Revisiting Cardiovascular Reflexes and Resetting in Healthy Adolescents to Analyse Mechanisms of Physiological and Pathophysiological Factors Influencing Individual Blood-Pressure Components
Автор: Shantala S. Herlekar
Журнал: Журнал стресс-физиологии и биохимии @jspb
Статья в выпуске: 2 т.17, 2021 года.
Бесплатный доступ
Background and objectives: Understanding oscillations of cardiovascular parameters (BP, HR, blood flow, heart contractility, etc.) has been a puzzling issue. This paper intends to assess the effects of various physiological and pathological factors like gender, age, BMI, handedness acute perceived stress and chronic perceived stress on individual components of blood pressure, and to evaluate and gauge the physiological and pathophysiological reflex mechanisms for the same. Methods: 120 normotensive, healthy adults were included with equal gender ratio. After obtaining consent, age, BMI, Handedness and STAI for perceived acute and chronic stress were recorded. BP components i.e. SBP, DBP, PP, MAP and RPP were recorded and calculated. Physical, psychological, physiological and pathological factors affecting cardiac and vascular systems were deliberated. Mean, SD, T-test and Pearson’s correlation were used for analysis. Results: Gender difference in BP showed cardiac and vascular protective role of oestrogen in females through eNOS. Age had significant negative correlation with RPP suggesting early changes in cardiac mass reducing oxygen extraction by the myocardium, while based on various neuroendocrinal, hormonal and renal mechanisms, BMI showed strong positive correlation with SBP, DBP and MAP, proposing changes within circulating blood volume, cardiac output and large vessels. Unlike previous studies, there was no correlation between handedness and BP components on subjects at rest, suggesting cerebral dominance on autonomic influences might be active only in BP stimulating situations. Acute perceived stress showed negative correlation with all BP components recommending extended biopsychosocial model and active baroreceptor reflex unlike acute physical stress, which shows elevated BP, which can only be obtained by resetting threshold response of baroreceptor to higher level. Chronic perceived stress correlated with elevated SBP and MAP suggesting rumination, cardiovascular remodelling, reflex adaptation and resetting. Conclusion: Our study has tried to hypothesise specific physiological and pathophysiological mechanisms which might be involved in changes of individual blood pressure components. It is fascinating to notice that none of the observed factors (physiological and pathological) has any correlation with Heart Rate. Our subjects were at rest and hence, heart rate was normal, showing no variations. This article helps to understand probable underlying mechanisms for the same.
Rumination, rate pressure product, perceived stress, extended biopsychosocial model, reflex resetting
Короткий адрес: https://sciup.org/143173888
IDR: 143173888
Текст научной статьи Revisiting Cardiovascular Reflexes and Resetting in Healthy Adolescents to Analyse Mechanisms of Physiological and Pathophysiological Factors Influencing Individual Blood-Pressure Components
Blood pressure is the lateral pressure exerted by the column of blood within the major arterial system. As measured in the brachial artery, blood pressure is maintained by cardiac output and the total peripheral resistance (TPR). The ideal blood pressure adequately perfuse all organ systems, without causing damage. Because the arterial pressure is the product of the cardiac output and the peripheral resistance, it is affected by conditions that affect either or both of these factors. Genders, menstruation, age, BMI, stress are few to name.1, 2
Blood pressure is conventionally separated into systolic and diastolic blood pressure. The systolic blood pressure is the maximum pressure experienced in the aorta when the heart contracts and ejects blood from the left ventricle, approximately 120 mm Hg. The diastolic blood pressure is the minimum pressure experienced in the aorta when the heart is relaxing before ejecting blood; often approximately 80 mm Hg. Systolic blood pressure determines the highest systolic pressure of left ventricle and measures “cardiac component”. While diastolic blood pressure signifies total peripheral resistance and is a measure of “vascular component”. The mean arterial pressure (MAP) is the average of the arterial pressures measured millisecond by millisecond over a period of time. The mean arterial pressure is determined about 60 per cent by the diastolic pressure and 40 per cent by the systolic pressure. Baroreceptors respond mainly to changes in mean arterial pressure and normal functional baroreceptors maintain MAP within a narrow range of 85 and 115 mm Hg.3 The difference between systolic and diastolic pressure is pulse pressures and is about 40-50 mm Hg. Two major factors affect pulse pressure: (1) the stroke volume of the heart and (2) the compliance (total distensibility) of the arterial tree, directly proportional to former and inversely proportional to the latter.4 Rate Pressure Product (RPP) is the product of heart rate and systolic blood pressure. It is an easily measurable index which correlates well with myocardial oxygen demand and defines the response of coronary circulation to myocardial metabolic demands.5
Blood pressure and its various components are affected by multiple physiological, psychological and pathological factors. Reflex mechanisms within the cardiovascular systems are well established which alter blood pressure, but probable focused mechanism for each factor affecting specific components of blood pressure (SBP, DBP, MAP, PP, RPP) has a large scope for discussion, re-evaluation and frequent revisiting.
OBJECTIVES
-
1. To assess the effects of various physiological factors like gender, age, BMI and handedness on individual components of blood pressure.
-
2. To assess the effects of pathological factors like acute perceived stress and chronic perceived stress on individual components of blood pressure.
-
3. Evaluating and gauging the physiological and pathophysiological reflex mechanisms for the above.
MATERIALS AND METHODS
“The departmental ethical committee and college Dissertation and research committee, KLE JNMC, Belgaum” issued institutional ethical clearance (Reference number: MDC/PG/742). A well-informed oral and written consent was taken from all subjects, after explaining the procedure and merits of the study. This study was conducted in department of Physiology research lab on working days (except Saturdays and Sundays) between 4pm to 6pm. After conducting a pilot study, and taking ά = 0.05, ά = 1.65, β = 0.2, Power 80%, β = 0.84, sample size was calculated and 120 healthy young adults in the age group of 18-22years were included in the study with equal number of girls and boys. Subjects with history of drug intake, smokers, alcoholics, endocrine dysfunctions, autonomic dysfunction, hypertension, family history of disorders, menstrual disorders or any health issues were excluded from the study. Anthropometric parameters were recorded.
Blood pressure components: Blood pressure was recorded in upper right arm in sitting position after 30 minutes of complete rest with Omron BP Monitor Semi -Automatic (HEM-4030). BP was measured twice at 10min intervals. The average value of these 2 records was taken into the analysis. The following parameters were determined.
-
• Blood pressure (BP)(mm of Hg): systolic blood pressure (SBP), diastolic blood pressure (DBP)
The following parameters were calculated by the formulas
-
• Pulse pressure (PP) (mm of Hg) = SBP-DBP
-
• Mean arterial pressure (MAP) (mm of Hg) = DBP + 1/3 PP
-
• RPP (mm Hg. beats per min.10-2) = SBP*HR 5, 20
Physiological factors
-
• Gender: male, female.
-
• Age in years: calculated from date of birth.
-
• Height in mts: By commercial stadiometer
-
• Weight in kgs: By digital weighing scale (seca) with an accuracy of ±100grms
-
• Body mass index (Kg/mts2): weight (kg) height (mts)2
-
• Handedness : was determined using Annett
Handedness Questionnaire.7
Pathological factors:
-
• Stress: To assess acute and chronic perceived anxiety, State Triat Anxiety Inventary (STAI) was used. This comprises separate self-report scales for measuring “state” and “trait” anxiety. The S-Anxiety scale consists of twenty statements that evaluate how respondents feel “right now, at this moment” indicating acute perceived stress. The T-Anxiety scale consists of twenty statements that assess how the respondents feel “generally” indicating chronic perceived stress. The scores for the S-Anxiety and T-Anxiety scales were obtained by adding the weighted scores for the twenty items. Scores for both scales can vary from a minimum of 20 to a maximum of 80.8
Statistical analysis; was performed using SPSS software version 20. Mean, SD, T-test and Pearson’s correlation were used for analysis. Values are expressed as mean ± standard deviation (SD). P < 0.05 was considered as statistically significant.
RESULTS AND DISCUSSION
Following observations were made in 120 healthy subjects. Data has been arranged into physiological and pathological factors affecting different components of blood pressure. Significant values have been highlighted. Results will be followed by the probable Physiological and Pathological mechanism that might have caused the observed change.
Gender and blood pressure components:
Table 1 shows gender difference obtained in all components of Blood pressure. It is evident that all values i.e SBP, DBP, PP, MAP and RPP are higher in males compared to females. It indicates that few factors in females affect both the cardiac and the vascular system, protecting them from higher blood pressure. It is interesting to know that women of same race and age have smaller heart and major blood vessels compared to men.9
This study was done in young adolescent subjects. All female subjects had attained menarche and had regular menstrual cycles. Estrogen is a potent steroid hormone present in high levels in females from adolescence to menopause and in low levels in men. There are two established estrogen receptors, α and β on which E2 (estrogen) acts. ERα is present in cardiac and vascular tissue while ER β is present mainly in cardiac tissue (table 2). ERα and β are found both in association with the plasma membrane and in the nucleus.10 The following paragraphs briefly enumerate the effects of estrogen on vascular system and the cardia separately.
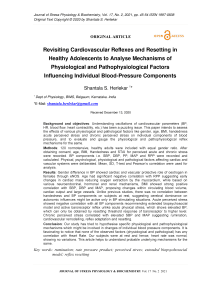
Vascular effects: (figure:1) ERα knockout reduced basal NO production in the aorta which causes vascular relaxation, while ERβ knockout had no effect on NO production. It activates eNOS, inhibits VSMC proliferation and inhibits increase in medial thickness. Estrogen is also known to reduce atherosclerosis and improves flow-induced arteriole dilatation.11 All these effects on vascular system probably leads to decrease vascular resistance and in turn DBP in females as compared to males.
Cardiac effects: (figure:2) through ER α and β, estrogen has cardioprotective effects and reduces apoptosis by stabilizing the mitochondrial membrane and preventing apoptosome formation.12 It prevents pathological hypertrophy associated with hypertension and prevents cardiac fibrosis.13 It also reduces damage in settings of cardiac ischemia and reperfusion. In addition ER2 increases heat shock proteins and reduces the gene expression for pro-inflammatory cytokines.14
Other contributory factors : At all ages, women have reduced sympathetic activity and enhanced parasympathetic activity relative to men. Similarly, men tend to have higher plasma norepinephrine levels than women.15 Additionally, since women have smaller heart than men, this leads to lower stroke volume and thus lower cardiac output.9, 16 The effective circulatory blood volume is less in females compared to males.17 These effects might reduce SBP in adolescent female as compared to males.
Reduced MAP in females can be explained based on the finding that the means of SBP and DBP is less. Also total peripheral resistance in males is more which leads to increased DBP, which in turn is a major determinant of MAP.15 PP is the ratio of stroke volume and compliance of blood vessels.18 In females, less blood volume leads to lesser stroke volume and, the blood vessels are more compliant. Thus the altered ratio leads to reduced pulse pressure. Heart rate reading reversed in males i.e less in males compared to females and can be explained based on well-established Marys law in Physiology which states that, within physiological limits, heart rate is inversely proportional to blood pressure.
Age and blood pressure components:
As age advances, various macroscopic and microscopic changes take place in both cardiac and vascular system. To name a few; in the vascular system there is thickening and dilation of large arteries, arterial wall media hypertrophy, extracellular matrix accumulation, calcium deposits, vascular endothelium dysfunction, that are associated with increased vascular stiffness and pulmonary arterial remodelling. While in the cardia, there is increase in myocardial thickness due to increased myocyte size, thickening of interventricular septum, decrease in the total number of cardiomyocytes, likely due to apoptosis, increase in collagen content, fibrosis, and deposition of cardiac amyloid and lipofuscin within the connective tissue.19 All these changes occur after 3rd decade of life and accelerate after 5th decade.
Our study consisted of young healthy adults in early 20s. A significant negative correlation is seen of yearly advancing age with Rate Pressure Product i.e RPP. As mentioned in introduction, Rate Pressure Product is the product of heart rate and systolic blood pressure. It correlates well with myocardial oxygen and metabolic demand and defines the coronary perfusion status.5, 20 A negative correlation of age with RPP indicates reduced myocardial metabolic demands which might indicate early reduction in myocyte mass probably due to apoptotosis and fibrotic changes or, lipofuscin and amyloid deposits within cardiacmyocytes as early as 2nd decade of life and progressing every year of advancing age. But this statement need further research and proof.
BMI and blood pressure components:
Effect of elevated BMI on blood pressure is through multiple mechanisms. Its role in metabolic, endothelial and vascular dysfunction, neuroendocrine imbalance, sodium retention, glomerular hyper filtration, proteinuria, maladaptive immune and inflammatory responses are well established. 21 In our study BMI independently and positively correlates with SBP, DBP and MAP (table 3). Let us look for various mechanisms which might bring about these changes.
Elevated SBP: increase BMI leads to increase glucose load in circulation and eventually in the renal system. The proximal convoluted tubule up-regulates sodium-glucose symporter to reabsorb glucose and, along with this, excess sodium is reabsorbed, leading to glucose toxicity and sodium excess in circulation.22 This increases intravascular volume in obesity, directing cardiac output and SBP to rise. Also increase in adipose mass and extracellular matrix accumulation is said to compress the renal medulla, which leads to inappropriate Renin-Angiotensin-Aldosterone-System (RAAS) and Sympathetic Nervous System (SNS) activation, further contributing to increased sodium reabsorption.22 These and many other neuroendocrine factors, deregulated RAAS (especially angiotensin II and aldosterone) and, along with autonomic dysfunction, might lead to significant rise in total blood volume preceding increasing cardiac work load during systole and positive correlation of BMI with SBP.
Elevated DBP: endothelial dysfunction, arterial stiffness, changes in extracellular matrix, and vascular smooth muscle dysfunction are some of the earliest changes in obesity seen even before the onset of prehypertension.23 Elevated adipose tissue mass produces elevated levels of RAAS components especially angiotensin II and aldosterone, which have well proven vascular effects. Hyperinsulinemia, hyperleptinemia and baroreflex dysfunction also promote activation of sympathetic nervous system in diverse tissues like skeletal muscle.21 This is a major seat for peripheral resistance. The immune system, with its innate and adaptive limb, plus increased inflammatory response leads to vascular intimal injuries. All these may lead to increased peripheral resistance thus showing positive correlation with DBP.24-26, 41
Elevated MAP: MAP is the main player for regulating baroreceptor reflex. Previous research indicates baroreceptors initially respond to changing heart rate and cardiac output, but after 6-8sec changing arterial pressure is mainly determined by the effect of peripheral resistance on baroreceptor.27 As BMI increases, due to metabolic dysregulation or abnormal neuroendocrine functions, sympathetic nerves overacts and baroreceptors become hyporesponsive.21 From the above discussion, it is noted that both SBP and DBP increase which might explain the effect of BMI on MAP.
Handedness on Blood Pressure components:
Research has indicated a differential control of each cerebral hemisphere over dynamics of the heart like heart rate, blood pressure and myocardial contractility. The right hemisphere is said to have a greater control over heart rate while the left hemisphere affects myocardial contractility. These studies suggest that cerebral hemispheres have differential control over the heart which must happen via the autonomic nervous system. There is evidence that sympathetic activity is controlled by the right cerebral hemisphere, which is dominant in left handers. Therefore, handedness may also modulate autonomic control of the heart.28 Handedness is typically described as the hand one prefers to use for unimanual tasks. Human hand preference emerges very early in an infant’s life, where genetics and environmental influences are believed to play a key role in development.7 Our study did not show any significant correlation with baseline variations in blood pressure components with hand preferences (table 3). Probably this might indicate that cerebral dominance and control of autonomic function becomes evident in stressful conditions where blood pressure is up regulated. Subjects were at rest in our study.
Acute percieved stress on Blood pressure components:
Blood pressure responds to both physical and mental stress. This is necessary to maintain adequate blood flow towards stress responsive organs. But the response obtained changes for physical and mental stress. This has been explained as “extended biopsychosocial model”.29, 30 To understand this concept, a comparison between response to physical stress and mental stress is helpful.
Physical stress : Baroreceptor reflex is a part of negative feedback system that stabilises fluctuations in arterial pressure due to various factors. During physical stress eg: exercise, an increase in arterial pressure, heart rate, cardiac output and sympathetic activity is seen.31 What causes BP to rise in physical exercise even with a normal functional baroreceptor? Human and animal experiments, using variable pressure neck collar, have suggested that during dynamic exercise, Baroreceptors are reset to work at a higher range of arterial pressure than compared to resting levels. The gain of the system remains unchanged.32 2 factors that are responsible for the resetting are; the Central command by motor cortex and, afferent inputs from mechanoreceptors and chemoreceptors of active skeletal muscles.33
Mental stress: The response of blood pressure and baroreceptor to mental stressors is slightly different. This depends on pre-existing psychological traits which also determines the direction of BP change. This is called “extended biopsychosocial model”.34 Stress which are handled by active coping strategy result in elevated BP.35 “Active coping” means taking action or exerting efforts to remove or circumvent the stressor which includes acceptance of the situation, planning to confront and positive reframing i.e. seeing it in a more positive light. Yoga, meditation, listening to music and other recreations can all be a part of active coping. Denial can be another outcome with stress, where there is attempt to reject the reality, along with behavioural disengagements like giving up, withdrawal efforts, avoidant strategies including use of alcohol, tobacco and drug abuse. Genetic composition also plays a role.36
In our study a significant negative correlation was seen between acute perceived stress and SBP, DBP, MAP and RPP (table 3). The probable explanations could be: acute mental stress lead to rise in cardiac output, heart rate and sympathetic nervous system. This lead to reflex activation of baroreflex and hence as mental stress increased, BP components reduced. This could in-turn mean that adolescents in our study used negative coping strategies as, response to their mental stress was reduced BP. (Baroreceptor was not reset to higher levels).35 Decreased SBP indicates cardiac component, DBP indicates vascular component, MAP indicates mean of blood pressure and RPP indicates coronary circulation efficacy. All these are various limbs of baro-receptor reflex.
Chronic stress on Blood pressure components:
Physiology of blood pressure homeostasis during stress should remain active only uptill the stress is present. If it persists beyond this point, the response becomes damaging. “Rumination” is a type of perseverative cognition which is, repetitive, negative thoughts, including anger, frustration, depression, anxiety which can sustain elevated BP. In other words stress related thoughts can persist for a substantial amount of time in anticipation of future stress and dealing with past stress.37
Our study, interestingly, showed significant negative correlation of blood pressure components with acute perceived stress but significant positive correlation with chronic perceived stress. Relation between BP and acute stress could be explained based on “extended biopsychosocial model”, as in previous paragraph while, relation of chronic stress to BP can be explained based on “rumination” effect. Subjects in our study probably had a common trait of persistent recall of negative experience, which activated their emotional stress response through the dorsomedial hypothalamus and perifornical area.38 During mental stress, these areas reset the baroreceptors to operate over higher range with increased gain.32 It has been hypothesised that, failure to return to baseline values following end of stressful stimuli, lack of habituation to repeated stress of similar type, and exaggerated response to acute stress are all precursors to development of hypertension.39,40 Our study showed significant positive correlation of chronic stress to SBP and MAP, probably early changes to chronic stress. This prospect needs further investigation.
Nitric Oxide t eNOS
Ф NO
^Relaxation фFlow-induced arteriole dilation
Atherosclerosis
^^ ;ldl fHDL ^Adhesion molecules ф Monocyte adhesion
ф ROS ф Inflammatory cytokines
Figure 1: Effects of estrogen on various components of vascular system. Reprint with permission 21
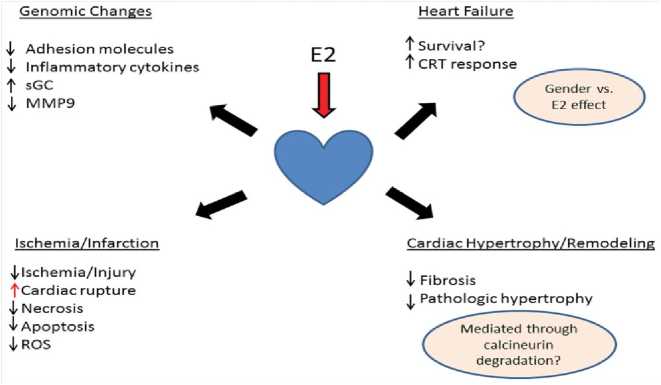
Figure 2: Effects of estrogen on heart. (Reprint with permission 21)
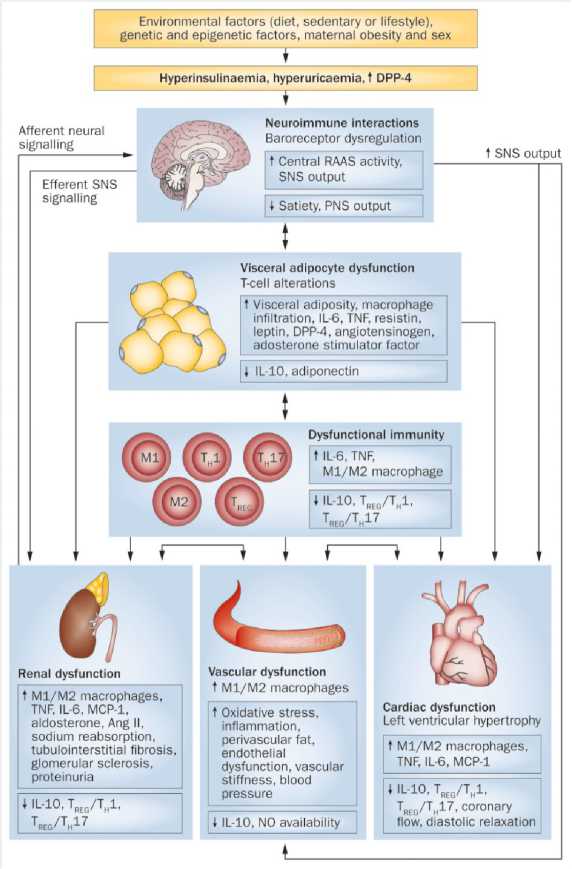
Figure 3 : Effect of elevated BMI on various organ systems. (Reprint with permission 21)
Obesity contributes to the development of hypertension via the interaction of dietary, genetic, epigenetic and environmental factors. Visceral adipocyte dysfunction leads directly to renal, cardiac and vascular dysfunction, via an impaired immune or inflammatory response, and by affecting neuroimmune interactions that alter SNS
signalling. Cardiac and/or renal abnormalities can lead to vascular dysfunction and vice-versa. Obesity-related hypertension is associated with structural and functional changes in the kidney, heart and vasculature. Hyperuricaemia might also affect adipocyte function and vascular remodelling, and cause renal abnormalities. Abbreviations: ↑, increased; ↓, decreased; Ang II, angiotensin II; DPP-4, dipeptidyl peptidase 4; MCP-1, monocyte chemoattractant protein-1; PNS, parasympathetic nervous system; RAAS, renin–angiotensin– aldosterone system; SNS, sympathetic nervous system; TH, T helper cell; TREG, T regulatory cell.
CONCLUSION
Our study has tried to hypothesise specific physiological and pathophysiological mechanisms which might be involved in changes of individual blood pressure components. It is fascinating to notice that none of the observed factors (physiological and pathological) has any correlation with Heart Rate. Our subjects were at rest and hence, heart rate was normal, showing no variations. This article is useful to evaluate/predict outcome of specific factor modification influencing specific blood pressure components. It also helps to understand probable underlying mechanisms for the same.
ACKNOWLEDGMENTS
ABBREVIATIONS:
-
• TPR: Total Peripheral Resistance
-
• RPP: Rate Pressure Product
-
• STAI: State Triat Anxiety Inventary
-
• E2: Estrogen
-
• RAAS: Renin Angiotensin Aldosterone System
-
• SNS: Sympathetic Nervous System
DECLARATIONS SECTION
-
• Ethical Approval and Consent to participate:
“The departmental ethical committee and college Dissertation and research committee, KLE JNMC, Belgaum” issued institutional ethical clearance (Reference number: MDC/PG/742;
dated:21/10/2011). Written and informed consent was obtained from all 120 participants
-
• Consent for publication: was obtained from
guide.
-
• Consent for publication of individual data: not relevant to the article.
-
• Availability of supporting data: is open for access
-
• Competing interests: None
-
• Funding: None
-
• Authors' contributions: inception of idea, data
collection, analysis, final write up and proof reading was done by single author.
Список литературы Revisiting Cardiovascular Reflexes and Resetting in Healthy Adolescents to Analyse Mechanisms of Physiological and Pathophysiological Factors Influencing Individual Blood-Pressure Components
- Brzezinski WA. Blood Pressure. In: Walker HK, HallWD, Hurst JW, editors. Clinical Methods: TheHistory, Physical, and Laboratory Examinations.3rd edition. Boston: Butterworths; 1990. Chapter16. Available from:https://www.ncbi.nlm.nih.gov/books/NBK268/.
- Ganong WF. Review of medical physiology. 23rded. Lange medical publications. 2010. Chapter 32,“Blood as a Circulatory Fluid & the Dynamics ofBlood & Lymph Flow”: pg: 545-546.
- Guyton AC and Hall JE. Textbook of medicalPhysiology. 11th ed. Elsevier Saunders publication.2006. Chapter 15, “Vascular Distensibility andFunctions of the Arterial and Venous Systems: pg175-76.
- Homan TD, Bordes S, Cichowski E. Physiology,Pulse Pressure. [Updated 2020 Apr 28]. In:StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing; 2020 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK482408/.
- Cockcroft JR, Wilkinson IB, Evans M, McEwan P,Peters JR, Davies S, Scanlon MF, Currie CJ. Pulsepressure predicts cardiovascular risk in patientswith type 2 diabetes mellitus. Am J Hypertens.2005 Nov;18(11):1463-1467.
- Kvaal K, Ulstein I, Nordhus IH, et al. SpielbergerState-Trait Anxiety Inventory (STAI): the state scalein detecting mental disorders in geriatric patients.Int J Geriatr Psychiatry; 2005; 20: 629-34.
- Annett M. (1970a). A classification of handpreference by association analysis. Br. J.Psychol. 61303–321 10.1111/j.2044-8295.1970.tb01248.x [PubMed].
- Knowlton AA and Lee AR. Estrogen and theCardiovascular System. Pharmacol Ther. 2012 July; 135(1): 54–70.doi:10.1016/j.pharmthera.2012.03.007.
- Vasan RS, Larson MG, Levy D, Evans JC,Benjamin EJ. Distribution and categorization ofechocardiographic measurements in relation toreference limits: The Framingham Heart Study.Formulation of a height-and sex-specificclassification and its prospective validation.Circulation 96: 1863–1873, 1997. [PubMed:9323074].
- Darblade B, Pendaries C, Krust A, Dupont S,Fouque MJ, Rami J, et al. Estradiol Alters NitricOxide Production in the Mouse Aorta Through theα-, but not the β-, Estrogen Receptor. Circ Res.2002; 90:413–419. [PubMed: 11884370].
- LeBlanc AJ, Reyes R, Kang LS, Dailey RA,Stallone JN, Moningka NC, et al. Estrogenreplacement restores flow-induced vasodilation incoronary arterioles of aged and ovariectomizedrats. AJP - Regulatory, Integrative and ComparativePhysiology. 2009; 297:R1713–R1723.
- Suzuki K, Murtuza B, Sammut IA, Latif N,Jayakumar J, Smolenski RT, et al. Heat ShockProtein 72 Enhances Manganese SuperoxideDismutase Activity During Myocardial Ischemia-Reperfusion Injury, Associated With MitochondrialProtection and Apoptosis Reduction. Circulation.2002; 106:270I–276.
- Pedram A, Razandi M, O’Mahony F, Lubahn D,Levin ER. Estrogen Receptor-{beta} PreventsCardiac Fibrosis. Molecular Endocrinology. 2010;24:2152–2165. [PubMed: 20810711].
- Knowlton AA and Lee AR. Estrogen and theCardiovascular System. Pharmacol Ther. 2012 July; 135(1): 54–70.doi:10.1016/j.pharmthera.2012.03.007.
- Geelen G, Laitinen T, Hartikainen J, Bergstrom K,Niskanen L. Gender influence on vasoactivehormones at rest and during a 70 degree head-uptilt in healthy humans. J Appl Physiol 92: 1401–1408, 2002. [PubMed: 11896003].
- Hammond IW, Devereux RB, Alderman MH,Laragh JH. Relation of blood pressure and bodybuild to left ventricular mass in normotensive andhypertensive employed adults. J Am Coll Cardiol12: 996–1004, 1988. [PubMed: 3417996].
- Lentner C (editor). Geigy Scientific Tables (8th ed.).Basel, Switzerland:Ciba-Geigy, vol. 3, 1982.21.
- Homan TD, Bordes S, Cichowski E. Physiology,Pulse Pressure. [Updated 2020 Apr 28]. In:StatPearls [Internet]. Treasure Island (FL):StatPearls Publishing; 2020 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK482408/.
- Fleg JL. Age-associated changes in cardiovascularstructure and function: a fertile milieu for futuredisease. Heart Fail Rev. 2012 September ; 17(0):545–554.
- Segan R, Gupta V, Walia L, Mittal N. Rate pressureproduct predicts Cardiovascular risk in type 2Diabetics with cardiac autonomic neuropathy. NatlJ Physiol Pharm Pharmacol 2013; 3:43-47.
- DeMarco VG, Aroor AR and Sowers JR. Thepathophysiology of hypertension in patients withobesity. Nat Rev Endocrinol. 2014 June ; 10(6):364–376. doi:10.1038/nrendo.2014.44.
- Vallon V, Richter K, Blantz RC, Thomson S,Osswald H. Glomerular hyperfiltration inexperimental diabetes mellitus: potential role oftubular reabsorption. J Am Soc Nephrol. 1999;10:2569–2576. [PubMed: 10589696].
- Kurukulasuriya LR, Stas S, Lastra G, Manrique C,Sowers JR. Hypertension in obesity. Med ClinNorth Am. 2011; 95:903–917. [PubMed:21855699].
- Stenmark KR, et al. The adventitia: essentialregulator of vascular wall structure and function.Ann Rev Physiol. 2013; 75:23–47. [PubMed:23216413].
- Sehgel NL, et al. Increased vascular smoothmuscle cell stiffness; a novel mechanism for aorticstiffness in hypertension. Am J Physiol Heart CircPhysiol. 2013; 305:H1281–H1287. [PubMed:23709594].
- Rumantir MS, et al. Neural mechanisms in humanobesity-related hypertension. J Hypertens. 1999;17:1125–1133. [PubMed: 10466468]).
- Raven, P. B., Fadel, P. J., and Ogoh, S. (2006).Arterial baroreflex resetting during exercise: acurrent perspective. Exp. Physiol. 91, 37–49. doi:10.1113/expphysiol.2005.032250.
- Jaju DS, Dikshit MB, Purandare VR and Raje S.Heart rate and blood pressure responses of lefthandersAnd right-handers to autonomic stressors.Indian j physiol pharmacol 2004; 48 (1) : 31–40.
- Egger JW (2008) Grundlagen der ‘‘Psychosomatik’’- Zur Anwendung des biopsychosozialenKrankheitsmodells in der Praxis. PsychologischeMedizin 19: 12–22.
- Rozanski A, Kubzansky LD (2005) Psychologicfunctioning and physical health: a paradigm offlexibility. Psychosom Med 67 Suppl 1: S47–53.
- Rowell, L. B. (1974). Human cardiovascularadjustments to exercise and thermal stress.Physiol. Rev. 54, 75–159.
- Dampney RAL (2017) Resetting of the BaroreflexControl of Sympathetic Vasomotor Activity duringNatural Behaviors: Description and ConceptualModel of Central Mechanisms. Front. Neurosci.11:461. doi: 10.3389/fnins.2017.00461.
- Rowell, L. B., and O’Leary, D. S. (1990). Reflexcontrol of the circulation during exercise:chemoreflexes and mechanoreflexes. J. Appl.Physiol. 69, 407–418.
- Trapp M, Trapp E-M, Egger JW, Domej W, SchillaciG, et al. (2014) Impact of Mental and PhysicalStress on Blood Pressure and Pulse Pressureunder Normobaric versus Hypoxic Conditions.PLoS ONE 9(5): e89005.doi:10.1371/journal.pone.0089005.
- Sherwood A, Dolan CA, Light KC (1990)Hemodynamics of blood pressure responses duringactive and passive coping. Psychophysiology 27:656–668.
- Al-Dubai SA, Al-Naggar RA, Alshagga MA, RampalKG. Stress and coping strategies of students in amedical faculty in Malaysia. Malays J Med Sci.2011.
- Gerin W, Davidson KW, Christenfeld NJ, et al. Therole of angry rumination and distraction in bloodpressure recovery from emotional arousal.Psychosom Med. 2006; 68:64–72. [PubMed:16449413].
- Dampney, R. A. L. (2015). 2013 Carl ludwigdistinguished lectureship of the APS neural controland autonomic regulation section: centralmechanisms regulating coordinated cardiovascularand respiratory function during stress and arousal.Am. J. Physiol. 309, R429–R443. doi:10.1152/japplphysiol.01227.2010.
- McEwen BS. Protective and damaging effects ofstress mediators. N Engl J Med. 1998; 338:171–179. [PubMed: 9428819].
- Light KC, Girdler SS, Sherwood A, et al. Highstress responsivity predicts later blood pressureonly in combination with positive family history andhigh life stress. Hypertension. 1999; 33:1458–1464.[PubMed: 10373233].
- Ryan MJ. An update on immune system activationin the pathogenesis of hypertension. Hypertension.2013; 62:226–230. [PubMed: 23734005].