Anatomical and topographical features of the gracilis muscle of the thigh from the position of using it for autotransplantation
Автор: Gulyaev D.A., Begjanyan A.S., Kaurova T.A., Belov I.Yu., Kurnosov I.A.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 21, 2022 года.
Бесплатный доступ
Autotransplantation of a free flap of the gracilis muscle is currently actively used in reconstructive surgery for persistent prosoplegia, injuries of the brachial plexus, for plastic closure of defects in the upper lip, and in the treatment of pelvic sepsis. This study provides important information about the anatomical features of the gracilis muscle and its neurovascular bundle, which are highly variable. The study of the anatomical and topographic features of this fine thigh muscle was carried out on a sectional study of 25 corpses of both sexes, 50 lower limbs. The present study demonstrates that the median value of the total length of m. Gracilis, the length of its muscular part, as well as the length of the tendon were 452.25 (439.7; 462.0); 225.3(208.1;239.0); 230.5 (213.0; 244.4) mm, respectively. The number of vascular pedicles included in m. Gracilis, ranged from 1 to 5. In 86% of the cases, the deep femoral artery formed the dominant vascular pedicle, and in 14% of cases, it was the medial circumflex artery. Small secondary vascular pedicles originated from the descending genicular artery or the anterior branch of the obturator arter: from the basin of the internal iliac artery. The length of the main feeding artery varied from 76 to 134 mm, the median value was 100.5(90;110) mm, and its diameter ranged from 1.4 to 2.1 mm (M = 1.9(1.8;2, 0) mm. The innervation of the fine muscle of the thigh was carried out by the anterior branch of the obturator nerve, which in 82% of the cases was represented by a single trunk; less often a loose type of structure was observed. The proper nerve was located at a distance of 108.5 (96; 117) mm from the origin of the muscle; its diameter was 2.1 (1.9; 2.2) mm. Knowledge of the topographic and anatomical relationships of the neurovascular bundle with the surrounding formations, variants of its individual anatomical variability are the key to successful reconstructive surgery.
Thigh gracilis muscle, vascular pedicle, obturator nerve, transplantation
Короткий адрес: https://sciup.org/148324174
IDR: 148324174
Текст научной статьи Anatomical and topographical features of the gracilis muscle of the thigh from the position of using it for autotransplantation
Dmitry A. Gulyaev, Arthur S. Begjanyan, Tatiana A. Kaurova, Igor Yu. Belov, Ivan A. Kurnosov. Anatomical and topographical features of the thin muscle of the thigh from the position of using it for autotransplantation. Cardiometry; Issue 21; February 2022; p. 119-123; DOI: 10.18137/cardiometry.2022.21.119123; Available from: anatomical-topographical-features
Transplantation of a free flap of the gracilis muscle is increasingly used in modern reconstructive surgery. This includes prosoplegia of the facial muscles, lesions of the brachial plexus, plastic closure of upper lip defects, and even the treatment of pelvic sepsis. Usually, the surgical technique includes harvesting of the flap with its neurovascular bundle, revascularization using microvascular anastomoses, and reinnervation in order for the transferred gracilis muscle to become functionally significant. Thorough knowledge by the surgeon of the topographic and anatomical relationships of the neurovascular bundle with the surrounding formations and its variants of individual anatomical variability are the key to successful surgical intervention.
M. Gracilis is a thin long muscle located in the medial thigh most superficially relative to other adductor muscles. Its shape is flattened, wide at the top and gradually tapering downwards. It originates from the lower branch of the pubic and adjacent part of the ischial bones, and its tendon connects to the tendons of the sartorius and semitendinosus muscles and is attached to the upper part of the tibia medial to its tuberosity. The thin thigh muscle performs an auxiliary function in hip adduction and flexion, knee flexion, internal rotation of the knee, and therefore can be used as a donor without significant motor deficit, which is quickly and easily compensated by agonist muscles. On the other hand, such characteristics of M. Gracilis as size, shape, length, reliable blood supply to the dominant vascular pedicle provide a good cosmetic result, forming an adequate facial contour, and its innervation by the motor obturator nerve, acceptable muscle strength with a good excursion allow us to hope for a satisfactory functional rehabilitation [1-4]. However, to date, a number of unresolved problems remain associated with impaired blood supply to the transplanted muscle flap, a feature of modeling the muscle flap, “donor zone disease”. A more in-depth study of the anatomical and topographic features of m. Gracilis of its neurovascular bundle will obviously improve the results of surgical treatment of patients with persistent prosoplegia.
Materials and methods
The study of the variability in the structure of the small muscle of the thigh was carried out on a sectional study of 25 corpses of both sexes, 50 lower limbs (12 males and 13 females) on the basis of the patho-anatomical department of the V.A. Almazov National Medical Research Centre of the Ministry of Health of Russia. Criteria for inclusion in the study were the deceased without trauma, tumor, deformities of the medial surface of the thigh; diseases of the musculoskeletal system; age of the dead is over 18; prescription of death is not more than 24-36 hours. The bodies of the dead before the study were stored under the same conditions, in a refrigerator at a temperature of +2°C.
Our study was carried out using the standard thigh incisions to search for deep vein thrombi of the thigh. Leg length was measured from the anterior superior iliac spine to the lateral malleolus. The skin on the medial surface of the thigh was dissected, and the thin muscle of the thigh was exposed. The muscle, its vessels and nerve were separated from the surrounding tissues along the entire length. Total length of m. Gracilis was measured from its origin (inferior ramus of the pubis) to its insertion (upper part of the medial surface of the tibia). The width and thickness of the muscle, the length of its muscular and tendon parts were measured. The number of vascular pedicles, the entrance point of each of the vascular pedicles and their sources, the length and diameter of the vessels, the nerve in the dominant vascular pedicle, and the number of nerve branches were also studied. The study was approved by the Ethics Committee of the 120 | Cardiometry | Issue 21. February 2022
Federal State Budgetary Institution “V.A. Almazov Almazov National Medical Research Centre” of the Ministry of Health of Russia, Extract No. 03012020 from Record No. 1-20 dated January 20, 2020 prepared by the Ethics Committee meeting.
According to the results of measuring the parameters of m.Gracilis, distribution series were compiled. For each variation series, the median value and interquartile range were calculated. In the process of primary statistical data processing, the Kolmogorov-Smirnov criterion was less than 0.05, and due to that fact, non-parametric statistical methods were used for the non-normal distribution of data. Spearman’s coefficient was used to assess the relationship between the parameters represented by quantitative data. Qualitative characteristics of the tightness of the relationship of the rank correlation coefficient were assessed on the Chaddock scale. The indicators were considered statistically significant at p<0.05.
Results
The median length of the lower limbs was 904.4(871.1;930.0) mm. The corresponding value of the total length of m. Gracilis was 452.25(439.7;462.0) mm, the median value of the length of the muscular part was 225.3(208.1;239.0) mm, and the median value of the length of the tendon was 230, 5(213.0;244.4) mm. The median width in the belly of the gracilis muscle in its widest part was 34.5 (29.2; 37.5) mm. The median thickness of the belly and tendon was 7.3(6.8;8.0), 2.6(2.3;2.8) mm, respectively (Table 1). In this case, there was a direct noticeable correlation between the lengths of m. Gracilis and the lower limb (R=0.64, p=0.019). Additionally, a moderate statistically significant relationship was found between the width of the
Table 1
Morphometric characteristics of the gracilis muscle of the thigh (M. Gracilis)
The number of vascular pedicles included in m. Gracilis, ranged from 1 to 5. Most often, in 46% of the cases, there was one main vascular pedicle, less often, in 34% of the cases, there was a variant with one additional pedicle. In 14% of the studied cases, the main vascular pedicle with two additional ones was identified. Three additional vascular pedicles were found in 4% of the cases. Only in 2% of the cases there were four additional vascular pedicles.
The distance from the origin of m. Gracilis to the point of entrance of the main vascular pedicle into the muscle ranged from 78 to 130 mm. The length of the main feeding artery varied from 76 to 134 mm, the median value was 100.5(90;110) mm, and its diameter was from 1.4 to 2.1 mm (M = 1.9(1.8;2, 0) mm The artery was most often accompanied by two veins (see Table 2 herein).
Table 2
Morphometric characteristics of the neurovascular bundle of the fine muscle of the thigh (M. Gracilis)
|
Morphometric parameters |
Median (Q1;Q3) mm |
Мin (mm) |
Мax (mm) |
|
Distance to the entry of the main vascular pedicle |
100.5(90;110) |
78 |
130 |
|
Length of the main feeding artery |
109(98;119) |
76 |
134 |
|
Main feeding artery diameter |
1.9(1,8;2,0) |
1.4 |
2.1 |
|
Nerve length |
108.5(96;117) |
76 |
130 |
|
Nerve diameter |
2.1(1,9;2,2) |
1.5 |
3 |
In 86% of the cases, the deep femoral artery formed the dominant vascular pedicle. In 14% of the cases, this function was performed by its branch, the medial artery that circumflexed the femur. Small secondary vascular pedicles originated from the anterior branch of the obturator artery or descending genicular artery. The length of additional feeding vessels was measured from the lower branch of the pubic bone and varied from 58 mm to 291 mm, depending on the number of vascular bundles and the variant of their discharge (Table 3).
According to our data, the proper nerve was located at a distance of 108.5 (96; 117) mm from the origin of the muscle; its diameter was 2.1 (1.9; 2.2) mm.
In 41 preparations (82% of the cases) the indicated nerve was represented by one main trunk, in 5 cases the nerve was represented by 2 trunks (10%), and in 4 cases the loose type of nerve structure was recorded (8%).
Table 3
The length of the vessels that feed m. Gracilis of the thigh
|
Vascular pedicle |
Distance from the inferior ramus of the pubis Median (Q1;Q3) mm |
|
Main pedicle |
100.5(90;110) mm |
|
1st additional pedicle |
204 (189;210) mm |
|
2nd additional pedicle |
272 (250;288) mm |
|
3rd additional pedicle |
270 (270;291) mm |
|
4th additional pedicle |
58 mm |
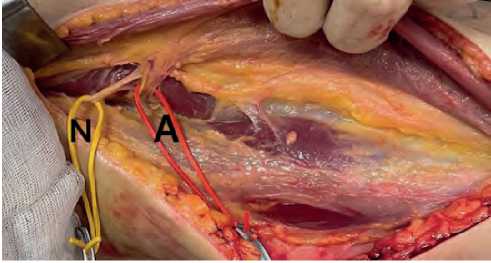
Figure 1. The most common structure of the neurovascular bundle of the M. gracilis pedicle (left side). Nerve (N). The main artery, accompanied by two veins (A).
Discussion
Thin muscle is widely used in reconstructive surgery. Previously, anatomical and radiological studies were carried out regarding the parameters of m. Gracilis and its vascular pedicles [5-7], which were focused on the length of the tendon part, due to purely applied tasks, i.e. the use of the muscle in rehabilitation operations for post-traumatic plexopathies. Only a few of them mentioned the muscle part used in the rehabilitation of mimic muscle paresis [9-14, 16,17].
An analysis of the literature data shows that the average width of the muscle part of m. Gracilis at its base, in the middle and at the end is 34.5±6.395, 26.3±4.682, 17.4±3.527 mm, respectively. At the same time, Dz-iedzic DW, et.al [8] and Rajeshwari MS, Roshankumar BN indicated the width of the belly of m. Gracilis 31.9 and 39 mm only, respectively [15].
The present study demonstrates that the median value of the total length of m. Gracilis, the length of its muscular part, as well as the length of the tendon are 452.25 (439.7; 462.0); 225.3(208.1;239.0); 230.5 (213.0; 244.4) mm, respectively.
In this case, there is a direct correlation between the lengths of m. Gracilis and the lower extremity, which is in full agreement with the results of the study
Issue 21. February 2022 | Cardiometry | 121
by Limitlaohaphan C et al. and Chiang et al. [18-21]. Additionally, a statistically significant relationship was found between the width of the useful muscle part of the graft, the width of the distal part of the tender muscle, and the length of the lower limb.
In the present study, attention was also focused on the study of the neurovascular pedicle of m. Gracilis. Its blood supply is variable and can be carried out from the branches of the femoral artery: the deep artery of the thigh, its branches - the medial artery, the circumflex femur, the descending knee artery, and also from the pool of the internal iliac artery - the anterior branch of the obturator artery [1-3].
Usually the above mentioned muscle of the thigh has two or three vascular pedicles penetrating into it from the inner surface. The proximal pedicle is dominant, enters at the junction of the upper and middle thirds of the muscle and is the main source of its blood supply, includes an artery, two draining veins, and the anterior branch of the obturator nerve. The medial circumflex femoral artery and the deep femoral artery usually form the proximal dominant vascular pedicle. The number of small secondary pedicles varies from one to five, and they include only vessels (artery and veins) and supply blood to the distal and smaller part of the muscle [3]. The small pedicle may include the anterior branch of the obturator artery, the descending genicular artery.
Our study showed that the number of vascular pedicles included in m. Gracilis, varied from 1 to 5, namely, in 46% of the cases there was one pedicle, in 34% of the cases we detected two pedicles, in 14% we revealed three pedicles, in 4% of the cases there were four pedicles, and extremely rarely - in 2% of the cases, the blood supply to the muscle was carried out according to the loose type and has at least five vascular pedicles. Most often (63.24%), the main vascular pedicle was located at a distance of 88-112 mm from the origin of m. Gracilis. These results were approximately the same as obtained in the observations of Rajeshwari MS, Roshankumar BN [15] and Vigato E et.al. [5], in which they mentioned that their number was 1-5 (most 1-3). The main pedicle enters the muscle at a distance of 100.5(90;110) mm. The diameter of the neurovascular pedicle at their entrance ranges from 1.4 to 2.1 mm, accompanied by two veins, which is somewhat larger than in the study of Vigato E et.al., the average value is 1.7 [5].
In this study, in all cases, the donor muscle was innervated by a branch of the obturator nerve. According to the reference literature, it is formed from 122 | Cardiometry | Issue 21. February 2022
L2-L4-spinal roots and, upon exiting their retroperitoneal space, bypassing the obturator canal, is divided into terminal posterior and anterior branches, the latter, having passed between the long and short adductor muscles, innervates the fine muscle of the thigh. Despite the fact that in most cases (82% of cases) this nerve is represented by one main trunk, loose types of its structure were also observed.
Conclusions
The anatomical structure of the neurovascular bundle of M. Gracilis is highly variable, however even the most extreme cases of individual anatomical variability it cannot exclude latter from being used as a donor in reconstructive surgery. This study provides important actual information about the anatomical features of m. Gracilis and can be useful in practice at the stage of preoperative planning.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Anatomical and topographical features of the gracilis muscle of the thigh from the position of using it for autotransplantation
- Standring S. Pelvic girdle and lower limb: overview and surface anatomy In: Gray’s anatomy: The Anatomical Basis of Clinical Practice, 41th ed, Elsevier Churchill Livingstone, Edinburgh, London, New York, Oxford, Philadelphia, St Louis, Sydney,Toronto. 2016;1337-1375.
- Shatari T, Niimi M, Fuiita M, Kodaira S. Vascular Anatomy of Gracilis muscle, arterial findings to enhance Graciloplasty. Surg. Radiol. Anat. 2000;22(1):21-4.
- Huemer GH, Dunst KM, Maurer H, Ninkovic M. Area enlargement of gracilis muscle flap through microscopically aided intramuscular dissection: ideas and innovations. Microsurgery. 2004; 24(5):369-73.
- Ortiz H, Armendariz P, DeMiguel M, Solana A, Alos R, Roig JV. Prospective study of artificial anal sphincter and dynamic graciloplasty for severe anal incontinence. Int J Colorectal Dis. 2003;18:349-54.
- Vigato E, et al. The clinical role of the gracilis muscle: an example of multidisciplinary collaboration. Pelviperineology. 2007; 26:149-51.
- Coquerel-Beghin D, Milliez PY, Auckbur IA, Lemierre G, Duparc F. The gracilis musculu cutaneous flap: Vascular supply of the muscle and skin components. Surg Radiol. Anat. 2006; 28:588-95.
- Singh H, Kaur R, Gupta N. Morphometric study of gracilis muscle and its rolein clinical recnstruction. J. Anat. Soc. India. 2011;60(2):202-6.
- Dziedzic DW, Bogacka U, Komarniţki L, Ciszek B. Anatomy and morphometry of the distal gracilis muscle tendon in adults and foetuses. Folia Morphol (Warsz). 2018;77(1):138-43.
- Elbarrany WG, Alasmari WA, Altaf FM. Morphometric analysis and blood supply of Gracilis and Semitendinosus tendons; their clinical importance in anterior cruciate ligament reconstruction. P J M H S. 2018;12(1):450-455.
- Kalra GDS, Sharma AK, Shende KS. Gracilis muscle transposition as a workhorse flap for anal incontinence: Quality of life and functional outcome in adults. Indian J Plast Surg. 2016;49(3):350-6.
- Hussy AJ, Laing AJA, Regan PJ. An anatomical study of the gracilis muscle and its application in groin wounds. Ann Plastic Surg. 2007;59(4):404-9.
- First A, et al. Gracilis transposition for repair of recurrent anovaginal and rectovaginal fistulas in Crohns disease. Int J Colorectal Diseases, 2007;8:51-4.
- Lorea P, Vercruysse N, Coessens VC. Use of gracilis muscle free flap for reconstruction of chronic osteomyelitis of foot and ankle. Acta Orthopaedica Belgica. 2001;67(3):267-73.
- Vranckx JJ, et al. The gracilis free flap is more than just a graceful flap for lower leg reconstruction. J Reconstructive Micro-surgery. 2004;20(2):143-8.
- Rajeshwari MS, Roshankumar BN. An anatomical study of gracilis muscle and its vascular pedicles. Int J Anat Res. 2015;3(4):1685-8.
- Mochizuki T, Akita K, Muneta T, Sato T. Pesanserinus: layered supportive structure on the medial side of the knee. Clin Anat. 2004;17(1):50-4.
- Yoshioka K, Keighley MRB. Clinical and manometric assessment of gracilis muscle transplant for faecal incontinence. Dis Colon Rectum. 1988;31:767-9.
- Limitlaohaphan C, Kijkunasatian C, Saitongdee P. Length of semitendinosus and gracilis tendons and the relationship of graft length and leg length. J Med Assoc Thai. 2009;92(6):200-3.
- Chiang ER, et al. Hamstring graft sizes differ between Chinese and Caucasians. Knee Surg Sports Traumatol Arthrosc. 2011:25. [PubMed].
- Pereira RN, et al. Correlation Between anthrometric data and length and thickness of tendons of semitendinosus and gracilis muscles used for graft in reconstruction of anteriorcruciate ligament. Rev Bras Ortop.2016;51:175-80.
- Nakornchai C, Charakorn K. Correlation between the Length of Gracilis and Semitendinosus Tendon and Physical Parameters in Thai Males. J Med Assoc Thai. 2012;95(10):142-6.


