A comparative study between functional outcomes of proximal humerus fracture treated using closed reduction and JESS external stabilization system and open reduction and internal fixation with PHILOS plate at a tertiary health care center
Автор: Garg D., Wagh N.P., Shinde M.B., Sarwey K., Jethliya S., Bahl R., Chunawala S., Yadav D., Zaveri A., Singh Y.N., Gupta A., Kaulgud V.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 5 т.31, 2025 года.
Бесплатный доступ
Introduction Proximal humerus fractures account for 5 % of all fractures. Their incidence increases with age, especially in women over 60. Most of them (85 %) are minimally displaced and managed non-operatively, while 15 % require surgery. Neer’s classification guides treatment, which includes conservative methods and operative methods. The operative techniques are PHILOS plating, pinning, nailing, or arthroplasty. The JESS fixator, developed by Dr. B.B. Joshi, offers a minimally invasive alternative. Purpose To compare the functional results of proximal humerus fractures treated with PHILOS plating and JESS fixation. Material and method The prospective observational study was conducted over 24 months on 36 patients with proximal humerus fractures. Patients were divided into two groups, 18 in each group, based on the surgical technique used: JESS fixation and PHILLOS plating. JESS group had more females, while PHILOS had more males. The Constant – Murley Scores were used to compare the functional outcome in both groups at regular intervals. Complications of both techniques were assessed. Results Falls were the main cause in JESS (72.22 %), while road accidents were more common in PHILOS (55.55 %) group. Both groups showed significant improvement in Constant – Murley Scores (p < 0.005). JESS group had one case each of avascular necrosis, malunion, and pin tract infection. PHILOS group had one implant failure and one avascular necrosis case, both managed effectively. Conclusion In the management of proximal humerus fractures, JESS fixation and PHILOS plating are equally effective. This study also led us to the conclusion that JESS fixation for proximal humerus fractures is a semi rigid, inexpensive technique that permits early mobilization, needs few implants, requires a short hospital stay and surgical period, resulting in good to excellent functional results with a minimal risk of complications.
JESS, PHILOS, proximal humerus, Constant – Murley Scores, osteoporosis
Короткий адрес: https://sciup.org/142246006
IDR: 142246006 | УДК: 616.717.41/.43-001.5-089.227.84:616-089.168 | DOI: 10.18019/1028-4427-2025-31-5-558-566
Текст научной статьи A comparative study between functional outcomes of proximal humerus fracture treated using closed reduction and JESS external stabilization system and open reduction and internal fixation with PHILOS plate at a tertiary health care center
Roughly 5 % of all fractures are proximal humerus fractures, making them common injuries [1]. Their frequency rises with age, especially in individuals over 60 with a female-to-male ratio of 3:1 in this age group [2]. While 15 % of these fractures necessitate surgical intervention because of the substantial displacement of fracture fragments, the majority (85 %) are minimally displaced and manageable non-operatively [3]. Falling on an outstretched arm is the most common cause of proximal humerus fractures, especially in older individuals with osteoporosis [4]. A thorough clinical history is essential, including the patient’s age, hand dominance, mechanism of injury, and injury severity [5]. Additionally, any pre-existing medical conditions, previous shoulder surgeries, and symptoms such as paresthesia, elbow or wrist pain, or functional impairment of the affected limb should be evaluated [6].
Neer CS classified these fractures to determine which cases would benefit from open reduction and which were at higher risk of avascular necrosis, necessitating prosthetic replacement [7]. Successful therapy depends on the correct diagnosis and classification of the fracture [8]. The formation and displacement of fracture fragments depend on the force exerted by muscles attached to the greater and lesser tuberosities and the humeral shaft [9].
The treatment of proximal humerus fractures varies based on fracture severity and patient factors. Conservative management includes the use of a U-slab (hanging cast), a universal shoulder immobilizer (USI), or functional bracing [10]. Surgical alternatives include closed reduction with percutaneous pinning, open reduction with internal fixation utilizing a locked PHILOS plate, trans-osseous suture fixation, intramedullary nailing, hemiarthroplasty, total shoulder arthroplasty, and reverse shoulder arthroplasty [11]. The surgical procedure used is determined by criteria such as fracture type, patient’s age, bone quality, comorbidities, and the surgeon's expertise and preferences [12].
Dr. B.B. Joshi of Bombay devised a highly modular small external fixator device that offers a simple and effective solution for handling difficult upper limb fractures [13]. This method is minimally invasive, has a high safety rating, and enables early physiotherapy [14]. It is simple to use, even in remote locations, and requires little instrumentation, making it a viable alternative to the present treatment options [15].
The purpose of this study is to compare the functional results of proximal humerus fractures treated with PHILOS plating and JESS fixation.
MATERIALS AND METHODS
This prospective observational study was conducted over 24 months and included 36 patients with proximal humerus fractures. Institutional ethics committee approval was obtained, and informed consent was collected from all participants. Patient details were documented using a standardized clinical history proforma at a tertiary care center.
Inclusion Criteria :
-
• Patients with displaced two- or three-part humerus fractures;
-
• Age over 18 years;
-
• Injury that occurred within two weeks before surgery.
Exclusion Criteria :
-
• Pediatric patients with active growth plates;
-
• Open fractures;
-
• Proximal humerus fractures with pre-existing shoulder conditions such as arthritis, rotator cuff tears, or frozen shoulder;
-
• Associated ipsilateral upper limb injuries or fractures;
-
• Cases with neurovascular compromise.
Preoperative evaluation included an assessment of the patient's general health and a thorough examination of the neurovascular status of the upper extremity. Radiographic evaluation consisted of anteroposterior and axillary views of the shoulder and a CT scan for detailed fracture visualization.
Surgical Procedure
Joshi External Stabilizing System (JESS)
The surgical technique was carried out under general or local anesthesia, with the patient lying supine and a sandbag used to elevate the shoulder. We used 2.5-mm pins. The greater tuberosity pins posed a risk to the axillary nerve and the posterior humeral circumflex artery. In contrast, the proximal lateral pins posed a risk to the anterior branch of the axillary nerve. Additionally, the cephalic vein, biceps tendon, and musculocutaneous nerve were at risk during anterior pin implantation. The greater tuberosity pins were inserted with the shoulder externally rotated to reduce danger, moving the axillary nerve and posterior circumflex artery away from the humeral neck. Three pins were placed into the humeral head at 30° intervals in the same horizontal plane: one just lateral to the bicipital groove, another in the appropriate lateral plane, and a third posterior to the central one. Two more wires were inserted into the shaft near the greater tuberosity. These fixator wires functioned as joysticks to aid with reduction before attaching the frame. The purpose of reduction was to re-establish proper alignment, with an angulation of less than 45° and displacement of less than 1 cm.
After reduction, beta clamps were used to secure each pin to the external fixator bars, resulting in a stable construction. On the first day following surgery, patients were advised to start actively mobilizing the afflicted extremity while wearing a triangle sling for comfort. After evaluating radiological union and functional improvement, the external fixator was removed.
PHILOS (Proximal Humeral Internal Locking System) Plate Fixation
In this technique, a “beach chair” position was given to the patient after general or regional anaesthesia. A single preoperative dose of 1.5 grams of Cefuroxime was administered intravenously at the initiation of anaesthesia. Surgical landmarks for the deltopectoral approach were marked. A 10-cm incision from the coracoid process to the shaft of the humerus was taken. The conjoint tendon retracted medially to allow access to the fracture site.
With the help of an image intensifier, the fracture fragments were directly reduced, and K-wires were used for the temporary fixation of these fragments. Ethibond No 5 was also used for manipulation of the proximal fracture to aid in reduction. After confirmation of fracture reduction, the PHILOS plate was positioned. Care was taken to position this plate at least 8 mm distal to the upper end of the greater tuberosity using an insertion guide. The biceps tendon was also used to guide for plate positioning. To avoid tendon impingement, the plate was positioned laterally to the long head of the biceps tendon. The locking screws were used to secure the humeral head fragment and metaphyseal shaft. The appropriate-length locking screws were inserted using a specially designed star drive screwdriver. The anteroposterior and axillary views were taken using an image intensifier for the final confirmation of fracture reduction and plate positioning. Before the procedure was completed, the stability, range of motion, and absence of impingement were evaluated intraoperatively. Following surgery, all patients were placed in either a sling or an abduction brace for support.
Postoperative Protocol
Following surgery, physical therapy was started right away on the next day. It started with pendulum exercises, passive forward flexion, and external rotation exercises, and advanced to unrestricted range of motion by 6–7 weeks. Exercises including active range of motion and active assistance were recommended. Patients were monitored for clinical and radiological union at 4, 8, and 12 weeks.
Outcome Assessment
Functional outcomes were assessed using the Constant-Murley Score (CMS), a 100-point scale evaluating pain levels and the patient’s ability to perform daily activities [15]. The CMS is interpreted as follows:
-
• 0–55 points = Poor;
-
• 56–70 points = Fair;
-
• 71–85 points = Good;
-
• 86–100 points = Excellent.
Complications, including pin-tract infections, malunion, avascular necrosis, and implant failure, were documented throughout the follow-up period.
Statistical Analysis
Statistical analysis was performed using SPSS software, version 22. Qualitative data were presented as frequency and percentage, while quantitative data were analyzed using a paired t-test. A p -value of < 0.05 was considered statistically significant.
RESULTS
This study included 36 patients. Both groups had a total of 18 patients each. In the JESS group, there were eight males (44.44 %) and 10 females (55.55 %), while in the PHILOS group there were 15 males (83.33 %) and three females (16.67 %). The mode of injury in the JESS group was fall in 13 cases (72.22 %) and road traffic accidents in five cases (27.78 %), whereas in the PHILOS group, eight cases (44.44 %) were due to falls and 10 cases (55.55 %) resulted from road traffic accidents. Neer’s classification showed seven two-part (38.90 %) and 11 three-part (61.10 %) fractures in the JESS group, while the PHILOS group had nine two-part (50 %) and nine three-part (50 %) fractures. Both groups had a total of 18 patients each (Table 1).
Table 1
Demographic details
|
JESS ( n = 18) |
PHILOS ( n = 18) |
||||
|
n |
% |
n |
% |
||
|
Male |
8 |
44.44 |
15 |
83.33 |
|
|
Female |
10 |
55.55 |
3 |
16.67 |
|
|
Mode of injury |
Fall |
13 |
72.22 |
8 |
44.44 |
|
Road traffic accident |
5 |
27.78 |
10 |
55.55 |
|
|
Neer’s type |
2 parts |
7 |
38.90 |
9 |
50 |
|
3 parts |
11 |
61.10 |
9 |
50 |
|
In the JESS group, the mean Constant-Murley Score increased from 29.02 before surgery to 60.27 at four weeks postoperatively, 70 at eight weeks postoperatively, and 82.33 at 12 weeks postoperatively. Similarly, in the PHILOS group, the mean Constant-Murley Score increased from 32.12 preoperatively to 55.82 at four weeks postoperatively, 66.76 at eight weeks postoperatively, and 77.06 at 12 weeks postoperatively. When comparing preoperative assessments with postoperative scores at 4, 8, and 12 weeks, the p -value for both groups was less than 0.005, suggesting a highly significant improvement (Table 2).
Table 2
Constant Murley Score at a regular interval
|
Constant Murley Score |
|||||||||
|
Technique |
Pre-op |
Post-op 4 weeks |
Post-op 8 weeks |
Post-op 12 weeks |
P -value |
||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
||
|
JESS |
29.22 |
5.58 |
60.27 |
8.04 |
70 |
8.6 |
82.33 |
11 |
< 0.001 |
|
PHILOS |
32.12 |
5.02 |
55.82 |
5.04 |
66.76 |
7.88 |
77.06 |
11.42 |
< 0.001 |
In the JESS fixation group, there were three cases of complications: one case of avascular necrosis of the humeral head (successfully treated with hemiarthroplasty), one case of malunion (without significant impact on the functional outcome), and one case of pin-tract infection (successfully managed with daily dressing and oral antibiotics). On the other hand, with PHILOS fixation, there were two complications: one case of avascular necrosis (treated with hemiarthroplasty) and one case of implant failure (screw backout) (Table 3).
Table 3

Fig. 1. Pre-op JESS
Complications
|
Technique |
Implant failure |
Malunion |
Avascular necrosis |
Infection |
None |
|||||
|
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
|
|
JESS ( n = 18) |
0 |
1 |
5.55 |
1 |
5.55 |
1 |
5.55 |
15 |
83.33 |
|
|
PHILOS ( n = 18) |
1 |
5.55 |
0 |
1 |
5.55 |
0 |
16 |
88.88 |
||
Fig. 2. Post-op JESS

Fig. 3. 12 weeks post-op JESS
Fig. 4. Pre-op PHILOS
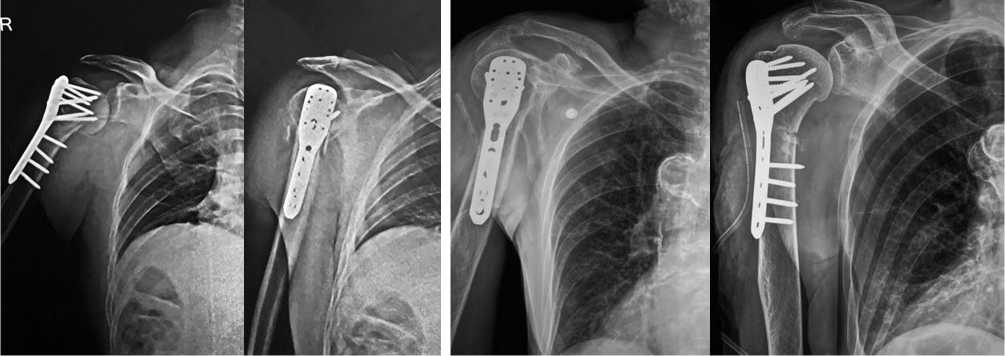
Fig. 5. Post-op PHILOS
Fig. 6. 12 weeks Post-op PHILOS
DISCUSSION
Proximal humerus fractures are rather common in the elderly, and there are numerous treatment options for closed fractures. These options range from minimally invasive percutaneous pinning to hemiarthroplasty, and each has pros and downsides. One main disadvantage of non-operative treatment is delayed mobilization, which frequently results in joint stiffness. Additionally, conservative treatment increases the risk of malunion or nonunion of fractures.
Joshi External Stabilization
In our research, the application of an external fixator system facilitated satisfactory bone healing, accompanied by favourable to outstanding functional results. The procedure generally took less time, under 30 minutes, was economical, and utilized minimal resources. Despite the suboptimal anatomical reduction achieved through this percutaneous fixation method, the functional results remained favorable. These findings are supported by multiple studies. Some techniques incorporate a locking mechanism attached to the pins to prevent migration while operating on the same principle as percutaneous fixation. Additionally, the mutual connection of K-wires generates extra valgus force, counteracting the deforming forces exerted by the supraspinatus and deltoid muscles. However, further biomechanical studies are needed to validate this claim.
Another approach, known as the "hybrid technique", involves initial open reduction followed by stabilization with K-wires and an external fixator [16]. While this method yields comparable functional and radiographic results, it is associated with wound healing complications.
Our study included eight female and ten male patients, with a mean age of 61 years. All patients underwent surgery within three days of injury, and the procedure took less than 30 minutes, with minimal to no blood loss. Postoperatively, active-assisted shoulder flexion and extension exercises, along with wrist and elbow range-of-motion exercises, were initiated on the first day. Patients were advised to maintain upper limb exercises and perform external fixator care at home. Follow-up assessments were conducted at four, eight, and twelve weeks.
A steady improvement in functional outcomes, as assessed by the Constant – Murley Score, was observed: 60.27 at four weeks, 70.00 at eight weeks, and 82.33 at twelve weeks. Complications such as avascular necrosis, pin-tract infection, and malunion were rare, with only one case of each; all of which were successfully treated. A.K. Gupta et al. [17] found that in their research of JESS fixation, the average postoperative VAS score was 2.1 (± 0.73), while the Constant Score averaged 78.1 (± 9.61) over a follow-up period of six months. The average time required for union was 6.5 (± 1.18) weeks. Reported complications included one instance of K-wire loosening and one occurrence of pin tract infection.
T. Goyal et al. [18] in their study found that the mean preoperative Constant-Murley Score was 29.09, which improved to 60.39 at four weeks postoperatively, 69.97 at eight weeks postoperatively, and 79.64 at twelve weeks postoperatively. Similarly, P.R. Kandel et al. [19] reported comparable results and concluded that surgically treating displaced proximal humerus fractures with JESS leads to good functional and radiological outcomes. It results in less pain, reduced stiffness, and greater range of motion (ROM). Consequently, the JESS fixator serves as an economical and effective alternative treatment for proximal humerus fractures, presenting minimal complications.
Internal Fixation with Locking Plates
Historically, internal fixation using non-locking plates was associated with high failure rates and unsatisfactory clinical outcomes. Pre-contoured anatomical locking compression plates offer greater adaptability and higher union rates, particularly in osteoporotic bone [20]. Regardless of the fixation method, fracture reduction remains critical for optimal surgical outcomes. Proper plate positioning is equally important, as even minor displacement can result in shoulder impingement. According to AO-OTA principles, the upper edge of the plate should be placed 5–8 mm distal to the greater tuberosity to avoid impingement.
Our study included fifteen male and three female patients, with a mean age of 48 years. Physiotherapy was initiated in the second postoperative week, beginning with passive-assisted range-of-motion exercises, followed by active exercises starting from the third week. Follow-up assessments at four, eight, and twelve weeks showed continuous improvement in functional outcomes, with Constant-Murley Scores of 55.82 at four weeks, 66.76 at eight weeks, and 77.06 at twelve weeks.
Despite the advantages of locking plates, they are associated with complications such as plate breakage, screw cutout, avascular necrosis, varus malreduction, and the need for revision surgery. R. Jhamnani et al. [21] studied 32 proximal humerus fractures treated with PHILOS plating, reporting excellent outcomes in 62.5 %, satisfactory in 21.87 %, poor in 9.38 %, and failure in 6.25 %. Two-part fractures had better results than three-part fractures. Complications were minimal, with 65.6 % showing stiffness, malunion (9.38 %), and avascular necrosis (6.25 %) were noted. In the study by P. Spolia et al. [22], the mean Constant – Murley Score at six months was 79.4 (range: 38–92). Among 30 patients, 40 % had excellent, 30 % good, 20 % moderate, and 10 % poor outcomes. One four-part fracture had the lowest score (38). Complications (16.7 %) included varus malunion, avascular necrosis, and stiffness. A similar study was done by P. Ethirajk et al. [23], on 40 patients and reported that the functional outcome was found to be excellent in 2 patients (5 %), good in 22 patients (55 %), fair in 7 patients (17.5 %), and poor in 9 patients (22.5 %). The mean Constant – Murley score achieved was 68.75 ± 14.03.
In our study, the screw cutout (implant failure) rate was significantly lower at 5.55 %. In a study by K.C. Owsley et al. [24], involving 53 patients, the screw cutout rate was reported to be 23 %, identifying it as a leading cause of revision surgery. C. Doshi et al. [25] also reported 5.66 % screw cutout rate in their study. Another long-term complication observed in comminuted three- and four-part fractures is avascular necrosis, which typically develops years after fixation and can compromise functional outcomes. We encountered avascular necrosis in 5.55 % of cases. E.V. Geiger et al. [26] reported 7.28 % cases of avascular necrosis in their study on 28 patients. A. Kaushal et al. [27] showed 2.5 % cases of avascular necrosis following PHILOS plating.
Alternative Surgical Approaches
Hemiarthroplasty and reverse total shoulder arthroplasty are viable alternatives, particularly for complex fractures. However, these procedures require advanced surgical skills and tertiary healthcare facilities, which are often inaccessible in our country. A more biological approach has been proposed, though it poses risks to the articular cartilage and is commonly associated with persistent shoulder pain. Intramedullary nailing is another technique preferred by some orthopaedic surgeons.
The main limitation of this study was a relatively small sample size. A larger randomized controlled trial comparing various fixation techniques would provide more comprehensive insights into this treatment approach.
CONCLUSION
This study concluded that both techniques, JESS fixation and PHILOS plating, are equally effective in treating proximal humerus fractures in terms of functional outcome. This study also led us to the conclusion that JESS fixation for proximal humerus fractures is a semi-rigid, inexpensive technique that permits early mobilization, needs few implants, requires a short hospital stay and surgical period, resulting in good to excellent functional results with a minimal risk of complications.
Conflict of interest The authors have no conflicts of interest to declare.
Funding source There is no funding source for the research work.
Ethics approval Ethics committee approval was taken from the institutional Ethics committee.
Consent for publication Consent was taken from all the participants.
Availability of data and materials The datasets used in and/or analyzed in the current study are available from the corresponding author upon reasonable request.
The manuscript was read and approved by all the authors.


