Telemedicine in modern conditions: the attitude of society and the vector of development
Автор: Medvedeva Elena I., Aleksandrova Olga A., Kroshilin Sergei V.
Журнал: Economic and Social Changes: Facts, Trends, Forecast @volnc-esc-en
Рубрика: Social and economic development
Статья в выпуске: 3 т.15, 2022 года.
Бесплатный доступ
The intensive development of information technology and the external challenges, primarily the coronavirus pandemic, have caused a revision of attitudes toward telemedicine. The article is devoted to the study of problems concerning the development of Russian telemedicine, analysis of existing trends and the possibilities of its application, taking into account the development of communication technology and the legal field. Research on this issue is connected, on the one hand, with analyzing modern capabilities of telemedicine technologies and the need for their application in connection with the complex epidemiological situation in a number of Russia’s regions, on the other hand, with the assessment of the level of trust in telemedicine on the part of end users: who, how, when and where can use telemedicine services. The object of our research is telemedicine technology, the subject is the dynamics of perception of new forms of medical services by Russian society. We use a classical approach to studying the problems under consideration: at the first stage, we conduct a comprehensive desk study and analyze secondary information; at the second stage, we collect primary data: on the basis of the developed tools, we conduct an exploratory study of the attitude of Russian society toward telemedicine. The uniqueness and novelty of our findings are due to the comparison of the data concerning the attitude of Russians toward telemedicine, obtained before the outbreak of the pandemic, with the data obtained at the stage of a significant reduction in the incidence of COVID-19 in regions that have become “pilot” ones in the use of telemedicine technologies in primary care in the midst of the epidemic. During data collection and analysis, we applied statistical, mathematical and sociological methods, including content analysis to study legal issues of the possibility of using telemedicine technologies. The study has revealed the main reasons for Russians’ distrust of telemedicine, as well as possible ways and areas of its application in the future to provide medical care to the population. The results obtained can be used to study the application of telemedicine in Russia in the system of training and retraining of medical personnel, as well as by health care organizers, lawyers and other specialists who deal with the application of telemedicine technologies, including at the level of legislative and executive authorities.
Quality of life, healthcare organization, telemedicine, telemedicine technologies, attitude toward telemedicine, covid-19 pandemic, medical care, legal foundations of telemedicine
Короткий адрес: https://sciup.org/147238049
IDR: 147238049 | УДК: 330.16, | DOI: 10.15838/esc.2022.3.81.11
Текст научной статьи Telemedicine in modern conditions: the attitude of society and the vector of development
Nowadays, telemedicine technology is an integral part of healthcare delivery to the population around the world1, enabling people to have equal access to medicine. The active use of information technology (IT) in the work of medical institutions in providing medical services to the population in primary care has practically become a standard in most countries of the world. The use of such technologies is actively developing in Russia as well. Online medical appointment booking, virtual queue management system, and other IT advances are already being used in Russian polyclinics. The main goal of this direction is to improve the quality of patient care and increase the efficiency of medical personnel, as well as to reduce the cost of medical services.
The demand for telecommunication technology has increased significantly during the COVID-19 pandemic because of the possibility to provide remote patient care and consultation. At the present stage, telemedicine allows many other things: advanced diagnosis and treatment of a whole range of diseases, remote biomonitoring, which is in demand not only among the older generation, which usually has several chronic diseases, but also among young people, who are increasingly using electronic gadgets to monitor health and diagnose the main indicators of vital functions. In the midst of the pandemic, there were cases where a smart watch saved a person’s life by detecting a decrease in blood saturation, thus contributing to the early diagnosis of COVID-19.
Obviously, legal, moral and ethical aspects play an important role in the application of telemedicine technologies in modern conditions. First of all, it is the legal framework, which should provide legitimacy and a legal basis for the use of information concerning the results of tests, indicators taken with medical equipment, etc., which ultimately have an impact on the most important thing – the diagnosis. One question that arises is who will be responsible for making such decisions (as in all other systems that now use elements of “artificial intelligence”, such as self-driving cars, decisionmaking systems, electronic consultants (Kim et al., 2018), expert evaluations (Morozov et al., 2018), etc.)? It is very important at all stages of information processing to ensure information security (doctor-patient privilege) and confidentiality of personal information in accordance with the law. Obviously, electronic communication “doctor – patient” should be carried out through secured communication channels, using special systems with certified and guaranteed security (Zingerman et al., 2017). The purpose of this paper is to identify the dominant factors contributing to the active development of telemedicine technologies in the world, as well as to assess the corresponding trends in Russia.
The article presents the results of a comprehensive study and analysis of the specifics of trends in the use of telemedicine technologies in the world and in the Russian healthcare system, as well as the data that we received during a primary sociological study, the purpose of which was to study the prospects for the development of telemedicine in Russian conditions. The main objective of the research is to analyze the current capabilities of telemedicine technologies, as well as the features and necessity of their use in connection with the current epidemiological situation. The first stage included an analysis not only of trends in the development of telemedicine, but also of the confidence level in it on the part of end users. The second stage involved a comparative analysis of empirical data obtained earlier (before the pandemic) with the results of the author’s primary research conducted in a number of Russia’s regions using the developed tools.
The main objective of the reconnaissance study is to determine the attitudes of different age groups of Russians toward the use of telemedicine technologies in selected regions: Moscow, large and medium-sized cities in the southeast of the Moscow Oblast, and Ryazan. The choice of regions was primarily based on the capabilities of telemedicine technology implementation, as well as on the position of leaders in the organization of COVID-19 response measures. For example, some polyclinics in the Moscow Oblast were forced to move to a remote work with patients during the outbreak of the Omicron virus variant (this was the first time such a measure had been used in Russia).
The uniqueness and novelty of the work are due to the possibility of comparing data on the attitudes of Russians toward telemedicine, obtained before the pandemic, with indicators of the declining trend of COVID-19 incidence.
Theoretical review and experience of telemedicine application
Despite the fact that the history of telemedicine technology in the world goes back more than 120 years (Bashshur, Shannon, 2009), current trends, challenges, and especially the development of information and communication technology are forcing a new perspective on many issues.
A.V. Vladzimirskii has played a major role in studying the history, trends, and key factors in the development of telemedicine in the world and Russia. In his numerous works, he has covered the entire spectrum of issues related to this phenomenon (Vladzimirskii, 2017; Vladzimirskii, 2019; Vladzimirskii et al., 2019; Vladzimirskii et al., 2020 et al.). Yu.D. Volynsky considered telemedicine as a part of the information society (Volynskii, 1999), A.I. Grigor’ev, O.I. Orlov, and V.A. Loginov studied the specifics of clinical telemedicine (Grigorev et al., 2001). N.A. Voskolovich gave examples of telemedicine implementation in terms of development of paid services (Voskolovich, 2021). I.A. Zheleznyakova, T.A. Khelisupali, V.V. Omel’yanovskii, and S.N. Tishkina analyzed the adaptation of foreign experience in providing telemedicine services in Russia (Zheleznyakova et al., 2020), and B.V. Zingerman, N.E. Shklovski-Kordi, and A.I. Vorob’ev analyzed features of telemedicine implementation of the “patient – doctor” concept (Zingerman et al., 2017). All of the above-mentioned authors investigated particular areas or specific issues related to the features of the application of such technologies in Russia. Foreign experts focused their attention on applied issues. For example, R.L. Bashshur and G.W. Shannon dealt with the history of telemedicine and the problems of its transformation (Bashshur, Shannon, 2009); N. Charrier, K. Zarca, I. Durand-Zaleski, and C. Calinaud investigated the cost effectiveness and accessibility of telemedicine care to the population (Charrier et al.); D. Giansanti, S. Morelli, V. Macellari, A.G. Ekeland, and A. Grittlund evaluated telemedicine technologies and proposed tools for a quality control system for medical services. The issues of telemedicine quality were also addressed by Russian scientists A.V. Vladzimirskii, S.P. Morozov, S.S. Simenyura, who during the COVID-19 pandemic published several articles on quality assessment of telemedicine consultations. All of these materials were specific in nature, examining a narrow problem in a particular time period. Our article takes a more comprehensive approach.
Currently, we can consider telemedicine to be a conventional term accepted in the academic community (Weinstein, 2018). Telemedicine (from a Greek tele – distance and a Latin meder – to heal), according to a number of scientists, is “... a health care tool that uses telecommunications and electronic information (computer) technology to provide medical care and services at the point of need (where the geographical distance between the health care provider and the patient is a critical factor)” (Vladzimirskii, Lebedev, 2018). At the present stage, the main direction in the development of telemedicine is the implementation of a “patient – doctor” communication system, which can include online consultations, home telemedicine, and remote biomonitoring. There is clinical remote interaction between medical organizations (Kamaev, 2001) and/or individual authorized medical workers (doctors, nurses) (Yarasheva et al., 2020) using telemedicine technology.
Telemedicine in Russian healthcare is also seen as a certain component of information support in the medical field. Such technologies are designed to ensure the realization of the constitutional right of any Russian citizen to receive medical care (Levanov et al., 2017). It is also a modern tool that is used when the state creates conditions for effective and affordable health care for Russians in accordance with constitutional rights (Stolbov, 2015). In isolation, this is also relevant in megalopolises: when accompanying elderly patients, as well as patients with chronic diseases. In this case, telemedicine technology can minimize risks and threats to health conditions and make more efficient use of health care resources (Charrier et al., 2016). Medical videoconferencing, teleconsultations, and teleseminars are becoming available to physicians to conduct any form of consultation and training through the use of information and telecommunication technologies (Zheleznyakova et al., 2020).
Research methodology
Our approach to the study of telemedicine application problems in modern conditions, as well as in the study of societal attitudes toward the possibility of applying new technologies in medicine, is based on the classical variant of sociological research. The design of the data acquisition framework includes two stages: the first is desk research of the analysis results of secondary information on the vectors of telemedicine development, as well as societal attitudes toward using of telemedicine technologies in the provision of medical services in the world and Russia, including during the coronavirus pandemic. The information base consists of Rosstat data, analytical materials, reports of the Ministry of Health of the Russian Federation, international health statistics data, monitoring of health indicators in the framework of the WHO Sustainable Development Goals, the results of research by public organizations.
The second stage is a primary sociological study, the main purpose of which was to examine the attitudes of different age groups of Russians toward the use of telemedicine technologies. We collected primary data using a questionnaire on Google-Forms. For the survey we used the CAWI (Computer Assisted Web Interviewing) method – a computer-based survey without the interviewer’s personal presence, when the respondent fills out the questionnaire on their own. A total of 252 respondents completed the survey. The sample is quota based on age distribution. According to experts, sampling error in such an organization of the survey meets the requirements of representativeness. Scope of the study: Moscow, cities of the southeast of the Moscow Oblast (Kolomna, Voskresensk, Egoryevsk, Lukhovitsy, Ozyory, Zaraisk), Ryazan. The cities represented can be called typical in terms of telemedicine technology capabilities and leading in terms of organizing the new infectious diseases response (in this case, COVID-19). Some polyclinics in the Moscow Oblast were forced to switch to a remote work with patients during the surge of new COVID-19 (Omicron) strains due to the current epidemiological situation (this was the first time such a measure had been used in Russia).
The survey was conducted in March 2022, a time when the downward trend of the COVID-19 pandemic can already be observed. The distribution of respondents by gender is slightly skewed toward the predominance of women (56.4%). It is well known that this part of the respondents is traditionally more attentive to their health and to making decisions concerning treatment for themselves and their family members. For the convenience of further analysis, we divided respondents into four age groups: I – 14 to 18 years old (9.5% of all respondents), II – 19–29 years old (35.4%), III – 30–49 years old (42.3%), and IV – over 50 years old (12.8%). Previously, the respondents had no experience with the use of telemedicine technologies or had encountered only some elements of information technologies when receiving medical services. In addition, those interviewed were not medical or nursing professionals, ensuring that there was no professionally based bias in the responses.
Initially, we put forward two hypotheses: first, whether Russian society, due to the spread of coronavirus disease and the introduction of restrictive “self-isolation” measures, would trust telemedical technologies. Second, whether the younger generation is more inclined to use information telemedicine technologies than people of older age, since they have more experience in using information and communication technologies in everyday life.
Results of the desk research
Currently there is a significant growth in the volume of the telemedicine services market in
Figure 1. Dynamics of the telemedicine services market volume in the Russian Federation, 2015–2019

□ Volume of the telemedicine market in the RF, million rubles
□ Growth rate of market volume to the previous year, %
Source: There is significant growth in the volume of the telemedicine market in Russia. Magazin issledovanii. RBK. Available at: (accessed: March 10, 2022).
Russia. But analysts, medics, statistical services, and the Ministry of Health have different approaches to its assessment. Some take as a basis only paid medical services provided on the basis of telemedicine technologies; others take into account the costs of purchasing equipment for communications and maintaining information and communication technologies, its implementation and support of medical institutions; others calculate the market potential and proceed from the real and projected need for such direction of medical development under the influence of external challenges, such as a pandemic. In this regard, estimates vary.
One of the options for calculating the dynamics of the market for telemedicine services in Russia is shown in Figure 1 .
The above estimate was made by analysts at GidMarket on the basis of data from Russian statistics, expert estimates in the field of telemedicine and data from Mobile Medical Technologies LLC. According to these calculations, the market volume in 2019 (before the pandemic) was 4.4 billion rubles. The growth relative to the previous year is 18%. The largest increase relative to the previous year one can observe in 2016 – almost a thousand and a half percent. Over the entire period presented, there is a noticeable upward trend in the volume of the telemedicine technology market (in current prices)2.
In Russia, the telemedicine market, as well as throughout the world3, has become extremely important in the era of the COVID-19 pandemic. Investments in this area have skyrocketed. According to experts from VEB Ventures, given on the analytical portal CNews, in the next few years, the average annual growth of telemedicine market can be about 100%4 (Fig. 2).
Figure 2. Forecast of telemedicine market dynamics in Russia, billion rubles
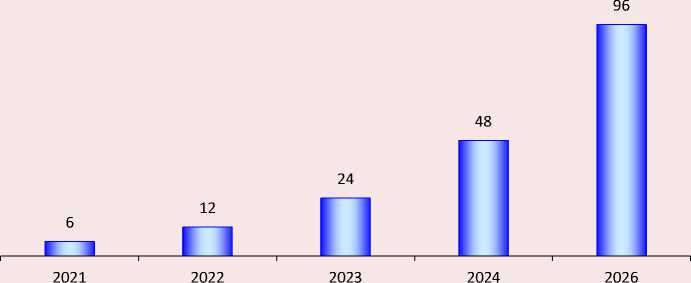
Source: CNews based on VEB Venteres data, 2020; IT in healthcare 2020. Analytical data of the C-News portal. Available at: (accessed: March 10, 2022).
Despite visible changes, the Russian telemedicine market is at the stage of sluggish growth. The introduction of telemedicine in other countries began much earlier. Not only the availability of funding channels (private clinics and medical institutions, insurance companies, etc.), but also a significant advance in the field of communications and the development of information technology contributed to this. For example, in the USA, about 70% of insurance companies offer telemedicine services because they save 30 to 40% of money. According to U.S. experts (Ekeland, Grittlund, 2015; Kidholm et al., 2017; Halpren-Ruder et al., 2019), telemonitoring of patients with chronic conditions can reduce costs by nearly twice as much as possible hospitalization for similar surveillance.
In 2021 the specialists of Romir Holding studied the attitudes of Russians toward telemedicine as part of an initiative survey. Only a quarter of Russian citizens (26%) are familiar with such a system of online consultations, 42% have a rough idea, and a third knows nothing about telemedicine ( Fig. 3 ).
At the height of the pandemic, in May 2020, the All-Russian Center for the Study of Public Opinion (VCIOM) conducted a telemedicine survey5. The main objective of the survey was to find out the degree of Russians’ awareness of the possibility to receive remote consultations from a doctor via the Internet or telephone and their attitude toward such consultations. More than half of the respondents (62%) were aware of the existence of telemedicine technologies and the possibility of remote consultation with a doctor. Traditionally, in the two capitals awareness of telemedicine is higher: 71% of respondents knew about the possibility to consult a doctor by phone and 73% via the Internet.
Figure 3. What telemedicine services do you know? % respondents
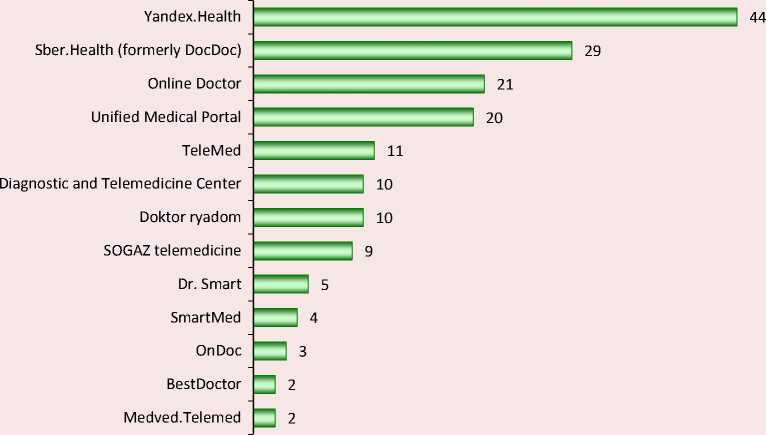
Source: Only a quarter of Russians trust telemedicine. 2020. Analytical data of the C-News portal. Available at: https://romir. ru/studies/lish-chetvert-rossiyan-doveryaet-telemedicine (accessed: March 10, 2022).
There were 8% of respondents who have already had experience in receiving telemedicine services in the form of a consultation, more than half (53%) potentially considered such an opportunity for themselves. According to the VCIOM survey, overall 48% of Russians considered the possibility of visiting a doctor via Internet technologies, of which the largest proportion (57%) were young people between the ages of 18 and 24. The reasons for receiving a telemedicine consultation were as follows: if there are signs of illness – one in four; if you feel “really poorly” or, on the contrary, “nothing serious” – one in ten. The possibility of visiting a doctor remotely is also considered in a situation when there is no possibility to come in person (5%) or when “just a consultation” is needed (5%). At the same time, one-third of Russians (33%) believe that telemedicine technologies should not be used because a personal examination is “necessary when visiting a doctor”. Among respondents, 13% doubt the quality of such medical services, and one in ten believes that it is not necessary at all and it is easier to go to a regular appointment6.
During the COVID-19 pandemic, the demand for physician teleconsultation (Levanov et al., 2014) increased dramatically. Due to the difficult epidemiological situation in many regions (for example, in the city of Moscow and the Moscow Oblast), primary care for those who fell ill with COVID-19 was restructured: polyclinics were forced to switch to remote work. Additional call centers have been set up. Thus, the pandemic has further sharpened the focus on the use of information technology in healthcare. During this period there was a high demand for hardware and software solutions in the field of telemedicine. Absolutely every opportunity was used to reduce the number of face-to-face doctor-patient contacts. In February
2022, the head of the Russian Ministry of Health assessed the situation as follows: “...First of all, the load falls on the outpatient-clinic stage, and in fact 92.5% receive help exactly in polyclinics. Unprecedentedly high load, the highest load on the entire outpatient and polyclinic unit and on the system as a whole”7. At that time, the number of sick health professionals was twice as high as the number of those infected in the fall. Hence the decision on the ability of the RF constituent entities to transfer polyclinics to a remote work mode.
The problem of a shortage of equipment for information and communication exchange existed in Russian healthcare even before the pandemic began, but the sharp increase in the number of patients has greatly exacerbated it. The process of providing medical care was slowing down, which could not but affect its efficiency and quality. During this period, there was a need for services for remote patient examinations in order, among other things, to reduce the risk of infection in the doctors themselves. That is why the development of Russian healthcare at the level of the Russian Ministry of Health began to be directly linked with telemedicine technologies.
The increased demand of patients for telemedicine consultations launched the process of rapid development of this area. According to data from constituent entities of the Russian Federation, more than 1.7 million telemedicine consultations have been provided to patients diagnosed with COVID-19 or pneumonia, acute respiratory infections and influenza. More than 197,000 patients were remotely monitored using telemedicine technology. The National Medical Research Centers of the Ministry of Health of Russia have conducted more than 72,000 telemedicine consultations and consiliums on complex cases at the request of doctors of regional medical organizations. According to the data of state statistical observation according to Form No. 30 in 2020 in the constituent entities of the Russian Federation more than 567 thousand “doctor – doctor” consultations were conducted using telemedicine technologies8; more than 6.437 million “doctor – patient” consultations were conducted; more than 800,000 consultations to provide opinions on diagnostic tests; more than 1.72 million patients were on remote monitoring of their health status; the federal anesthesiology and critical care remote consultation centers conducted 27,600 telemedicine consultations on requests from the regional remote consultation centers for complex cases.
As can be seen from the report of the Ministry of Health of the Russian Federation on the results of work in 2020 and tasks for 2021, most areas of development and medical services already provided during the COVID-19 pandemic are largely related to the possibility of using telemedicine technologies. That is why the attitude of the Russian society to telemedicine is of considerable interest in the framework of research.
The main problem is related to the issue of the identity of diagnostic decisions made remotely and in-person (Vladzimirskii, 2015). There are other problematic aspects to be assessed, such as technical reliability, information security, economic feasibility and accessibility of medical care. In addition, between 2000 and 2010, many techniques began to include assessments of patient satisfaction as well as efficiency and effectiveness (Vladzimirskii, 2020).
Currently, all methods of assessing the quality of telemedicine services are divided according to the directions of telemedicine: remote “doctor – patient” consultation (Zingerman et al., 2017) and “doctor – doctor” counseling (Kobrinskii, 2016). An important step was the emergence of methodological approaches for assessing telemedicine systems (Hersh et al., 2006), which have been published in peer reviews (Hailey et al., 2002), a condition of which has been significant experience with telemedicine technologies (Bergmo, 2009). The systematization of experience and the methodological base allowed a high level of evidence, which is the most critical for public health (Aoki et al., 2003). The problem of quality assessment is complicated by the versatility of care that can be provided in the “patient – doctor” format using telemedicine technologies, and because there are risks of specificity (Halpren-Ruder et al., 2019) of the subject area of remote communication (consultation) (Wootton et al., 2011). Today there is quite a lot of research in the aspect of quality (Shi et al., 2018) and performance of telemedicine “patient – doctor” consultations (Taylor, 2005) and remote monitoring (Resneck et al., 2016), approaches to analysis methodology are systematized (Martin-Khan et al., 2011).
In addition to improving the conceptual approaches for evaluating the quality of telemedicine technologies, it is necessary to take into account the opinion of the end user of medical services. In recent years a number of studies have been conducted using sociological methods, aimed at identifying the attitudes of the Russian society toward telemedicine technologies. For example, according to the IPT Group9 (2017), about 75% of Russians positively evaluated the possibility of remote communication with a doctor as part of medical care, and 68% considered such a possibility for themselves and/or their family members in the future (Fig. 4).
Figure 4. Results of answers to the question “Do you know that it is now possible to receive telemedicine services in the Russian Federation?”, % the number of respondents
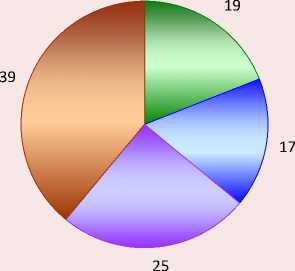
-
□ Yes, I know about such services and the decision made
-
□ I know about such services, but
I didn't know about this decision
-
□ I had heard something about such services, but did not know about such a decision
-
□ I've never heard of such a service or such a decision
Figure 5. Results of answers to the question “Please indicate to what extent do you agree with the given statements?”, %
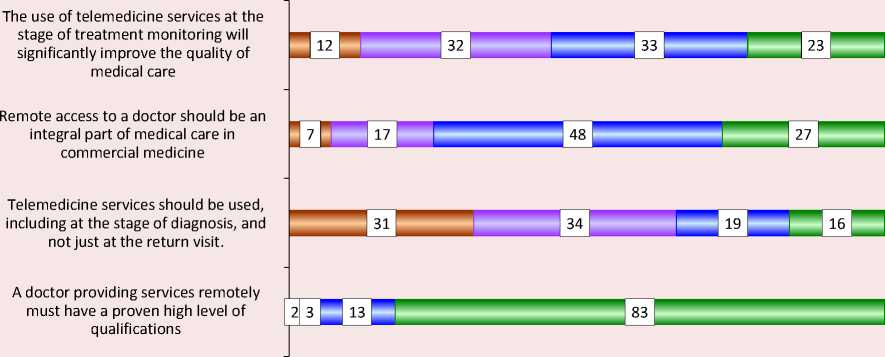
□ I do not agree □ I rather do not agree □ I rather agree □ I agree
Source: Among the population, 75% welcomes telemedicine services in commercial medicine (2017). IPT Group. Available at: https://iptg.ru/press/smi/75-naseleniya-privetstvuyut-telemeditsinskie-uslugi-v-kommercheskoy-meditsine-issledovanie-ipt-group/ (accessed: March 10, 2022).
In 2017, almost one in five (19%) Russians knew about the existence of such services, a quarter (25%) had heard something about them, and 39% had no idea about it at all (Fig. 5) .
Among those surveyed, 56% agreed and 44% disagreed with the statement that the use of telemedicine services in the monitoring stage of the treatment process would significantly improve the quality of medical care. 75% of respondents believe that remote communication with a doctor should become an integral part of medical care in commercial medicine. More than one third (35%) agree that telemedicine services can be used, including at the stage of diagnosis, and not only for return visits to the doctor. And an absolute majority of respondents (96%) agreed that a physician providing services remotely must have a proven high level of qualifications (Kroshilin et al., 2020).
In 2017, 68% of those surveyed agreed to consider using telemedicine for themselves or their family members in the next two years. At the same time, potential patients equally perceived the possibility of providing such services both in state medical institutions (41%) and in private medical clinics and centers (42%). Some respondents (17%) implied the use of telemedicine services in the format of communication (consultation) exclusively with their attending physician (a doctor they know). And 11% of respondents were ready to receive telemedicine services for a fee10.
Thus, according to the results of a study on the level of trust in telemedicine in 2017, we could say that 75% of the population is ready to use paid telemedicine services in commercial medicine, and more than 40% do not see obstacles to the use of these technologies in public health facilities.
The Romir 2021 study of Russians’ attitudes toward telemedicine showed that only 4% of respondents fully trust such technologies, a little more than one-fifth (21%) of respondents “rather trust”, 57% of respondents have no confidence in telemedicine, and every fifth Russian (19%) does not fully trust it. And 69% of Russians do not plan to use telemedicine technology for medical care in the future. Only 3% of respondents regularly use telemedicine11.
The Clinical Diagnostic and Telemedicine Research Center of the Moscow Department of Health conducted research to assess the quality of consultations with telemedicine technologies for patients with symptoms of acute respiratory infections (COVID-19) in early 2020. As an experiment, they conducted 20 consultations of simulated patients with signs of acute respiratory illness in 10 popular telemedicine services. It was found that in half of the cases, poor anamnesis (allergological – in 60% of cases, epidemiological – in 35%) was collected when providing medical services, and requesting information about chronic diseases (which posed enormous risks in terms of infection and the course of coronavirus infection) was recorded only in half of the cases. Based on the results obtained, the researchers concluded that telemedicine services did not work: they did not provide medical care at the appropriate level (in particular, in 60% of cases, medication was incorrectly prescribed). According to researchers, within the framework of the application of the considered telemedicine services in the “patient – doctor” system, their performance can be assessed as unsatisfactory (Vladzimirskii et al., 2020).
A more in-depth study of attitudes toward telemedicine was conducted by the Research Institute of Health Organization and Medical
Management of the Moscow Department of Health (NIIOZMM) in October 2019 (before the coronavirus pandemic). The survey concerned the implementation of telemedicine technologies in healthcare in Moscow. In contrast to the previously considered studies, in this case the opinion of not only patients, but also doctors was studied. From the point of view of doctors, telemedicine services are needed primarily by patients in remote regions, low-mobility patients, and parents of infants. According to doctors, remote services can be related to consultations such as nutrition or care, various observations and telemetry, as well as prescriptions and other electronic documents (Bogdan et al., 2020).
The main advantages of telemedicine technologies, according to the surveyed medical specialists, are, first, the possibility of prompt assistance (26%), second, remote assistance, which is most important for people with limited mobility (25%), and third, increased accessibility of specialists, reduced waiting time (17%). From the patients’ point of view, the use of telemedicine is acceptable for general practitioners or physicians (78%), only one-third (27%) consider the use of such technology by specialists, and 15% – by nurses. In general, everyone sees the possibilities of such services in obtaining medical reports and certificates (45%), prescriptions (39%), medical advice on the need for examination (36%), as well as in the correction of previously prescribed treatment (25%). Patients consider messengers (61%), video conferencing (45%), and dedicated apps (23%) as means of communication within telemedicine (Bogdan et al., 2020).
When examining attitudes toward telemedicine in general, the analysts at the Research Institute NIIOZM) obtained the following results (Fig. 6) .
As we can see, doctors have a significantly more positive attitude toward the possibility of using telemedicine technologies, the same applies to those who hesitate to respond: there are almost twice
-
Figure 6. Attitude toward telemedicine (patients’ and doctors’ opinions), % of respondents
Patients' Opinion

в Neutral
□ Hesitate to respond
s Positive
а Negative
Doctors' opinion
|
45 |
12 |
1 43 1 |
||
|
□ Positive |
□ Negative |
□ ЗHesitate to respond |
||
Source: Telemedicine is coming to Moscow healthcare. The Research Institute NIIOZMM. Available at: telemeditsina-prikhodit-v-moskovskoe-zdravookhranenie/?sphrase_id=65885 (accessed: March 10, 2022).
as many of them among doctors; the proportion of those who have a negative attitude toward telemedicine among patients and doctors is approximately the same (Bogdan et al., 2020).
Summarizing the secondary analysis of the data concerning the attitude of Russians to the introduction, development and spread of telemedicine technologies, we can say that among doctors more than a third speak positively, 45% of potential and actual patients agree with them; only 14% of doctors and 12% of patients do not share optimism about providing medical services in a remote mode.
Results of an exploratory sociological study
As part of our continuing study of the conditions and prospects for the use of telemedicine technologies, we conducted our own exploratory sociological study, the purpose of which was to determine the attitudes of Russians toward telemedicine.
As a result of the study, we found that 61.1% of respondents believe it is possible to use telemedicine services only for preliminary consultation; a little more than half admit the use of telemedicine technology when contacting a general practitioner or physician; one-third believe that a remote subspecialty consultation is possible. One in ten respondents did not exclude the possibility of using telemedicine to contact nursing staff (Fig. 7).
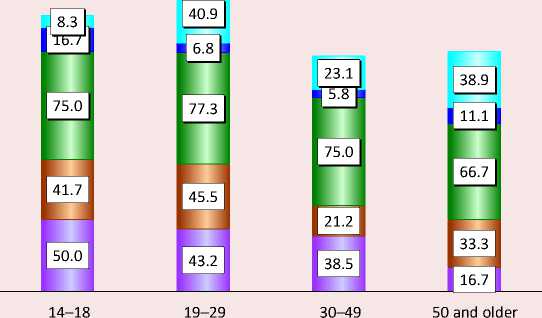
As for the influence of age, three quarters of respondents aged 19–29 recognize the use of telemedicine only for preliminary consultation. More than half of the respondents aged 50 and older agreed with them, and the same number of people in this age group indicated the possibility of remote appointment for general practitioners and physicians. It should be noted that the younger generation (14–18 years old) is less willing than others to use the possibilities of telemedicine: a third less (25%) would agree to a remote appointment with a general practitioner, even less (16.7%) would use the telemedicine opportunities to consult with a subspecialists. At the same time, young people agree to use telemedicine technologies for consultations: 75.0% of respondents in the 14–18 age group and 54.5% in the 19–29 age group said yes. The older generation (50 and older) is not prepared at all to use telemedicine when interacting with nursing staff, and this includes 5.8% of respondents aged 30–49. Younger people (19–29 years old) have less prejudice: 18.2% trust remote consultations by nurses (Fig. 8).
-
Figure 7. Opinion of respondents on the possibility of providing medical services using telemedicine technologies (several answers are possible), % of respondents
Preliminary consultation only
Physician or general practitioner
Subspecialty physician
Nursing staff
Other
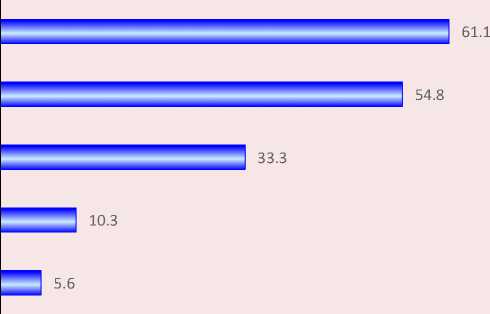
Source: the results of our own research in 2022.
-
Figure 8. Opinion of respondents in different age groups about the services that could be received using telemedicine (several answers are possible), % of each age group
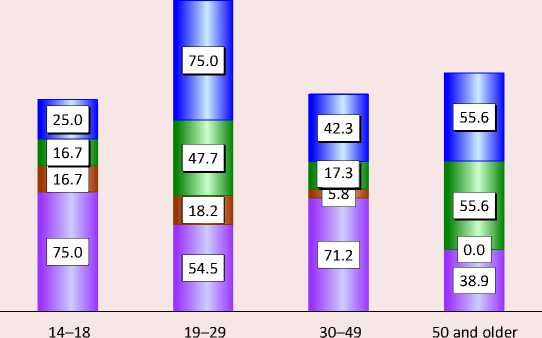
п Physician and general practitioner
□ Subspecialty physician о Nursing staff
D Preliminary consultation only
Source: the results of our own research in 2022.
According to the respondents, the most acceptable option for the provision of services using telemedicine is primarily the issuance of health certificates and sick leaves, in second place is the organization of teleconsultations, in third place is pre-registration for an appointment with a doctor, in fourth place is getting electronic prescriptions for drugs. The “primary consultations” option received less than half of the votes (Fig. 9) .
Respondents are much less willing to use telemedicine technologies for remote health monitoring (biomonitoring), adjusting previously prescribed treatment, and obtaining a medical opinion after the examination.
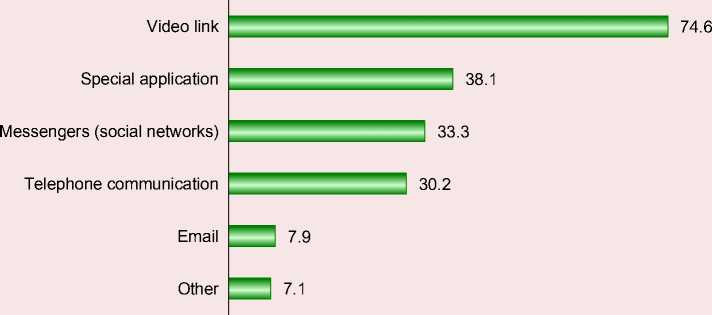
According to three-quarters of respondents, the best way to communicate when providing telemedicine services is via video link (since, apparently, the number of people who
-
Figure 9. What medical services could be provided using telemedicine (several answers are possible), % of respondents
Issuance of medical certificates and sick leaves
Teleconsultations
Make an appointment in advance
Prescriptions for drugs
Preliminary consultations
Health monitoring
(Remote Biomonitoring)
Adjustment of previously prescribed treatment
Medical reports (after examination)
Other
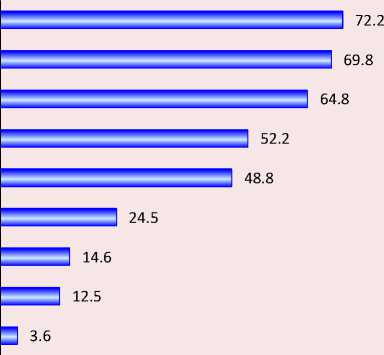
Source: the results of our own research in 2022.
have successfully mastered this method of communication has increased significantly in the face of the coronavirus pandemic in self-isolation). At the same time, noticeably more than a third believe that there should be a dedicated application, and this is primarily argued by the need to protect personal data, which “ordinary” messengers (social networks) cannot provide. In favor of the latter, a third of those surveyed agreed to have consultations over the phone (Fig. 10).
As for the dependence on age, video communication is more preferable for respondents
Figure 10. Distribution of respondents’ opinions on the best way to communicate to receive medical treatment (several answers are possible), % of the number of respondents
Source: the results of our own research in 2022.
of all ages. Telemedicine advice is more convenient for 38.9% of respondents aged 50 and older, and an even higher proportion of those aged 19– 29. Young people are more likely to talk about a dedicated app: 50% of 14- to 18-year-olds and 43.2% of 19- to 29-year-olds indicated this. To a lesser extent, people are interested in using e-mail: the younger generation notes its excessive overload, representatives of older age groups – problems with its use (Fig. 11) .
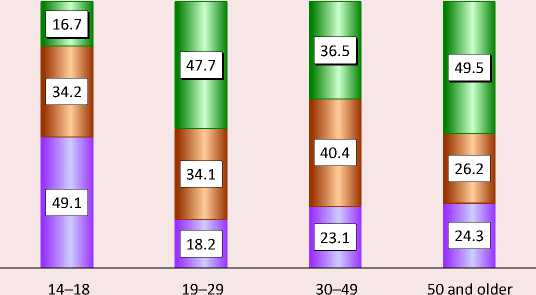
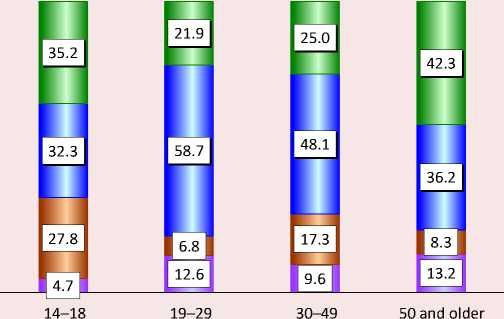
One of the main objectives of the study was to determine the degree of public confidence in the new possibilities of receiving medical services. For this purpose, we asked the question “If you were now offered telemedicine instead of visiting a general practitioner, would you accept it?”. On the sample as a whole, 40.5% of respondents agreed, one-fifth (22.2%) hesitated to respond, and the rest refused. The distribution of the answers received in relation to age is shown in Figure 12 .
Figure 11. Opinion of respondents in different age groups about methods of communication in the provision of telemedicine services (several answers are possible), % of each age group
□ Telephone communication
□ Video link
D Messengers
П Special application
Source: the results of our own research in 2022.
Figure 12. Results of responses to the question “If you were now offered telemedicine instead of visiting a general practitioner, would you accept?”, % of each age group
-
□ Yes
-
□ No
-
□ Hesitate to respond
Source: the results of our own research in 2022.
As we can see, the largest proportion of those willing to use a remote consultation with a physician was among the older generation; a little less – in the 19–29 age group, even less, though more than a third – in the 30–49-year-old group. We should note that almost half of the 14–18-year-old respondents were undecided at all, with the least number of those who gave a positive answer (16.7%).
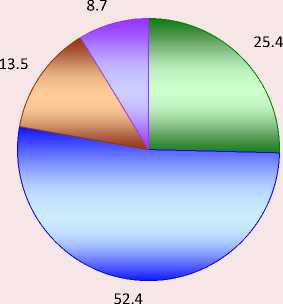
In general, the study showed that a quarter of the respondents had a positive attitude toward telemedicine, more than half had a neutral attitude, and one in ten had a negative attitude (Fig. 13) .
When analyzing the distribution of responses by age (Fig. 14) , we found that people aged 50–70 years and the youngest age group have the most positive attitude toward telemedicine technologies.
Figure 13. Respondents’ attitudes towards telemedicine, % of respondents
-
□ Positive
-
□ Neutral
-
□ Negative
-
□ Hesitate to respond
Source: the results of our own research in 2022.
Figure 14. Respondents’ attitudes toward telemedicine, % of each age group
-
□ Positive
п Neutral
-
□ Negative
о Hesitate to respond
Source: the results of our own research in 2022.
Respondents aged 19–29 had the least loyal perception of telemedicine: they most often have a neutral attitude toward it. Most likely due to the absence of chronic diseases and infrequent visits to doctors, they do not see any real problems when making appointments at the clinic and hospital. Negative attitudes are most pronounced in the youngest group and among middle-aged respondents.
Discussion
A primary study conducted allowed obtaining data on the attitudes of Russians toward receiving medical services through telemedicine technologies in regions typical not only in terms of telemedicine technology implementation capabilities, but also in terms of leading organization of the COVID-19 response measures. The survey was conducted at a period when the impact of the pandemic on society was noticeably diminishing (it was at this time that the incidence of the disease went down, including due to reasonable decisions made in the field of prevention and treatment of coronavirus infection). One can compare these results with an earlier study of Russians’ attitudes toward telemedicine conducted by the Research Institute NIIOZMM shortly before the pandemic in October 2019 (Bogdan et al., 2020). Thus, there is a unique opportunity to compare the results of two surveys carried out before the pandemic and after its active phase – the decline in the number of recorded cases and the almost complete removal of all restrictions in the regions studied.
Before the pandemic, the use of telemedicine was possible for 67% of respondents; after the pandemic, this number increased by 10%. Remote technologies were perceived positively by 34% of respondents before the pandemic and 25% after the pandemic, but the proportion who viewed them neutrally increased to 52% (33% before the pandemic). There is one percent less of those who have a “negative” attitude toward such technologies, and 5 percent less of those who cannot make up their minds.
Before the pandemic, 45% of respondents agreed to receive medical reports and certificates via telemedicine technologies, and after the acute phase of the pandemic, their proportion increased 1.6-fold (to 72.2%). As for teleconsultation, 36% of respondents had a positive perception before the pandemic and 69.8% afterwards (an almost two-fold increase). Getting prescriptions using telemedicine technology has also become more popular (an increase of 1.3 times). The proportion of those willing to use telemedicine for health monitoring increased 1.4-fold (from 17.0% to 24.5%).
Before the pandemic, 27.0% were willing to get a remote consultation with a subspecialist; after the pandemic, slightly more – 33.3%. The rate of readiness to potentially see a general practitioner or physician via telemedicine technology decreased from 78.0% to 54.8% after the pandemic. However, in the 2022 survey, 40.5% of respondents agreed to get a remote therapist consultation right now (a similar question had not been asked before), and one-fifth were undecided at that time. It seems that much of the reason for this hesitation lies in the convenience of organizing this kind of communication with the doctor. After the pandemic, the respondents indicated video communication as the main means of communication for the organization of telemedicine “doctor – patient” consultations (74.6%); 45% chose this type of communication before the pandemic (1.6 times less frequently). Among those surveyed after the pandemic, 38.1% were in favor of a dedicated application (primarily to protect personal data), while before the pandemic – 23% of respondents. A third of respondents noted that it would be easier to use messengers (social networks); before the pandemic, there were twice as many people willing to use a social network to communicate with a doctor, which was due to the underdevelopment of video communication systems at the time.
Key takeaways
Thus, after analyzing the results of the two studies, we can conclude that Russian citizens have become more loyal to the use of telemedicine technologies for various types of medical care. The main questions that arise from potential and actual patients are mostly related to the accuracy of the recommendations and diagnoses that doctors make and give, communicating with patients only remotely. However, external challenges (e.g., the coronavirus pandemic) that society is facing are forcing the use of such technologies. The best practices and techniques developed during the pandemic, which have proven their validity and relevance, will continue to be replicated in the health care system. The second component of patient wariness about telemedicine has to do with the moral and ethical aspects of organizing communication with doctors. On the one hand, the pandemic period allowed many to gain experience using video communication; on the other hand, there are issues of security, compliance with the Federal Personal Data Law, medical ethics, etc. that have not been fully resolved.
The results of the work confirmed the hypotheses put forward at the beginning of the research: first, indeed, due to the spread of coronavirus infection and the introduction of restrictive measures, Russian society has become more trusting of telemedicine technologies than before the pandemic. Secondly, the younger generation is more predisposed to the use of information telemedicine technologies (higher level of trust in ICTs): according to its representatives, this approach saves time in a medical institution and allows receiving the appropriate level of quality medical services.
Conclusion
Currently, telemedicine in Russia, as well as throughout the world, has become an integral part of the work of medical institutions at virtually all levels. Information technology is now also used for patient consultation at home, remote telemetry for vital signs, and for accompanying critically ill patients. The provision of remote medical care through the use of modern communication technologies has become extremely popular during the peak of COVID-19. Under such conditions, due to the critical situation in the healthcare system and epidemiological indicators, polyclinics in some regions of the country were forced to switch to a remote form of providing medical care to the population in order to preserve the efficiency and more effective work of the primary care. An unprecedented number of call center operators were engaged to assist the population around the clock. This required changes not only in the organization of the direct provision of medical care, but also significant adjustments to the legislation. Such changes were implemented primarily in the regulation of the use of telemedicine technologies, electronic prescriptions, sick-leave certificates, etc. All these measures allowed reducing the level of morbidity and, ultimately, helped the primary care system to survive in the current situation.
It is obvious that today there are still many problems related to the use of telemedicine technologies. There is a need to regulate the workload of doctors when performing such consultations. The issues of payment for such services remain acute (the degree of development and prevalence of information and communication technologies varies in different regions, the density of the population and its spatial dispersion are uneven). It is necessary to simplify the identification of patients as much as possible, because they are mostly elderly people who do not have the necessary level of information technology. Doctors need a clear mechanism for telemedicine, which would allow consulting patients not only from the offices.
At the decision-making stage, it is necessary to draw on the experience of those who are directly involved in the provision of medical services “doctor – patient”, which will make it possible to organize the process using the best practices of telemedicine.
Thus, this study proves that during a pandemic, telemedicine technology is necessary, and the best practices can and should be used even in the absence of such a force majeure. Russian doctors and patients already agree to a certain extent and are ready to use telemedicine tools when providing medical care, and the healthcare system has the necessary technology to a certain extent at both the regional and federal levels. There are positive changes in the legal field as well: during the pandemic, amendments to laws, decrees, and orders regulating telemedicine activities were adopted. Telemedicine is a clear trend in the future development of Russian healthcare, which, given the continued improvement in ICTs on the one hand, and the likelihood of new external challenges on the other, will only intensify.
The most promising telemedicine technologies today are remote patient monitoring, which can significantly reduce loss of time and increase the efficiency of medical services (including by reducing the transportation costs of both medical institutions and patients), as well as remote diagnosis and treatment of complex clinical cases.
Similar technologies are already being used in the creation of a single database of CT scans of the lungs of people with coronavirus infection. Such a telemedicine system based on elements of artificial intelligence makes it possible to diagnose and determine the degree of lung damage in COVID-19 disease accurately and promptly enough. Another use of telemedicine is the monitoring of public health on the basis of universal medical examinations in the workplace using telemedicine mobile units and systems. Finally, one cannot ignore the prospect of global dissemination and consolidation of advanced professional knowledge and skills through telemedical consultations.
To conclude, in view of the doubts among both the public and the medical community about telemedicine, we would like to quote Dr. Kenneth T. Baird (Bashshur, 2007), whose statements best describes the vision of telemedicine technology in its early days and is just as relevant today: “... telemedicine depends on the doctor and their specialized capabilities. It does not replace them and is not an alternative to a doctor. In fact, telemedicine increases the efficiency of the specialist and empowers them to be at the very center of medical activity”. This is what Russian doctors and their patients must experience as they continue to develop telemedicine in Russian healthcare.
Список литературы Telemedicine in modern conditions: the attitude of society and the vector of development
- Aoki N., Dunn K., Johnson-Throop K.A., Turley J.P. (2003). Outcomes and methods in telemedicine evaluation. Journal of Telemedicine and E-Health, 9(4), 393–401.
- Bashshur R. (2007). Telemedicine, history, challenges and transformation. In: Presentation at the Second eHealth Congress, October. Turkey, Antalya, 18–20.
- Bashshur R.L., Shannon G.W. (2009). History of Telemedicine: Evolution, Context, and Transformation. New York: New Rochelle.
- Bergmo T.S. (2009). Can economic evaluation in telemedicine be trusted? A systematic review of the literature. Cost Effectiveness Resource Allocation, 7(18). DOI: 10.1186/1478-7547-7-18
- Bogdan I.V., Gurylina M.V., Chistyakova D.P. (2020). Prospects and risks of telemedicine: Survey results. In: Sotsiologiya i obshchestvo: traditsii i innovatsii v sotsial’nom razvitii regionov: sb. dokladov VI Vserossiiskogo sotsiologicheskogo kongressa (Tyumen’, 14–16 oktyabrya 2020 g.) [Sociology and Society: Traditions and Innovations in Social Development of Regions: Proceedings of the VI All-Russian Sociological Congress (Tyumen, October 14–16, 2020)]. Moscow: ROS; FNISTs RAN. DOI: 10.19181/kongress.2020.307 (in Russian).
- Charrier N., Zarca K., Durand-Zaleski I., Calinaud C. (2016). Efficacy and cost effectiveness of telemedicine for improving access to care in the Paris region: Study protocols for eight trials. BMC Health Service Research, 8, 16–45. DOI: 10.1186/s12913-016-1281-1
- Ekeland A.G., Grїttland A. (2015). Assessment of mast in European patient-centered telemedicine pilots. International Journal of Technology Assessment in Health Care, 31(5), 304–311. DOI: 10.1017/S0266462315000574
- Grigor’ev A.I., Orlov O.I., Loginov V.A. et al. (2001). Klinicheskaya telemeditsina: monografiya [Clinical Telemedicine: Monograph]. Moscow: Slovo.
- Hailey D., Roine R., Ohinmaa A. (2002). Systematic review of evidence for the benefits of telemedicine. Journal of Telemedicine and Telecare, 8(1), 1–30.
- Halpren-Ruder D., Chang A.M., Hollander J.E., Shah A. (2019). Quality assurance in telehealth: Adherence to evidence-based indicators. Telemedicine Journal and E-Health, 25(7), 599–603. DOI: 10.1089/tmj.2018.0149
- Hersh W.R., Hickam D.H., Severance S.M. et al. (2006). Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. Journal of Telemedicine and Telecare, 12(1), 3–31.
- Kamaev I.A., Levanov V.M., Sergeev D.V. (2001). Telemeditsina: klinicheskie, organizatsionnye, pravovye, tekhnologicheskie, ekonomicheskie aspekty: monografiya [Telemedicine: Clinical, Organizational, Legal, Technological, and Economic Aspects: Monograph]. Nizhny Novgorod: NGMA.
- Kidholm K., Clemensen J., Caffery L.J., Smith A.C. (2017). The Model for Assessment of Telemedicine (MAST): A scoping review of empirical studies. Journal of Telemedicine and Telecare, 23(9), 803–813. DOI: 10.1177/1357633X17721815
- Kim E.J. et al. (2019). Cardiology electronic consultation (e-consult) use by primary care providers at VA medical centres in New England. Journal of Telemedicine and Telecare, 25(6), 370–377. DOI: 10.1177/1357633X18774468
- Kobrinskii B.A. (2016). Telemeditsina v sisteme prakticheskogo zdravookhraneniya [Telemedicine in the Practical Healthcare System]. Moscow: Berlin: Directmedia.
- Kroshilin S.V., Medvedeva E.I., Aleksandrova O.A. et al. (2020). Analysis of professional training and demand for nursing staff in the context of modern health policy. Ekonomika i predprinimatel’stvo=Journal of Economy and entrepreneurship, 8(121), 1148–1161. DOI: 10.34925/EIP.2020.121.8.230 (in Russian).
- Levanov V.M., Kirpicheva I.S., Yashin A.A. et al. (2014). Typical mistakes in teleconsultations. Meditsinskii al’manakh=Medical Almanac, 1(31), 15–18 (in Russian).
- Levanov V.M., Perevedentsev O.V., Sergeev D.V. et al. (2017). Telemedicine legislation: 20 years of development. Zhurnal telemeditsiny i elektronnogo zdravookhraneniya=Russian Journal of Telemedicine and E-Health, 3 (in Russian).
- Martin-Khan M. et al. (2011). A systematic review of studies concerning observer agreement during medical specialist diagnosis using videoconferencing. Journal of Telemedicine and Telecare, 17(7), 350–357.
- Morozov S.P. et al. (2018). Telemedicine-based system for quality management and peer review in radiology. Insights into Imaging, 9(3), 337–341.
- Morozov S.P., Vladzimirskii A.V., Simenyura S.S. (2020). The quality of primary direct-to-consumer telemedicine consultations (by results of testing telemedicine services). Vrach i informatsionnye tekhnologii=Information technologies for the Physician, 1, 51–62 (in Russian).
- Resneck J.S. Jr., Abrouk M., Steuer M. et al. (2016). Choice, transparency, coordination, and quality among direct-to-consumer telemedicine websites and apps treating skin disease. JAMA Dermatology, 152(7), 68–75. DOI: 10.1001/jamadermatol.2016.1774
- Shi Z., Mehrotra A., Gidengil C.A. et al. (2018). Quality of care for acute respiratory infections during direct-to-consumer telemedicine visits for adults. Health Affairs (Millwood), 37(12), 20–23. DOI: 10.1377/hlthaff.2018.05091
- Stolbov A.P. (2015). About the definition and classification of telemedicine services. Vrach i informatsionnye tekhnologii=Information technologies for the Physician, 2, 12–27 (in Russian).
- Taylor P. (2005). Evaluating telemedicine systems and services. Journal of Telemedicine and Telecare, 1, 167–177.
- Vladzimirskii A.V. (2015). The first 150 years of a telemedicine history. Zhurnal mezhdunarodnogo obshchestva telemeditsiny i elektronnogo zdravookhraneniya – Rossiya=Russian Journal of Telemedicine and E-Health, 1(1), 10–16 (in Russian).
- Vladzimirskii A.V. (2017). Patient initiated direct-to-consumer telemedicine consultations: First step for a methodology systematization. Zhurnal telemeditsiny i elektronnogo zdravookhraneniya=Russian Journal of Telemedicine and E-Health, 2, 109–120 (in Russian).
- Vladzimirskii A.V. (2019). Istoriya telemeditsiny: stoya na plechakh gigantov (1850–1979) [History of Telemedicine: Standing on the Shoulders of Giants (1850–1979)]. Moscow: De`Libri.
- Vladzimirskii A.V. (2020). Matrix for direct-to-consumer telemedicine quality assessing. Zhurnal telemeditsiny i elektronnogo zdravookhraneniya=Russian Journal of Telemedicine and E-Health, 6(4), 34–44. DOI: https://doi.org/10.29188/2542-2413-2020-6-4-34-44 (in Russian).
- Vladzimirskii A.V., Lebedev G.S. (2018). Telemeditsina: monografiya [Telemedicine: Monograph]. Moscow: GEOTAR-Media.
- Vladzimirskii A.V., Morozov S.P., Urvantseva I.A. et al. (2019). Primenenie telemeditsinskikh tekhnologii v kardiologii [Telemedicine in Cardiology]. Surgut: SurGU.
- Vladzimirskii A.V., Morozov S. P., Simenyura S. S. (2020). Telemedicine and COVID-19: Quality of patient-initiated teleconsultations in case of acute respiratory disease. Vrach i informatsionnye tekhnologii=Information Technologies for the Physician, 2, 52–63. DOI: 10.37690/1811-0193-2020-2-52-63 (in Russian).
- Volynskii Yu.D. (1999). Telemedicine is part of the information society. Informatsionnoe obshchestvo=Information Society, 5, 15–21 (in Russian).
- Voskolovich N.A. (2021). Ekonomika platnykh uslug [Economics of Paid Services]. Moscow: Yurait.
- Weinstein R.S. et al. (2018). Clinical examination component of telemedicine, telehealth, mhealth, and connected health medical practices. Medical Clinics of North America, 102(3), 533–544.
- Wootton R., Vladzymyrskyy A., Zolfo M., Bonnardot L. (2011). Experience with low-cost telemedicine in three different settings. Recommendations based on a proposed framework for network performance evaluation. Global Health Action, 4. DOI: 10.3402/gha.v4i0.7214
- Yarasheva A.V., Aleksandrova O.A., Medvedeva E.I. (2020). Problems and prospects of personnel support of the Moscow healthcare system. Ekonomicheskie i sotsial’nye peremeny: fakty, tendentsii, prognoz=Economic and Social Changes: Facts, Trends, Forecast, 13(1), 174–190. DOI: 10.15838/esc.2020.1.67.10 (in Russian).
- Zheleznyakova I.A., Khelisupali T.A., Omel’yanovskii V.V. et al. (2020). Application of foreign experience of telemedicine services in the Russian Federation. Meditsinskie tekhnologii. Otsenka i vybor=Medical Technologies. Assessment and Choice, 2, 26–34. DOI: https://doi.org/10.17116/medtech20204002126 (in Russian).
- Zingerman B.V., Shklovskii-Kordi N.E., Vorob’ev A.I. (2017). About telemedicine “Patient to Doctor”. Vrach i informatsionnye tekhnologii=Information Technologies for the Physician, 61–79 (in Russian).