Трудности диагностики нетрадиционной дисплазии, возникшей на фоне воспалительных заболеваний кишечника
Автор: Ахриева Х. М., Тертычный А. С., Пачуашвили Н. В., Урусова Л. С.
Журнал: Вестник медицинского института "РЕАВИЗ": реабилитация, врач и здоровье @vestnik-reaviz
Рубрика: Морфология. Патология
Статья в выпуске: 3 т.14, 2024 года.
Бесплатный доступ
Цель: дать морфологическую характеристику дисплазии, возникающей на фоне воспалительных заболеваний кишечника с учётом новой классификации дисплазии.
Дисплазия, колоректальная карцинома, ассоциированная с колитом, р53, воспалительные заболевания кишечника, морфологическая диагностика
Короткий адрес: https://sciup.org/143183289
IDR: 143183289 | УДК: 616.34-002-07-085 | DOI: 10.20340/vmi-rvz.2024.3.MORPH.2
Текст научной статьи Трудности диагностики нетрадиционной дисплазии, возникшей на фоне воспалительных заболеваний кишечника
Воспалительные заболевания кишечника (ВЗК), к которым традиционно относят язвенный колит (ЯК), болезнь Крона (БК) и связанное с ними хроническое повреждение слизистой оболочки, повышают риск возникновения дисплазии и аденокарциномы. У большинства пациентов колоноскопический скрининг начинается через 8–10 лет после первичного выставления диагноза ВЗК. Степень выраженности колита, продолжительность заболевания и признаки сохраняющейся на фоне лечения гистологической активности служат независимыми факторами риска развития дисплазии. За последние годы, в связи с улучшением медикаментозной терапии и внедрением передовых методов эндоскопического наблюдения, наблюдается снижение заболеваемости колоректальным раком (КРР). Тем не менее, оценочный риск развития КРР у пациентов с ВЗК по-прежнему составляет 1% и 7% через 10 лет и 30 лет соответственно. Данный показатель ещё выше у пациентов с ВЗК и сопутствующим первичным склерозирующим холангитом (ПСХ), у которых, несмотря на более низкое кумулятивное влияние воспаления, риск развития неоплазии увеличивается в 3–4 раза по сравнению с пациентами только с ВЗК без ПСХ [1, 2].
Патогенез неоплазии при ВЗК является многофакторным. Предполагается, что изменённый мик- робиом и повторяющиеся периоды воспалительного повреждения приводят к генетическим и эпигенетическим изменениям у пациентов с длительным течением заболевания. Стволовые клетки крипт приобретают мутации, чаще всего в генах TP53 и/или KRAS, которые обеспечивают селективное преимущество роста в условиях хронического повреждения. Эти аномальные клетки затем повторно заселяют повреждённую слизистую оболочку, создавая «эффект опухолевого поля» на больших участках слизистой оболочки, склонных к неопластическому прогрессированию [3]. Молекулярные аномалии, включая мутации TP53 и анеуплоидию, могут быть обнаружены в повреждённой слизистой оболочке даже при отсутствии морфологически распознаваемой дисплазии [4].
На молекулярном уровне карциномы, ассоциированные с колитом (КAК), заметно отличаются от своих спорадических аналогов. Хотя мутации APC гена возникают на ранних стадиях перехода от аденомы к карциноме при многих спорадических поражениях, в большинстве КАК данные мутации отсутствуют. Наиболее часто выявляемая мутация — TP53. Она возникает на более ранних стадиях неопластического процесса. КАК также имеет более высокие показатели анеуплоидии, мутаций IDH1, амплификации MYC и хромосомной нестабильности. КАК может различаться по своим гистологиче- ским особенностям, часто демонстрируя муцинозную и перстневидную морфологию, с подгруппой случаев, демонстрирующих уникальную тубу-логландулярную морфологию низкой степени злокачественности [6, 7]. Дополнительно можно увидеть иммуногистохимическую (ИГХ) потерю экспрессии SATB2 в 50% КАК и в 40% связанных с ней диспластических поражениях [8].
Учитывая повышенный риск развития карциномы, выявление дисплазии имеет жизненно важное значение для обеспечения пациентов своевременными эндоскопическими и хирургическими вмешательствами. Рекомендации SCENIC, представленные в 2015 году, изменили терминологию классификации пациентов с дисплазией [9]. От термина «поражение или образование, связанное с дисплазией» (DALM) отказались, поскольку стало понятно, что эндоскопия высокого разрешения и хромоэндоскопия позволяют визуализировать такие ранние поражения, которые раньше считались невидимыми или плоскими. Такая улучшенная визуализация дис-пластических поражений позволяет определять лечение пациентов в зависимости от того, является ли поражение эндоскопически операбельным. Согласно рекомендациям SCENIC, пациенты с ре-зектабельной дисплазией (полипоидной или сидячей) могут пройти контрольную колоноскопию. Колэктомию обычно назначают пациентам с резистентным к медикаментозному лечению заболеванием, неоперабельными поражениями, стойкой дисплазией высокой степени или мультифокальной дисплазией низкой степени [10].
Классическая дисплазия. Патологоанатомы играют решающую роль в ведении пациентов с дисплазией. Из-за воспаления и регенеративных изменений, наблюдаемых при колите, выявление дисплазии может быть затруднено. Классификация классической дисплазии, первоначально описанная доктором Робертом Риделом и его коллегами, разделяет биопсии на отрицательные в отношении дисплазии, неопределенные и положительные в отношении слабой или тяжёлой дисплазии [11]. Поражения, классифицируемые как дисплазия низкой степени, напоминают тубулярную аденому. Неопла- стические клетки имеют удлинённые ядра в форме карандаша, которые располагаются на разных уровнях и часто доходят до поверхности просвета. Поражения высокой степени злокачественности характеризуются повышенной цитологической ати-пией и сложностью архитектуры. Ядра увеличенные, округлые, с повышенным плеоморфизмом. Заметна потеря полярности. Категорию «неопределенный в отношении дисплазии» часто используют при атипичной слизистой оболочке с выраженным воспалением, при которой реактивный/регенеративный процесс остаётся в рамках дифференциального диагноза. Несмотря на эти чётко определённые категории, точная характеристика этих поражений может быть сложной задачей. Отмечаются высокие показатели вариабельности между наблюдателями, даже среди опытных патологов, специализирующихся в патологии желудочно-кишечного тракта [12, 13].
Нетрадиционная дисплазия. Недавно было описано несколько новых моделей дисплазии. Данные поражения называются «нетрадиционная дисплазия (НД)» из-за их клинико-патологических отличий от классической дисплазии. Они часто недооцениваются и могут быть диагностированы как отрицательные или неопределённые для дисплазии при скрининговой биопсии из-за незнания патологоанатомов. Идентификация и правильная классификация этих поражений имеет важное значение, поскольку исследования показали, что они несут повышенный риск развития поздней стадии неоплазии по сравнению с обычной дисплазией [14]. На сегодняшний день описано как минимум 7 подтипов (и 2 системы классификации): гипермуцинозная дисплазия (ГМД); дисплазия с дефицитом бокаловидных клеток (ДБК); атипия/дисплазия клеток крипт (ДКК); дисплазия с повышенной дифференцировкой клеток Панета (ДПД); дисплазия, подобная сидячим зубчатым по-липам/поражениям (СЗП); дисплазия, подобная традиционной зубчатой аденоме (ТЗА); зубчатая дисплазия без дополнительных уточнений (БДУ) (табл. 1). Как и классическая дисплазия, нетрадиционные подтипы чаще встречаются у пациентов с длительным ВЗК. ГМД, ДБК и ДКК также часто встречаются у пациентов с сопутствующим ПСХ [15].
Таблица 1 . Морфологические, прогностические и молекулярные характеристики нетрадиционной дисплазии
Table 1 . Morphological, prognostic and molecular features of non-conventional dysplasia
|
Параметр |
Гипермуцинозная |
С дефицитом бокаловидных клеток |
Дисплазия клеток крипт |
Дисплазия с клетками Панета |
ТЗА-подобная |
СЗА-подобная |
|
Подтип |
Желудочный |
Кишечный |
Кишечный |
Кишечный |
Зубчатый |
Зубчатый |
|
Форма |
Полиповидная |
Плоская |
Плоская |
бляшковидная |
Полиповидная на широком основании |
Полиповидная на широком основании |
|
Морфология |
Тубуло-ворсинчатая |
Тубулярная |
Тубулярная |
Тубулярная |
Зубчатая |
Зубчатая |
|
Молекулярные характеристики |
ТР53 Анеуплоидия KRAS |
ТР53 KRAS PIK3CA Анеуплоидия |
Анеуплоидия ТР53 |
Нет данных |
KRAS BRAF |
BRAF KRAS |
Целью нашего исследования было описание особенностей собственных наблюдений нетрадиционной дисплазии, развившейся у пациентов с ВЗК, и отработка на их примере предлагаемых диагностических критериев.
Материалы и методы
На текущем диагностическом материале биопсий толстой кишки за 2023 год нами было диагностировано 5 случаев нетрадиционной дисплазии у пациентов с ВЗК. Всего за этот период наблюдения диагноз ВЗК был установлен или подтверждён у 257 человек. Пациенты проходили лечение в клиниках Сеченовского университета в период с 2018 по 2023 годы. Возраст пациентов варьировал от 19 до 63 лет. Во всех случаях диагноз был установлен на основании комплекса клинико-лабораторных и инструментальных методов диагностики. У всех пациентов при проведении колоноскопии были получены множественные биоптаты.
Обработка материала биопсий проводилась по общепринятой методике. Гистологические срезы толщиной 3–5 мкм были окрашены гематоксилином и эозином. Для подтверждения диагноза было выполнено иммуногистохимическое исследование с антителами к ТР53 (DO-7, RTU, Leica, Германия), которое позволило подтвердить мутацию гена ТР53 в опухолевых клетках. Процесс иммуногистохимического (ИГХ) окрашивания препаратов проводили в автоматическом режиме на иммуностейнере Bond Max фирмы «Leica» (Германия).
Результаты исследования
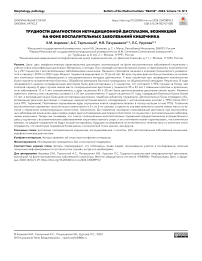
Нетрадиционная дисплазия была диагностирована у 5 пациентов, что составило 1,95% случаев за более чем 6-летний период наблюдения. В двух случаях имела место гипермуцинозная дисплазия (рис. 1). У пациентов 35 и 43 лет с язвенным колитом и длительностью заболевания 12 и 9 лет соответственно в сигмовидной и прямой кишке были обнаружены полиповидные образования тубуло-ворсинчатого строения. Ворсинки были выстланы высокими муцинозными столбчатыми эпителиальными клетками с морфологией, напоминающей желудочные фовеолярные клетки. Степень цитологической атипии была незначительной и уменьшалась к поверхности ворсинок, тем самым имела обманчиво доброкачественный вид. Такой вариант дисплазии имел как чистую гипермуцинозную морфологию, так и сочетался с зубчатым диспластическим компонентом (рис. 2).
У двух пациентов 30 и 40 лет была диагностирована дисплазия клеток крипт. Оба поражения локализовались в сигмовидной кишке и не были видны при проведении эндоскопического исследования (были «невидимыми»). Анамнез язвенного колита у этих пациентов составил 10 и 12 лет соответственно.
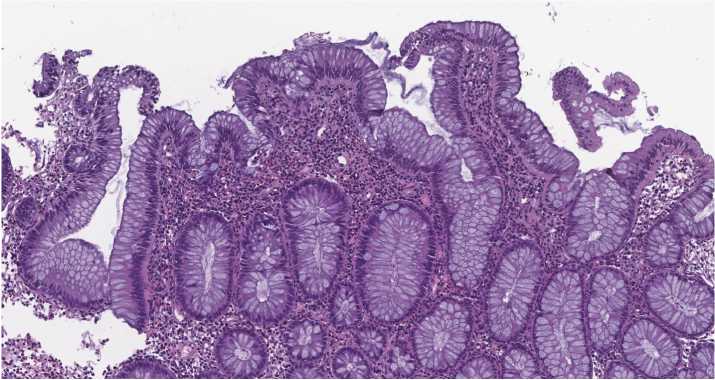
Рисунок 1. Гипермуцинозная дисплазия. Очаг поражения имеет тубуло-ворсинчатое строение и выстлан эпителием с высоким содержанием слизи в цитоплазме клеток. Окраска гематоксилином и эозином, ув. ×200
Figure 1 . Hypermucinous dysplasia. The lesion has a tubulo-villous structure and is lined with epithelium with a high content of mucus in the cytoplasm of cells. Staining with hematoxylin and eosin. ×200
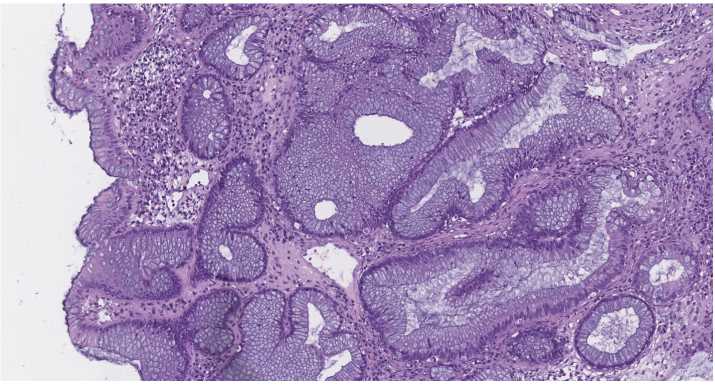
Рисунок 2. Гипермуцинозная дисплазия. Очаг поражения имеет зубчатые очертания крипт в базальных отделах и выстлан эпителием с высоким содержанием слизи в цитоплазме клеток. Отмечается расширение просвета крипт с накоплением слизи. Окраска гематоксилином и эозином, ув. ×200
Figure 2 . Hypermucinous dysplasia. The lesion exhibits jagged outlines of crypts in the basal sections, lined with epithelium containing a high concentration of cytoplasmic mucus. Crypt lumens are expanded with mucus accumulation. Staining with hematoxylin and eosin. ×200
При гистологическом исследовании дисплазия клеток крипт демонстрировала сохранённую архитектуру крипт и не имела явного поражения поверхности, наблюдаемого при классической дисплазии. Эпителиальные клетки в базальных отделах крипт были слегка увеличены и гиперхромны при микроскопическом исследовании, с ядрами от округлых до овальных и с неровными контурами ядер на поверхности поражения (рис. 3). Неопластическая пролиферация заметно отличалась от фоновой слизистой оболочки. При использовании ИГХ исследования наблюдался мутантный паттерн экспрессии р53 (рис. 4), что позволило провести дифференциальный диагноз с реактивными изменениями эпителия крипт.
У одной пациентки 51 года, страдавшей болезнью Крона более 15 лет, в восходящей кишке была диагностирована дисплазия, подобная зубчатому поражению. Гистологические особенности зубчатоподобной дисплазии демонстрировали зубчатый столбчатый характер роста эпителия в поверхностных отделах, а клетки имели характерную микрове-зикулярную цитоплазму. Этот вариант дисплазии демонстрировал более выраженную степень цитологической атипии и менее упорядоченный характер роста крипт, чем типичные спорадические зубчатые поражения. Эпителиальные зазубрины затрагивали поверхностную часть поражения. Ядерная атипия распространялась от основания крипт до поверхностного эпителия. Ядра клеток были расположены базально, имели округлую или овальную форму, гиперхромны и плеоморфны (рис. 5). При ИГХ реакции было получено позитивное окрашивание ядер клеток преимущественно в эпителии крипт, что свидетельствовало в пользу мутации в гене р53 (рис. 6).
Клинико-морфологические характеристики пациентов представлены в таблице 2.
Обсуждение
В течение четырёх десятилетий, прошедших с момента публикации оригинальной стандартизированной системы классификации дисплазии при ВЗК среди патологоанатомов растёт признание того, что «аденомоподобная» дисплазия, которая исторически считалась прототипом предшественников КРР при ВЗК, не полностью объясняет морфологическое разнообразие потенциальных неопластических поражений-предшественников КРР у этих пациентов.
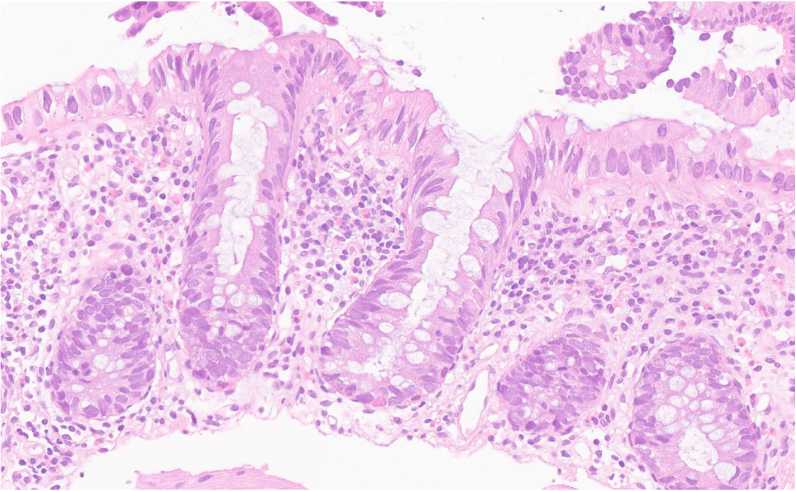
Рисунок 3. Дисплазия клеток крипт. Эпителиальные клетки в базальных отделах крипт увеличены и гиперхромны, с ядрами от округлых до овальных и с неровными контурами ядер на поверхности поражения. Окраска гематоксилином и эозином, ув. ×250 Figure 3 . Dysplasia of crypt cells. Epithelial cells in the basal crypts are enlarged and hyperchromic, with nuclei from rounded to oval and with uneven contours of the nuclei on the surface of the lesion. Staining with hematoxylin and eosin. ×250
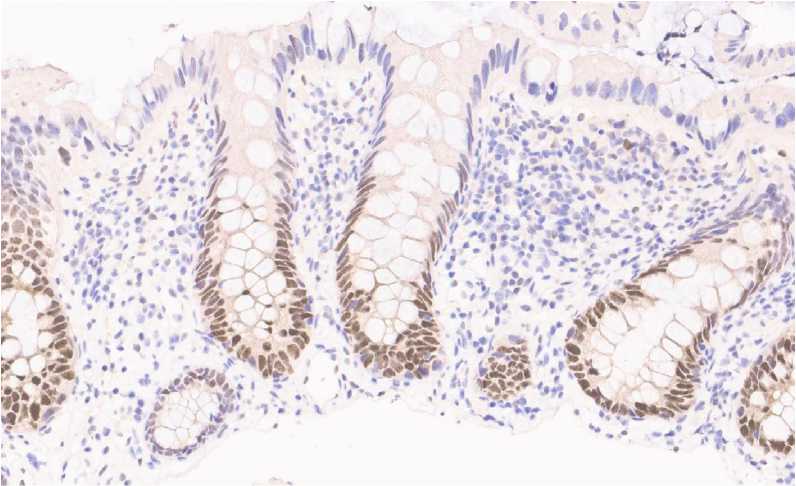
Рисунок 4. Дисплазия клеток крипт. Эпителиальные клетки в базальных отделах крипт с позитивным окрашиванием ядер в реакции с р53. ИГХ реакция с антителом р53, ув. ×250
Figure 4 . Dysplasia of crypt cells. Epithelial cells in the basal crypts with positive nuclear staining in reaction with p53. IHC reaction with antibody p53. ×250
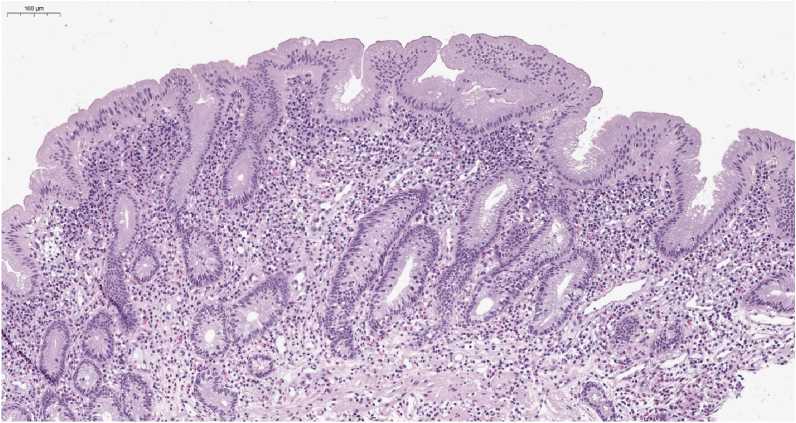
Рисунок 5 . Зубчато-подобная дисплазия. Зубчатые очертания крипт в поверхностных отделах выстланные эпителием с микровезикуляр-ной цитоплазмой. Окраска гематоксилином и эозином, ув. ×150 Figure 5 . Sessile serrated lesion-like dysplasia. The surface sections of hypermucinous dysplasia display jagged outlines of crypts, lined with epithelium characterized by microvesicular cytoplasm. Staining with hematoxylin and eosin. ×150

Рисунок 6. Дисплазия клеток крипт. Эпителиальные клетки крипт и покровного эпителия с позитивным окрашиванием ядер в реакции с р53. ИГХ реакция с антителом р53, ув. ×200
Figure 6 . Dysplasia of crypt cells. Epithelial cells of crypts and foveolar epithelium with positive staining of nuclei in reaction with p53. IHC reaction with antibody p53, ×200
Таблица 2 . Клинико-морфологические характеристики пациентов с ВЗК и нетрадиционной дисплазией Table 2 . Clinical and morphological features of IBD patients with non-conventional dysplasia
|
Пациент |
Возраст, лет |
Пол |
Диагноз |
Длительность заболевания |
Локализация |
Эндоскопическая характеристика |
Вариант дисплазия |
Дополнительные особенности |
|
1 |
35 |
м |
ЯК |
9 |
Сигмовидная кишка |
Видимый полиповидный очаг |
Гипермуцинозная |
Тотальный колит |
|
2 |
43 |
м |
ЯК |
12 |
Прямая кишка |
Видимый полиповидный очаг |
Гипермуцинозная |
ПСХ |
|
3 |
40 |
м |
ЯК |
12 |
Сигмовидная кишка |
Подозрение на плоский очаг |
Клеток крипт |
– |
|
4 |
30 |
м |
ЯК |
10 |
Сигмовидная кишка |
Невидимый |
Клеток крипт |
Тотальный колит |
|
5 |
51 |
ж |
БК |
15 |
Восходящая ободочная кишка |
Полип на широком основании |
Зубчатая |
– |
Примечание: ЯК – язвенный колит, БК – болезнь Крона; ПСХ – первичный склерозирующий холангит.
Основной проблемой при изучении нетрадиционных дисплазий является ограниченность литературы по их морфологическим особенностям, что делает их менее знакомыми патологоанатомам, которые могут не заметить некоторые из этих дис-пластических поражений как доброкачественные, реактивные или обычные дисплазии. В настоящем исследовании мы использовали определённые гистологические термины для характеристики данных нетрадиционных поражений (табл. 1). ГМД демонстрирует трубчато-ворсинчатую/ворсинчатую архитектуру с высокими муцинозными клетками, составляющими более 50% поражения. Она обычно показывает диспластические признаки низкой степени, поражающие крипты с лёгким увеличением ядер и гиперхромазией, а также удлинёнными, слегка неправильными ядрами. Примечательно, что степень атипии имеет тенденцию к уменьшению к поверхности поражения. Она может представлять собой чистый или смешанный тип (либо с классической дисплазией, либо с другим нетрадиционным подтипом); однако, чтобы классифицироваться как смешанный тип, гипермуцинозный компонент должен составлять более 50% поражения. ДПД демонстрирует тубулярный характер роста с диспластически-ми криптами, выстланными в основном удлиненными гиперхромными ядрами, а также повышенную дифференцировку клеток Панета, включающую, по крайней мере, две смежные крипты в двух разных очагах (помимо того, что присутствует в фоновой слизистой оболочке) [16]. Хотя ожидается некоторая потеря бокаловидных клеток, бокаловидные клетки не должны отсутствовать. Важно отметить, что ДПД отличается от ДКК. В то время как ДПД показывает в основном удлинённые, гиперхроматические ядра и всегда демонстрирует повышенную дифференцировку клеток Панета, ДКК характеризуется в основном круглыми или овальными, неслоистыми ядрами со случайной дифференцировкой клеток Панета. ДБК похожа на ДПД, но демонстрирует полное или почти полное отсутствие бокало- видных клеток [14, 15]. Рассеянные клетки Панета могут присутствовать в очаге поражения и в прилегающей слизистой оболочке, но не в множественных скоплениях диспластических крипт, как при ДПД. Поскольку метапластические (т.е. метаплазия клеток Панета) и реактивные изменения могут имитировать дисплазию ДПД и ДБК соответственно, важно отметить, что диагноз ДПД или ДБК требует обязательных гистологических доказательств дисплазии, демонстрирующих отчётливое отсутствие созревания поверхности и/или тяжёлую цитологи-ческую/архитектурную атипию [17]. Что касается зазубренных поражений, ТЗА-подобные поражения имеют трубчато-ворсинчатую/ворсинчатую структуру с зазубренными ворсинками, выстланными высокими столбчатыми клетками с удлинёнными ядрами и интенсивно эозинофильной цитоплазмой. Отмечаются также характерные эктопические крипты. СЗП-подобные поражения отмечены заметными зазубринами и/или расширением в основании и на поверхности крипты. Наличие расширенных L- или перевернутых T-образных крипт является диагностическим признаком. Зубчатые поражения без определенных признаков ТЗА или СЗП следует классифицировать как зубчатые поражения БДУ. Все зубчатые поражения должны иметь выраженный зубчатый профиль, составляющий более 50% поражения. У них может быть дисплазия, которая может быть ограничена нижней частью или охватывать всю толщу слизистой оболочки [18].
Одной из проблем в этой области дисплазии, связанной с ВЗК, является путаница, связанная с зубчатыми поражениями при ВЗК. Эндоскопически видимые ТЗА-подобные и СЗП-подобные поражения у пациентов с ВЗК могут представлять собой поражения, связанные с ВЗК, но они также могут быть спорадическими зубчатыми полипами. На самом деле известно, что зубчатые поражения, связанные с ВЗК, имеют сходные клинические и молекулярные особенности со своими спорадическими аналогами, хотя их естественное течение в значительной степени неизвестно [19].
Интересно, что в системе Riddell и соавт. 1983 г., предложенной для оценки дисплазии, связанной с ВЗК, было отмечено, что зубчатые поражения с «гиперпластический полип (ГП)-подобными» чертами могут проявляться полным спектром эпителиальных изменений в диапазоне от негативных до неопределённых и диспластических, и что дисплазия в зубчатых поражениях чаще ограничивается нижней частью слизистой оболочки, в то время как верхняя часть показывает более зрелые клетки и зазубренный рисунок [11]. Также следует отметить, что зубчатые поражения, включая зубчатые поражения БДУ и ТЗА-подобные поражения, могут представлять собой второстепенный компонент ГМД. Поскольку поверхностная биопсия и/или проблемы со взятием биопсий (например, биопсия прилегающей слизистой оболочки или незначительного компонента основного поражения) могут помешать оценке все-го/основного поражения, поэтому рекомендуется использовать термины «ТЗА-подобный», «СЗП-подобный», или «зубчатое поражение БДУ» для описания зубчатых поражений, обнаруженных у пациентов с ВЗК, особенно для эндоскопически видимых зубчатых поражений, обнаруженных в сегментах толстой кишки с признаками хронического колита. Для эндоскоепически невидимых поражений дифференциальный диагноз в этой ситуации включает «зубчатое изменение эпителия», которое является термином, используемым для эпителиальной зубчатости без дисплазии в неполипоидных случайных биопсиях толстой кишки у пациентов с ВЗК. Зубчатые изменения эпителия при ВЗК могут представлять собой отдельный самостоятельный вариант эндоскопически видимых зазубренных поражений, поскольку небольшое число случаев зубчатых изменений эпителия демонстрировало ане-уплоидию, тогда как анеуплоидия не была обнаружена в СЗП (с дисплазией или без нее) или ГП независимо от статуса ВЗК [20].
Чтобы заложить основу для будущих клинических, патологических, молекулярных исследований, была разработана обновленная классификация дисплазии при ВЗК, которая является всеобъемлющей и воспроизводимой. В разработанной классификационной системе диспластические поражения разделены на основные группы на основе их кишечной, желудочной или смешанной дифференциации, а также характеристик тубулярного/ворсинчатого или зубчатого роста, в результате чего выделяют шесть диагностических категорий нетрадиционной дисплазии (табл. 1). Результаты проверки воспроизводимости данной классификации в целом оказались удовлетворительными, большинство поражений (67-81%) из этих диагностических категорий были диагностированы патологоанатомами с высокой степенью достоверности, что привело к существенному согласию между наблюдателями в этих случаях и умеренному согласию при объединении всех случаев. Кроме того, основные категории дисплазии кишечного и желудочного типа, а также зубчатых и незубчатых вариантов дисплазии привели к существенному и умеренному согласию соответственно. На основании этих данных авторы пришли к выводу, что эта система классификации подходит для будущих исследований, направленных на единообразное и последовательное определение наличия клинически значимых биологических различий между различными типами поражений [21]. Важно подчеркнуть, что авторы новой классификации использовали термин «дисплазия» для всех поражений, несмотря на то что, некоторые из них не обязательно демонстрируют традиционные цитологические особенности неопластических поражений-предшественников рака. В последние десятилетия становится всё более очевидным, что некоторые типы неопластических поражений-предшественников рака в желудочно-кишечном тракте (например, аденома пилорических желез, дисплазия крипт при пищеводе Барретта, сидячие зубчатые поражения) не проявляют традиционных признаков «дисплазии», несмотря на доказательства, подтверждающие наличие у них биологического потенциала развития рака. Однако, учитывая, что термин «дисплазия» закреплён в опубликованной литературе, понимается и признаётся клиницистами во всем мире как важный объект, который значительно увеличивает риск развития рака у пациента, данный термин был сохранён в новой системе классификации. Недавно появились данные, позволяющие предположить, что некоторые «нетрадиционные» подтипы дисплазии при ВЗК с очевидными морфологическими особенностями низкой степени могут на самом деле быть биологически агрессивными, как и поражения высокой степени, однако этот вопрос требует дальнейшего изучения [22, 23].
Заключение
Мы обратили внимание, что до появления последних классификаций дисплазии при ВЗК нами крайне редко диагностировалась дисплазия в биоп-татх от пациентов с ВЗК. Теперь мы понимаем, что спектр потенциальных неопластических поражений-предшественников КРР у пациентов с ВЗК намного шире, и это понимание может гарантировать, что клинически важные, но редкие поражения не будут упущены из виду, признавая, что будущие исследования их естественного течения могут в конечном итоге определить, что некоторые поражения более важны с клинической точки зрения, чем другие.
Наши результаты показывают, что система классификации в целом может применяться с высоким уровнем достоверности и воспроизводимости. Таким образом, они могут служить основой для будущих клинических и фундаментальных исследований, основанных на определённых категориях дисплазии, а не на гетерогенных комбинациях поражений с потенциально разнообразными клиническими и молекулярными характеристиками.
Морфологический вид дисплазии, возникающей на фоне ВЗК, неоднороден и может отличаться от традиционного классического, по своим характеристикам являющегося прототипом тубулярной аденомы [14–17]. Поскольку биопсия для скрининга ВЗК является рутинным исследованием в большинстве лечебных учреждений, занимающихся лечением пациентов с ВЗК, важно, чтобы практикующие патологоанатомы знали о подтипах нетрадиционных вариантов дисплазии, чтобы гарантировать точную и своевременную диагностику и соответствующее лечение пациентов.
Список литературы Трудности диагностики нетрадиционной дисплазии, возникшей на фоне воспалительных заболеваний кишечника
- Magro F., Langner C., Driessen A., Ensari A., Geboes K., Mantzaris G.J. European consensus on the histopathology of inflammatory bowel disease. Journal of Crohn's & colitis. 2013;7(10):827-851. https://doi.org/10.10167j.crohns.2013.06.001
- Castano-Milla C., Chaparro M., Gisbert J.P. Systematic review with meta-analysis: the declining risk of colorectal cancer in ulcerative colitis. Alimentary pharmacology & therapeutics. 2014;39:645-59. https://doi.org/10.1111/apt.12651
- Choi C.R., Bakir I.A., Hart A.L., Graham T.A. Clonal evolution of colorectal cancer in IBD. Nature reviews. Gastroenterology & hepatology. 2017;14:218-29. https://doi.org/10.1038/nrgastro.2017.1
- Rubin C.E., Haggitt R.C., Burmer G.C., Brentnall T.A., Stevens A.C., Levine D.S. et al. DNA Aneuploidy in colonic biopsies predicts future development of dysplasia in ulcerative colitis. Gastroenterology. 1992;103:1611-20. https://doi.org/10.1016/0016-5085(92)91185-7
- Shah S.C., Itzkowitz S.H. Colorectal cancer in inflammatory bowel disease: mechanisms and management. Gastroenterology. 2022;162:715-30. https://doi.org/10.1 053/j.gastro.2021.10.035
- Wanders L.K., Cordes M., Voorham Q., Sie D., de Vries S.D., d'Haens G.R.A.M. et al. IBD-associated dysplastic lesions show more chromosomal instability than sporadic adenomas. Inflammatory bowel diseases. 2020;26:1 67-80. https://doi.org/10.1093/ibd/izz171
- Hartman D.J., Binion D.G., Regueiro M.D., Miller C., Herbst C., Pai R.K. Distinct histopathologic and molecular alterations in inflammatory bowel disease-associated intestinal adenocarcinoma: C-MYC amplification is common and associated with mucinous/signet ring cell differentiation. Inflammatory bowel diseases. 2018;24:1780-90. https://doi.org/10.1093/ibd/izy057
- Ma C., Henn P., Miller C., Herbst C., Hartman D.J., Pai R.K. Loss of SATB2 expression is a biomarker of inflammatory bowel disease-associated colorectal dysplasia and adenocarcinoma. The American journal of surgical pathology. 2019;43:1314-22. https://doi.org/10.1097/PAS.0000000000001330
- Laine L, Kaltenbach T, Barkun A, McQuaid K.R., Subramanian V., Soetikno R. SCENIC International consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 201 5;81:489-501. https://doi.org/1 0.1053/j.gastro.2015.01.031
- Murthy S.K., Feuerstein J.D., Nguyen G.C., Velayos F.S. AGA clinical practice update on endoscopic surveillance and management of colorectal dysplasia in inflammatory bowel diseases: expert review. Gastroenterology. 2021;161:1043-51. https://doi.org/10.1053/j.gastro.2021.05.063
- Riddell R.H., Goldman H., Ransohoff D.F., Appelman H.D., Fenoglio C.M., Haggitt R.C. et al. Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Human pathology. 1983;14:931-68. https://doi.org/10.1016/s0046-8177(83)80175-0
- Feakins R.M., British Society of Gastroenterology. Inflammatory bowel disease biopsies: updated British Society of Gastroenterology reporting guidelines. Journal of clinical pathology. 201 3;66(12): 1005-1026. https://doi.org/10.1136/jclinpath-2013-201885
- Тертычный А.С., Ахриева Х.М., Коган Е.А., Зайратьянц О.В., Селиванова Л.С. Современные подходы в морфологической диагностике воспалительных заболеваний кишечника. Российский журнал гастроэнтерологии, гепатологии, колопроктологии. 2022;32(2):73-84. Tertychnyy A.S., Akhriyeva Kh.M., Kogan E.A., Zayratyants O.V., Selivanova L.S. Modern Approaches in the Morphological Diagnosis of Inflammatory Bowel Diseases. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2022;32(2):73-84. (In Russ).
- Lee H., Rabinovitch P.S., Mattis A.N., Lauwers G.Y., Choi W.T. Non-conventional dysplasia in inflammatory bowel disease is more frequently associated with advanced neoplasia and aneuploidy than conventional dysplasia. Histopathology. 2021;78:814-30. https://doi.org/10.1111/his.14298
- Choi W.T. Non-conventional dysplastic subtypes in inflammatory bowel disease: a review of their diagnostic characteristics and potential clinical implications. Journal of pathology and translational medicine. 2021;55:83-93. https://doi.org/10.4132/jptm.2021.02.1 7
- Pereira D., Kоvаri B., Brown I., Chaves P., Choi W.T., Clauditz T., et al. Non-conventional dysplasias of the tubular gut: a review and illustration of their histomorphological spectrum. Histopathology. 2021;78:658e75. https://doi.org/10.1111/his.14294
- Choi W.T., Yozu M., Miller G.C., Shih A.R., Kumarasinghe P., Misdraji J., et al. Nonconventional dysplasia in patients with inflammatory bowel disease and colorectal carcinoma: a multicenter clinicopathologic study. Modern pathology. 2020;33:933-43. https://doi.org/10.1038/s41379-019-0419-1
- Alipour Z., Stashek K. Recently described types of dysplasia associated with IBD: tips and clues for the practicing pathologist. Journal of clinical pathology. 2024;77:77-81. https://doi.org/1 0.1136/jcp-2023-209141
- Ахриева Х.М., Коган Е.А., Тертычный А.С., Раденска-Лоповок С.Г., Зайратьянц О.В., Селиванова Л.С. Новый взгляд на структурную перестройку слизистой оболочки толстой кишки и стадии хронического колита при воспалительных заболеваниях кишечника. Архив патологии. 2021 ;83(6):14-19. Akhrieva Kh.M., Kogan E.A., Tertychnyi A.S., Radenska-Lopovok S.G., Zayratyants O.V., Selivanova L.S. A new look at colonic mucosal structural rearrangement and the stages of chronic colitis. Archive of Pathology = Arkhiv patologii. 2021;83(6): 14-19. (In Russ).
- Waters K.M., Singhi A.D., Montgomery E.A. Exploring the spectrum of serrated epithelium encountered in inflammatory bowel disease. Human pathology. 2023;132:126-34. https://doi.org/10.1016/j.humpath.2022.06.018
- Harpaz N., Goldblum J.R., Shepherd N.A., Riddell R.H., Rubio C.A., Vieth M., et al. Colorectal dysplasia in chronic inflammatory bowel disease: a contemporary consensus classification and interobserver study. Human pathology. 2023;138:49-61. https://doi.org/10.1016/j.humpath.2023.05.008
- Тертычный А.С., Ахриева Х.М., Маев И.В., Зайратьянц О.В., Селиванова Л.С. Проблемы диагностики гистологической ремиссии у больных с воспалительными заболеваниями кишечника. Архив патологии. 2017;79(3):3-9. Tertychny A.S., Akhrieva Kh.M., Maev I.V., Zairat'yants O.V., Selivanova L.S. Diagnostic problems of histological remission in patients with inflammatory bowel disease. Russian Journal of Archive of Pathology. 2017;79(3):3-9. (In Russ).
- Park S., Abdi T., Gentry M., Laine L. Histological Disease Activity as a Predictor of Clinical Relapse Among Patients With Ulcerative Colitis: Systematic Review and Meta-Analysis. The American journal of gastroenterology. 2016; 111(12):1692-1701. https://doi.org/10.1038/ajg.2016.418