Clinical and epidemiological characteristics of liver damage during COVID-19 in patients with a fatal outcome
Автор: Mahto Monika Rani, Bommineni Sekar Swathy, Zakirova Gulkaiyr, Buranchieva Aisuluu
Журнал: Бюллетень науки и практики @bulletennauki
Рубрика: Медицинские науки
Статья в выпуске: 6 т.9, 2023 года.
Бесплатный доступ
It is now known that the SARS-CoV-2 virus can infect cells in the gastrointestinal tract as well as the liver. Liver dysfunction is found in 14-53% of patients with COVID-19. Scientists have found that the SARS-CoV-2 virus can directly infect liver cells and cells lining the intra- and extrahepatic bile ducts (cholangiocytes), since they contain, although in low concentrations, a special enzyme ACE-2, which serves as an entry point into cells of some coronaviruses, including SARS-CoV-2. The next stage in the development of pathology is inflammation and the formation of blood clots. With a violent reaction of the immune system, an excessive release of cytokines occurs, which aggravates the condition and, in some cases, leads to reactive hepatitis.
Coronavirus infection, alanine aminotransferase, aspartate aminotransferase, fatty liver
Короткий адрес: https://sciup.org/14127986
IDR: 14127986 | УДК: 616-079.3 | DOI: 10.33619/2414-2948/91/32
Текст научной статьи Clinical and epidemiological characteristics of liver damage during COVID-19 in patients with a fatal outcome
Бюллетень науки и практики / Bulletin of Science and Practice
UDC 616-079.3
It is now known that the SARS-CoV-2 virus can infect cells in the gastrointestinal tract as well as the liver. Liver dysfunction is found in 14–53% of patients with COVID-19. Scientists have found that the SARS-CoV-2 virus can directly infect liver cells and cells lining the intra- and extrahepatic bile ducts (cholangiocytes), since they contain, although in low concentrations, special enzyme ACE-2 which serves as the entry point into cells for some coronaviruses, including SARS-CoV-2 [1-17].
The next stage in the development of pathology is inflammation and formation of blood clots. With a violent reaction of the immune system, an excessive release of cytokines occurs, aggravating the condition and in some cases leading to reactive hepatitis [4, 7-17].
To study the incidence of liver pathologies and the nature of its manifestations in COVID-19 patients with a fatal outcome. The material of the study was the data of a retrospective analysis of 63 case histories of patients with a fatal outcome, hospitalized in the Republican Clinical Infectious Diseases Hospital for the period from May to November 2021. Statistical analysis was performed using Microsoft Office Excel 2016 (Microsoft, USA) and Statistica 10 software (StatSoft Inc., USA).
Results
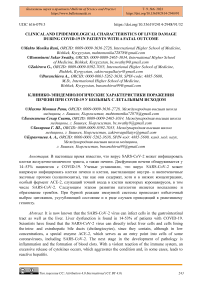
For the period from May to November 2021, there were more men (62%) than women (38%) among the hospitalized patients at the Republican Clinical Infectious Diseases Hospital. The age groups of patients were presented as follows: 25-44 years old — 3 patients (4%), 45-60 years old — 13 patients (21%), 61-75 years old — 37 patients (59%), 76-90 years old — 10 patients (16%) (Figure 1) [3, 8].
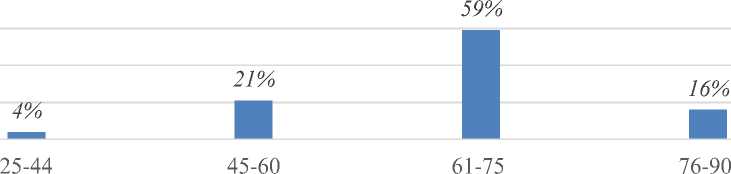
Figure 1. Age structure of COVID-19 patients
As can be seen in Figure 2., the majority of patients were over the age of 60 years and in general accounted for 75% of the total number of patients with a fatal outcome. According to the epidemiological anamnesis, the majority of patients with a fatal outcome, 69.8%, were urban residents, and 30.2% of patients were rural residents, respectively (Figure 2) [5].
Close family contact was noted in 73% of patients, and in 27% of cases contact was not established (Figure 3).
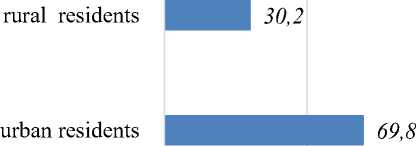
Figure 2. Residents allocation
unknown source of infection patients with family contact
Figure 3. The epidemiological contact with
COVID-19 patients
The prevalence of patients by region is shown in Figure 4, which shows that the majority of patients were from the city of Bishkek and the Chui region. Among patients with fatal outcome, 35 patients (55.5%) were pensioners, 20 patients (31.8%) were unemployed and the remaining 8 patients (12.7%) were employed (Figure 5). The first cases of severe coronavirus infection with a fatal outcome in the period from May to November 2021 began to appear in May. Figure 7 shows that the highest mortality rates were registered in July (51.3%) and November (43%).
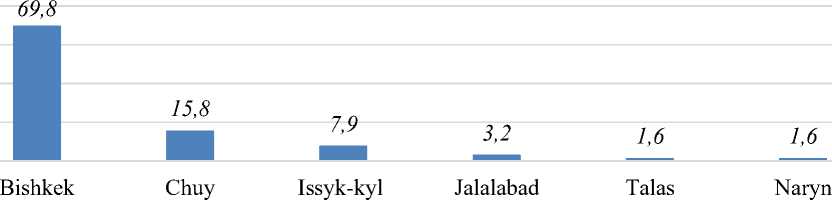
Figure 4. Prevalence by region
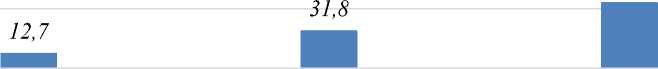
employed unemployed retired people
Figure 5. Employment structure
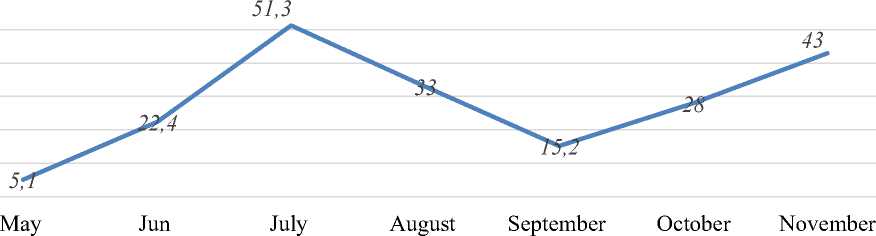
Figure 6. The number of cases of COVID-19 by months
The analysis of clinical symptoms showed that the most common symptoms of patients with Covid-19 were weakness (100%), headache (94%), fever (100%), cough (81%), anosmia, ageusia (52% ), loss or lack of appetite (81%), abdominal pain (68%), pain in the right hypochondrium (64%) (Table). Such symptoms as chest discomfort (21%), palpitations (17%), and peripheral edema (3%) were less common.
Table CLINICAL SYMPTOMS OF COVID-19
|
FREQUENT SIGNS (30%) > |
OCCASIONAL SIGNS (30%) < |
||
|
Clinical signs |
Clinical signs |
||
|
Headache |
94% |
Nausea |
27% |
|
Fever |
100% |
Vomiting, diarrhea |
20% |
|
Dry cough |
81% |
Chills |
25% |
|
Loss of smell, loss of taste |
52% |
Muscle and joint pain |
21% |
|
Weakness |
100% |
Chest discomfort |
21% |
|
Shortness of breath |
78% |
Palpitation |
17% |
|
Loss of appetite |
81% |
Dizziness |
27% |
|
Abdominal distention, abdominal pain |
68% |
Peripheral edema |
3% |
|
Pain in the right upper part of abdomen |
64% |
||
The severe form of the disease was predominant, and this form developed in patients with a burdened premorbid background.
As can be seen in Figure 8, 62% of patients with a fatal outcome had concomitant diseases from the cardiovascular system, pathologies of the gastrointestinal tract (35%), diabetes mellitus (35%), hypertension (32%), chronic hepatitis (30 %), which contributed to the severe course of the disease with the development of a lethal outcome. Patients experienced complications such as ARDS (98.5%), multiple organ failure (92.3%), DIC (96.8%), respiratory failure (90%), community-acquired pneumonia (98.3%), brain edema (86.5%), cardiovascular insufficiency (83%), sepsis (56%) and others. Pneumonia and acute respiratory distress syndrome, DIC were the leading causes of death in the period from May to November 2021.
Cardiovascular system disorders
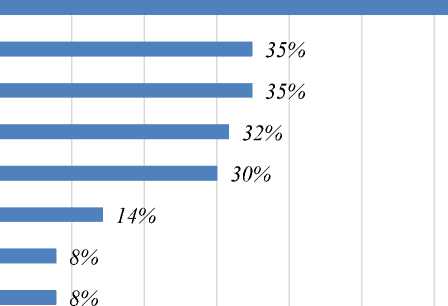
62%
Pathological changes of the gastrointestinal tract
Diabetes melitus
Hypertension
Chronic hepatitis
Urinary tract disorders
Obesity
Anemia
Figure 7. Comorbidities in COVID-19 patients with fatal outcome
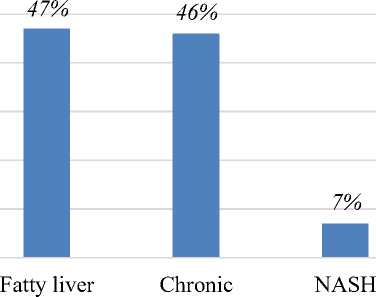
A complex of clinical and laboratory studies revealed the following. On average, patients with a fatal outcome were admitted on the 7th-8th day of illness and stayed in hospital for 26 days. It is necessary to note the dynamics of the increase in the level of transaminases on days 12-13 of the disease with a predominance of the ALT level, which indicated the severity of the course of the disease (Figure 8). In a laboratory and instrumental study of abdominal ultrasound in patients with a fatal outcome, the following changes in the function of the gastrointestinal tract were found: fatty hepatosis (47%), chronic hepatitis (46%) and steatohepatitis (7%) (Figure 9) [3, 9].
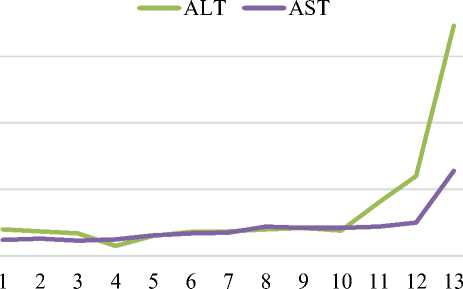
Figure 8. Dynamics of AST and ALT activity during hospitalization
hepatitis
Figure 9. Liver ultrasound data in patients with fatal outcome
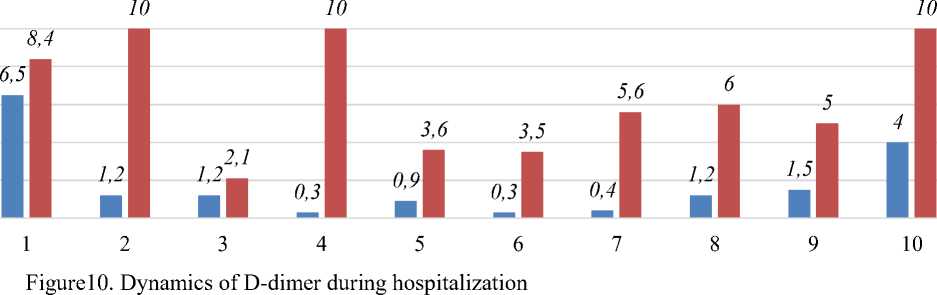
As can be seen from Figure 9, fatty hepatosis (47%) and chronic hepatitis (46%) occurred with almost the same frequency, which may have contributed to the aggravation of the course of the disease and the development of lethal outcome. In Figure 10, we see a persistent rise in the D-dimer index, which are determinants of thrombosis.
■ D-dimer on admission(mg/l) ■ D-dimer in dynamics(mg/l)
Conclusions
Liver pathology is often developed in males over 60 years of age. Liver pathology is often developed with concomitant diseases of the hepato-biliary system. Transaminase activity increases in the second week in patients with a fatal outcome. The causes of death in patients were pneumonia, ARDS, DIC. Ultrasound data of patients with COVID-19 with fatal outcome more often detected NAFLD and chronic hepatitis.
Список литературы Clinical and epidemiological characteristics of liver damage during COVID-19 in patients with a fatal outcome
- Bloom, P. P., Meyerowitz, E. A., Reinus, Z., Daidone, M., Gustafson, J., Kim, A. Y., ... & Chung, R. T. (2021). Liver biochemistries in hospitalized patients with COVID‐19. Hepatology, 73(3), 890-900. https://doi.org/10.1002/hep.31326
- Cai, Q., Huang, D., Yu, H., Zhu, Z., Xia, Z., Su, Y., ... & Xu, L. (2020). COVID-19: Abnormal liver function tests. Journal of hepatology, 73(3), 566-574. https://doi.org/10.1016/j.jhep.2020.04.006
- Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., ... & Zhong, N. S. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine, 382(18), 1708-1720. https://doi.org/10.1056/NEJMoa2002032
- National Health Commission of the People's Republic of China. (2020). Handbook of prevention and treatment of the pneumonia caused by the novel coronavirus (2019‐nCoV). National Health Commission of the People’s Reupblic of China.
- Li, G., Fan, Y., Lai, Y., Han, T., Li, Z., Zhou, P., ... & Wu, J. (2020). Coronavirus infections and immune responses. Journal of medical virology, 92(4), 424-432. https://doi.org/10.1002/jmv.25685
- Zhang, Y., Zheng, L., Liu, L., Zhao, M., Xiao, J., & Zhao, Q. (2020). Liver impairment in COVID‐19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver international, 40(9), 2095-2103. https://doi.org/10.1111/liv.14455
- Chyngyshpaev, D. S., Kerimaly, M., Pasanova, A. M., Alymkulov, A. T., Uzakova, A. O., & Uzakov, O. J. (2022). Prognostic value of osteoprotegerin in assessing risk of cardiovascular complications and osteoporotic fractures in comorbid pathology. Eurasian Medical Journal, (7), 17- 25. https://doi.org/10.1530/EJE-08-0554 13
- Sharma, M., & Buranchieva, A. A. (2020). Clinical and epidemiological characteristics of Covid-19 in Jaipur, India during the pandemic. Eurasian Medical Journal, (2), 23-27. https://doi.org/10.52680/16948254_2020_2_23
- Soni, D., & Buranchieva, A. A. (2020). Epidemiological features of Covid-19 in Kota (Rajasthan, India). Eurasian Medical Journal, (2), 13-15.
- Uzakov, O. Z., Komissarova, S. Y., Alymkulov, A. T., & Kermaly, K. M. (2021). Comparative characteristics of the frequency and level of anxiety disorders among respondents living in Kyrgyzstan and Kazakhstan during the COVID-19 pandemic. Eurasian Medical Journal, (3), 24-31. https://doi.org/10.52680/16948254_2021_3_24
- Asheraliev, M. E., Alymkulov, A. T., & Richa, G. (2021). Frequency and possible causes of biliary dyskinesia in patients with bronchial asthma in the Kyrgyz Republic. Eurasian Medical Journal, (3), 3-7. https://doi.org/10.52680/16948254_2021_3_3
- Uzakov, O. Zh., Komissarova, S. Yu., & Alymkulov, A. T. (2020). Ob organizatsii tsentra reabilitatsii lyudei v “belykh khalatakh”. Meditsina Kyrgyzstana, (3), 24-25. (in Russian).
- Uzakov, O., Akhunbaev, S., Komissarova, S., & Alymkulov, A. (2020). Anxiety Disorder, Depressive Symptoms and Sleep Quality During COVID-19. Bulletin of Science and Practice, 6(9), 120-126. (in Russian). https://doi.org/10.33619/2414-2948/58/13
- Abaeva, T. S., Satybalbiev, M. A., Alymkulov, A. T., & Ergesheva, A. M. (2019). Morphology of intramural lymph vessels of the human heart. Heart, Vessels and Transplantation, 3(4), 173-176. https://doi.org/10.24969/hvt.2019.148
- Baktybekova, M. B., Alymkulov, A. T., & Abaeva, T. S. (2018). Struktury limfangionov grudnogo protoka. Vestnik Kyrgyzsko-Rossiiskogo Slavyanskogo universiteta, 18(6), 156-157. (in Russian).
- Akhunbaev, S. M., Uzakov, O. Zh., Atykanov, A. O., & Alymkulov, A. T. (2021). Reaktivnaya i lichnostnaya trevozhnost' u meditsinskikh rabotnikov v sravnenii mezhdu pervymi I vtorymi volnami COVID-19 v Kyrgyzskoi Respublike – prospektivnaya kogorta . In Materialy Vserossiiskoi nauchno-prakticheskoi konferentsii «Nauka i sotsium» (No. XII, pp. 14-21). (in Russian). https://doi.org/10.38163/978-5-6045317-2-3_2021_14
- Alymkulov, A. T., & Satybaldiev, M. A. (2018). O limfangionakh serdtsa cheloveka. Vestnik Mezhdunarodnogo Universiteta Kyrgyzstana, (3), 39-43. (in Russian).