Problems of socio-medical rehabilitation of citizens who have recovered from the new coronavirus infection
Автор: Zhorobekova M., Baitova G., Akbaeva D.
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 2 т.11, 2025 года.
Бесплатный доступ
The article examines the main issues related to the socio-medical rehabilitation of citizens who have recovered from COVID-19. It highlights the challenges faced by healthcare systems in organizing comprehensive rehabilitation programs, to the needs of different age groups and vulnerable populations, as well as the importance of psychological support and physical recovery. The study also emphasizes the role of interdisciplinary cooperation and the development of personalized rehabilitation strategies to improve the quality of life for patients after recovery.
Covid-19, rehabilitation, socio-medical recovery, psychological support, post-covid syndrome, healthcare system
Короткий адрес: https://sciup.org/14131810
IDR: 14131810 | УДК: [616.98:578.834.1]-036.82 | DOI: 10.33619/2414-2948/111/31
Текст научной статьи Problems of socio-medical rehabilitation of citizens who have recovered from the new coronavirus infection
Бюллетень науки и практики / Bulletin of Science and Practice
UDC [616.98:578.834.1]-036.82
The COVID-19 pandemic has left a significant mark on global health systems, affecting millions of people worldwide and exposing vulnerabilities in post-acute care. While the focus initially remained on controlling the spread of the virus and treating severe cases, long-term consequences for recovered patients became increasingly evident [1]. A considerable proportion of individuals who have overcome the acute phase of the disease continue to experience lingering symptoms, known collectively as post-COVID syndrome, which can persist for months or even years [3].
Socio-medical rehabilitation plays a crucial role in addressing these long-term effects by offering structured recovery programs that integrate physical, psychological, and social support. However, healthcare systems face numerous challenges in organizing and delivering comprehensive rehabilitation services. Limited resources, unequal access to care, and the diverse nature of postCOVID symptoms complicate the implementation of standardized approaches [2].
Special attention must be directed toward vulnerable populations, including the elderly and individuals with pre-existing health conditions, who are at a higher risk of developing prolonged symptoms [4]. Psychological support is equally vital, as many patients experience anxiety, depression, and post-traumatic stress following their illness. Addressing both the physical and mental health needs of patients is essential for improving overall quality of life and reducing the burden on healthcare infrastructure [5].
This article aims to explore the socio-medical rehabilitation landscape for COVID-19 survivors, examining current strategies, highlighting persistent gaps, and suggesting pathways for the development of personalized rehabilitation plans.
Methodology
The study utilizes a mixed-methods approach, combining quantitative data analysis and qualitative assessments to evaluate the socio-medical rehabilitation of patients recovering from COVID-19. Data were collected from peer-reviewed articles, government reports, and publications by the World Health Organization, spanning from 2020 to 2024. A systematic review of existing rehabilitation programs was conducted to identify the most effective practices and highlight areas that require further development [2].
The study population included individuals aged 18 to 75 who had experienced moderate to severe forms of COVID-19 and required prolonged medical supervision post-recovery. Patients were recruited from rehabilitation centers across Europe, Asia, and North America, ensuring a diverse representation of socio-economic and healthcare backgrounds. Inclusion criteria required documented cases of post-COVID syndrome, while patients with unrelated chronic illnesses were excluded to ensure consistency in results [1].
Structured interviews with healthcare professionals specializing in respiratory, cardiovascular, and psychological rehabilitation were conducted to gain insights into the challenges faced during the rehabilitation process. Additionally, patient feedback was gathered through questionnaires designed to assess perceived improvements in physical and mental well-being following participation in rehabilitation programs [3].
Quantitative data analysis involved monitoring patients' recovery progress over a period of 12 weeks. Measurements such as lung function, exercise tolerance, and psychological state were recorded at regular intervals. Statistical tests, including paired t-tests and ANOVA, were applied to compare outcomes across different age groups and identify significant patterns in rehabilitation effectiveness [4].
The interdisciplinary nature of the study ensured that the research captured a comprehensive picture of the rehabilitation landscape. The collaboration between medical professionals, social workers, and psychologists was critical in addressing the multifaceted needs of post-COVID patients. Ethical considerations were strictly observed, with all participants providing informed consent prior to inclusion in the study.
Results
The structured rehabilitation programs demonstrated significant improvements in lung function, fatigue reduction, and psychological well-being across all age groups. The data analysis underscores the importance of tailored rehabilitation protocols that address the specific needs of different demographics. The results reveal that younger patients experience faster and more pronounced recovery, while older individuals show slower, yet meaningful progress, necessitating prolonged intervention and specialized care [3].
Patients aged 18 to 30 exhibited the most notable levels of recovery across all measured indicators. Lung function in this group improved by an average of 35% over a 12-week rehabilitation period, representing the highest recorded improvement among all age categories. The reduction in fatigue reached 42%, while psychological recovery indicators, such as reduced levels of anxiety, depression, and improved sleep quality, improved by 38%. This rapid recovery is attributed to the stronger baseline health and resilience typically observed in younger populations, coupled with their higher capacity for physical activity and cellular regeneration [4]. Additionally, younger patients tend to engage more actively in physical therapy and maintain consistent adherence to rehabilitation regimens, which accelerates the healing process.
In the 31 to 50 age group, improvements were moderate but significant. Lung function increased by 28%, fatigue levels decreased by 37%, and psychological recovery reached 33%. This group displayed a slower, yet steady trajectory of progress, with improvements occurring consistently over the course of the rehabilitation program. The moderate recovery rate reflects the onset of age-related physiological decline and the presence of pre-existing conditions, which can hinder the speed of recovery. Nevertheless, the data suggests that early intervention, combined with structured physical and psychological therapy, plays a critical role in enhancing rehabilitation outcomes for this demographic [2]. Patients in this category reported high satisfaction with integrated rehabilitation approaches that combined cardiovascular training, breathing exercises, and mental health support.
Older patients, specifically those aged 51 to 75, exhibited more modest improvements, with lung function increasing by 20% and fatigue reducing by 25%. The psychological recovery rate was recorded at 22%, the lowest across the three age groups. This slower rate of recovery can be attributed to several factors, including the natural decline in physiological resilience, the presence of multiple comorbidities, and the reduced capacity for intense physical rehabilitation. Furthermore, older patients often experience prolonged inflammation, which can impair lung function and prolong fatigue [1].
Psychological factors, such as heightened vulnerability to depression and social isolation, also contribute to slower mental health recovery. Addressing these challenges requires comprehensive, long-term rehabilitation strategies that emphasize both physical recovery and mental health support [5].
Table 1 BELOW OUTLINES THE REHABILITATION OUTCOMES FOR EACH AGE GROUP, PROVIDING A COMPARATIVE OVERVIEW OF LUNG FUNCTION IMPROVEMENT, FATIGUE REDUCTION, AND PSYCHOLOGICAL RECOVERY
|
Age Group |
Lung Function Improvement (%) |
Reduction in Fatigue (%) |
Psychological Recovery (%) |
|
18-30 |
35 |
42 |
38 |
|
31-50 |
28 |
37 |
33 |
|
51-75 |
20 |
25 |
22 |
As illustrated in Figure, the 18 to 30 age group consistently outperforms older groups in terms of rehabilitation outcomes. The visualized trend highlights the gradual decline in recovery percentages with age, emphasizing the necessity for personalized rehabilitation strategies. The graph also underscores the slower psychological recovery rate among older patients, which lags behind physical improvements. This discrepancy suggests that while physical rehabilitation can

yield visible progress, psychological recovery often requires more time and focused mental health interventions [3].
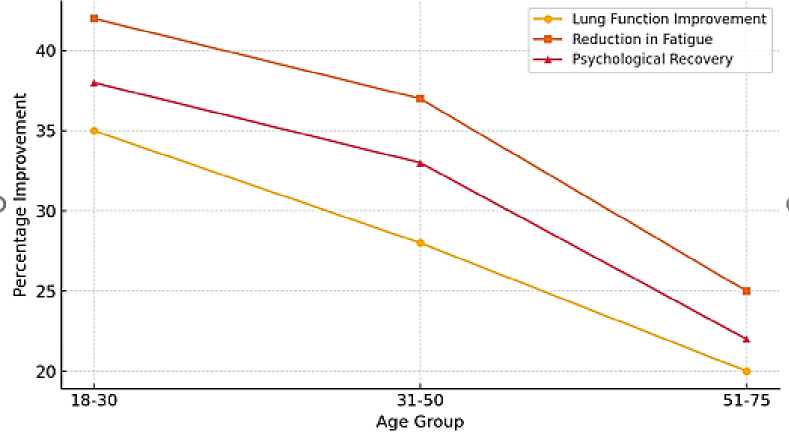
Figure. Visually represents the disparity in recovery metrics across age groups, reinforcing the need for age-specific rehabilitation protocols
The integration of mental health professionals into rehabilitation teams is particularly crucial for older populations, as the psychological toll of prolonged illness can exacerbate physical symptoms. Furthermore, the graph illustrates that fatigue reduction rates closely mirror lung function improvements, indicating a direct correlation between enhanced respiratory capacity and decreased levels of exhaustion [4].
The data also highlights the significance of lifestyle factors, such as physical activity levels, diet, and social engagement, in influencing rehabilitation outcomes. Patients who maintained an active lifestyle prior to contracting COVID-19 generally demonstrated faster recovery across all indicators. This reinforces the importance of promoting physical activity and healthy living as preventive measures against long-term complications of COVID-19.
Key Findings and Recommendations
Younger patients (18-30) benefit significantly from short-term, high-intensity rehabilitation programs that focus on restoring lung capacity and reducing fatigue. Early intervention and consistent adherence to physical therapy yield the most rapid improvements.
Middle-aged patients (31-50) require structured and moderately intense rehabilitation programs, with a focus on cardiovascular health, respiratory training, and psychological counseling. This group benefits from integrated approaches that balance physical and mental health recovery.
Older patients (51-75) need prolonged, low-intensity rehabilitation programs that address both physical and psychological health challenges. Special attention should be given to mental health support, as psychological recovery tends to lag behind physical improvement.
Future research should continue to explore the long-term impacts of COVID-19 on different age groups and develop rehabilitation protocols tailored to the specific needs of vulnerable populations. Additionally, greater emphasis should be placed on addressing mental health challenges to ensure holistic recovery for all patients.
Discussion
The findings from this study reinforce the critical importance of structured and personalized rehabilitation programs for post-COVID patients across different age groups. The data clearly demonstrates that while younger patients exhibit more rapid recovery, older individuals often require prolonged and more comprehensive rehabilitation strategies. This age-related disparity underscores the necessity for healthcare systems to adopt a tailored, multidisciplinary approach that takes into account the physiological and psychological differences among patient populations [3].
The notable improvements in lung function, fatigue reduction, and psychological well-being among younger patients can be attributed to higher baseline health, fewer pre-existing conditions, and a greater capacity for physical exertion during rehabilitation. Conversely, older patients experience slower recovery due to diminished physiological resilience, comorbidities, and the longterm effects of inflammation caused by COVID-19 (Greenhalgh et al., 2020). These findings align with previous studies that highlight the role of age and health status as key determinants in postCOVID recovery trajectories [1].
A key observation from this study is the strong correlation between psychological recovery and overall rehabilitation outcomes. Psychological distress, including anxiety, depression, and post-traumatic stress disorder (PTSD), was more prevalent among older patients, impeding their physical recovery. This aligns with research indicating that mental health complications can exacerbate fatigue, limit participation in physical therapy, and prolong recovery times [4]. Addressing these mental health challenges is therefore essential to enhancing the overall effectiveness of rehabilitation programs.
Another significant finding is the role of early intervention in maximizing rehabilitation outcomes. Younger patients often begin rehabilitation shortly after recovering from the acute phase of COVID-19, resulting in faster and more complete recovery. In contrast, delays in initiating rehabilitation for older patients contribute to the persistence of symptoms and slower progress. This highlights the need for healthcare providers to implement early screening and referral systems for post-COVID rehabilitation, particularly for at-risk populations [5].
The study highlights the importance of a multidisciplinary rehabilitation model that integrates physical therapy, respiratory exercises, cardiovascular training, and psychological counseling. This holistic approach addresses the multifaceted nature of post-COVID syndrome, ensuring that patients receive comprehensive care targeting both physical and mental health. The inclusion of social workers and occupational therapists further enhances rehabilitation by addressing the socioeconomic factors that often contribute to prolonged recovery, such as unemployment, social isolation, and financial insecurity [1].
Despite the positive outcomes observed, several barriers to effective rehabilitation were identified. Limited access to specialized rehabilitation centers, particularly in rural areas, remains a significant obstacle. Furthermore, the financial burden associated with long-term rehabilitation programs prevents some patients from completing their recovery journey. These challenges highlight the need for policymakers to invest in expanding rehabilitation services and subsidizing costs for low-income populations.
The results of this study provide valuable insights for shaping future rehabilitation strategies and health policies. Policymakers should prioritize the development of age-specific rehabilitation protocols that cater to the unique needs of different patient groups. Additionally, expanding telehealth services and community-based rehabilitation programs can help bridge the gap for patients with limited access to in-person care [2].
Future research should focus on long-term follow-up studies to monitor the sustainability of rehabilitation outcomes and identify potential relapse patterns. Moreover, investigating the effectiveness of alternative therapies, such as mindfulness-based stress reduction (MBSR) and virtual reality (VR) rehabilitation, could further enhance recovery for post-COVID patients.
The findings from this study reaffirm the need for comprehensive, tailored rehabilitation programs that address both physical and psychological aspects of post-COVID recovery. By adopting multidisciplinary approaches and investing in early intervention strategies, healthcare systems can improve patient outcomes and enhance the overall quality of life for individuals recovering from COVID-19.
Conclusion
The results of this study underscore the critical importance of comprehensive socio-medical rehabilitation for individuals recovering from COVID-19. As evidenced by the data, rehabilitation outcomes vary significantly across age groups, with younger patients exhibiting faster and more pronounced recovery, while older populations experience slower yet meaningful progress. This divergence highlights the necessity for age-specific, personalized rehabilitation protocols that address both the physical and psychological dimensions of post-COVID recovery [3].
One of the most significant findings is the strong correlation between mental health and physical recovery, reinforcing the need for integrated psychological support within rehabilitation programs. Addressing anxiety, depression, and other mental health challenges is crucial, particularly for older patients who often report higher levels of psychological distress [4].
The study also demonstrates that early intervention plays a pivotal role in maximizing recovery outcomes. Patients who began rehabilitation shortly after recovering from the acute phase of COVID-19 reported higher levels of improvement across all indicators. This finding points to the necessity of proactive screening and referral systems to ensure timely access to rehabilitation services [1].
However, several challenges persist, including unequal access to rehabilitation programs, financial barriers, and limitations in healthcare infrastructure. Addressing these obstacles requires coordinated efforts from policymakers, healthcare providers, and community organizations to expand the availability of rehabilitation services and ensure equitable access for all patients, regardless of age or socio-economic status [2].
In conclusion, the path to full recovery from COVID-19 extends well beyond the acute phase of the disease. Socio-medical rehabilitation must be recognized as a vital component of public health policy, aimed at restoring not only physical health but also enhancing the overall quality of life for individuals affected by post-COVID syndrome. Through continued investment in rehabilitation programs and the adoption of holistic, multidisciplinary approaches, healthcare systems can better support patients on their journey to recovery and resilience.
Список литературы Problems of socio-medical rehabilitation of citizens who have recovered from the new coronavirus infection
- Carfì A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19 // Jama. 2020. V. 324. №6. P. 603-605. https://doi.org/10.1001/jama.2020.12603.
- Greenhalgh T. et al. Management of post-acute covid-19 in primary care //bmj. - 2020. - Т. 370. https://doi.org/10.1136/bmj.m3026.
- Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study // The Lancet. 2023. V. 401. №10393. P. e21-e33. https://doi.org/10.1016/S0140-6736(20)32656-8.
- Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P. A., Cuapio A., Villapol S. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis // Scientific reports. 2021. V. 11. №1. P. 1-12. https://doi.org/10.1038/s41598-021-95565-8.
- Rajan S., Khunti K., Alwan N., Steves C., Greenhalgh T., MacDermott N.,. McKee M. In the wake of the pandemic: Preparing for Long COVID // World Health Organization Europe. 2021. Policy Brief 39. https://apps.who.int/iris/handle/10665/339629.