Clinical assessment difference between patellar resurfacing and retention groups with grade IV osteoarthritis in total knee arthroplasty
Автор: Kamolhuja Eshnazarov, Jong Keun Seon, Eun Kyoo Song
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 4, 2015 года.
Бесплатный доступ
Introduction. Despite the excellent clinical success with total knee arthroplasty (TKA), there is disagreement about whether or not to replace the patellar articular surface. This led to randomized controlled trials. Such studies are the most reliable source of evidence of the effectiveness of potential interventions. But most of these studies include the study of results at all degrees of osteoarthritis of the patellofemoral joint. Therefore, the authors conducted a prospective study to compare the clinical and radiological outcomes after TKA with the replacement of the patellar articular surface in patients with osteoarthritis of the patellofemoral joint of the fourth degree. Materials and methods. The study included 123 patients with Kellgren-Lawrence patellofemoral joint osteoarthritis. Patients were randomly assigned to groups, in one of which the patellar joint surface was replaced (62 cases), in the other case, they were not performed, i.e. retained the patella (61 cases). Among them were 114 patients who were observed for more than two years (group with replacement of the articular surface - 59 cases, the group without replacement - 55 cases). Preoperative and postoperative clinical data were evaluated and evaluated on the scale of the Hospital for Special Surgery Patellar (HSSP) (total score of 100, presence of pain in the anterior part of the knee, functional limitations, tenderness in palpation or pressure, crepitation , Q-force). Scales developed at the Special Surgery Hospital (HSS), and the WOMAC scale, as well as the volume of movements (ROM), were also used. Results. The mean HSSP score in the group with replacement of the patellar articular surface was 85 points and 83 points in the group without replacement, which showed no significant differences between the groups (p = 0.75). When assessing the presence of pain in the anterior part of the knee, there were also no significant differences between the groups (40 in the group with articular replacement, 36 in the group without replacement, p = 0.52). HSS scores improved to 94 points in the group with articular replacement and up to 95 in the group without replacement, which also indicated no significant difference (p = 0.92). The WOMAC score and the volume of movements were 32 and 128 ° ± 10.5 ° in the replacement group and 29 points and 126 ° ± 11.5 ° - in the group without replacement, there was no significant difference between the groups (p> 05) . The conclusion. Thus, identical good clinical outcomes without significant differences were achieved after TKA with and without replacing the patellar articular surface in patients with a high degree of osteoarthritis of the patellofemoral joint. TKA without replacing the articular patella surface is a good option in patients with a high degree of osteoarthritis of the patellofemoral joint.
Knee osteoarthritis, total knee arthroplasty, patella resurfacing
Короткий адрес: https://sciup.org/142134611
IDR: 142134611 | УДК: 616.718.49-002-089.844 | DOI: 10.18019/1028-4427-2015-4-27-30
Текст научной статьи Clinical assessment difference between patellar resurfacing and retention groups with grade IV osteoarthritis in total knee arthroplasty
In the patients with knee osteoarthritis widely use total knee arthroplasty (TKA), because the destruction and degree of deterioration of the articular surface cartilage are more occurring [1].
Despite the improvement equipment technologies, surgery techniques, results of treatment knee osteoarthritis and the excellent clinical success of TKR, controversy remains concerning whether or not to resurface the patella [2, 5, 7].
This has led to a number of clinical and randomized controlled trials [3, 4, 5]. Randomized controlled trials constitute the most reliable source of evidence for the evaluation of the efficacy of a potential intervention. But most of these studies
Ш Kamolhuja Eshnazarov, Jong Keun Seon, Eun Kyu Song. Клиническая оценка различий при тотальной артропластике коленного сустава с заменой суставной поверхности надколенника и без нее у пациентов с остеоартритом IV степени // Гений ортопедии. 2015. № 4. С. 27-30.
include all degree of osteoarthritis of the patellofemoral joint [4, 5, 12]. And on the other hand numerous research were conducted to certain solves of the questions resurfacing or retention patellofemoral joint. [6, 7, 8, 10], however precise definition of the issue decision patellar resurfacing in patients with grade IV osteoarthritis on patellofemoral joint, undergoing TKA did not specify no one of the studies.
The purpose of this prospective study was to compare clinical outcomes after TKA with or without patellar resurfacing in patients with grade IV osteoarthritis on patellofemoral joint. We enrolled only patients with Kellgren-Lawrence grade IV or ICRS grade IV osteoarthritis on patellofemoral joint performed primary TKA.
MATERIALS AND METODS
To study our goal we have gathered all the materials of the patient with osteoarthritis grade IV on patellofemoral joint, undergoing TKA in Chonnam National University Hospital during the 2004-2013 years (123 cases). Preoperatively and intraoperatively were confirmed a high grade of osteoarthritis in each patient. The patients assessed clinical outcomes were divided into two groups, 62 cases of patellar resurfacing and 61 cases of patella retention group. Among them, 114 cases that could be followed for more than 2 years were included in this study, 59 cases of resurfacing group and 55 cases of retention group.
In patellar resurfacing group were 59 knees of 42 patients which average age equal 66.3 year and in retention group 55 knees of 49 patients with average age were 65.6 year. Gender demographics shows that most of the researched patients with osteoarthritis grade IV on patellofemoral joint were female: in resurfacing group 31 female, 11 male and in non-resurfacing group 42 female, 7 male. Patients were performed cemented primary TKA with patellar resurfacing and retention with a medial parapatellar approach. In the retention group, we did patelloplasty including osteophyte removal and denervation around patellar using electrocautery (Figure 1). For the patients performing patellar resurfacing were used 3 – Peg all – polyethylene patella implant after remove all osteophytes and synovial insertions from around the patella (Figure 2). For the comparison of preoperative state of the patient and clinical outcomes, we evaluated and compared outcomes regarding the total and subjective anterior knee pain scores based on the Hospital for Special Surgery Patellar (HSSP) scoring system. We also compared Hospital for Special Surgery (HSS) and WOMAC score, and range of motion (ROM) before and after surgery in both groups.

Figure 1. Patellaplasty including osteophyte removal and denervation around patellar using electrocautery

Figure 2. Postoperative Resurfacing and Retention Patellofemoral Joint
RESULTS
The clinical assessment results before surgery in both Almost repeating the preoperative assessment results groups were approximately similar without big difference. between the clinical finds studying groups postoperatively were inconsiderable difference.
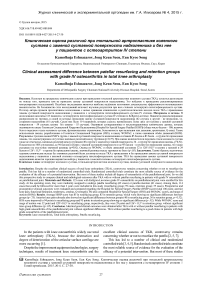
Difference between average preoperative and postoperative HSS score in resurfacing group was 46.3 point and in retention group 49 point. The findings showed significant improving results of treatment (Figure 3).
Preoperative average HSSP score in patients were almost identical 64.3±9.7 within resurfacing and 63.7±10.5 in retention groups. Postoperative measures results showed a marked improvement of indicators average 85.2±6.4 within resurfacing group and 83.4±5.9 in retention group, which were showing no significant differences outcomes assessment between groups (p=0.75). While WOMAC score after surgery was 31.7±6.4 point in resurfacing group, respectively, 29.2±6.9 point was in retention group, without significant intergroup difference (Figure 4).
Anterior knee pain subscale also showed no significant differences between groups (P-value: 0.52). In resurfacing group preoperative anterior knee pain was 28.6±7.6 with growing to 40.3±6.2 postoperatively and in retention group was 29.0±8.7 before surgery with improving to 38.2±5.7 after surgery. Despite the high limitation of movement within knee joints were identified in the patents before surgery, postoperative ranges of motion were sufficiently satisfied (Figure 5). In terms of peripatellar complication, we observed painless patellar crepitus in 3 cases of resurfacing group and 6 cases of retention group.
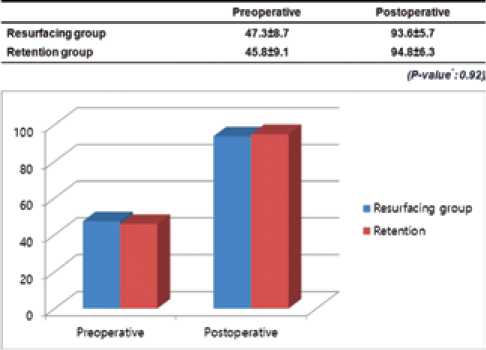
Figure 3. HSS score
Figure 4. WOMAC score
DISCUSSION
Figure 5. ROM
This unresolved questions, performing or not performing patellar resurfacing in TKR still leads to a lot of discussion. Some authors finds shows that patient with not resurfaced knees had slightly better satisfaction than patellar resurfaced patients [3, 9] and with correctly execution TKA, resurfacing patella is unnecessary [10, 13]. But after obtaining good clinical outcomes and because of the possibility of a subsequent deterioration of the patella with osteoarthritis in long-term follow-up, other group of researches consider that resurfacing of the patella during primary total knee arthroplasty is one of the best solution [2, 12, 16, 20]. To studying outcomes result after total knee arthroplasty in the patient with patellar resurfacing and retention we separated particular group of patients.
During the selecting a solution resurfacing or retention patellar surface we must pay attention to a lot of criteria; preoperative clinical diagnostic measures, intraoperative findings and of course postoperative treatment outcomes.
The majority of patients with pathology of the knee osteoarthritis radiologically determined patellofemoral osteoarthritis with severe of grade [16, 17]. However we include in our study only the high degree of patellofemoral osteoarthritis. Determination of the grade of osteoarthritis using with Kellgren-Lawrence grade widely used by many researchers [18, 19].
Based on these decisions we enrolled only patients with Kellgren-Lawrence grade IV or ICRS grade IV osteoarthritis on patellofemoral joint performed primary TKA. Assessment of the patellar cartilage intraoperative and make decision on patellar resurfacing are trustworthy in patient undergoing TKR after osteoarthritis, however, despite the patellar cartilage was damaged, only the status of the patellar articular cannot be determining main factor for patellar resurfacing [5]. Naturally and we intraoperatively checked the preoperative diagnostic findings.
When osteoarthritis has not severe pain even there are many changes in the cartilage, treatment knee arthritis manage without patellofemoral arthroplasty [14]. Patellar resurfacing have better functional results in patient with several arthritis as compared with patellar retention and lead the most reliable clinical results in patient with noninflammatory groups [2, 4, 7] and has low complications rate and morbidity for the treatment of anterior knee pain [6, 8, 11]. To determine the answer this issue we decided to study difference between clinical assessment outcomes in both group. Some authors showed significantly better clinical rating Knee Society Scores in the unresurfaced patient group [4, 9]. But many of authors believe that measures of surgical outcomes like WOMAC is more precisely reflect patient satisfaction in patellofemoral arthroplasty [12, 16] or another researchers are prefer using HSS scores to definition patients satisfaction after TKA [20]. To get more detailed clinical results, we used once preoperative and postoperative determination difference between the patients groups several assessment methods: The Hospital for Special Surgery Patellar (HSSP) score (total 100 point; anterior knee pain, functional limitation, tenderness, crepitus, Q-strength), Hospital for Special Surgery (HSS), WOMAC scores, and range of motion (ROM). Our clinical results after surgery showed higher improving (average WOMAC 23.7 point, Anterior knee pain 11.3 point and Range of motion 12 degree) than other authors results [3, 12, 16]. But difference postoperative results between group were equal with other authors results
[4, 5, 9] showing not significant statistic results.
In TKA performed without resurfacing, the patella contact force does not significantly increase and cartilage contact stress doesn't increase and this lead to prevent most expected complications [13]. Nevertheless the risk of postoperative complications is highest in patellar resurfacing group than not resurfacing group [3]. To conclude to this view and we believe that getting a good result from the treatment of osteoarthritis of the knee, is more dependent on the correct technical operation, rather than performing patellar resurfacing or not.
Notwithstanding our study intended to achieve a specific decision to making or not patellofemoral arthroplasty during the primary TKR in patient with Kellgren-Lawrence grade IV or ICRS grade IV osteoarthritis and had a wider range of assessment there were some limitations. We cannot include in our study all of the methods of clinical assessment and not described all prosthesis and implants features.
CONCLUSION
Identical good clinical outcomes were obtained after TKA with or without patellar resurfacing in patients with high grade osteoarthritis of the patellofemoral joint without significant differences. TKA without patellar resurfacing is a good choice in patients with high grade osteoarthritis of the patellofemoral joint.
Список литературы Clinical assessment difference between patellar resurfacing and retention groups with grade IV osteoarthritis in total knee arthroplasty
- The degeneration and destruction of femoral articular cartilage shows a greater degree of deterioration than that of the tibial and patellar articular cartilage in early stage knee osteoarthritis: a cross-sectional study/S. Hada, H. Kaneko, R. Sadatsuki, L. Liu, I. Futami, M. Kinoshita, A. Yusup, Y. Saita, Y. Takazawa, H. Ikeda, K. Kaneko, M. Ishijima//Osteoarthritis Cartilage. 2014. Vol. 22, No 10. P. 1583-1589.
- Hanssen A.D. Orthopaedic crossfire -All patellae should be resurfaced during primary total knee arthroplasty: in the affirmative//J. Arthroplasty. 2003. Vol. 18, No 3 Suppl. 1. P. 31-34.
- Selective patellar resurfacing in total knee arthroplasty: a prospective, randomized, double-blind study/D.W. Roberts, T.D. Hayes, C.T. Tate, J.P. Lesko//J. Arthroplasty. 2015. Vol. 30, No 2. P. 216-222.
- Resurfacing versus not resurfacing the patella in total knee arthroplasty/D. Mayman, R.B. Bourne, C.H. Rorabeck, M. Vaz, J. Kramer//J. Arthroplasty. 2003. Vol. 18, No 5. P. 541-545.
- Intraobserver and interobserver reliability of the assessment of the patellar articular cartilage in osteoarthritic patients undergoing total knee arthroplasty/I. Han, C.B. Chang, Y.G. Kang, S.W. Yoon, S.C. Seong, T.K. Kim//J. Arthroplasty. 2006. Vol. 21, No 4. P. 567-571.
- The impact of patellar resurfacing in two-stage revision of the infected total knee arthroplasty/A. Glynn, R. Huang, J. Mortazavi, J. Parvizi//J. Arthroplasty. 2014. Vol. 29, No 7. P. 1439-1442.
- Patellofemoral arthritis/J.A. Karam, C.A. Higuera, E.B. Smith, P.F. Sharkey//Operative Techniques in Orthopaedics. 2012. Vol. 22, No 4. P. 196-202.
- Garcia R.M., Kraay M.J., Goldberg V.M. Isolated resurfacing of the previously unresurfaced patella total knee arthroplasty//J. Arthroplasty. 2010. Vol. 25, No 5. P. 754-758.
- Farr J., Lattermann J. Management of patellofemoral arthritis without arthroplasty//Semin. Arthroplasty. 2009. Vol. 20, No 3. P. 136-141.
- Total knee arthroplasty without patellar resurfacing in isolated patellofemoral osteoarthritis/N.W. Thompson, A.L. Ruiz, E. Breslin, D.E. Beverland//J. Arthroplasty. 2001. Vol. 16, No 5. P. 607-612.
- Leadbetter W.B., Mont M.A. Patellofemoral arthroplasty: a useful option for recalcitrant symptomatic patellofemoral arthritis//Semin. Arthroplasty. 2009. Vol. 20, No 3. P. 148-160.
- Patellar reshaping versus resurfacing in total knee arthroplasty -Results of a randomized prospective trial at a minimum of 7 years' follow-up/Z.T. Liu, P.L. Fu, H.S. Wu, Y. Zhu//Knee 2012. Vol. 19, No 3. P. 198-202.
- Patellar contact forces with and without patellar resurfacing in total knee arthroplasty/R. Singerman, S.M. Gabriel, C.B. Maheshwer, J.W. Kennedy//J. Arthroplasty. 1999. Vol. 14, No 5. P. 603-609.
- Bumbaširevic M., Lešic A., Bumbaširevic V. Anterior knee pain//Orthop. and Trauma. 2010. Vol. 24, No 1. P. 53-62.
- Factors affecting the outcome of distal realignment for patellofemoral disorders of the knee/C.J. Wang, Y.S. Chan, H.H. Chen, S.T. Wu//Knee. 2005. Vol. 12, No 3. P. 195-200.
- Farrokhi S., O’Connell M., Fitzgerald G.K. Altered gait biomechanics and increased knee-specific impairments in patients with coexisting tibiofemoral and patellofemoral osteoarthritis//Gait Posture. 2015. Vol. 41, No 1. P. 81-85.
- Is patellofemoral osteoarthritis common in middle-aged people with chronic patellofemoral pain?/R.S. Hinman, J. Lentzos, B. Vicenzino, K.M. Crossley//Arthritis Care Res. 2014. Vol. 66, No 8. P. 1252-1257.
- Hidden osteophyte formation on plain X-ray is the predictive factor for development of knee osteoarthritis after 48 months -data from the Osteoarthritis Initiative/J. Katsuragi, T. Sasho, S. Yamaguchi, Y. Sato, A. Watanabe, R. Akagi, Y. Muramatsu, S. Mukoyama, Y. Akatsu, T. Fukawa, J. Endo, H. Hoshi, Y. Yamamoto, T. Sasaki, K. Takahashi//Osteoarthritis Cartilage. 2015. Vol. 23, No 3. P. 383-390.
- Sensitivity and associations with pain and body weight of an MRI definition of knee osteoarthritis compared with radiographic Kellgren and Lawrence criteria: a population-based study in middle-aged females/D. Schiphof, E.H. Oei, A. Hofman, J.H. Waarsing, H. Weinans, S.M. Bierma-Zeinstra//Osteoarthritis Cartilage. 2014. Vol. 22, No 3. P. 440-446.
- Does malrotation of components correlate with patient dissatisfaction following secondary patellar resurfacing?/G. Bhattee, P. Moonot, R. Govindaswamy, A. Pope, N. Fiddian, A. Harvey//Knee. 2014. Vol. 21, No 1. P. 247-251.