack of competence among parents in the prevention of children’s morbidity.
Experts emphasize that medical examinations of children are screening checkups aimed at timely detection of any violations or pathologies, and therefore they are fast. If deviations from the norm are detected, parents are informed of the need for more detailed consultation with required specialists and treatment. Thus, the problem is that parents barely understand the content and purpose of a professional examination and partially transfer their responsibilities to maintain children’s health to medical professionals. Data confirms this statement: at the end of 2018, reproductive pathologies and abnormalities were identified among more than 4,000 children during professional examinations of girls aged 0–18 years. Only 1,000 of them were registered and received treatment. The purpose of preventive examinations is to identify a violation, contact a family, undergo a treatment, and bring a child to the “healthy” group. Failure to comply with this algorithm subsequently leads to an aggravation of health. The most common reason for the violation of this “ideal formula”, according to experts, is that medical professionals and schools fail to adequately inform parents about the results of professional examinations due to the lack of time and personnel . Parents, in turn, often “blindly”
trust doctors and believe that examinations lead to improvement or preservation of health. Thus, they do not take any actions and, unwillingly, become the culprits of the formation of children’s chronic pathologies.
Experts’ opinions on a poor availability of free medical services and high costs of medicines were somewhat divided. Some of them call the underfunding of insurance medicine and, as a result, an inadequate system of tariffs, namely their over reduced sizes , the main reasons for this situation. Other experts believe that it is incorrect to talk about unavailability of medicines, since there is a supply, and it is conducted for federal and regional categories of aided people. Specialists recognize that certain medicines may not be included in this list, but if a patient needs them, applications are made at requests. Considering unavailability of free medical services, some experts skeptically noted that the provision of assistance is regulated by a list of state guarantees, but if a certain procedure is still not available for a patient, the problem is solved by, for example, concluding contracts with third-party organizations. Meanwhile, they point out that currently functioning recording methods, including remote ones, effectively solve the problem of difficulties in making appointments with specialists.
Discussion of the results
Preservation and promotion of children’s health implies a well-coordinated and purposeful work of family, health, and education institutions. Each one experienced significant transformations that had an impact, sometimes negative, on younger generations’ health during the post-Soviet period. Currently, the main task is to coordinate activities of these institutions, focusing on priorities – wellbeing of child population, creation of conditions for the best development and implementation of its human potential.
Obviously, within the state social policy, there are attempts to ensure a proper functioning of healthcare and education spheres, and to improve social and financial situation of families with children, but so far it has been insufficient. Construction of perinatal centers, implementation of an active policy in the area of developing resource potential of healthcare, especially in pregnancy and childbirth fields, monitoring and medical services for children in the first year of life have made it possible to achieve significant success in reducing infant and maternal mortality, detecting hereditary diseases and congenital developmental pathologies. These achievements serve as motivation for further steps toward improving children’s healthcare. The issues of improving the health of newborns remain on the agenda. To solve them, it is important to conduct competent and more active work with population of reproductive age. As one of the areas of such activity, we can suggest expanding the practice of preparing future parents for child conception and pregnancy by, for example, sending them to family, health, and reproduction centers (or other similar organizations), where future parents could undergo a comprehensive health examination, receive advice from medical specialists, and psychological support.
The solution of personnel issues in the regional healthcare system is among the priority tasks of the Vologda Oblast. According to the regional target program “Development of healthcare in the Vologda Oblast for 2021–2025”, it is planned to allocate 1 398 555.8 thousand rubles for the development of the personnel potential of the industry19. Unfortunately, among the indicators of the state program, there is no indicator of the provision of children with pediatricians and specialists. Given the observed shortage of these doctors in the region, it is necessary to monitor these indicators.
Development of human resources and issues of ensuring a regular presence of a medical worker in an educational organization are the most important prerequisites for building a successful regional healthcare system for children. Within the framework of federal and regional programs for developing the industry, tools and financial support are provided for the training of specialists in the child health area. For medical personnel employed in educational organizations, there are currently no such management resources. Experts see specific solution to this problem in maintaining all the privileges for the medical staff of kindergartens and schools in terms of remuneration, pension savings, and benefits , provided that the conditions for licensing medical offices are simplified and they are assigned to the healthcare system to preserve medical experience and salaries, in accordance with the roadmap for paying medical workers. Alternatively, it is possible to focus on the experience of licensing a medical office in universities that use it on the rights of operational management , i.e. the office is in federal ownership, and an university is engaged in its maintenance (repair, purchase of equipment). On a contractual basis, medical employees work among the staff of a medical organization, and, as a result, all benefits are preserved for them.
Meanwhile, the presence of medical workers in educational institutions and a regular entrance monitoring of children’s health do not yet serve as an absolute guarantee of health safety during pedagogical and educational process. A countereffort from parents and teachers is also required. In particular, it seems appropriate to conduct explanatory conversations with parents about not bringing children with symptoms of an infectious disease to a kindergarten group and not sending them to school. Undoubtedly, in reality, parents often find themselves in a difficult situation when they do not receive understanding of an employer. Therefore, they are forced to choose between caring for a sick child and performing official duties. The inclusion of additional guarantees for working parents with young children in the Labor Code can prevent the occurrence of such dilemmas. For example, expansion of an opportunity for parents of young children to have a flexible work schedule or remote employment format (if nature of work allows it), at least for the period of a child’s illness. Such forms of work are very popular, especially among single parents who cannot rely on help of family members in caring for children.
We should not forget about the organization of the health-saving environment within an educational organization. As previously mentioned, significant losses of child health occur during their schooling. It is the school educational process that places increased demands on the endurance of a child’s body, its ability to resist stress and adapt to changing social conditions. Teachers need to provide all possible support to children, combining their efforts within a team, as well as involving parents and school healthcare workers. The solution of this problem requires not only the development of school health-saving programs, but also the introduction of a specialist (for example, a head teacher of health-saving) responsible for the quality and effectiveness of health-saving activities and its organization. Priorities of the school healthcare system should include improvement of notification of parents about the results of professional examinations, increase of interest among parents to not only obtain this information, but also to conduct, if necessary, additional examinations and follow recommendations of medical professionals, instilling health-saving skills in a family.
To develop inter-institutional cooperation in the field of healthcare, it is important to regularly exchange information, and its forms can be diverse – from thematic meetings and “round tables” to special NPOs projects on children’s health issues involving parents, medical and educational organizations, social protection agencies, representatives of public organizations, and the scientific community.
Conclusion
The study, conducted using comprehensive methodological tools, revealed several personnel, organizational, and material issues in the field of preserving and strengthening child population’s health. The key one is the problem of weak interaction between families, education, and healthcare. Each institute is simultaneously an object of state social policy, which makes it possible to adjust their current state and conditions of functioning. Thus, the focus group study showed the importance of an integrated approach to solving the problems of access to quality medical services for families with children. The authors proved that the improvement of the financial situation of families is no less important for the preservation of children’s health than the development of infrastructure and human resources of the state health system. It is shown that opinions of parent and specialists, engaged in healthcare, significantly differ on a number of aspects. This actualizes the work on building a dialogue between them. The role of educational organizations in the system of preserving and promoting children’s health can be called “coordinating”, since they represent a primary environment for the socialization of children aged 3–18 years.
In general, the coherence of the identified problems led to the development and justification of a list of actions to overcome them that takes into account different aspects of child health and integrates efforts of several social institutions (family, healthcare, education). The practical significance of proposed actions is an opportunity to implement them with minimal costs by integration into existing work algorithms of healthcare and education specialists. They can also be a basis for development and implementation of new management tools for preserving the health potential among children. In the future, it is planned to study the reasons for a weak interaction of institutions, involved in the preservation of child health, more deeply.
Список литературы Preserving children's health: search for the ways of solving relevant issues
- Rimashevskaya N.M., Rusanova N.E. Health of the Russian population in the context of socio-economic modernization. Narodonaselenie=Population, 2015, no. 4 (70), pp. 96–105 (in Russian).
- Bradshaw J., Hoelscher P., Richardson D. An Index of child well-being in the European Union. Social Indicators Research, 2007, vol. 80, pp. 133–177. DOI: 10.1007/s11205-006-9024-z
- Richardson D., Hoelscher P., Bradshaw J. Child well-being in Central and Eastern European Countries (CEE) and the Commonwealth of Independent States (CIS). Child Indicators Research, 2008, vol. 1, pp. 211–250. DOI: 10.1007/s12187-008-9020-8
- Ben-Arieh A. Indicators of children’s well-being: What should be measured and why? Social Indicator Research, 2007, vol. 84, pp. 249–250.
- Shabunova A.A., Morev M.V., Kondakova N.A. Zdorov’e detei: itogi pyat-nadtsatiletnego monitoringa: monografiya [Children’s health: Results of fifteen years of monitoring: Monograph]. Vologda: ISEDT RAS, 2012. 262 p.
- Obrazhei N.V. Social infrastructure of childhood as important direction of social policy in the field of children health protection. Sotsiologicheskii al’manakh=Sociological Almanac, 2016, no. 7, pp. 93–100.
- Amerijckx G., Humblet P.C. Child well-being: What does it mean? Children & Society, 2013. DOI: 10.1111/chso.12003
- What is Child Well-Being?: Does It Matter How We Measure It? National Council on Family Relations Annual Conference, San Antonio, Texas (November 7, 2013). Available at: https://www.childtrends.org/wp-content/uploads/2013/12/2013-57ChildWBMeasureIt1.pdf
- Bradshaw J., Richardson D. An Index of Child Well-Being in Europe. Child Indicators Research, 2009, vol. 2 (3), pp. 319–351.
- Hernandez D.J., Napierala J.S. Disparities in U.S. Parental employment insecurity and child well-being across income groups: before, during, and after the great recession. Child Indicators Research, 2020, vol. 13, pp. 741–775. Available at: https://doi.org/10.1007/s12187-019-09713-8
- Bass L.E. Social focus on health and children’s well-being. Sociological Inquiry, 2011, vol. 81 (4), pp. 495–498.
- Fernandes L., Mendes A., Teixeira A.A.C. A review essay on the measurement of child wellbeing. Social Indicators Research, 2012, vol. 106 (2), pp. 239–257.
- Buck K.D., Summers J.K., Smith L.M. et al. Application of the human well-being index to sensitive population divisions: A Children’s Well-Being Index development. Child Indicators Research, 2018, vol. 11, pp. 1249–1280. Available at: https://doi.org/10.1007/s12187-017-9469-4
- Rees G. The association of childhood factors with children’s subjective well-being and emotional and behavioural difficulties at 11 years old. Child Indicators Research, 2018, vol. 11, pp. 1107–1129. Available at: https://doi.org/10.1007/s12187-017-9479-2
- Vujčić M.T., Brajša-Žganec A., Franc R. Children and young peoples’ views on well-being: A qualitative study. Child Indicators Research, 2019, vol. 12, pp. 791–819. Available at: https://doi.org/10.1007/s12187-018-9559-y
- Fattore T., Fegter S., Hunner-Kreisel C. Children’s understandings of well-being in global and local contexts: Theoretical and methodological considerations for a multinational qualitative study. Child Indicators Research, 2019, vol. 12, pp. 385–407. Available at: https://doi.org/10.1007/s12187-018-9594-8
- Amholt T.T., Dammeyer J., Carter R. et al. Psychological well-being and academic achievement among schoolaged children: A systematic review. Child Indicators Research, 2020, vol. 13, pp. 1523–1548. Available at: https://doi.org/10.1007/s12187-020-09725-9
- Vishnevskii A.G., Andreev E.M., Shcherbakova E.M. Demographic challenges of Russia. Part one – population and space. Demoskop Weekly=Demoskop Weekly, 2017, no. 749–750, pp. 1–10 (in Russian).
- Kolosnitsyna M.G., Kossova T.V., Sheluntsova M.A. Factors of the life expectancy increase: Country-level cluster analysis. Demograficheskoe obozrenie=Demographic Review, 2019, vol. 6, no. 1, pp. 124–150 (in Russian).
- Rybakovsky O.L., Sudoplatova V.S., Tayunova O.A. The potential for reducing mortality in Russia. Sotsiologicheskie issledovaniya=Sociological Studies, 2017, no. 3, pp. 29–42 (in Russian).
- Zaitseva E.V., Goncharova N.V. Analysis of the influence of pronatalistic policy on reproduction of population and position of large families. Vestnik UrFU. Seriya ekonomika i upravlenie=Bulletin of Ural Federal University Series Economics and Management, 2019, vol. 18, no. 6, pp. 967–988. DOI: 10.15826/vestnik.2019.18.6.047 (in Russian).
- Razvarina I.N. Assessment of economic damage caused by child mortality. Vestnik UrFU. Seriya ekonomika I upravlenie=Bulletin of Ural Federal University Series Economics and Management, 2018, vol. 17, no. 4, pp. 620–634 (in Russian).
- Rostovskaya T.K., Kuchmaeva O.V., Bezverbnaya N.A. Current state and prospects of family policy in Russia: Socio-demographic analysis. Ekonomicheskie i sotsial’nye peremeny: fakty, tendentsii, prognoz=Economic
- and Social Changes: Facts, Trends, Forecast, 2019, vol. 12, no. 6, pp. 209–227. DOI: 10.15838/esc.2019.6.66.12 (in Russian).
- Makar S.V., Simagin Yu.A., Yarasheva A.V. Demographic situation in Russia and social infrastructure. Narodonaselenie=Population, 2020, vol. 23, no. 1, pp. 67–75. DOI: 10.19181/population.2020.23.1.6 (in Russian).
- Rybakovsky O.L., Tayunova O.A. Fertility in Russia and demographic waves. Narodonaselenie=Population, 2017, no. 4 (78), pp. 56–66. DOI: 10.26653/1561-7785-2017-4-4 (in Russian).
- Klupt M.A. Influence of family policy and normative beliefs about family on fertility: Comparative analysis. Sotsiologicheskie issledovaniya=Sociological Studies, 2020, no. 3, pp. 40–50. DOI: 10.31857/S013216250008812-6 (in Russian).
- Shcherbakov A.I. Increasing fertility is the main aim of demographic policy in Russia. Sotsial’no-trudovye issledovaniya=Social and Labor Research, 2019, no. 3 (36), pp. 143–152. DOI: 10.34022/2658-3712-2019-36-3-143-152 (in Russian).
- Baranov A.A. et al. Results of preventive medical examinations of minors in the Russian Federation. Rossiiskii pediatricheskii zhurnal=The Russian Pediatric Journal, 2016, no. 19 (5), pp. 287–293 (in Russian).
- Namazova-Baranova L.S. et al. Morbidity of children aged 5 to 15 years in the Russian Federation. Meditsinskii sovet=Medical Council, 2014, no. 1, pp. 6–10 (in Russian).
- Rimashevskaya N.M., Breeva E.B. The “field” of childhood. Narodonaselenie=Population, 2011, no. 4, pp. 17–26 (in Russian).
- Sukhareva L.M., Rapoport I.K., Polenova M.A. The health of the Moscow schoolchildren and the factors that influence its formation (longitudinal study). Zdorov’e naseleniya i sreda obitaniya=Public Health and Life Environment, 2014, no. 3 (252), pp. 28–30 (in Russian).
- Shabunova A.A. Twenty years of children’s health monitoring: Organization, results, conclusions. Ekonomicheskie i sotsial’nye peremeny: fakty, tendentsii, prognoz=Economic and Social Changes: Facts, Trends, Forecast, 2015, no. 2 (38), pp. 116–128. DOI: 10.15838/esc/2015.2.38.7 (in Russian).
- Baranov A.A., Albitskiy V.Yu. State of health of children in Russia, priorities of its preservation and improving. Kazanskii meditsinskii zhurnal=Kazan Medical Journal, 2018, vol. 99, no. 4, pp. 689–705 (in Russian).
- Baranov A.A., Yakovleva T.V., Albitsky V.Yu., Modestov A.A., Antonova E.V. Reduction of avertable loss of health in children – the strategy of social pediatrics. Voprosy sovremennoi pediatrii=Current Pediatrics, 2008, vol. 7, no. 4, pp. 6–8 (in Russian).
- Baranov A.A., Albitsky V.Yu., Terletskaya R.N., Zelinskaya D.I. Conception of decreasing of preventable health loss in children. Voprosy sovremennoi pediatrii=Current Pediatrics, 2010, vol. 9, no. 5, pp. 5–9 (in Russian).
- Albitsky V.Yu., Modestov A.A., Yakovleva T.V., Mendelevich B.D. Preventability of losses in children’s health as an effective resource saving strategy in public health. Sotsial’nye aspekty zdorov’ya naseleniya=Social Aspects of Population Health, 2010, no. 4 (16) (in Russian).
- Farrakhov A.Z., Shavaliev R.F., Sadykov M.M. Health centers for children as a priority direction of the prophylactic activity of pediatrics service. Meditsinskii al’manakh=Medical Almanac, 2013, no. 2 (26), pp. 12–15 (in Russian).
- Kovtun O.P., Anufrieva E.V., Malyamova L.N., Tsarkova S.A. Organization of preventive medical examinations of minors in the Sverdlovsk region: Ways to improve quality. Ural’skii meditsinskii zhurnal=Ural Medical Journal, 2018, no. 6 (161), pp. 118–125 (in Russian).
- Sukhareva L.M., Namazova-Baranova L.S., Rapoport I.K. The morbidity of Moscow schoolchildren in thedynamics of the learning from the first to the ninth grade (longitudinal study). Rossiiskii pediatricheskii zhurnal=The Russian Pediatric Journal, 2013, no. 4, pp. 48–53 (in Russian).
- Natsun L.N. Incidence of Malignant Neoplasms in Children in the Regions of the North-Western Federal District. In: Instituty razvitiya chelovecheskogo potentsiala v usloviyakh sovremennykh vyzovov: sbornik statei XI Ural’skogo demograficheskogo foruma: v 2-kh t. [Human development institutions in the context of modern challenges: Collection of articles of the XI of the Ural Demographic Forum: in 2 volumes.]. Volume II. Ekaterinburg: Institut ekonomiki UrO RAN, 2020. pp. 187–193 (in Russian).
- Banteva M.N., Manoshkina E.M., Sokolovskaya T.A., Matveev E.N. Trends in incidence and dynamics of chronic pathology in children aged 0-14 in the Russian Federation. Sotsial’nye aspekty zdorov’ya naseleniya=Social Aspects of Population Health, 2019, no. 65 (5). DOI: 10.21045/2071-5021-2019-65-5-10 (in Russian). Available at: http://vestnik.mednet.ru/content/view/1105/30/lang,ru/ (accessed: 19.08.2020).
- Razvarina I.N., Natsun L.N. Health of children aged 0–3 in the Vologda region. Sotsial’nye aspekty zdorov’ya naseleniya=Social Aspects of Population Health, 2019, no. 1 (65). DOI: https://dx.doi.org/10.21045/2071-5021-2019-65-1-7 (in Russian). Available at: http://vestnik.mednet.ru/content/view/1047/30/lang,ru/ (in Russian).
- Baranov A.A. et al. Trends and the health status of the child population of the Russian Federation. Rossiiskii pediatricheskii zhurnal=The Russian Pediatric Journal, 2012, no. 6, pp. 4–9 (in Russian).
- Shabunova A.A., Kondakova N.A. Children’s health and development: Results of a 20-year monitoring. Ekonomicheskie i sotsial’nye peremeny: fakty, tendentsii, prognoz=Economic and Social Changes: Facts, Trends, Forecast, 2014, no. 5 (35), pp. 33–54 (in Russian).
- Ivanova M.A., Lyutsko V.V. Analysis of the security and staffing pediatricians precinct in the Russian Federation for the period 2007-2016 years. Sovremennye problemy zdravookhraneniya i meditsinskoi statistiki=Current Problems of Health Care and Medical Statistics, 2019, no. 1, pp. 167–185. DOI: 10.24411/2312-2935-2019-10011 (in Russian).
- Razvarina I.N., Kalachikova O.N. Private or public? Parental assessment of the conditions of children’s medical service. Diskurs=Diskurs, 2018, no. 12 (26), pp. 293–310 (in Russian).


