Role of copper in type 2 diabetes mellitus: a mini-review
Автор: Shirur Varsha, Dhone Swati Kale, Shah Shreyas, Sinha Anamika, Sachdev Sanpreet Singh
Журнал: Журнал стресс-физиологии и биохимии @jspb
Статья в выпуске: 3 т.20, 2024 года.
Бесплатный доступ
Diabetes Mellitus (DM) presents a significant global health challenge, with escalating prevalence rates and associated morbidity and mortality. Despite medical advancements, the mortality rates continue to rise, necessitating a deeper understanding of the pathophysiology and potential therapeutic targets. Copper, a vital trace element, plays an important role in various metabolic processes and homeostatic functions within the human body. Dysregulation of copper metabolism has been implicated in the pathogenesis and progression of DM, contributing to oxidative stress, insulin resistance, altered glycemic control, and metabolic abnormalities. The present review provides an illustrative overview of the role of copper in DM, elucidating its impact on oxidative stress, insulin resistance, glycemic control, and metabolic disturbances.
Diabetes, hyperglycemia, metabolic disorders, trace elements, insulin resistance
Короткий адрес: https://sciup.org/143182800
IDR: 143182800
Текст обзорной статьи Role of copper in type 2 diabetes mellitus: a mini-review
Diabetes Mellitus is a cause of global concern In the global adult population. India is rightly known as the global hub for diabetes, owing to the high prevalence rate reported across various studies. A significantly high morbidity and mortality rate is associated with the disorder owing to its tendency to cause damage to various organs including arteries, heart, kidneys, brain, nerves, and retina (Fujita et al. , 2013).
A recent World ealth Organization (W O) estimate reported that DM accounts for more than 2 million deaths on a global scale and there has been a 3% rise in the mortality rates associated with diabetes despite advancements in medicine (Ong et al. , 2023). Numerous bio-molecules and pathways are involved in the pathogenesis process of the disease. To tackle the pathology, however, it is imperative to understand the physiological regulatory processes of blood glucose and insulin. Among the many regulatory parameters, an important association between blood glucose levels, DM, and copper levels in the body (Naka et al. , 2103; Samadi et al. , 2020).
Pathophysiology of Copper:
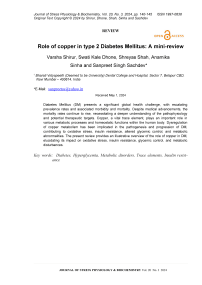
Copper is a trace element present in various organs such as the liver, brain, and bones as well as in relatively lesser concentrations in the heart, pancreas, and kidneys (Jomova et al. , 2022). The copper element acts as a co-factor in various metabolic reactions and plays a pivotal role in the homeostasis processes of the human body (Figure 1). The intake of copper is generally adequate owing to its abundance in the normal diet (Lelièvre et al. , 2020). It binds to albumin in the liver after being absorbed and transported from the gastrointestinal system. The circulation of copper in the bloodstream occurs in conjunction with ceruloplasmin (Maung et al. , 2021). A copper membrane transporter-1 (CMT-1) protein aids in the transport of the element inside the cells and binds it to metallothioneins (Mandal et al. , 2020). Both CMT-1 and metallothioneins are found abundantly in the liver cells, and ultimately the excretion of copper occurs in bile.
Inadequate dietary copper leads to increased production of free radicals, alkaline phosphatase activity, and cytotoxicity (Davis 2003). Zinc may act as a competitor for the absorption of copper in the small intestine and hence, at times, copper deficiency may be pronounced in individuals with high zinc supplementation (Freeland et al., 2020). Owing to the ability of ceruloplasmin to oxidize iron, a deficiency of copper may lead to the development of symptoms of iron deficiency anemia (Moon et al., 2021).
Ceruloplasmin acts as a chelating agent and absorbs almost 90% of the copper in the blood and the excess of Cu returns to the liver to be excreted into the bile duct through ATP7B, the second human Cu(I)-ATPase (Linder et al. , 2020). The toxicity of copper facilitates the formation of reactive oxygen species by acting as a prooxidant which may, in turn, cause cell death. This leads to the development of various diseases including Alzheimer’s disease, osteoarthritis, and cardiomyopathy (Philbert eta l., 2022; Cui et al. , 2022).
Copper and Type 2 Diabetes Mellitus:
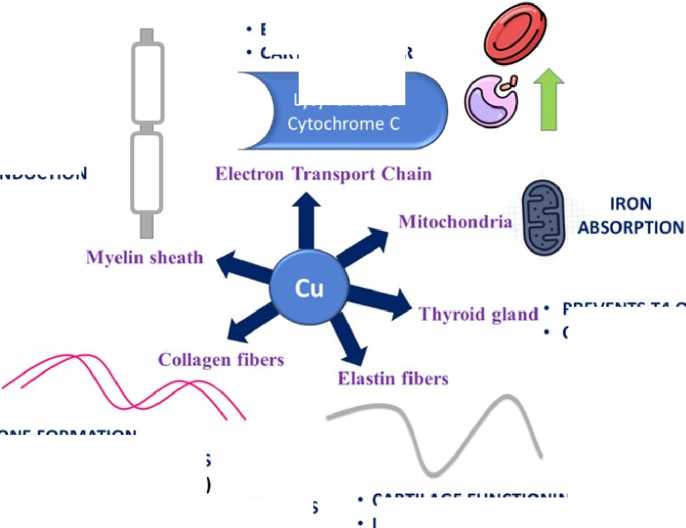
Copper dysregulation contributes to oxidative stress, insulin resistance, altered glycemic control, and metabolic abnormalities in DM through various mechanisms (Figure 2).
Oxidative Stress in DM : Oxidative stress, arising from an imbalance between reactive oxygen species (ROS) production and antioxidant defense mechanisms, plays a pivotal role in DM progression (Singh et al. , 2022; Jomova et al. , 2023). Copper, along with zinc, serves as a cofactor for antioxidant enzymes such as superoxide dismutase (SOD), mitigating ROS-induced damage (Rosa et al. , 2021; Chidambaram et al. , 2024). Dysregulation of copper-dependent antioxidant systems exacerbates oxidative stress, leading to endothelial dysfunction, β-cell damage, and insulin resistance in DM. Tanaka et al. , (2009) demonstrated increased ROS levels in DM patients, implicating copper-mediated oxidative stress in disease pathogenesis. Copperchelating agents reduce ROS by excreting through the cell in bound forms, highlighting the role of Cu in the pathogenesis of DM (Singh et al. , 2022; Jomova et al. , 2023).
Copper and Insulin Resistance: Insulin resistance, a hallmark feature of DM, is exacerbated by disruptions in copper homeostasis. Excess copper accumulation promotes ROS generation and impairs insulin signalling pathways, leading to diminished glucose uptake and utilization by peripheral tissues (Zhang et al., 2021; Badran et al., 2016). Furthermore, copper toxicity potentiates lipid peroxidation and inflammatory cytokine production, further exacerbating insulin resistance (Caturano et al., 2023). The generation of copper-induced oxidative stress in DM highlights its role in insulin resistance and metabolic dysfunction (González-Domínguez et al., 2022).
Copper and Glycemic Control: Disturbances in copper levels have been implicated in altered glycemic control in DM. Elevated copper levels stimulate glycation reactions and ROS-mediated damage to pancreatic β-cells, impairing insulin secretion and exacerbating hyperglycemia (Kant et al., 2021). Conversely, copper deficiency compromises glucose tolerance and exacerbates diabetic complications. An association between elevated copper levels and impaired glycemic control in DM patients has been found, underscoring the importance of copper homeostasis in metabolic regulation ( asano et al., 2020).
Copper and Metabolic Abnormalities : Metabolic dysregulation in DM influences trace element metabolism, including copper. Lower copper levels in DM patients have been reported, suggesting a role for copper in metabolic disturbances (Almajdoub et al. , 2023; Bjørklund et al. , 2020). Conversely, copper excess contributes to mitochondrial dysfunction and ROS overproduction, perpetuating metabolic abnormalities in DM (Ruiz et al. , 2021). Mazi et al. (2020) highlighted the implications of copper dysregulation in lipid and protein metabolism, underscoring its role in DM progression (Zhang et al. , 2021).
NEURAL CONDUCTION
-
• INNATE IMMUNITY
-
• ERYTHROPOIESIS BODY GROWTH CARTILAGE REPAIR
PREVENTS T4 OVERABSORPTION CONTROLS CALCIUM LEVELS
Lysyl oxidase
-
• BONE FORMATION
-
• INTEGRITY OF MEMBRANES (Basement and Endothelial)
-
• MAINTENANCE OF SKIN, BLOOD VESSELS AND CONNECTIVE TISSUE
CARTILAGE FUNCTIONING
INTEGRITY OF CELL MEMBRANES
Figure 1: Role of copper in various homeostatic functions
Figure 2: Dysregulation of copper-zinc-superoxide dismutase system leading to Diabetes mellitus
CONCLUSION
Copper emerges as a key player in the pathogenesis and progression of Type 2 Diabetes Mellitus. Dysregulated copper homeostasis contributes to oxidative stress, insulin resistance, altered glycemic control, and metabolic abnormalities in DM patients. Targeting copper metabolism may offer novel therapeutic avenues for managing DM and mitigating its complications. Further research is warranted to elucidate the precise mechanisms underlying copper-mediated metabolic dysfunction in DM and explore potential interventions targeting copper homeostasis for improved clinical outcomes.
CONFLICTS OF INTEREST
The authors declare that they have no potential conflicts of interest.
Список литературы Role of copper in type 2 diabetes mellitus: a mini-review
- Almajdoub, A. A., Alzwayi, M. M., & Alaasswad, N. M. (2023). Estimated Blood Levels of Zinc and Copper Among Type-2 Diabetic Patients and Their Relationship to Insulin Resistance. Wadi Alshatti University Journal of Pure and Applied Sciences, 9-15.
- Badran, M., Morsy, R., Soliman, H., & Elnimr, T. (2016). Assessment of trace elements levels in patients with type 2 diabetes using multivariate statistical analysis. Journal of Trace Elements in Medicine and Biology, 33, 114-119.
- Bj0rklund, G., Dadar, M., Pivina, L., Doça, M. D., Semenova, Y., & Aaseth, J. (2020). The role of zinc and copper in insulin resistance and diabetes mellitus. Current medicinal chemistry, 27(39), 6643-6657.
- Caturano, A., D'Angelo, M., Mormone, A., Russo, V., Mollica, M. P., Salvatore, T..... & Sasso, F. C. (2023). Oxidative stress in type 2 diabetes: impacts from pathogenesis to lifestyle modifications. Current Issues in Molecular Biology, 45(8), 66516666.
- Chidambaram, S. B., Anand, N., Varma, S. R., Ramamurthy, S., Vichitra, C., Sharma, A., ... & Essa, M. M. (2024). Superoxide dismutase and neurological disorders. IBRO Neuroscience Reports, 16, 373-394.
- Cui, X., Wang, Y., Liu, H., Shi, M., Wang, J., & Wang, Y. (2022). The molecular mechanisms of defective copper metabolism in diabetic cardiomyopathy. Oxidative Medicine and Cellular Longevity, 2022.
- Davis, C. D. (2003). Low dietary copper increases fecal free radical production, fecal water alkaline phosphatase activity and cytotoxicity in healthy men. The Journal of nutrition, 133(2), 522-527.
- Freeland-Graves, J. H., Sachdev, P. K., Binderberger, A. Z., & Sosanya, M. E. (2020). Global diversity of dietary intakes and standards for zinc, iron, and copper. Journal of Trace Elements in Medicine and Biology, 61, 126515.
- Fujita, T., Hemmi, S., Kajiwara, M., Yabuki, M., Fuke, Y., Satomura, A., & Soma, M. (2013). Complement-mediated chronic inflammation is associated with diabetic microvascular complication. Diabetes/metabolism research and reviews, 29(3), 220-226.
- González-Domínguez, Á., Millán-Martínez, M., Domínguez-Riscart, J., Mateos, R. M., Lechuga-Sancho, A. M., & González-Domínguez, R. (2022). Altered metal homeostasis associates with inflammation, oxidative stress, impaired glucose metabolism, and dyslipidemia in the crosstalk between childhood obesity and insulin resistance. Antioxidants, 11(12), 2439.
- Hasanato, R. M. (2020). Trace elements in type 2 diabetes mellitus and their association with glycemic control. African Health Sciences, 20(1), 287-293.
- Jomova, K., Makova, M., Alomar, S. Y., Alwasel, S. H., Nepovimova, E., Kuca, K..... & Valko, M. (2022). Essential metals in health and disease. Chemico-biological interactions, 367, 110173.
- Jomova, K., Raptova, R., Alomar, S. Y., Alwasel, S. H., Nepovimova, E., Kuca, K., & Valko, M. (2023). Reactive oxygen species, toxicity, oxidative stress, and antioxidants: Chronic diseases and aging. Archives of toxicology, 97(10), 2499-2574.
- Kant, R., Verma, V., Patel, S., Chandra, R., Chaudhary, R., Shuldiner, A. R., & Munir, K. M. (2021). Effect of serum zinc and copper levels on insulin secretion, insulin resistance and pancreatic p cell dysfunction in US adults: findings from the National Health and nutrition examination survey (NHANES) 2011-2012. Diabetes Research and Clinical Practice, 172, 108627.
- Leliévre, P., Sancey, L., Coll, J. L., Deniaud, A., & Busser, B. (2020). The multifaceted roles of copper in cancer: A trace metal element with dysregulated metabolism, but also a target or a bullet for therapy. Cancers, 12(12), 3594.
- Linder, M. C. (2020). Copper homeostasis in mammals, with emphasis on secretion and excretion. A review. International journal of molecular sciences, 21(14), 4932.
- Maung, M. T., Carlson, A., Olea-Flores, M., Elkhadragy, L., Schachtschneider, K. M., Navarro-Tito, N., & Padilla-Benavides, T. (2021). The molecular and cellular basis of copper dysregulation and its relationship with human pathologies. The FASEB Journal, 35(9), e21810.
- Mandal, T., Kar, S., Maji, S., Sen, S., & Gupta, A. (2020). Structural and functional diversity among the members of CTR, the membrane copper transporter family. The Journal of membrane biology, 253, 459-468.
- Mazi, T. A., Shibata, N. M., & Medici, V. (2020). Lipid and energy metabolism in Wilson disease. Liver research, 4(1), 5-14.
- Moon, N., Aryan, M., Westerveld, D., Nathoo, S., Glover, S., & Kamel, A. Y. (2021). Clinical manifestations of copper deficiency: a case report and review of the literature. Nutrition in Clinical Practice, 36(5), 1080-1085.
- Naka, T., Kaneto, H., Katakami, N., Matsuoka, T. A., Harada, A., Yamasaki, Y..... & Shimomura, I. (2013). Association of serum copper levels and glycemic control in patients with type 2 diabetes. Endocrine journal, 60(3), 393-396.
- Ong, K. L., Stafford, L. K., McLaughlin, S. A., Boyko, E. J., Vollset, S. E., Smith, A. E..... & Brauer, M. (2023). Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. The Lancet, 402(10397), 203-234.
- Philbert, S. A., Schönberger, S. J., Xu, J., Church, S. J., Unwin, R. D., & Cooper, G. J. (2022). Elevated hippocampal copper in cases of type 2 diabetes. EBioMedicine, 86.
- Rosa, A. C., Corsi, D., Cavi, N., Bruni, N., & Dosio, F. (2021). Superoxide dismutase administration: A review of proposed human uses. Molecules, 26(7), 1844.
- Ruiz, L. M., Libedinsky, A., & Elorza, A. A. (2021). Role of copper on mitochondrial function and metabolism. Frontiers in molecular biosciences, 8, 711227.
- Samadi, A., Isikhan, S. Y., Tinkov, A. A., Lay, I., Do§a, M. D., Skalny, A. V..... & Bj0rklund, G. (2020). Zinc, copper, and oxysterol levels in patients with type 1 and type 2 diabetes mellitus. Clinical nutrition, 39(6), 1849-1856.
- Singh, A., Kukreti, R., Saso, L., & Kukreti, S. (2022). Mechanistic insight into oxidative stress-triggered signaling pathways and type 2 diabetes. Molecules, 27(3), 950.
- Tanaka, A., Kaneto, H., Miyatsuka, T., Yamamoto, K., Yoshiuchi, K., Yamasaki, Y..... & Matsuhisa, M. (2009). Role of copper ion in the pathogenesis of type 2 diabetes. Endocrine journal, 56(5), 699-706.
- Zhang, J., Duan, D., Song, Z. L., Liu, T., Hou, Y., & Fang, J. (2021). Small molecules regulating reactive oxygen species homeostasis for cancer therapy. Medicinal Research Reviews, 41(1), 342-394.