Associated applicance of artroscopic debridement and proximal fibular osteotomy at the treatment of patients with deformic artritis of knee
Автор: Irismetov Murodjon E., Fozilov Khusniddin T., Khakimov Sherali K., Safarov Navruz B.
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 6 т.28, 2022 года.
Бесплатный доступ
Introduction The problem of varus deformed knee joint osteoarthritis remains one of the actual topics of modern adult orthopedics. The use of many well-known methods of surgical interventions and arthroscopic technology are not rational in terms of restoring the biomechanical axis of the lower limb. The purpose of the research Analysis of the results of arthroscopic debridement and the use of proximal fibular osteotomy (PFO) in the treatment of varus deformed knee osteoarthritis. Materials and investigation methods Our study included a survey of 152 patients with deforming osteoarthritis of I-II-III degree and varus deformity of the knee joint, dividing them into 2 groups: Group I (control) consisted of 131 patients who underwent debridement of the articular surface. Group II (main) consisted of 19 patients with debridement and PFO developed in our clinic. The analysis of the achieved results was assessed on the basis of indicators of the KSS scale. Results The results of the surgery in both groups were reviewed comparatively at 1 year after surgery by KSS scale data with results:
Knee joint, deforming osteoarthrosis, osteotomy, artroscopy
Короткий адрес: https://sciup.org/142236802
IDR: 142236802 | УДК: 616.728.3-007.248-089.81 | DOI: 10.18019/1028-4427-2022-28-6-768-773
Текст научной статьи Associated applicance of artroscopic debridement and proximal fibular osteotomy at the treatment of patients with deformic artritis of knee
Original article
Введение . Проблема лечения остеоартрита коленного сустава с варусной деформацией остаётся одной из актуальных тем современной взрослой ортопедии. Применение многих известных методов оперативных вмешательств и артроскопической технологии не является рациональным в плане восстановления биомеханической оси нижней конечности. Цель . Анализ результатов артроскопического дебридмента с проксимальной фибулярной остеотомией (ПФО) в лечении деформирующего остеоартрита коленного сустава. Материалы и методы . В исследование включено 152 больных с деформирущим остеоартритом I-II-III степени и варусной деформацией коленного сустава, которые разделены на 2группы. Iгруппу (контрольную) составил 131больной. У данныхпациентоввыполнялидебридемент суставной поверхности. Группу II (основную) составили 19 пациентов, у которых выполнен дебридемент и ПФО по разработанной в нашей клинике методике. Анализ достигнутых результатов оценивали на основе показателей шкалы КСС. Результаты . Сравнительно проанализированы результаты в обеих группах через 1 год после операции по данным шкалы KSS. Показатели < 60 баллов расценены как неудовлетворительные; 60-69 баллов – удовлетворительные; 70-79 баллов – хорошие; 80-100 баллов – очень хорошие. Выводы . Шкала KSS для оценки отдаленных результатов лечения больных с деформирующим остеоартрозом коленного сустава является оптимальной. Комбинированное применение артроскопического дебридемента и ПФО позволило увеличить долю хороших результатов до 89 % против 69 % у больных, которым применяли артроскопическую манипуляцию без ПФО, а также снизить долю неудовлетворительных результатов до «нуля» по сравнению с 9 % у пациентов при использовании только артроскопического дебридемента.
RELEVANCE OF THE SUBJECT
Among large support joints, the rate of injury due to degenerative-dystrophic changes of the knee joint remains high, leading to a sharp disruption of the normal movement biomechanics of the human musculoskeletal system, patients needing additional support and a significant decrease in functional and social adaptation [1, 2]. An analysis of recent literature shows that the initial change in knee joint biomechanics occurs in 20 % of people, of which 87 % of patients with deformable osteoarthritis have varus deformity, and 100 % of patients over 51 years of age have knee joint biomechanical disorders [3]. Arthroscopic diagnosis and treatment – determining the functional status
of the joint, debridement of degenerative-dystrophic tissue, cleaning of chondromalacia foci, tunneling operations have solved important problems of advanced orthopedics [4].
Knee joint debridement is 74 % effective, including procedures such as degenerative-dystrophic altered tissue of the joint, cleaning of chondromalacia foci and synovial joint surfaces, as well as removal of meniscectomy and osteophytes [5].
According to scientists, after the operation of proximal fibular osteotomy (PFO) in deformed osteoarthritis of the knee, due to the weakening of the external components of the knee joint changes the balance of the joint and the mechanism of redistribution of load on the outer and inner plateaus [6, 7, 8].
However, the above-mentioned degenerative-dystrophic changes in the knee joint and debridement aimed at restoring the biomechanical axis of the lower limb and the combined use of proximal fibular osteotomies are emerging [9].
The Department of Sports Trauma of the Republican Specialized Scientific-Practical Medical Center for Traumatology and Orthopedics and the Bukhara branch of the Republican Scientific Center of Emergency Care have increased the share of good results in the complex use of joint arthroscopic debridement and PFO in the treatment of deforming osteoarthritis of the knee in 2018-2020.
The purpose of the research . Analysis of the results of arthroscopic debridization and the use of PFO in the treatment of varus deformed knee osteoarthritis.
MATERIALS AND INVESTIGATION METHODS
In our study, we included 152 patients with grade I-II-III deformity arthritis and varus deformity of the knee joint, who treated in the Department of Sports Trauma of the Republican Specialized Scientific-Practical Medical Center for Traumatology and Orthopedics and the traumatology department of Bukhara branch of the Republican Scientific Center of Emergency Care between 2018 and 2020. The average age of the patients was 55,3 ± 2,7 years (min – 35; max – 80).
Severity of degenerative-dystrophic changes in the joint were divided into groups according to the classification by Kosinsky N.S. (1961) [4]. All patients were divided into 2 groups and long-term postoperative outcomes were studied. Group I (control) consisted of 131 patients, of which 115 were women and 18 were men. Patients in this group underwent debridement of joint surfaces. Group II (basic) consisted of 19 patients, including 15 women, 4 men. This group of patients underwent joint debridement and PFO, the surgical procedure developed in our clinic and a utility model patent (FAP 01859) was obtained (Table 1).
All treated patients had varus deformities of the knee joints. For diagnostic purposes, radiography and MRI of the knee joint were performed in 2 projections.
Patients underwent knee debridement and PFO surgeries performed according to standard techniques. Surgical procedures were performed under arthroscopy. Surgical procedures were performed under arthroscopy. The analysis of the obtained results was evaluated on the basis of indicators of KSS (Knee Society Scores) scale (Insall J. et all, 1989), proposed by the American Knee Association.
Statistical data The study results were processed using the Microsoft Excel program. Differences were considered statistically significant at p < 0.05, where p is the level of significance of these criteria. All results are presented as M ± σ, where M is the sample mean, σ is the standard deviation.
Outcome analysis
The results of the surgery were reviewed at 3, 6, 12 months (short-term) and 1 year (long-term) after the operation.Evaluation of the obtained results was carried out on the basis of anterior and lateral projection radiographic data and KSS scale.
The KSS scale was used to assess knee joint function, and the results were evaluated on days 1, 2, 3 before surgery and 1 and 6 months after surgery.In the assessment by the KSS method, the knee joint was assessed based on its clinical-functional status and the stability of the tibiolateral joint,scores were summarized in the evaluation of results: < 60 points – unsatisfactory; 60-69 points – satisfactory; 70-79 points – good; 80-100 points – rated very good (Tables 2 and 3).
In Tables 2 and 3 above, the results of surgical procedures performed in 133 patients of control groups and 19 patients of the basic groups with osteoarthritis of the knee joint were evaluated based on the analysis of clinical and functional indicators of the KSS scale. From the clinical indicators, the intensity of pain syndrome was assessed on the basis of "mild pain and moderate pain" criteria and showed a significant decrease in the number of patients in the control group after arthroscopic debridement + PFO procedures performed in the basic group of patients, in the control group, “mild pain” increased by 14.3 %, “moderate pain” decreased by 46 %, and in the basic group of patients, “mild pain” decreased by 5 %, and “moderate pain” decreased by 63 %.
Table 1
Division of patients by gender, type of surgical procedure used
|
Criteria |
Basic group (n = 19) |
Control group (n = 133) |
Total |
|||
|
Gender |
female |
male |
Female |
male |
152 |
|
|
15 |
4 |
115 |
18 |
|||
|
Surgical procedures performed |
Joint debridement + PFO (n = 19) |
Joint debridement (n = |
133) |
152 |
||
|
Degree of pathology |
II degree |
III degree |
I degree |
II degree |
III degree |
152 |
|
11 (61,2 %) |
8 (38,8 %) |
5 (3,8 %) |
89 (67,9 %) |
39 (29,8 %) |
||
Table 2
|
Criteria |
Control group patients (n = 133) |
||||||||||||||
|
Clinical evaluation |
Pain |
Walking |
No pain |
Weak pain |
Moderate pain |
Acute pain |
|||||||||
|
-/97 (-/72,9 %) |
5/24 (3,7/18 %) |
73/12 (55/9 %) |
55/- (41,3/- %) |
||||||||||||
|
Climbing the stairs |
No pain |
Mild pain |
Moderate pain |
Acute pain |
|||||||||||
|
-/74 (-/55,6 %) |
12/31 (9/23,3 %) |
87/28 (65,4/21 %) |
34/- (25,6/-) |
||||||||||||
|
Amplitude of motion |
5 degrees |
10 deg. |
15 deg. |
20 deg. |
25 deg. |
||||||||||
|
71/13 (53,4/9,8 %) |
26/37 (19,5/28 %) |
21/56 (15,8/42 %) |
15/22 11,3/16,5 %) |
-/5 (-/3,7 %) |
|||||||||||
|
Tibiolateral stability |
Anterior-posterior |
Less than 5 mm |
5-10 mm |
10 + mm |
|||||||||||
|
63/66 (47,4/49,6 %) |
47/51 (35,3/38,4 %) |
23/16 (17,3/12 %) |
|||||||||||||
|
Medio-lateral |
Less than 5 mm |
5-10 mm |
10 + mm |
||||||||||||
|
72/84 (54/63 %) |
36/43 (27/32,5 %) |
25/6 (19/4,5 %) |
|||||||||||||
|
Contracture |
Bending |
5-10 deg. |
11-15 deg. |
16-20 deg. |
> 20 deg. |
||||||||||
|
51/95 (38,3/71,4 %) |
37/14 (27,8/10,5 %) |
35/16 26,4/12 %) |
10/8 (7,5/6,1 %) |
||||||||||||
|
Unbending |
Not detected |
<10 deg. |
10 - 20 deg. |
> 20 deg. |
|||||||||||
|
86/91 (64,7/68,5) |
27/32 20,3/24 %) |
20/10 (15/7,5 %) |
-/- (-/- %) |
||||||||||||
|
Deviation line |
Less than 5 deg. |
5-10 deg. |
More than every 5 degrees |
||||||||||||
|
78/96 (58,6/72,2 %) |
37/25 (27,8/19 %) |
18/12 (13,5) |
|||||||||||||
|
Functional evaluation |
Walking |
Unlimited |
>2 km |
1 – 2 km |
< 1 km |
Tied |
Can't walk |
||||||||
|
38/17 (28,6/12,8 %) |
19/8 (14,3/6 %) |
30/75 (22,6/56,5 %) |
36/28 (27/21 %) |
10/5 (7,5/3,7 %) |
-/- (-/- %) |
||||||||||
|
Climbing the stairs |
№ climbs |
Easy up, hard down |
Up and down hard |
Easy down, hard up |
Can’t climb |
||||||||||
|
67/84 (50,4/63,2 %) |
46/32 (34,6/24 %) |
18/15 (13,5/11,3 %) |
2/2 (1,5/1,55) |
-/- (-/- %) |
|||||||||||
|
Walking using a walking device |
Doesn’t use |
Using a crutch |
Using a double-sided crutch |
Using a crutch or wheelchair |
|||||||||||
|
61/89 (45,9/67 %) |
47/25 (35,3/18,8 %) |
18/14 (13,5/10,5 %) |
7/5 (5,3/3,7 %) |
||||||||||||
Table 3
|
Criteria |
Control group patients (n = 133) |
||||||||||||||
|
Clinical evaluation |
Pain |
Walking |
No pain |
Weak pain |
Moderate pain |
Acute pain |
|||||||||
|
-/14 (-/74 %) |
5/4 (26/21 %) |
13/1 (68/5 %) |
1/- (6/ %) |
||||||||||||
|
Climbing the stairs |
No pain |
Mild pain |
Moderate pain |
Acute pain |
|||||||||||
|
-/11 (-/58 %) |
9/7 (47/36,7 %) |
7/1 (37/5,3 %) |
3/- (16/- %) |
||||||||||||
|
Amplitude of motion |
5 deg. |
10 deg. |
15 deg. |
20 deg. |
25 deg. |
||||||||||
|
2/1 (11/6 %) |
4/1 (21/6 %) |
5/8(26/42 %) |
5/7 (26/36 %) |
3/2 (16/10 %) |
|||||||||||
|
Tibiolateral stability |
Anterior-posterior |
Less than 5 mm |
5-10 mm |
10 + mm |
|||||||||||
|
6/3 (32/16 %) |
9/7 (47/37 %) |
4/9 (21/47 %) |
|||||||||||||
|
Medio-lateral |
5 мм дан кам |
5-10 мм |
10 + мм |
||||||||||||
|
8/5 (42/26,3 %) |
8/9 (42/47,4 %) |
3/5 (16/26,3 %) |
|||||||||||||
|
Contracture |
Bending |
5-10 deg. |
11-15 deg. |
16-20 deg. |
> 20 deg. |
||||||||||
|
6/9 (32/47 %) |
7/8 (37/42 %) |
5/2 (26/11 %) |
1/- (5/ %) |
||||||||||||
|
Unbending |
Not detected |
< 10 deg. |
10-20 deg. |
> 20 deg. |
|||||||||||
|
8/9 (42/47 %) |
7/8 (37/42 %) |
4/2 (21/11 %) |
-/- (-/- %) |
||||||||||||
|
Deviation line |
Less than 5 deg. |
5-10 deg. |
More than every 5 degrees |
||||||||||||
|
7/9 (37/47 %) |
7/8 (37/42 %) |
5/2 (26/11 %) |
|||||||||||||
|
Functional evaluation |
Walking |
Unlimited |
>2 km |
1-2 km |
< 1 km |
Tied |
Can't walk |
||||||||
|
3/7 (16/37 %) |
10/8 (52/42 %) |
4/2 (21/11 %) |
2/2 (11/11 %) |
-/- (-/- %) |
-/- (-/- %) |
||||||||||
|
Climbing the stairs |
№ climbs |
Easy up, hard down |
Up and down hard |
Easy down, hard up |
Can’t climb |
||||||||||
|
7/9 (37/47 %) |
6/7 (31,6/37 %) |
3/1 (15,7/5 %) |
3/2 (15,7/11 %) |
-/- (-/- %) |
|||||||||||
|
Walking using a walking device |
Doesn’t use |
Using a crutch |
Using a double-sided crutch |
Using a crutch or wheelchair |
|||||||||||
|
11/14 (58/74 %) |
4/5 (21/26 %) |
-/- (-/- %) |
4/- (21/- %) |
||||||||||||
Patients in the control group underwent surgery and subsequent outcomes were evaluated as per the KSS scale
The basic group of patients underwent surgery and subsequent outcomes were evaluated as per the KSS scale
Surgical procedures performed in all patients resulted in an increase in range of motion in the knee joint. Analysis of indicators in patients of the main and control groups The complex application of arthroscopy + PFO led to an increase in the criterion of painless "amplitude of movement" based on the correction of the biomechanical axis of the lower limb in patients, in patients of the control group "10-degree movement amplitude" increased by
-
8 .5 %, 15 deg. – increased by 26.2 %, 20 deg. – increased by 5.2 %, and in the basic group of patients – 10 deg. – decreased by 15 %, 15 deg. – increased by 16 % and 20 deg. – increased by 10 %.
The improvement in knee joint function was also explained by a decrease in the criterion of "bending and unbending contracture" of the knee joint, i.e. the developed knee joint "bending contracture – 16-20 and > 20 degree"
in the control group decreased by 14 % and 1.4 %, "unbending contracture" decreased by 7.5 %, and in the basic group of patients "bending contracture" decreased by 15 %, after surgery > 20 degrees. Patients with "bending contracture of the knee joint" were not identified. Patients with "> 20 degree knee unbending contracture" decreased by 10 % and "> 20 degree knee unbending contracture" contract were not identified.
When we functionally evaluated the results, the pre-and post-operative outcomes were analyzed according to the criterion of “walking” among the patients of the basic and control groups. At the same time, patients in the control group with no "walking limits" before the surgery accounted for 28.6 %, and this figure decreased to 12.8 % after the surgery.In the basic group of patients, this criterion increased from 16 % to 37 %, and the criterion of "walking up to 2 km" decreased from 14.3 % to 6 % in the control group. In the basic group of patients, it decreased from 52 % to 42 %.The indicators obtained on the criterion of "walking limit" for 1-2 km increased from 22.6 % to 56.5 % in patients of the control group, in the basic groupit decreased from 21 % to 11 %. The criterion "walking with a crutch or additional support devices" decreased from 7.5 % to 3.7 % in patients in the control group, among the basic group of patients, no patients "walking with a crutch or additional support devices" were identified.
In the functional assessment of long-term postoperative outcomes, they were assessed according to the criterion of
“climbing the stairs”, at the same time, the criterion "easy to climb stairs and difficult to descend" increased from 31.6 % to 37 % in the basic group of patients;in control group patients, it decreased from 34.6 % to 24 %. According to the criterion "difficult to climb and descend the stairs" there was a decrease from 13.5 % to 11.3 % in patients of the control group, and from 15.7 % to 5 % in patients of the basic group.
Comparing pre- and postoperative parameters in the control and basic group of patients on the criterion of "walking using the device"showed that patients who did not use a walking device increased from 61 % to 89 % in the control group; in the basic group, it increased from 58 % to 74 %. Among patients of the control group with the “crutch” or “wheelchair”, the number decreased from 5.3 % to 3.7 %, in the basic group, 21 % of such patients were identified before surgery, and no patients with “crutches” or “wheelchairs” were identified after surgery.
Clinical example
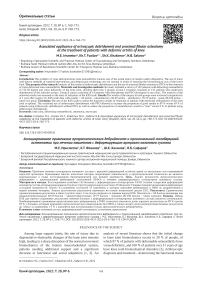
Patient A. was born in 1957. Medical card No. 7376, on November 18, 2019 was admitted to the Department of Sports Trauma of the Republican Specialized Scientific-Practical Medical Center of Traumatology and Orthopedics with the following diagnosis:Deforming osteoarthritis of both knee joints, grade III, right knee joint synovitis, medial meniscus meniscopathy, chondromalacia of the hip and tibia, grade IV.
On November 22, 2019, the patient underwent “Knee joint debridement and PFO surgeries” (Fig. 1).
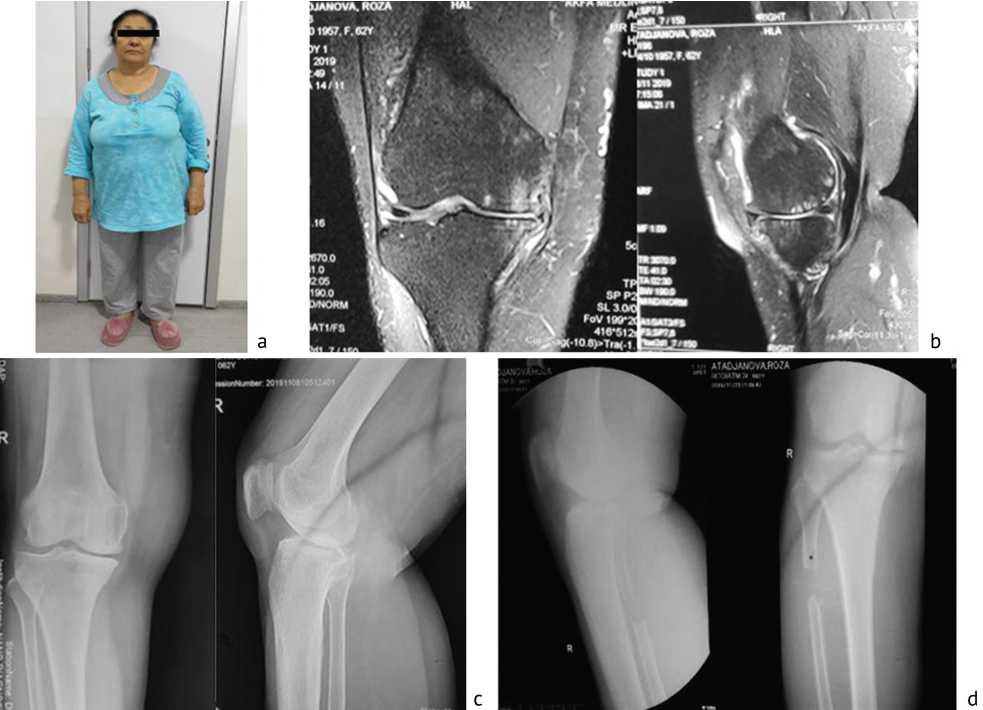
Fig. 1. Patient A., deforming arthrosis of the knee joint: a – general view; b – MRI image, medial meniscopathy, suprapatellar bursitis; c – X-ray image, the edges of the bone are pointed, narrowing of the medial joint gap of the knee joint, and osteophytes are detected; d – X-ray image, postoperative symptoms of proximal fibular osteotomy are detected
DISCUSSION
Based on the literature, the concept of "debridement" is understood as a part of synovectomy, resection of degeneratively injured menisci, removal of loose bodies, treatment of osteophytes, resection of intra-articular scars and knee joint detection, as well as the effectiveness of concomitant use of joint lavage was found to be 74 % increased.
According to V.I. Shevtsov (2009), using the practice of arthroscopy during the period of 2000 to 2009, analysis of long-term postoperative outcomes of 30 patients aged 21-69 years diagnosed with deforming osteoarthritis of the knee joint was found to be good in 96.7 % of cases [10].
D.N. Zubok and co-authors (2010) demonstrated the benefits of debridement arthroscopy in the treatment of patients with deforming osteoarthritis of the knee joint and it was acknowledged that the proportion of postoperative complications was reduced by 3.8 times [11].
The uniqueness of the role of arthroscopy in the surgical treatment of degeneratively altered tissue of the knee joint has been proven in the literature, however, the biomechanical effects of knee deforming arthrosis in varus deformities have not been studied [12, 13, 14].
Osteotomy and resection of the proximal part of the fibula in varus deformities of the knee joint have been performed by a group of scientists and have been shown to increase the proportion of good results in the short time period [15, 16, 17].
It is known that proximal fibular osteotomy in deforming osteoarthritis of the knee joint was first developed and used by Indian scientists Dr. Yeshwanth Subash and Dr. Gunalan K Naidu (2018) [18, 19].
L. Prakash (2019) performed PFO surgeries in 51 patients with medial varus osteoarthritis of the knee joint, indicating that a number of indicators approached the significant normal range,i.e., the femoral-tibial angle decreased from 181 ± 1.9° to 178 ± 2.0°, and the medial joint gapincreased from 1.2 ± 0.7 mm to 4.5 ± 1.1 mm (P < 0.001), and the lateral joint gapwas reduced from 7.2 ± 1.2 mm to 5.2 ± 1.1 mm(P < 0,001) [20].
CONCLUSION
The use of the KSS scale to assess the long-term results of treatment of patients with deformed osteoarthritis of the knee joint is optimal.
The combined use of arthroscopic debridement with PFO in patients with OA of the knee joint allowed to increase the proportion of good results to 89 % versus 69 % of patients using arthroscopic debridement without PFO, as well as reduce the proportion of unsatisfactory results to “zero” versus 9 % of patients using arthroscopic debridement.
Список литературы Associated applicance of artroscopic debridement and proximal fibular osteotomy at the treatment of patients with deformic artritis of knee
- Shane A.A., Loeser R.F. Why is osteoarthritis an age-related disease? // Best. Pract. Res. Clin. Rheumatol. 2010. Vol. 24, No 1. P. 15-26. DOI: 10.1016/j.berh.2009.08.006.
- Radiographic measures of settlement phenomenon in patients with medial compartment knee osteoarthritis / T. Dong, W. Chen, F. Zhang, B. Yin, Y. Tian, Y. Zhang // Clin. Rheumatol. 2016. Vol. 35, No 6. P. 1573-1578. DOI: 10.1007/s10067-015-3146-0.
- EULAR Recommendations 2003: an evidence based approach to management of knee osteoarthritis: Report of task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) / K.M. Jordan, N.K. Arden, M. Doherty, B. Bannwarth, J.W. Bijlsma, P. Dieppe, K. Gunther, H. Hauselmann, G. Herrero-Beaumont, P. Kaklamanis, S. Lohmander, B. Leeb, M. Lequesne, B. Mazieres, E. Martin-Mola, K. Pavelka, A. Pendleton, L. Punzi, U. Serni, B. Swoboda, G. Verbruggen, I. Zimmerman-Gorska, M. Dougados; Standing Committee for International Clinical Studies Including Therapeutic Trials ESCISIT // Ann. Rheum. Dis. 2003. Vol. 62, No 12. P. 1145-1155. DOI: 10.1136/ ard.2003.011742.
- Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors / D.E. Bonasia, F. Dettoni, G. Sito, D. Blonna, A. Marmotti, M. Bruzzone, F. Castoldi, R. Rossi // Am. J. Sports Med. 2014. Vol. 42, No 3. P. 690-698. DOI: 10.1177/0363546513516577.
- Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up / T. Duivenvoorden, R.W. Brouwer, A. Baan, P.K. Bos, M. Reijman, S.M. Bierma-Zeinstra, J.A. Verhaar // J. Bone Joint Surg. Am. 2014. Vol. 96, No 17. P. 1425-1432. DOI: 10.2106/JBJS.M.00786.
- Proximal fibular osteotomy to treat medial compartment knee osteoarthritis: Preoperational factors for short-term prognosis / B. Liu, W. Chen, Q. Zhang, X. Yan, F. Zhang, T. Dong, G. Yang, Y. Zhang // PLoS One. 2018. Vol. 13, No 5. P. e0197980. DOI: 10.1371/journal. pone.0197980.
- Бадокин В.В. Остеоартроз коленного сустава: клиника, диагностика, лечение // Современная ревматология. 2013. Т. 7, № 3. С. 70-75.
- Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis / L. Wei, X. Wang, Z. Lv, B. Zhao, Zh. Duan, W. Wu, B. Zhang, X. Wei // J. Inern. Med. Res. 2017. Vol. 45, No 1. P. 282-289. DOI: 10.1177/0300060516676630.
- Helminen H.J. Sports, loading of cartilage, osteoarthritis and its prevention // Scand. J. Med. Sci. Sports. 2009. Vol. 19, No 2. P. 143-145. DOI: 10.1111/j.1600-0838.2008.00881.x.
- Морфорентгенометрическая диагностика остеоартроза коленного сустава у больных пожилого возраста / В.И. Шевцов, В.Д. Макушин, О.К. Чегуров, Л.Л. Саблукова // Гений ортопедии. 2011. № 3. С. 71-77.
- Макушин В.Д., Чегуров О.К. Гонартроз: отдалённые результаты применения высокой вальгизирующей остеотомии большеберцовой кости (обзор зарубежной литературы) // Гений ортопедии. 2007. № 1. С. 137-141.
- High tibial osteotomy for the treatment of medial osteoarthritis of the knee with new iBalance system: 2 years of follow-up / D. Ghinelli, A. Parma, M. Baldassarri, A. Olivieri, M. Mosca, G. Pagliazzi, R. Buda // Eur. J. Orthop. Surg. Traumatol. 2016. Vol. 26, No 5. P. 523-535. DOI: 10.1007/ s00590-016-1768-9.
- Pre-operative arthritis severity as a predictor for total knee arthroplasty patients' satisfaction / C. Schnurr, M. Jarrous, I. Güdden, P. Eysel, D.P. König // Int. Orthop. 2013. Vol. 37, No 7. P. 1257-1261. DOI: 10.1007/s00264-013-1862-0.
- The pathophysiology of osteoarthritis: a mechanical perspective on the knee joint / K.R. Vincent, B.P. Conrad, B.J. Fregly, H.K. Vincent // PM&R. 2012. Vol. 4, No 5 Suppl. P. S3-S9. DOI: 10.1016/j.pmrj.2012.01.020.
- Early clinical effect of proximal fibular osteotomy on knee osteoarthritis / G. Zou, W. Lan, Y. Zeng, J. Xie, S. Chen, Y. Qiu // Biomed. Res. 2017. Vol. 28, No 21.
- Oakley S.P., Lassere M.N. A critical appraisal of quantitative arthroscopy as an outcome measure in osteoarthritis of the knee // Semin. Arthritis Rheum. 2003. Vol. 33, No 2. P. 83-105. DOI: 10.1016/s0049-0172(03)00082-9.
- Medial Compartment Decompression by Fibular Osteotomy to Treat Medial Compartment Knee Osteoarthritis: A Pilot Study / Z.Y. Yang, W. Chen, C.X. Li, J. Wang, D.C. Shao, Z.Y Hou, SJ. Gao, F. Wang, J.D. Li, J.D. Hao, B.C. Chen, Y.Z. Zhang // Orthopedics. 2015. Vol. 38, No 12. P. e1110-e1114. DOI: 10.3928/01477447-20151120-08.
- Subash Y., Naidu G.K. The role of proximal fibular osteotomy in the management of medial compartment osteoarthritis of the knee // Int. J. Orthop. Sci. 2018. Vol. 4, No 3. P. 369-372.
- The pathogenesis research of non-uniform settlement of the tibial plateau in knee degeneration and varus / Y. Zhang, C. Li, J. Li, F. Wang, Y.B. Zhu, G. Yang, Y. Tian // J. Hebei. Med. Univ. 2014. Vol. 35, No 2. P. 218-219.
- Prakash L. PFO - Proximal Fibular Osteotomy in Medial Compartment Arthritis of the Knee with Varus Deformity // EC Orthopaedics. 2019. Vol. 10, No 5. P. 315-321.