Cervical cancer demystified: exploring epidemiology, risk factors, screening, treatment modalities, preventive measures, and the role of artificial intelligence
Автор: Mohammad N., Khan M., Maqsood M., Naseeb A.
Журнал: Сибирский онкологический журнал @siboncoj
Рубрика: Обзоры
Статья в выпуске: 2 т.24, 2025 года.
Бесплатный доступ
Cervical cancer remains a significant global health challenge, particularly in low- and middle-income countries where access to preventive measures and early detection is limited. This review aims to summarize current evidence on cervical cancer prevention, screening, and treatment, emphasizing the emerging role of artificial intelligence (AI) in improving diagnostic and therapeutic approaches. Material and Methods.A comprehensive literature review was conducted using peer-reviewed articles from Google Scholar, PubMed, and Scopus. The search focused on human papillomavirus (HPV) vaccination, cervical cancer screening methods, treatment strategies, and AI applications in cervical cancer management. Results. Despite advancements in prevention and early detection, cervical cancer remains a leading cause of cancer-related mortality in women, particularly in underdeveloped regions. Screening methods such as Pap smears, HPV DNA testing, and visual inspection with acetic acid (VIA) have been instrumental in reducing incidence rates in developed countries. Additionally, HPV vaccination programs have significantly decreased the prevalence of high-risk HPV infections, contributing to a decline in cervical cancer cases. However, disparities persist due to limited healthcare infrastructure and access to routine screening. AI-driven technologies, including deep learning algorithms and machine learning models, are emerging as valuable tools in cervical cancer detection, risk assessment, and treatment planning. These innovations have the potential to enhance diagnostic accuracy, reduce human error, and improve patient outcomes, particularly in resource-limited settings. Conclusion. The integration of HPV vaccination, advanced screening techniques, and AI-based diagnostic tools represents a transformative approach to cervical cancer prevention and management. Addressing healthcare disparities through the implementation of these innovations is essential for achieving equitable global cervical cancer control. Future research should focus on optimizing AI applications for broader clinical use and ensuring accessibility in low-resource regions.
Cervical cancer, early detection, treatment, HPV vaccination, artificial intelligence
Короткий адрес: https://sciup.org/140309147
IDR: 140309147 | УДК: 618.146-006-07-08-084:004.8 | DOI: 10.21294/1814-4861-2025-24-2-117-125
Текст научной статьи Cervical cancer demystified: exploring epidemiology, risk factors, screening, treatment modalities, preventive measures, and the role of artificial intelligence
Cervical cancer is a significant health issue for women globally, especially in underdeveloped countries [1]. It has a high death rate in countries with a low Human Development Index (HDI) [2]. Cervical cancer begins in the cervix due to abnormal cell growth, potentially affecting surrounding tissues and organs. The risk increases with human papillomavirus (HPV) infection. Symptoms, such as irregular menstruation, weight loss, pelvic pain, and vaginal discharge, appear after the cancer has progressed [3]. This review will provide comprehensive insights into cervical cancer’s risk factors, screening methods, preventive measures, and treatment strategies by analyzing previous literature (Table).
Cervical Cancer Subtypes
Understanding cervical cancer rates requires knowledge of its histological subtypes, mainly squamous cell carcinoma and adenocarcinoma. Early detection is critical, and the effectiveness of screening varies by subtype [4]. Pap smears can detect squamous cell carcinoma but not adenocarcinoma due to their location in the upper endocervix. HPV detection is more effective for adenocarcinoma [5]. Studies indicate squamous cell carcinoma accounts for 82.72 % of cases, while adenocarcinoma comprises 12.18 %. Squamous cell carcinoma is more prevalent in subSaharan Africa and South-Central Asia [6].
Epidemiology Overview
Cervical cancer is one of the most common cancers in women and the second-leading cause of cancer deaths globally. Annually, 529,000 new cases are reported, predominantly from underdeveloped countries, resulting in approximately 275,000 deaths. The prevalence rate is 11.7 %, with higher rates in Saharan Africa (24.0 %), Europe (21.4 %), and Latin America (16.1 %). Developed countries have seen an 80 % decline in cases due to adequate screening and vaccination programs, whereas developing countries face higher incidence and mortality rates due to inadequate healthcare infrastructure [7].
Table/Òàблицà
List of cervical cancer prevention, screening, and treatment techniques
Måтîды пðîфилàêтиêи, ñêðинингà и лåчåния ðàêà шåéêи мàтêи
Prevention/Профилактика
Primary prevention/ Первичная профилактика Knowledge/ Знания Awareness/
Осведомленность Vaccination/ Вакцинация Secondary prevention/ Вторичная профилактика Early detection and screening/ Раннее выявление и скрининг Tertiary Prevention/ Третичная профилактика Treatment/
Лечение Rehabilitation/ Реабилитация
Screening/Скрининг
Treatment/Лечение
Pap smear/Мазок Папаниколау HPV detection test/
Тест на выявление ВПЧ Visual testing methods/ Визуальные методы тестирования VIA and VILI/ Визуальный осмотр шейки матки с помощью уксусной кислоты и/или с помощью раствора Люголя Computer-aided systems/ Компьютерные системы Colposcopy/
Кольпоскопия Conization/cone biopsy/ Конизация
Nanotechnology/Нанотехнологии Deep learning and Machine learning/ Глубокое обучение и машинное обучение
Surgery/ Операция
Radical hysterectomy/ Радикальная гистерэктомия
Robotic surgery/ Роботизированная хирургия Radiotherapy/Радиотерапия Intensity-modulated radiotherapy (IMRT)/ Интенсивно-модулированная лучевая терапия Image-guided brachytherapy/ Брахитерапия под визуальным контролем
Brachytherapy/ Брахитерапия External beam radiotherapy/ Дистанционная лучевая терапия Chemoradiation/ Химиорадиотерапия
Chemotherapy/ Химиотерапия Anti-angiogenic treatment/ Антиангиогенная терапия Targeted therapy/ Таргетная терапия Immunotherapy/ Иммунотерапия
Note: created by the authors.
Примечание: таблица составлена авторами.
Prevalence of Cervical Cancerin Developing Countries
Cervical cancer is more common in developing countries, accounting for 85 % of cases. Survival rates are lower due to poor infrastructure and healthcare facilities. In Asian countries like Pakistan, India, Bangladesh, and Iran, cervical cancer remains a major issue. In 2007, 90,708 cases were reported in India, with 126,000 new cases annually [8]. China and India report 80 % of cases [9]. In 2010, 528,000 cases were reported globally, with 266,000 deaths. Cervical cancer causes 12 % of all female cancer cases in underdeveloped countries [10]. The incidence rate is highest in the Caribbean, South and Central America, South Asia, and Sub-Saharan Africa [11].
Cervical Cancer in Pakistan
Gynecological cancers are a significant health concern for women worldwide, with varying rates due to factors like lifestyle, genetics, and socio-economic status. While cases are decreasing in developed countries due to effective screening and vaccination programs, cervical cancer remains a major problem in Pakistan. Epidemiological data is inconsistent due to poor reporting [12]. In 2002, WHO reported a prevalence of 0.009 % (9/100,000), increasing to 0.019 % (19.5/100,000) by 2008. The mortality rate is high, with 20 deaths daily. By 2030, WHO predicts 500,000 deaths, 98 % in developing countries like Pakistan [13].
Crucial Risk Factors
The main cause of cervical cancer is HPV, which is transmitted through sexual intercourse [14]. Risks increase with multiple partners, early marriage, and unprotected sex. Other risk factors include an unhealthy lifestyle, a lack of exercise, and contraceptive use. Consuming foods rich in antioxidants and vitamins, like vegetables, seafood, nuts, and fruits, can reduce the risk [15].
Early Detection:Shield Against Cervical Cancer
Early detection is the key to reducing cervical cancer mortality. Screening tests, such as the Pap smear and HPV DNA testing, are tailored based on age (younger women may start with Pap smears, while older women may undergo both Pap smears and HPV testing), specific risk factors (e.g., HPV exposure, immune status), and medical history (e.g., previous abnormal Pap results or family history of cervical cancer) [16]. Developed countries have seen decreased mortality due to effective screening while developing countries face challenges due to inadequate healthcare. Affordable and accessible screening tests are needed in low-income countries [17]. This review covers basic and advanced detection techniques presented in Figure 1.
A Papanicolaou Smear (Pap smear) pap smear is a reliable and common method for detecting cervical cancer. Despite the potential for human error, it remains a widely used detection strategy [18].
HPV types 16, 18, and other high-risk strains are responsible for approximately 70 % of cervical cancer cases worldwide. HPV DNA testing is recommended for detecting these specific strains in women aged 25–74 [19].
VIA (visual inspection with acetic acid) and VILI (visual inspection with Lugol’s iodine) are used to detect abnormalities in the cervix [20].
Colposcopy involves magnifying the cervix to observe abnormalities, in which a speculum is inserted into the vagina and the area of the cervix or vagina is magnified, so then the doctor can easily observe any change or abnormality [21]. To increase the rate of survival from cervical cancer, it is important to detect the disease at an early stage. Early detection is crucial for survival, with developing countries facing high mortality due to late diagnosis and inadequate healthcare. A study by J. Lu et al. (2020) also emphasized that early detection is the key to reducing the rate of cervical cancer mortality all around the world [22].
Conization, or cone biopsy, is another early detection technique for observing abnormalities in the cervix [23].
Nanotechnologies such as nanoparticle-based biosensors, including gold nanoparticle sensors, are being explored for their potential to detect HPV with high sensitivity and specificity [23].
Deep learning and machine learning algorithms analyze large datasets, including histopathological images and cervical cell samples, to detect abnormalities. However, challenges such as ensuring high-quality data and the need for large, well-annotated datasets for training these models remain major hurdles. These algorithms have the potential to be used for cervical cancer detection in the future, but before utilizing these modern techniques, further research must be conducted to ensure the efficiency of these new detection strategies [24].
Commonly used CAD systems for cervical cancer detection include Dynamic Spectral Imaging System (DYSIS), which helps automate the detection process and reduce human error. Computer-aided diagnostic [25].
Conquering Cervical Cancer:Treatment Breakthroughs
There is always a need to develop novel techniques for early detection and treatment of cervical cancer to reduce the mortality rate. However, 80 %–95 % of cervical cancer cases can be cured with chemotherapy or surgery, but the treatment of this metastatic disease remains a challenge [26]. Research is focused on on-
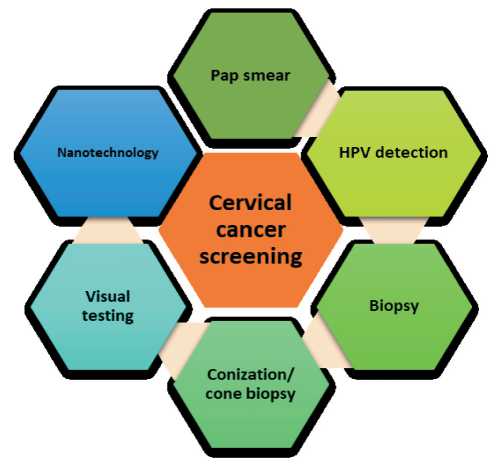
Fig. 1. Screening and Detection Methods for Cervical Cancer. Note: created by the authors
Рис. 1. Методы скрининга и диагностики рака шейки матки. Примечание: рисунок выполнен авторами cogenes and their role in cervical cancer [27]. Studies suggest that oncoproteins can play an important role in inducing or maintaining a specific malignant phenotype. When cervical cancer occurs, numerous abnormal changes also occur, which can alter or disrupt the control of the cell cycle, the immune response against tumor formation, and changes in gene and microRNA expression [28]. This review covers common and advanced treatment strategies presented in Figure 2.
Surgical treatment is the primary method for managing early-stage cervical cancer [29].
Radical hysterectomy is a successful surgical strategy, but to achieve a good survival rate, the patient must
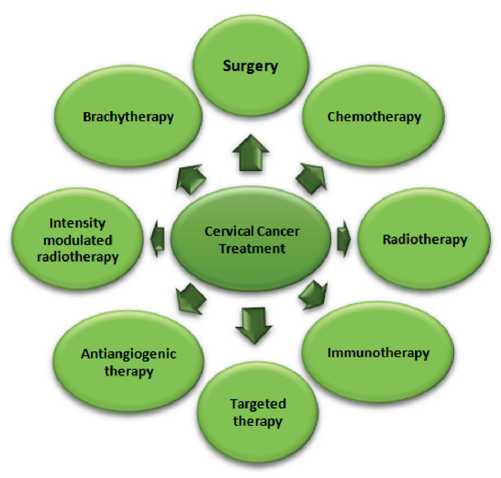
Fig. 2. Current Treatment Options for Cervical Cancer.
Note: created by the authors
Рис. 2. Современные варианты лечения рака шейки матки. Примечание: рисунок выполнен авторами maintain a healthy lifestyle after the operation [30]. Most cervical cancer cases are reported in females at a young age. Trachelectomy, laparoscopic radical hysterectomy, and robotic surgery are used to preserve fertility. Recovery after operation and oncological safety can be maintained by laparoscopic radical hysterectomy. Assessing the lymph nodes can reduce the need for an unwanted lymphadenectomy [31].
Robotic surgery is widely used for early-stage cervical cancer, offering fertility preservation options for young patients [32]. Many female reproductive cancers are being treated and managed by robotic surgery. Young female patients with cervical cancer want to preserve the fertility option to have children in the future. For this purpose, trachelectomy, laparoscopy, and robotic surgery techniques are used. However, it is necessary to conduct more research to ascertain the sensitivity and feasibility of such methods [33].
Radiotherapy is a major treatment method, including intensity-modulated radiotherapy (IMRT), image-guided brachytherapy, and chemoradiation [34]. In the 20th century, concurrent chemotherapy with radiotherapy was introduced, which improved the rate of cervical cancer survival [35].
Intensity-Modulated Radiotherapy (IMRT) is a kind of radiotherapy that can be used to determine the dose of radiotherapy, and gastrointestinal toxicity can also be reduced by IMRT [36].
With the help of image-guided brachytherapy, it is easy to determine the volume of high doses needed to treat tumor extension [37].
To manage and treat cervical cancer, brachytherapy and external beam therapy are common techniques. Brachytherapy can be performed as a preoperative technique [38].
For the treatment of advanced tumors, chemoradiation is used with the boost of brachytherapy [39].
Chemotherapy is common for advanced cervical cancer treatment, with concurrent chemoradiation improving survival rates [40]. 30–40 % of patients with advanced stages are unable to get complete results, which is why taking alternative approaches is required for the improvement of outcomes for each patient. Survival of metastatic and recurrent cervical cancer is improved by bevacizumab treatment. Bevacizumab is an inhibitor that inhibits vascular endothelial growth and is used along with chemotherapy. Further research is required to determine the effects of adjuvant chemotherapy in patients with stage III–IVA. Other studies are also on their way to develop new agents that can be used to target molecular pathways [41].
Angiogenesis is the process in which new blood vessels are developed, which can play an important role in the development of cervical cancer. Anti-angiogenic treatments, which regulate proangiogenic factors such as platelet-derived growth factor and vascular endothelial growth factor, are primarily used in the treatment of advanced cervical cancer [42].
Several studies are being conducted for the development of new treatment methods, including antibody-
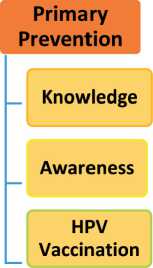
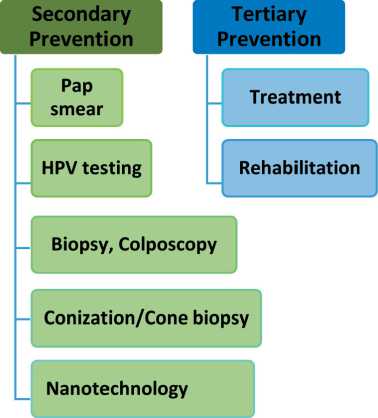
Fig. 3. Cervical cancer prevention includes three approaches: primary prevention, secondary prevention, and tertiary prevention. Note: created by the authors
Рис. 3. Профилактика рака шейки матки включает три подхода: первичная профилактика, вторичная профилактика и третичная профилактика.
Примечание: рисунок выполнен авторами
drug conjugates, vaccines, and immune checkpoint inhibitors, showing promising safety and efficacy results [43].
Preventing Cervical Cancer:Strategies for Protection
Cervical cancer prevention includes three approaches: primary prevention, secondary prevention, and tertiary prevention (Fig. 3).
Primary Prevention
To prevent cervical cancer, knowledge and awareness about sexually transmitted human papillomavirus (HPV) are important. HPV infection can be prevented by vaccination. As HPV is the main cause of cervical cancer, it is responsible for developing many changes in the cervix, which eventually lead to cancer. In 2006, the first vaccine for cervical cancer prevention was licensed, named Gardasil, and developed in Pennsylvania [44]. This vaccine is effective against different types of HPV, which include HPV 6, 11, 16, and 18. Another vaccine, Cervarix, was developed in 2009 in Belgium and is effective against HPV 16 and 18 [45]. Gardasil and Cervarix are prophylactic and now available in more than eighty countries. HPV vaccines such as Cecolin and Walrinvax have been registered in China, while Cervavac has been registered in India. As of August 2024, the WHO prequalified Walrinvax as the fifth HPV vaccine, following prior prequalification of Cecolin, Cervarix, Gardasil, and Gardasil-9. The data confirms that these vaccines are safe and effective in terms of preventing HPV infection [46].
The most successful results from vaccination are reported in Australia, where cases of cervical cancer decreased by a nationwide HPV vaccination campaign. While vaccination campaigns have shown a reduction in HPV infection rates, a decrease in cervical cancer incidence is typically observed after 15–20 years of vaccination [47]. Recent advancements in HPV vaccination strategies include the approval of Cecolin®, a WHO-prequalified vaccine, for use in a single-dose schedule. This decision, based on new evidence, enhances vaccine accessibility and sustainability, particularly in low-resource settings. As of 2024, 57 countries have implemented single-dose schedules, resulting in over 6 million additional girls being vaccinated in 2023. The adoption of this approach aligns with WHO’s cervical cancer elimination target of vaccinating 90 % of girls by 15 years of age and offers a cost-effective alternative to two- and three-dose regimens[48].
Secondary Prevention
Early detection of precancerous lesions is an important way to prevent cervical cancer. In secondary prevention, asymptomatic patients must take detection tests to prevent the spread of cancer. Detection techniques such as Pap smears, HPV DNA testing, visual inspection with acetic acid (VIA), and colposcopy are crucial in identifying cervical cancer early and reducing progression and mortality rates. The greatest example of a decrease in cervical cancer occurrence is from Nordic countries. In these countries, cervical cancer occurrence and mortality rates decreased by 10–80 % by introducing organized cervical cancer detection methods [49].
According to the World Health Organization, countries that are facing economic issues are unable to provide screening tests for every female individual. WHO recommended that in such countries, screening tests be provided for women aged 35 years or older. Women aged 35 or above should go for screening every five years for a minimum of three times during their whole life, which can help reduce cervical cancer mortality in low-resource countries [50].
Tertiary Prevention
The purpose of tertiary prevention of cervical cancer is to reduce disability and aid in rehabilitation. As we know, it is easy to prevent the progression of cervical cancer from precancerous lesions to invasive ones through early detection and diagnosis. To manage cervical cancer properly, cryotherapy and large-loop excision of the transformation zone (LLETZ) is helpful. Cryotherapy is effective when the endocervix is not damaged and only 1–2 quadrants of the cervix are affected [51]. Whereas, LLETZ can be effective in the treatment of the entire transformation zone. LLETZ can also treat the lesion in the endocervical canal if the lesion is not extended to 1 cm [52].
Cryotherapy is less complicated than LLETZ. In the case of cryotherapy, watery discharge is observed for about 3–4 weeks, while vaginal bleeding is rarely reported. Cryotherapy is a simple procedure that does not affect pregnancy or future fertility. Cryotherapy can be performed by any gynecologist. However, in the case of LLETZ, it is necessary to provide an electrical supply during the procedure, and the gynecologist must be very skilled to carry out this procedure. After the LLETZ procedure, blood discharge, cramps, and pain in the abdomen were also reported. LLETZ can also affect fertility in terms of causing preterm labor or even infertility [53].
Use of Artificial Intelligencefor Cervical Cancer Screening and Diagnosis
In the world of modern technology, artificial intelligence (AI) is an amazing breakthrough. AI is helping human beings in various fields, including the field of medical diagnostics. AI is helping in the screening and diagnosis of cervical cancer. The use of AI is beneficial in various ways; it reduces the need for professional personnel and also reduces time consumption. AI use also eliminates the risk of bias in the case of subjective factors [54]. This review focuses on describing the role of AI in cervical cancer screening and diagnosis.
Improving Screening Methods with AI
AI is now being used for the detection, diagnosis, and treatment of cervical cancer. With the use of complex algorithms, AI can extract features, recognize images, and classify them automatically. The use of AI is making screening and diagnosis methods more accurate and also helping to reduce the problem of limited human resources. Studies have confirmed that the accuracy of screening and detection increases with the assistance of AI. The rate of detection accuracy can be improved by AI as compared to standard biopsy results. A study was conducted on 700,000 female individuals to determine the accuracy of AI-based screening methods. In that study, Bao et al. conducted a cytological system based on AI assistance. The results of 94.7 % of cases confirmed a 5.8 % increase in sensitivity as compared to other conventional manual reading methods [55].
For the detection of cancer or CIN, another study was conducted to observe the CIN2 and CIN3+ rates. The results showed that 92.6 % and 96.1 % detection rates were observed for CIN2 and CIN3+, respectively. These results confirmed that AI-based detection methods are significantly more accurate than manual reading methods. The main purpose of screening methods is to differentiate between normal and cancerous lesions [56]. The screening methods focus on normal, CIN1, CIN2, and CIN3+ lesions to determine the severity of cervical cancer. When CIN2 or CIN3 lesions are observed in screening, treatment must be started. For distinguishing low-grade or high-grade lesions, Kim et al. designed an algorithm in which the computer interprets the driven data. In the analysis, they observed the texture and color of cervical cancer images. Which provided 74 % and 90 % sensitivity and specificity for the differentiation of normal, low-grade, and high-grade cervical cancer lesions, respectively. Thus, AI-based screening methods enhance the rate of accuracy and sensitivity for the determination of cervical cancer as compared to normal conventional methods [57].
Pros and Cons of AI Use
Every technique or procedure has its pluses and minuses, as well as some limitations, so AI. AI has helped the field of medical research and diagnosis in various ways, like computing and analyzing images. AI also enhanced the accuracy of screening tests. AI use has made remarkable changes in the field of medical research. With the help of AI-assisted results, doctors are now able to make decisions easily without any doubt, which also reduces the burden of work on them. With the help of AI, the need for technical experts is also reduced, which can be helpful in screening and diagnosing cervical cancer in low-resource countries around the world. However, AI has some limitations


