A protocol for customization of protective mouth guards for athletes undergoing strenuous exercise
Автор: Shemonaev V.I., Rudova Ju.V., Stepanov V.A.
Журнал: Человек. Спорт. Медицина @hsm-susu
Рубрика: Спортивная тренировка
Статья в выпуске: 1 т.21, 2021 года.
Бесплатный доступ
Aim: to develop a protocol for customization of protective mouth guards for athletes undergoing strenuous exercise and to provide substantiation for the protocol being developed. Materials and methods. We analyzed clinical data and findings obtained from a dynamic follow-up of 50 light heavyweight (74-87 kg) males (age range 25-44). The participants were divided into 2 groups based on the method used for fabricating protective mouth guards. In the first group, the protective mouth guard was fabricated using a vacuum-forming technique with the mandible being in the centric occlusion. In the second group, a custom vacuum formed protective mouth guard was used and the bioelectrical activity of the masticatory muscles and the position of the temporomandibular joint (TMJ) were evaluated. Results. We evaluated the efficacy of protective mouth guards in athletes of the first group and found a reduction in the bioelectrical activity of masticatory muscles with insignificant variations. In the athletes of the second group, the function of the masticatory and temporal muscles was balanced, the muscle electrical activity was stabilized and muscular synchrony was achieved after mouth guard wear. Conclusion. A protocol for customization of protective mouth guards for athletes undergoing strenuous exercise was developed. Our findings show that wearing custom-made mouth guards during strenuous exercise plays a role in regulating bioelectrical activity and maintaining the synchrony of masticatory muscles which is confirmed by electromyography (EMG) of masticatory and temporal muscles and computed tomography of the TMJ.
Protective mouth guards, emg of the masticatory muscles, masticatory muscledeprogramming
Короткий адрес: https://sciup.org/147231903
IDR: 147231903 | УДК: 796.012.453 | DOI: 10.14529/hsm210119
Текст научной статьи A protocol for customization of protective mouth guards for athletes undergoing strenuous exercise
Athletes who exercise strenuously during a workout or a sporting event are required to utilize custom protective devices to provide protec- tion to the body. Also, the need for specific trauma treatment planning strategies that support the individual’s recovery is anticipated.
Protective mouth guards which are nowadays worn by athletes can be standard over-the-counter (OTC) mouth guards and custom-made which are an exact fit to the mouth. The latter can only imitate tooth morphology; however, bioelectrical activity of the masticatory muscles and the position of the TMJ are not considered when fabricating custom mouth guards. This often leads to adjustable remodeling of the muscular, connective and bone tissue, morphological changes in the disc, articular surfaces, intraarticular ligaments and the retrodiscal (bilaminar) zone of the TMJ [7, 8].
Protective mouth guards fabricated using precise measurements of the muscular and articular structures appear to be the most effective in protecting from orofacial traumatic injuries. They have been shown to impact positively an indivi- dual’s ability to balance and contribute to increased oxygenation of muscles and the brain. In order to achieve this, it is necessary to determine the optimal position of the mandible, i.e. when the condyles are positioned centrally in the glenoid fossa, muscle activity is balanced and the mandible can move smoothly and freely. However, exposure to chronic stress as well as increased activity of the masticatory muscles can make it difficult to achieve this. Poor masticatory muscle performance, in its turn, tends to result in the shift of the mandible in relation to three rotations (+pitch, roll, and yaw). The mandibular functional shift is accompanied by occlusal imbalance and TMJ disorders. Subsequently, the antagonistic teeth and TMJ components undergo a compensatory adaptation to the mandibular changes. Deprogramming devices make it possible to stabilize masticatory muscle activity, to examine and record using a quick-setting recorder the spatial position of the mandible in which orofacial muscles are balanced [3, 9, 10].
The purpose of the study is to develop a protocol for customization of protective mouth guards for athletes undergoing strenuous exercise and provide substantiation for the protocol being developed.
Materials and methods. The work was performed at the Department of Prosthetic Dentistry with a Clinical Dentistry Course at the Volgograd State Medical University.
We analyzed clinical assessment data and findings obtained from dynamic follow-up of 50 light heavyweight (74–87 kg) males (age range 25–44).
The participants were divided into two groups. All mouth guards used by the participants in group 1 (n = 25) were fabricated using a vacuum-forming technique when the mandible was in the habitual occlusion. In group 2, a custom vacuum formed protective mouth guard was used and we also measured the bioelectrical activity of the masticatory muscles and evaluated the spatial position of the TMJ components.
We used interference EMG to identify bioelectrical activity imbalance of masticatory and temporal muscles. We recorded the bioelectrical activity of the masticatory and temporal muscles in athletes of the first and second groups at baseline and after mouth guard wear. The obtained findings were compared with the normal amplitude values of EMG masticatory and temporal muscle activity. Prior to the fabrication of the mouth guard for athletes in Group 2, an anterior Lucia jig deprogrammer was made using Refine Bright cold-cure acrylic resin. The study participants had to wear the anterior deprogrammer for 15 minutes.
As a result of the repeated contraction and relaxation, masticatory muscles relax and defense reflexes are no longer transferred to the brain, thus the mandibular condyles taking a more physiological position. We define this position as the ‘myocentric position of the mandible’ and we used this position when constructing the athletic mouth guards.
All the participants underwent computed tomography of the TMJ in the centric occlusion at baseline and after 1 month of mouth guard wear. We measured the width of the anterior, superior and posterior joint spaces using the method suggested by N.A. Rabukhina.
Discussion and Results. The maximum amplitude values of the masticatory and temporal muscle activity were determined in the study participants at baseline and after 1 month of mouth guard wear. The EMG activity of masticatory and temporal muscles in the athletes of the first and second groups was interfered. However, the use of athletic mouth guards in the first group showed a reduction in masticatory muscle bioelectrical activity, with insignificant activity remaining after mouth guard wear. The athletes of the second group demonstrated a functional balance of masticatory and temporal muscles, stabilization of the muscle electrical activity and muscular synchrony (Fig. 1).
In order to assess the anatomic topography of the TMJ components, the study participants underwent CT scanning of the joints. CT examination of the TMJ components demonstrated that all study participants (Group 1 and 2) had signs of TMJ disorders. In Group 1, all measurements were performed at baseline and after mouth guard wear. In Group 2, all measurements were performed prior to masticatory muscle deprogramming and after mouth guard wear (Table 1).
CT imaging of the TMJ showed that the values of the joint space width in athletes of Group 2 reached the means of the normal distribution as compared to the athletes in Group 1 suggesting that masticatory muscles should contract in consistent synchrony and the myocentric position of the mandible should be identified.
^ (д I) of masticatory and temporal muscles
S. m asset erat rest; 25,8
D. temporalisatrest;
S. temporalis during exercise; 360,1
D. masseter during exercise; 386,1
D. temporalisduring exercise; 359,2
S. tem poralisat rest;
34,2
D. masseter at rest;
26,3
S. masseter during exercise; 384,9
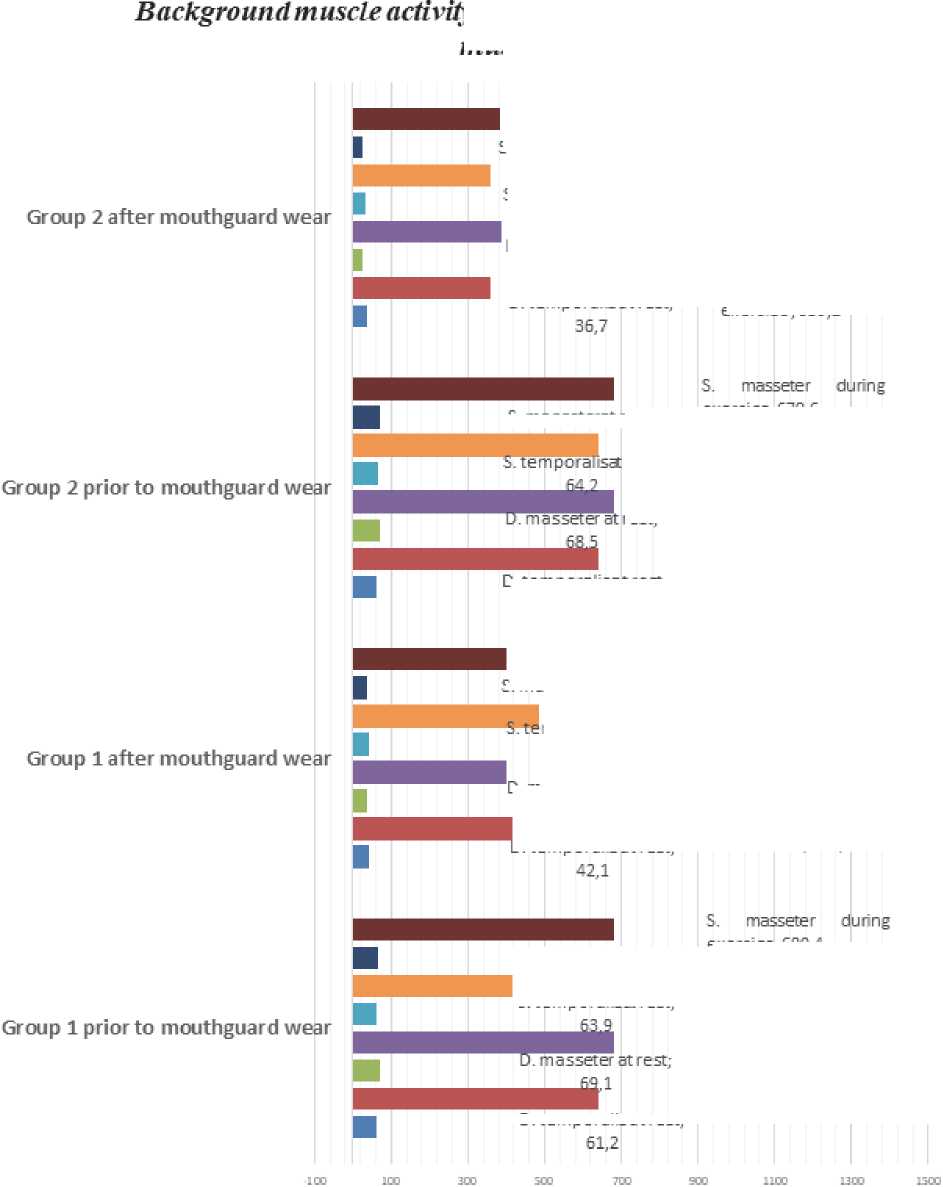
S. masseterat rest; 67,8
D. masseter during exercise; 683,2
D. temporalisduring exercise; 638,8
D. masseter during exercise; 401,1
D. temporalisduring exercise; 489,1
exercise; 680,4
S. temporalisduring exercise; 639,2
mporalisarest;
40,1
□. masseter at rest;
38,2
D. tem poralisat rest;
62,1
S. masseter during exercise; 399,4
S. temporalisduring exercise; 487,7
Fig. 1. Background muscle activity (μV) of masticatory and temporal muscles
S. masseterat
|
rest; 68,8 |
exercise; S. tempo |
679,6 iralisduring |
|
: rest; |
exercise; 639,1 |
|
|
rest; |
D. masseter during exercise; 680,2 |
|
D. temporalisduring exercise; 642,1
S. masseterat rest; 36,1
. temporalisat rest;
Ttemporalisat rest;
D. temporalisatrest;
TMJ joint space measurements (M ± m)
Table 1
|
TMJ spaces |
Group1 |
Group 2 |
||||||
|
At baseline (mm) |
After 1 month of mouth guard wear (mm) |
At baseline (mm) |
After 1 month of mouth guard wear (mm) |
|||||
|
D |
S |
D |
S |
D |
S |
D |
S |
|
|
Anterior |
3.1 ± 0.02 |
3.2 ± 0.12 |
2.9 ± 0.02 |
2.8 ± 0.12 |
3.2 ± 0.02 |
3.1 ± 0.12 |
2.3 ± 0.12 |
2.2 ± 0.02 |
|
Superior |
2.5 ± 0.12 |
2.6 ± 0.02 |
3.1 ± 0.12 |
3.0 ± 0.02 |
23 ± 0.02 |
2.4 ± 0.21 |
3.4 ± 0.21 |
3.3 ± 0.15 |
|
Posterior |
2.3 ± 0.21 |
2.4 ± 0.02 |
3.0 ± 0.02 |
3.1 ± 0.02 |
2.3 ± 0.02 |
2.2 ± 0.15 |
3.5 ± 0.3 |
3.4 ± 0.4 |
Assessment of muscle function and position of the TMJ
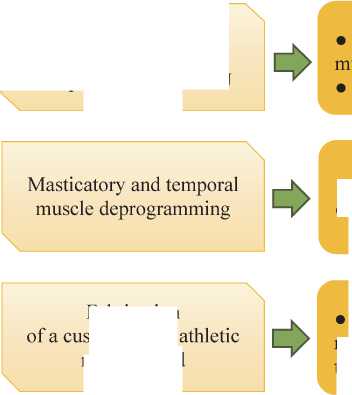
EMG of the masticatory and temporal
CT imaging of the TMJ
• Utilization of an anterior Lucia jig deprogramming device
Fabrication >tom-made mouth guard
Fig. 2. A protocol for customization of protective athletic mouth guards
Fabrication of a custom-made athletic mouth guard using a vacuum-forming technique
Conclusion. Today, high levels of stress and emotional load have become an inescapable part of sport at the elite level . Stress is also an inescapable part of our daily lives. Unfortunately, exposure to stress often exceeds the adaptive capacity of an organism.
The choice of an athletic mouth guard depends on a few factors including occlusal characteristics, topographic anatomy of the mouth as well as position of the mandibular condyles in the glenoid fossa. An athletic mouth guard fabricated when the mandible is positioned myocentrically contributes to a reduction in the amplitude of the bioelectrical activity of masticatory and temporal muscles. Also, protective mouth guards help to synchronize and stabilize the functioning of the orofacial muscles which is confirmed by electromyography of the masticatory muscles and CT scan of the TMJ. Differences in the right and the left temporomandibular joint space are caused by hyperactivity of the masticatory and temporal muscles. When the amplitude of the masticatory and temporal muscle bioelectrical activity is normal, the TMJ components are optimally positioned in the glenoid fossa. This allows the mandible to go to the myocentric position which is important for fabricating a custom-made athletic mouth guard.
Based on our findings we developed a protocol for customization of protective mouth guards for athletes undergoing strenuous exercise (Fig. 2).
The use of the protocol for customization of athletic mouth guards makes it significantly possible to normalize and synchronize the functioning of masticatory muscles which is confirmed by EMG of the masticatory muscles and CT scan of the TMJ.
Список литературы A protocol for customization of protective mouth guards for athletes undergoing strenuous exercise
- Ашуев, Ж.А. Медико-социальная деятельность при заболеваниях и травмах челюстно-лицевой области / Ж.А. Ашуев, А.А. Базиев, А.Е. Лаптева // Вестник Всероссийского общества специалистов по медико-социальной экспертизе, реабилитации и реабилитационной индустрии. - 2015. - № 4. - С. 12-20.
- Боян, А.М. Эффективность различных методов расслабления жевательных мышц у больных с мышечно-суставной дисфункцией височно-нижнечелюстных суставов / А.М. Боян // Вестник стоматологии. - 2017. - № 1 (98). - С. 30-36.
- Fabio Savastano. Neuromuscular Dentistry: Use and Abuse / Fabio Savastano // EC Dental Science. - 2019. - Vol. 18. - P. 2-3.
- Хорев, О.Ю. Окклюзионные интерференции и нейромышечная дисфункция / О.Ю. Хорев, Ю.Н. Майборода // Кубанский научный медицинский вестник. - 2017. - Т. 24. - № 6. - С. 161-167.
- Копецкий, И.С. Роль индивидуальных защитных зубных капп в профилактике спортивного травматизма челюстно-лицевой области / И.С. Копецкий, Ю.Л. Васильев // Dental Forum. - 2016. - № 3. - С. 32-34.
- Ретинский, Б.В. Индивидуальные защитные шины и спортивные каппы для спортсменов / Б.В. Ретинский // Символ науки. - 2016. - № 8-1 (20). - С. 195-199.
- Use of electromyography in dentistry - an overview with meta-analysis / N. Shamima, B. Rehana, A. Mohammad Khursheed // European Journal of dentistry. - 2016. - P. 419-426.
- Слюсар, О.И. Профилактика травм челюстно-лицевой области у спортсменов с применением индивидуальных капп / О.И. Слюсар, И.С. Копецкий, Ю.Л. Васильев // Современные проблемы науки и образования. - 2016. - № 3. - С. 92.
- Закарян, Г.А. Cравнительный анализ и способы изготовления защитных спортивных капп и шин для спортсменов / Г.А. Закарян // Современные научные исследования и инновации. - 2016. - № 9 (65). - С. 452-459.
- Закарян, Г.А. Спортивные защитные каппы / Г.А. Закарян // Символ науки. - 2016. - № 9-2 (21). - С. 140-146.


