An innovative solution to the problem of hypertension
Автор: Yakushin M.A., Yakushina T.I., Kudrin A.P., Vorobeva A.V., Vasiliev M.D., Gabrielyan A.R.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 31, 2024 года.
Бесплатный доступ
The results of the study of hemodynamic parameters in individuals of different age groups, the patterns of their age dynamics and the peculiarities of their influence on the formation of arterial hypo- and hypertension are presented. Based on the systematization of the profiles of systemic hemodynamics, clarifications in the pathogenesis of arterial hypertension are proposed. The rationale for an innovative approach to the choice of antihypertensive therapy, depending on the personal profile of hemodynamic parameters, is given.
Arterial hypertension, systemic hemodynamics, profile of systemic hemodynamics, volumetric compression oscillometry, antihypertensive drugs
Короткий адрес: https://sciup.org/148328855
IDR: 148328855 | DOI: 10.18137/cardiometry.2024.31.5462
Текст научной статьи An innovative solution to the problem of hypertension
Mikhail Yakushin, Alexey Kudrin, Anna Vorobeva, Mikhail Vasiliev, Artur Gabrielyan, Tatiana Yakushina. An innovative solution to the problem of hypertension. Cardiometry; Issue 31; May 2024; p. 54-62; DOI: 10.18137/cardiometry.2024.31.5462; Available from:
The situation with the treatment of arterial hypertension (AH), despite the successes in the development of effective antihypertensive drugs (AHD), continues to deteriorate. Incidence of AH, which already covers more than a third (30-45%) of the adult population, increases by about 1% annually, rapidly spreading to younger and, especially, older age groups [1,2]. The consequences of such expansion negatively affect mortality from cardiovascular diseases (myocardial infarction, stroke, coronary heart disease, chronic heart failure), for which AH is the leading risk factor and the cause of premature death of ten million people per year [3, 4].
There is a clear stagnation in established approaches to the management of AH. The updated European Clinical Guidelines on Arterial Hypertension (ECG), which are usually replete with fresh ideas, in addition to detailing previously proposed positions and “cosmetic” treatment tips, have not undergone significant changes compared to the previous version. The scheme of choosing AHD remained the same: drug combinations should include an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker in combination with a dihydropyridine calcium antagonist or diuretic [5-7].
As before, when choosing medicines, it is necessary to focus on concomitant diseases and prescribe such drugs that have the most evidence-based effectiveness for these diseases. In case of inefficiency, it is proposed to extensively change appointments, switching to combinations of three (this was the case until 2023), four or more (this is an innovation) AHD1.
The reason for the unsatisfactory treatment results is traditionally shifted by the ECG developers to doctors and patients: the former allegedly prescribe low doses of drugs and poorly control treatment, the latter do not fulfill medical appointments. “Strategists” claim that the technology they have developed for the treatment of AH, with full compliance with all recommendations, works flawlessly. As proof, there is a reference to our own research, which showed that “the implementation of the concept of using a triple (and now a quadruple or more) combination of AHD leaves only 5% of patients uncontrolled,” which represents the frequency of occurrence of true resistant (uncontrolled) hyperten-sion2. Such calculations are “broken down” into real indicators of the effectiveness of hypertension treatment, which, according to the highest estimates, does not exceed a third of all sufferers of this disease [8].
An analysis of the negative results of treatment indicates that one of the main causes of a persistent increase in blood pressure (BP) is a change in the ratio of systemic hemodynamics (SH). In domestic clinical recommendations (CR), SH telemonitoring is presented as a necessary element to improve the effectiveness of hypertension treatment; however, there is no regulation of the choice of AHD based on the state of SH in the CR [9,10].
The need to study SH in hypertensive patients seems quite justified, given that hypertension is usually accompanied by various kinds of hemodynamic disorders: spasm or dilation of blood vessels, a disorder of cardiac activity. According to the basic law of hemodynamics, systemic arterial pressure (SAP), which approximately corresponds to the blood pressure in the proximal aorta, is a derivative of the minute heart rate (HR), total peripheral vascular resistance (TPVR) and stroke volume of the heart (SVH):
SAP = HR * TPVR * SVH
Thus, the degree of deviation of HR, TPVR and SVH, on the one hand, the rate of progression of the disease, on the other, the effectiveness of the therapy [11,12].
The introduction of hemodynamic studies into the practice of hypertension is hampered by technical difficulties. Until recently, the Swann—Ganz pulmonary artery catheterization, which is 2-3% complicated by cardiac arrest, was considered the “gold standard” for measuring SVH and TPVR. An alternative method, compression oscillometry (CO), despite the advantageous non-invasive research format, has relatively recently entered the practice of healthcare and is still used in an experimental format [13].
We applied this technique in order to study the age-related features of hemodynamics and establish hemodynamic patterns of hypertension.
MATERIAL AND METHOD
Patients (n=294; including 117 men and 177 women aged 10 to 88 years) were grouped into 3 groups;
group I included “normotonics” – patients with blood pressure within 100-139/60-89; group II – “hypotonics” – patients with blood pressure below 100/60; group III – “hypertensive” (BP >140/90).
Since the values of SVH and TPVR depend on the height and weight of the patient, in our calculations we used their integral analogues: Ii (impact index), calculated as SVH/T, where T is the surface area of the human body (m2) and SPVR (specific peripheral vascular resistance), equal to TPVR/T. The standard value of Ii is 30-45 ml/ m2, SPVR is 32 ± 6% of the standard units. For normal HR, we took 60-80 beats per 1 min. We have designated the ratio HR, SPVR, Ii by the term “Profile”.
During the research, the device CAP TSG osm – “GLOBUS” was used – manufacturer Globus LLC; registration certificate dated 12/15/2017 No. RZN2017/6582.
RESULTS
During the examination of patients, 16 variants of the ratio HR, Ii and SPVR were revealed; each variant of the Profile of these indicators was designated by a combination of three digits: the first digit shows the heart rate level (1 – above normal, 2 – normal value; 3 – below normal), the second – the level of SPVR, the third – the level of Ii (Fig.1).
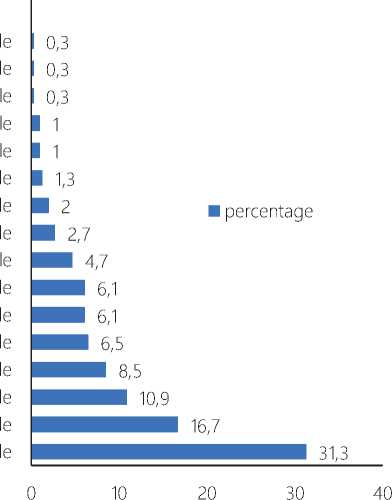
322 profi 223 profi 131 profi 113 profi 121 profi 331 profi 212 profi 321 profi 112 profi 132 profi 123 profi
231 profi 221 profi 232 profi 122 profi 222 profi
Figure 1. Profiles of SH
The normal Profile (222), in which HR, SPVR and Ii correspond to the standard values, was detected in only one third (31.2%) of patients. In 38.6% of cases, a Profile with a single impaired indicator was determined: 122 – 16,6%, 232 – 10,9%, 221 – 8,5%, 212 – 2%, 223 – 0,6%, 322 – 0,6%. A combined deviation of two indicators was observed in 27.8% of patients: 231 – 6,5%, 123 – 6,1%. 132 – 6,1%, 112 – 4,8%, 321 – 2,7%, 121 – 1%, 223 – 0,3%, 322 – 0,3%. Another 3% had all Profile indicators violated: 331 – 1,4%, 113 – 1%, 133 – 0,3%, 131 – 0,3%. Not recorded in any case 111, 133, 211, 213, 233, 311, 312, 313, 332, 333 Profiles, which is probably related to the specifics of the formation of compensatory hemodynamic processes.
In a healthy person, depending on the phase of vital activity (sleep-wakefulness), the level of physical and mental activity (rest-active activity), the indicators of SH can vary in wide ranges; at the same time, the blood SAP it should remain within the limits of regulatory values, ensuring stable blood supply to organs and tissues. Reactive deviations of HR, SPVR and Ii in response to changes in ergo- and trophotropic vital signs are compensatory mechanisms for maintaining the stability of the SAP, which determines the perfusion of oxygen and nutrients. Activation of cardiac activity (tachycardia, increased SVH) is compensated by a decrease in TPVR and vice versa: bradycardia, a decrease in SVH leads to vasospasm and increased TPVR. At the same time, TPVR and SVH are in antagonistic interaction, which is confirmed by the absence of Profiles with their single-vector displacement (111, 211, 311, 133, 233, 333).
Such a “qualitative” mechanism, in which the increase in some indicators is compensated by a decrease in others, reflects the universal process of maintaining a normal blood pressure level. The variety of Profiles is probably explained by the polymorphism of compensatory hemodynamic reactions. The absence of a normal profile in a person with stable blood pressure is not a pathology, but only indicates the consistency of compensatory hemodynamic processes. Figure 2 shows the prevalence of the normal Profile in various age groups. It is noteworthy that the largest proportion of Profiles other than normal (222) is observed in the younger age group (10-19 years). At the same time, in no case was there an increased blood pressure among the patients of this group. This fact indicates that the reason for the Profile change may be not only and not so much organic pathology, but functional disorders of the regulation of cardiovascular activity. Apparently, it is these disorders that determine the specifics of the initial stage and precede the formation of the second stage of hypertension.
It should be noted that the “qualitative” compensation of hemodynamic constants originates in the corridor of normal values; more than half of patients with a normal profile (222) have a deviation of one indicator towards the upper limit of the norm with a simultaneous shift of another indicator to the lower limit of the norm. We have designated this phenomenon by the term subthreshold compensation.
Some diseases of the nervous, cardiovascular, and endocrine systems, due to sympathoadrenal and re-nin-angiotensin-aldosterone stimulation, as well as disorders of carbohydrate and lipid metabolism, lead to deviations of certain parameters of SH. “Qualitative” compensation allows you to level out these deviations, maintaining the SAP within the limits of the
70 (1) ГС? 60
CD 40 Q.
-
■ Impaired profile
-
■ Normal profile
10-19 years old 78,9
21,1
20-29 years old 64,7
35,3
30-39 years old 58,4
41,6
40-49 years old 61
50-54 years old 66,7
33,3
55-59 years old 73,4 26,6
60-64 years old 66,7
33,3
Figure 2. The proportion of the normal profile in different age groups 56 | Cardiometry | Issue 31. May 2024
normative values. The compensation period of the SAP it can last for years; many “normotonics” and “hypotonics”, unknowingly, are “hypertensive” in the initial (latent) stage of hypertension. Indirectly, this is evidenced by a multiple increase in the prevalence of hypertension in the elderly and senile age, as well as a fairly low proportion of people (34%) with a normal profile among “normotonics” (Fig. 3). In the case of an increase in decompensation of cardiac activity and vasomotor regulation of vascular tone, compensatory processes are disrupted, followed by the formation of persistent hypertension (II, Stage III).
133 profile
131 profile
121 profile
113 profile
212 profile
321 profile
112 profile
132 profile
231 profile
123 profile
232 profile
221 profile
122 profile
222 profile
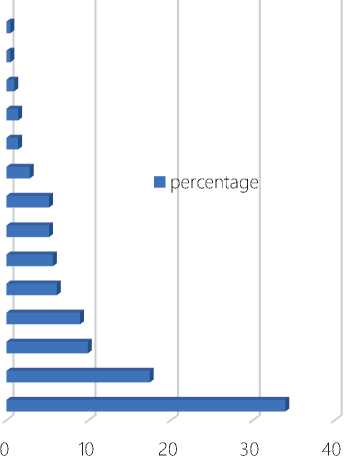
Figure 3. The SH profile of “normotonics”
Among patients of group II (hypotension), the following Profiles were most often determined: normal (27,1%), 232 (22,9%), 122 (12,5%), 123 (10,4%) and 132 (6.25%) (fig. 4).
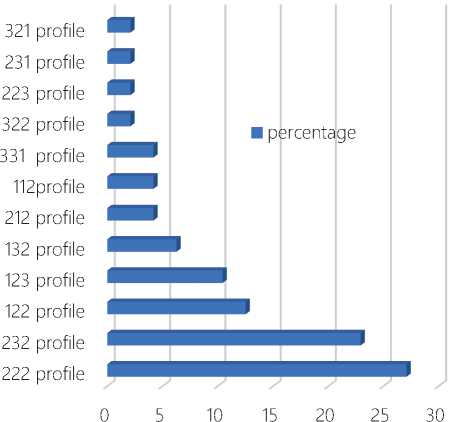
Figure 4. SH profiles for “hypotonics”
Among people with high blood pressure (group III – hypertension), the most common 122 (28,9%), 222 (18,4%), 231 (13,1%), 221 (10,5%) and 132 (7.9%) Profiles (Fig. 5).
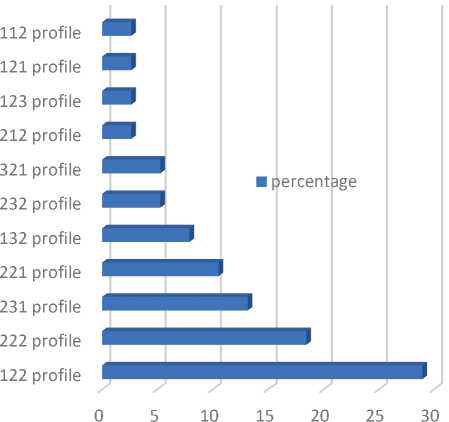
Figure 5. SH profiles for “hypertensive patients”
Attention is drawn to the coincidence of most Profiles in “hypo- and hypertensive patients” (112, 122, 123, 132, 212, 222, 231, 232, 321), this suggests a common pathogenetic processes in arterial hypo- and hypertension (Fig. 3, 4). A distinctive feature of patients with arterial hypotension is the presence of Profiles 223, 322 and 331; in patients with hypertension, in contrast to “hypotonics”, specific Profiles 121 and 221 are revealed [14,15].
To study the patterns of compensatory hemodynamic reactions, we investigated the specifics of Profiles in patients with increased and decreased values of each of its constants.
Hemodynamic compensation for a decrease TPVR in the examined patients was carried out mainly due to an increase in heart rate (87%), less often due to a combined increase HR and SVH (9.7%) (Fig.6).
HR HR HR, and reduc
SVH tion
SVH
■ percentage 87 9,7 3,2
Figure 6. Hemodynamic mechanisms of compensation for a decrease TPVR
The increase TPVR was compensated mainly by a decrease SVH (62.1%), less often (24.3%) due to a decrease HR (Fig. 7).
■ percentage
SVH
62,1
HR
24,3
Figure 7. Hemodynamic mechanisms of compensation TPVR
The decrease in SVH in 27.6% of cases was compensated by an increase in heart rate, in 25.4% – an increase in TPVR, in 40.9% – a combined increase in both indicators (Fig. 8).
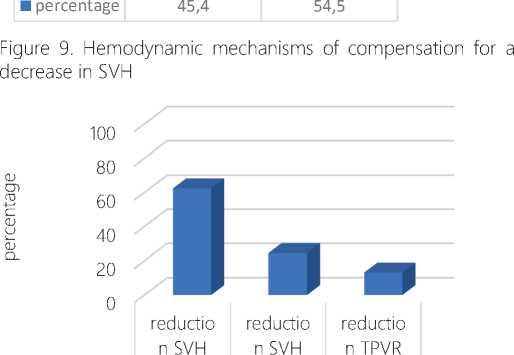
A 45.4% increase in SVH was offset by a decrease in TPVR, and a 54.5% decrease in combined TPVR and HR. It is noteworthy that in no case was compensation provided at the expense of bradycardia (Fig. 9).
increase increase increase d HR and d HR d TPVR
TPVR
40,9
In all patients with bradycardia, a compensatory increase in TPVR; tachycardia was compensated by a decrease in SVH (24.4%) and TPVR (13.2%), but most often (62.4%) – due to a combined decrease in both indicators (Fig. 10).
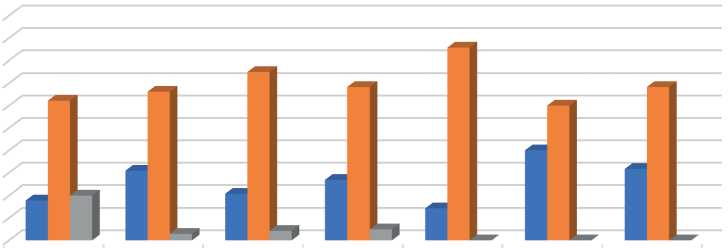
According to the results, the level of each SH indicator changed significantly with age. The maximum proportion of patients with an increased value of TPVR was in the younger age group (10-19 years old). The age group of 50-54 years corresponded to the main proportion of patients with normal TPVR (85.7%); the age group of 55-59 years – the maximum proportion of patients with reduced TPVR (Fig. 11).
■ percentage
27,6
25,4
Figure 8. Hemodynamic mechanisms of compensation for a decrease in SVH
TPVR TPVR and HR
On the contrary, the Ii tended to increase smoothly with age, with a peak of 50-54 years (Fig. 12). The proportion of patients with a reduced value of Ii, conversely, decreased to a minimum value in 50-59 years.
The age–related dynamics of HR had a similar profile with SVH, which gives reason to combine compensatory hemodynamic reactions realized by changing the values of SVH and HR into a single block – compensatory reactions of cardiac output (Fig. 13).
and
TPVR
■ percentage 62,4 24,4 13,2
Figure 10. Hemodynamic mechanisms of tachycardia compensation
DISCUSSION AND CONCLUSIONS
The revealed patterns make it possible to clarify the pathogenesis of hypertension in terms of hemodynamic processes. The increase TPVR and SVH that occur in childhood and adolescence due to functional disorders of the regulation of cardiovascular activity (vegetative-vascular dystonia) is compensated initially by subthreshold compensation, later by a “qualitative” discrepancy in the corresponding indicators: an increase SVH and (or) HR is offset by a decrease TPVR due to subthreshold compensation (Profiles 121 122,
10-19
years old
■ Below the norm 17,8
■ The norm 62,2
■ is above the norm 20
|
20-29 |
30-39 |
40-49 |
|
years old |
years old |
years old |
|
30,9 |
20,8 |
26,8 |
|
66,2 |
75 |
68,3 |
|
2,9 |
4,2 |
4,9 |
|
50-54 |
55-59 |
60-64 |
|
years old |
years old |
years old |
|
14,3 |
40 |
31,7 |
|
85,7 |
60 |
68,3 |
|
0 |
0 |
0 |
Figure 11. Age-related dynamics of the TPVR
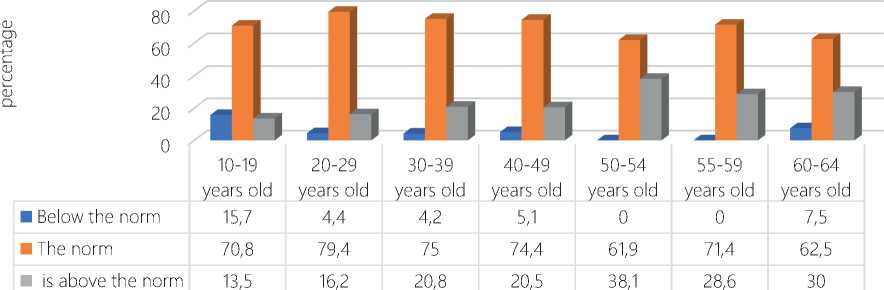
Figure 12. Age dynamics of SVH
|
80 60 0J 40 0J 20 0 |
лши 10-19 20-29 30-39 40-49 50-54 55-59 60-64 years old years old years old years old years old years old years old |
|
■ Below the norm |
4,4 4,4 0 2,4 0 13,3 8,3 |
|
■ The norm |
40,4 63,2 70,8 73,2 71,4 53,3 72,2 |
|
■ is above the norm |
55,2 32,4 29,2 24,4 28,6 33,4 19,5 |
Figure 13. Age-related dynamics of HR
123, 221) or a “qualitative” discrepancy (Profile 132). The listed profiles are united by the hypertensive tendency modulation of SH. In the case of progression of pathological processes, gradual exhaustion occurs, and then a breakdown of compensatory hemodynam- ic processes (Profiles 112, 212, 321, 231), which is clinically manifested by an increase SAP and the formation of persistent hypertension.
In this scheme of the pathogenesis of hypertension, the detection of 222 Profiles in 18.4% of people with elevated blood pressure and, especially, in 5.2% of 232 Profiles does not fit, which contradicts the basic law of hemodynamics, according to which hypertension must correspond to at least one increased indicator of SH! A small proportion of the 222 Profile in “hypertensive patients” can be correlated with a sub-threshold deviation of the SVH, since in a third (28.4%) of patients in this group, the SVH was at the upper limit of the norm, closer to the 221 Profile. However, this argument does not explain the presence of 232 Profiles in “hypertensive patients”.
The explanation for this phenomenon, in our opinion, lies in the basic law of hydrodynamics – Poiseuille’s law, according to which the pressure in a hollow tube is directly dependent on the length of this tube, and, consequently, on the volume of liquid circulating in it. Based on this, it is necessary to introduce another variable into the formula of the basic law of hemodynamics – the volume of circulating blood (VCB). The need to take into account VCB in the management of patients with hypertension is stipulated in CR, however, in practice this study is rarely carried out for technical reasons related to the need for intravenous administration of a special dye, followed by photometric determination of the degree of its dilution in the bloodstream on equipment that is not available in most medical institutions [16-18].
The inclusion of VCB in the formula of the SAP clarifies the possibility of a 232 Profile in “hypertensive patients”; an increase in blood pressure in this case is associated with an increase in BCC. Since an increase in VCB leads to an increase in venous blood return and a reflex increase in cardiac output, Profiles 121, 221, 231 and 321 against the background of increased blood pressure should be considered as an indirect sign of high VCB [11].
Based on the results obtained, we have substantiated the pharmacodynamic principle of choosing antihypertensive therapy. Attempts to use SH indicators as criteria for prescribing medicines have been made repeatedly. L.E. Murashko et al., (2005) proposed to base the choice of vasotropic drugs on the state of central hemodynamics, which, according to the authors, is divided into 3 types: hyperkinetic, eukinetic and hypokinetic3. The hyperkinetic type is characterized by an increase in cardiac output (CO) and a decrease TPVR; hypokinetic – by the inverse ratio (decrease in CO and increase in TPVR); eukinetic – by the normal value of both indicators. In the hypokinetic type, according to the authors, peripheral vasodilators (theonicol, apressin, phentolamine), myotropic antispasmodics (dibazole, papaverine), magnesium sulfate and central alpha-adrenomimetics (clofelin) should be prescribed, since these drugs “increase the cardiac index (CI) and reduce TPVR.”
The principle of correlating hemodynamic constants with the pharmacodynamics of drugs, put forward by L.E. Murashko et al., was used by us to substantiate the method of treating hypertension4. It is possible to restore the normal level of blood pressure by prescribing AHD that have a stabilizing effect on impaired indicators of SH (Table 1).
Table 1. The impact of AHD* on SH indicators
|
group |
systolic arterial pressure |
diastolic arterial pressure |
HR |
TPVR |
SVH |
VCB |
|
BB |
и |
1 |
1 |
TT |
т |
- |
|
АК |
I |
1 |
IT |
т |
- |
|
|
ТД |
I |
1 |
т |
т— |
т |
|
|
iACE |
I |
1 |
т |
т- |
- |
|
|
ARB |
и |
1 |
т |
т- |
- |
*AK – calcium antagonists, BB – beta-blockers, TD – thiazide and thiazide-like diuretics, iACE inhibitors, ARB – angiotensin receptor blockers; ↑ – increase, ↓ – decrease, “-” – no effect.
When choosing AHD, it is necessary to focus on the personal Profile of the patient: the desired drug should have a normalizing effect on each constant of the Profile, including VCB; information on the effect of AHD on SH is contained in the section of the annotation “Pharmacodynamics”. The possibility of modulation with diuretics 232, 222, 121, 221, 231, 321 Profiles belong to the category of assumptions based on the patterns we have identified; these assumptions need evidence-based research.
Table 2. The effect of AHD on the SH profile
|
group AHD |
AHD |
The influence of AHD on SH (Code)* |
|
Calcium antagonists |
Nitrendipine |
312 |
|
Nifedipine |
313 |
|
|
Diltiazem |
112 |
|
|
Amlodipine |
212 |
|
|
ACE inhibitors |
Perindopril, enalapril |
213 |
|
Zofenopril, captopril, lisinopril, lisinopril, ramipril, fosinopril |
212 |
|
|
Beta-blockers |
Betaxolol |
111 |
|
Nebivolol |
112 |
|
|
Atenolol, bisoprolol, metoprolol |
141 |
|
|
Angiotensin receptor blockers |
Losartan |
113 |
|
Valsartan, candesartan, eprosartan, irbesartan, telmisartan |
212 |
|
|
Selective imidazoline receptor agonists |
Moxonidine |
212 |
|
Diuretics |
Dichlotiazide, indapamide |
212, 232, 222, 121, 221, 231, 321 |
*The first component of the code contains information about the effect of AHD on HR (1 – reduces, 2 – does not affect, 3 – increases the value); the second – on TPVR (1- reduces, 2 – does not affect, 3 – increases the value, 4 – increases in the first month, decreases a month later and further); the third one affects the SVH (1 – reduces, 2 – does not affect, 3 – increases the value)
Conflict of Interest the authors declare that there is no conflict of interest.
Список литературы An innovative solution to the problem of hypertension
- Prevalence of risk factors for noncommunicable diseases in the Russian population in 2012-2013. The results of the ESSAY-RF study. Cardiovascular therapy and prevention 2014; 13(6):4-11.
- Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217–223.
- Franklin SS, Lopez VA, Wong ND, et al. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation 2009;119:243–250.
- Williams B, Mancia G, Spiering W et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. JHypertens 2018;36(10):1953–2041.
- Matsuzaki M, Ogihara T, Umemoto S et al. Combination Therapy of Hypertension to Prevent Cardiovascular Events Trial Group. Prevention of cardiovascular events with calcium channel blocker- based combination therapies in patients with hypertension: a randomized controlled trial. J Hypertens 2011;29:1649–1659.
- MacDonald TM, Williams B, Webb DJ et al. British Hypertension Society Programme of Prevention And Treatment of Hypertension With Algorithm-based Therapy (PATHWAY). Combination therapy is superior to sequential monotherapy for the initial treatment of hypertension: a double-blind randomized controlled trial. J Am Heart Assoc 2017.
- Egan BM, Bandyopadhyay D, Shaftman SR et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension 2012;59:1124–1131.
- Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 2009; 27:963–975.
- Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. 2013;31:455-468.
- Duan Y, Xie Z, Dong F, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens. 2017;31:427–437.
- Kubarko, A. I. D. A. Alexandrov, N. A. Basharkevich. Hemodynamics. Functional indicators of blood circulation in questions and answers: studies.- the method. Stipend. BSMU, 2012. – 26 p.
- Tatarkin, A. A. Systemic hemodynamics in patients with hypertension depending on age / A. A. Tatarkin // Collection of scientific theses and articles “Health and education in the XXI century”. – 2008. – Vol. 10, No. 2. – p. 323.
- Intensive care. A guide for doctors edited by V.D. Malyshev.// M.: Medicine, 2002.
- Hirmanov V.N., Tyurina T.V. Blood pressure profile in patients with arterial hyper- and hypotension and the effect of physiological loads on it // Cardiology. – 2002. – Vol. 42, No. 7. – pp. 44-46.
- Kantola I., Terént A., Kataja M., BreigAsberg E. ACE-inhibitor therapy with spirapril increases nocturnal hypotensive episodes in elderly hypertensive patients // J. Hum. Hypertension. – 2001. – Vol. 15, N 12. – P. 873-878.
- Savitsky N. N. Biophysical foundations of blood circulation and clinical methods for studying hemodynamics. L.: Medicine, Leningrad Publishing House; 1974.
- Ignatenko G.A., Mukhin I.V., Ignatenko T.S., Panieva N.Yu., Shcherbakov K.S., Stupakova K.A., Kontovsky E.A., Tumanova S.V., Brova Yu.A., Bryzhataya Yu.O., Rybalko G.S., Gavrilyak V.G., Fedorchenko A.A., Chebotareva E.N. The volume of circulating blood, circulating plasma and total peripheral vascular resistance in hypertensive patients with hypothyroidism. Bulletin of Hygiene and Epidemiology. 2020. Vol. 24. No. 1. pp. 11-14.
- Brin, V.B. Physiology of systemic circulation. Formulas and calculations. / V. B. Brin, B. Ya. Zonis. – Rostov University Press, 1984. – 88 p.


