Combination of type I diabetes mellitus and diabetes associated with GCK gene mutation: features of the clinical course in puberty
Автор: Cherkasova Yulia B., Pavlov Bogdan V., Sokolova Alyona I., Gladyshev Mikhail A., Kurochkin Artem D., Dukova Alexandra A., Sklyarov Bogdan A.
Журнал: Cardiometry @cardiometry
Статья в выпуске: 24, 2022 года.
Бесплатный доступ
This article discusses a clinical case of the manifestation of MODY2 diabetes, which complicated the course of type I diabetes mellitus in a patient of puberty. For 9 months, the dynamics of the patient's condition was monitored, who was on inpatient treatment in the endocrinology department of the State Medical Institution of the Tambov City Hospital for the entire period of observation. The criteria for daily monitoring of the patient's clinical condition were: blood glucose and glycated hemoglobin, the level of glucosuria, the concentration of ketone bodies in the blood and acetone in the urine. The patient underwent insulin therapy and infusion therapy. Despite the ongoing treatment, including, among other things, the treatment of complications of the underlying disease, by the 6th month the patient's condition worsened to an extremely severe degree. Additional laboratory and instrumental diagnostic studies were conducted, including a molecular genetic study for diabetes typing, the results of which made it possible to determine the cause of the progressive course of type I diabetes mellitus, which was the clinical manifestation of MODY2 diabetes with the development of insulin tolerance against the background of hormonal adjustment of puberty. The problem of timely and accurate diagnosis, and, accordingly, correct treatment, of type I diabetes mellitus combined with MODY2 diabetes, remains urgent and serious, due to the difficulty of interpreting differential diagnostic criteria with progressive type I diabetes mellitus of childhood and adolescence, which in turn can lead to multiple complications, including fatal exodus.
Mody, type i diabetes mellitus, blood glucose level, gen gck
Короткий адрес: https://sciup.org/148326586
IDR: 148326586 | DOI: 10.18137/cardiometry.2022.24.210216
Текст научной статьи Combination of type I diabetes mellitus and diabetes associated with GCK gene mutation: features of the clinical course in puberty
Imprint
Yulia B. Cherkasova, Bogdan V. Pavlov, Alyona I. Sokolova, Mikhail A. Gladyshev, Artem D. Kurochkin, Alexandra A. Duko-va, Bogdan A. Sklyarov. Combination of type i diabetes mellitus and diabetes associated with gck gene mutation: features of the clinical course in puberty. Cardiometry; Issue 24; November 2022; p. 210-216; DOI: 10.18137/cardiometry.2022.24.210216; Available from:
The global trend of a scaled increase in diabetes mellitus is a serious medical and social problem. Against the background of the wide spread of classical forms of diabetes mellitus, such as type 1 and type 2 diabetes, its rarer types with specific clinical presentation, course and prognosis, including MODY, are increasingly being diagnosed [1-3].
MODY diabetes is a heterogeneous group of genetic diseases with autosomal dominant inheritance, characterized by impaired functioning of pancreatic β-cells. MODY debuts at a young age. It is diagnosed in 2-5% of the total number of patients with diabetes mellitus of all types [1,4,5].
According to world statistics, MODY occurs in 1 case per 10,000 adults and 1 case per 23,000 children [6].
There are several subtypes of MODY-diabetes, of which MODY2 is the most common in Russia. As of 2021, 50 cases of neonatal diabetes mellitus (1 in 152,280) have been registered in Russia, a molecular genetic study has been performed, however, the prevalence of GCK in Russia remains largely uncertain due to the lack of nationwide screening for diabetes-associated autoantibodies and limited access to molecular genetic testing [7-9].
MODY2 diabetes is associated with mutations in the glucokinase (GCK) gene. Glucokinase is a regulator of maintaining glucose homeostasis at the level of the pancreas and liver. The consequence of the GCK gene mutation is a violation of glucose phosphorylation and, as a result, a failure in the regulation of insulin synthesis. More than 600 mutations in the GCK gene have been identified [8,10-13].
MODY2 is milder than other subtypes and is characterized by an asymptomatic course, moderate fasting hyperglycemia, the average level of glycemia is determined in the range of 5.5–8.0 mmol/l, HbA1c often does not exceed the upper limit of normal [8,9].
Such features of the clinical picture in the vast majority of cases lead to erroneous diagnoses, which in turn predetermines an incorrect treatment strategy with negative consequences. In view of this, only knowledge and a clear understanding of the etiology, pathogenetic mechanisms and specifics of the clinical manifestations of MODY will make it possible to correctly assume the diagnosis, verify it by molecular genetic testing, and develop a competent and effective treatment strategy with an individual approach [6,10,14].
Case description
on September 5, 2019, a boy X, born in 2005, was admitted to the Department of Endocrinology of the State Budgetary Healthcare Institution of Children’s Children’s Hospital of the Republic of Uzbekistan with complaints of severe thirst (the amount of fluid consumed per day was 5-6 liters), frequent urination, nausea, repeated vomiting that did not bring relief. When collecting an anamnesis, he answered questions slowly, was inhibited and disoriented in space. The level of glucose in the blood at admission was 21.3 mmol/l, glycated hemoglobin 6.7%, C-peptide 0.02 ng/ml, acetone in the urine 960 mg/l +++. The patient’s height is 172 cm, weight 63 kg, BMI 21.3.
Diagnosis at admission: Insulin-dependent diabetes mellitus in the stage of decompensation.
Medical history. At the age of 7 years, 2 weeks after undergoing surgical treatment of varicocele under local anesthesia, the patient showed a decrease in activity and constant drowsiness, frequent mood swings, increased thirst, frequent urination, loss of appetite. On May 8, 2012, the patient’s condition worsened, multiple vomiting began on the background of food or liquid intake. The boy was taken to the intensive care unit of the hospital on duty. Type 1 diabetes mel-litus was diagnosed, blood sugar level at the time of admission was 25.1 mmol/l, C-peptide 0.02 ng/ml, glycated hemoglobin 8%. The patient was prescribed dosed insulin therapy, which included 16 IU of Ac-trapid against the background of infusion therapy. After transfer to the endocrinology department, the patient was prescribed insulin therapy: Actrapid - 16 IU four times and Protafan HM - 28 IU twice a day. Regularly, the local therapist and endocrinologist of the polyclinic at the place of residence carried out correction of insulin therapy with a gradual increase in dosage, which by the age of 13 was: Actrapid - 24 IU, Protafan HM - 48 IU.
Anamnesis of life. The child was born full-term, with a weight of 3700 grams and a height of 52 cm. From the first days was bottle-fed (according to the results of research by Nicolai A. Lund-Blix et al., 2017, it was found that the risk of developing type 1 diabetes is twice as high in children who are formula-fed) [6]. From the age of 1 year, the child suffered from chronic tonsillitis. At the age of 4, he underwent a tonsillectomy. At the age of 5 he had been ill with rubella, at the age of 6 he had chicken pox of a protracted course. At 6 years after vaccination, a subscapular lipoma developed at the injection site, which was removed. At the age of 7, he underwent surgical treatment of varicocele. Before each surgical intervention, the patient underwent a biochemical blood test, including the level of blood glucose and glycated hemoglobin. All indicators were within the reference values. Hereditary history of diabetes mellitus is burdened on the maternal side.
On admission on the first day of hospitalization, the following treatment was prescribed:
-
1. 450 ml of NaCL solution 0.9% IV drip (60 drops / min) 2 times a day, at 8:00 and at 20:00.
-
2. Insulin therapy in / in 15 IU of Actrapida every 2 hours, during the infusion of NaCL - in / in, continuously using a dispenser. Subcutaneous insulin injections every 4 hours, depending on food intake and blood glucose levels.
-
3. Ringer-Lock solution 400 ml for 4 hours intravenously (60 drops / min), 10 ml / kg 2 times a day, in the morning - 400 ml, in the evening - 200 ml.
-
4. Antiemetic drug - Cerucal 1/2 tab / day.
-
5. Enterosorbent - Enterosgel (15 g per 100 mg of water 1 hour before meals)
Medical tests were prescribed: general urinalysis, complete blood count, biochemical blood test, glycated hemoglobin.
Within 3 days, the level of glucose in the blood did not decrease and remained within the range of 22-30 mmol / l, after which the treatment was adjusted:
-
1. NaCL solution 0.9% IV drip, 80 drops / min, 350 ml 2 times a day, at 8:00 am and 20:00 pm.
-
2. Insulin therapy: in / in 25 units of Actrapid using a dispenser with interval administration; subcutaneously prolonged insulin 44 IU Protafana HM.
-
3. Ringer-Lock solution 200 ml, for 3 hours, intravenously, 80 drops / min, 10 ml / kg, 2 times a day, in the morning - 200 ml, in the evening - 100 ml.
-
4. Enterosorbent - Enterosgel (20 g per 100 mg of water 1 hour before meals)
The indicator of acetone in urine decreased to 724 mg/l ++. The patient stopped vomiting and had a slight appetite. Against the background of increased thirst, polyuria was noted. The patient is lethargic, but the consciousness is clear.
On day 6, the blood glucose level decreased, but did not fall below 15.5 mmol/L. The specialists decided to transfer the patient from the intensive care unit to the endocrinology unit. Therapy was prescribed according to the blood glucose level:
-
1. NaCL solution 0.9% IV drip 70 drops/min, 250 ml, 1 time per day.
-
2. Insulin therapy: in / in 15 units of Actrapid using a dispenser with interval administration; subcutaneously prolonged insulin 44 IU Protafana HM and Actrapid 24 IU.
-
3. Enterosorbent - Enterosgel (20 g per 100 mg of water 1 hour before meals)
On the night of day 7, the patient’s condition worsened, the glucose level increased to 27.9 mmol/l, acetone in the urine - 824 mg/l +++, which was accompanied by repeated vomiting, tonic cramps of the calf muscles and numbness of the upper extremities, which indicated the development sensory diabetic neuropathy. The patient was transferred to the intensive care unit. Treatment prescribed:
-
1. NaCL solution 0.9% IV drip 70 drops/min, 400 ml, 1 time per day.
-
2. Insulin therapy: in / in 25 units of Actrapid using a dispenser with interval administration; subcutaneously prolonged insulin 20 IU Protafana HM and Actrapid 24 IU.
-
3. Vitamins of group B: B6, B2 - 2 mg 1 time per day, B3 - 15 mg 2 times a day in tablets, milgamma -2 ml (50 mg) intramuscularly once.
By day 11, the patient’s condition stabilized, blood glucose level was 14.8 mmol/l, acetone in urine was 186 mg/l+. The patient was transferred to the endocrinology department and made adjustments in the treatment:
-
1. NaCL solution 0.9% IV drip 65 drops/min, 200 ml, 1 time per day
-
2. Insulin therapy: in / in 10 units of Actrapid using a dispenser with interval administration; subcutaneously prolonged insulin 42 IU Protafana HM and Ac-trapid 24 IU; additionally short insulin Actrapid 12 IU per day for 4 injections, subject to preliminary control of blood glucose.
Within four days, the level of glucose in the blood ranged from 14.8 mmol/l to 20 mmol/l. There were no 212 | Cardiometry | Issue 24. November 2022
cramps in the calf muscles and numbness of the upper extremities.
On day 15, the patient’s condition worsened, the blood glucose level increased to 28.7 mmol/l, tonic cramps of the calf muscles were noted. The patient was urgently transferred to the intensive care unit. The medical consultation stated that the patient was tolerant to the administered insulin. It was decided to transfer the patient to another insulin in order to improve his condition. Instead of Actrapid and Protafan HM, NovoRapid and Levemir were proposed. The following treatment was prescribed:
-
1. NaCL solution 0.9% IV drip 60 drops / min, 600 ml, 2 times a day, at 10:00 in the morning and at 19:00 in the evening.
-
2. Insulin therapy: IV NovoRapid 20 IU using a dispenser with interval administration; subcutaneous insulin NovoRapid at a dosage of 36 units per day and Levemir 30 units per day.
-
3. Ringer-Lock solution 400 ml for 4 hours intravenously (60 drops / min), 10 ml / kg 2 times a day, in the morning - 400 ml, in the evening - 200 ml.
-
4. THROMBO ASS 100 mg/kg tablets, once a day.
-
5. Vitamins Doppelhertz 1 tablet a day 15 minutes before meals.
-
6. Diet number 9.
A day later, the patient was transferred to the endocrinology department and the treatment was supplemented:
Against the background of the prescribed treatment for the next two months, the patient’s condition was stable, there were no strong jumps in blood glucose levels, it ranged from 15 to 20 mmol/l, acetone in the urine ranged from 56 to 432 mg/l (+ and ++). For prevention, the patient was added to the treatment:
-
1. Intravenous (IV) injectionof Berlition 600 IU of action in 24 mg ampoules diluted with NaCL 0.9% at 200 mg, 60 drops per minute, for 10 days.
-
2. Enterosorbent Enterosgel (20 g per 100 mg of water 1 hour before meals).
Since the glucose level did not fall below 15 mmol/l, which indicated an inappropriate type of insulin, a decision was made to change the type of insulin. It was appointed:
-
1. Subcutaneous insulin NovoMix at a dosage of 46 IU per day.
-
2. Geninsulin R at a dosage of 18 units per day.
At the end of the 2nd month additionally appointed:
-
1. Neurolepon 600 mg in 20 ml ampoules diluted with NaCL 0.9% IV drip (60 drops/min) at 200 mg for 10 days.
-
2. Actavigin 40 mg/ml, IV.
-
3. Kombilipen 2 ml, 2 times a day, intramuscular injection.
The third, fourth and fifth months were without any significant changes during treatment, but blood glucose remained in the range of 15.5-21 mmol/l.
At the end of the 5th month, the patient began to complain of worsening vision in the left eye. Ophthalmologists diagnosed retinopathy with maculopathy. At the same time, the patient in the right inguinal region was found to have an enlarged lymph node measuring 2.9 cm, in the left - 1.3 cm. A biopsy study was prescribed.
In the first week of the 6th month, the patient underwent a biopsy of the inguinal lymph nodes. Histological examination revealed the presence of Berezovsky-Sternberg cells, proliferation of lymphoid tissue with an increase in plasma cells, fibroblasts, eosinophilic and neutrophilic leukocytes, resembling granulation tissue. According to the results of the clinical picture and biopsy, the diagnosis was made, Hodgkin’s disease, unspecified (ICD-10 C81.9). Lymphadenectomy carried out. On the background of surgery, the level of glucose in the blood rose to 30 mmol/l, and acetone in the urine became sharply positive (1600 mg / l), ketone bodies in the blood were determined at the level of 713 mg%. This led to the development of a hyperglycemic coma lasting five days. At the same time, sensory polyneuropathy develops. There was a sharp increase in blood pressure up to 180/110 mm Hg. The level of glucose in the blood rose to the critical figures of 54.9 mmol/l. The morning dawn syndrome was revealed, which was confirmed by the testosterone level, which exceeded the norm by 24 times. Based on these clinical indicators, an emergency medical commission suggested that the patient clinically manifested MODY 2 on the background of type I diabetes mellitus during puberty. With this in mind, the treatment was adjusted.
The patient’s blood was sent for molecular genetic testing for diabetes typing. Within a few weeks, the result was obtained: two types of the diabetes genetic code were found in the patient’s genotype: DR I and MODY 2. With additional targeted clarification of the anamnesis, hereditary burden for different types of diabetes melli-tus, including MODY (Figure 1), was established.
After resuscitation, the patient underwent insulin replacement with Humulin R (short-acting) and Hu-
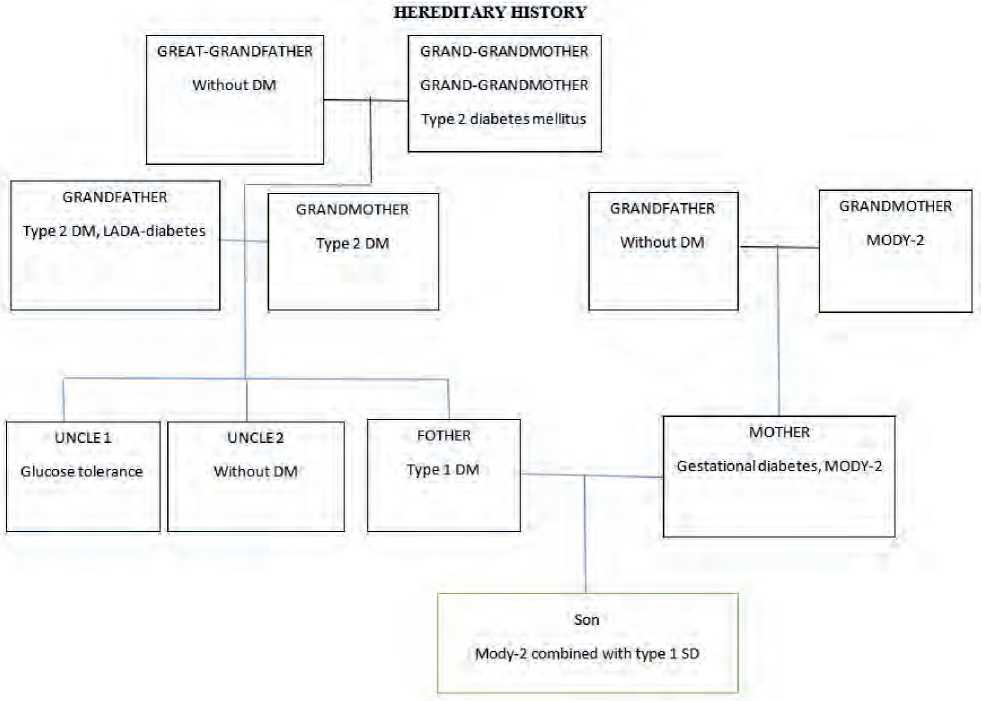
Figure 1. Family tree of patient X, 14 years old
mulin NPH (long-acting) to correct complicated type I diabetes mellitus MODY 2:
-
1. Insulin Humulin-R 36 IU per day.
-
2. Humulin-NPH 52 IU per day.
Against the background of adjusted insulin therapy, the patient showed a stable improvement in his condition, a decrease in the level of glucose in the blood, ketone bodies, glucose in the urine, and the disappearance of neurological symptoms.
Stabilization of the patient’s condition with the normalization of all parameters continued until the end of the 8th month.
At the beginning of the 9th month, against the background of insufficient intake of carbohydrate food, the blood glucose level dropped to 2 mmol/l, which led to the development of hypoglycemic coma, and the level of acetone in the urine at that moment was ++ (400 mg/l), which is not typical for this coma. The patient was brought out of this pathological condition quickly, by parenteral administration of glucose. For another month, the patient was in the hospital under observation to monitor the effectiveness and tolerability of the prescribed treatment. The outcome of this clinical case was favorable.
The patient was discharged with a diagnosis of:
MODY 2 combined with insulin-dependent diabetes mellitus with multiple complications in the compensation stage. Diabetic retinopathy, maculopathy, polyneuropathy (sensory form). Hodgkin’s disease, unspecified.
Blood glucose 6.3 mmol/l, glycated hemoglobin 7.9%, C-peptide = 0.02 ng/ml, acetone in urine 150 mg/l.
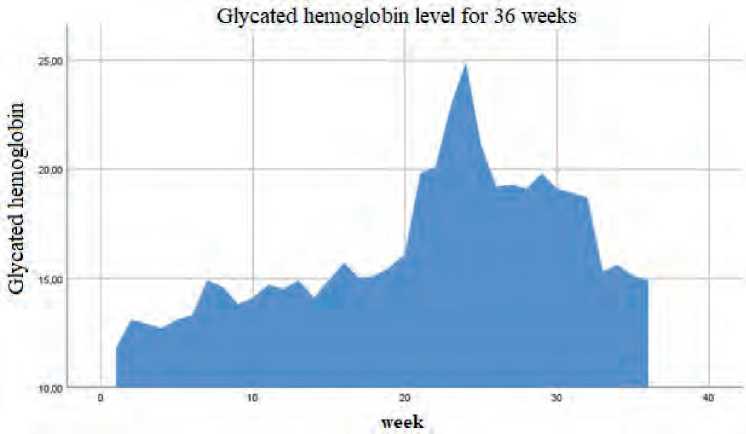
Figure 2. Glycated hemoglobin for 36 weeks in a patient with a combination of MODY-2 and DM 1
Ketone bodies in the blood for 36 week
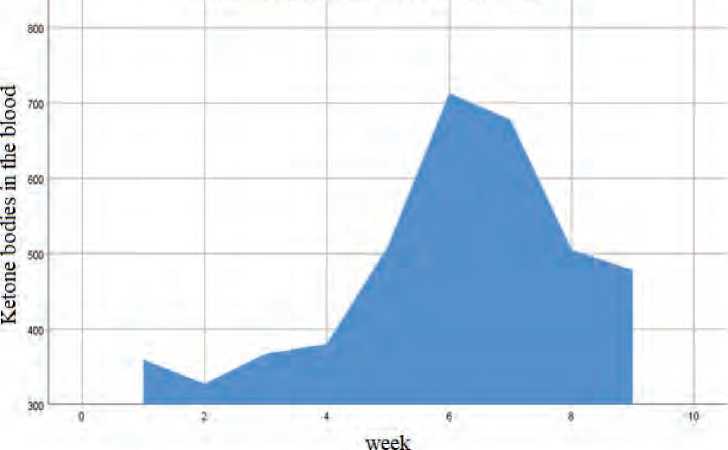
Figure 3. Ketone bodies in the blood for 36 weeks in a patient in combination with MODY-2 and DM 1
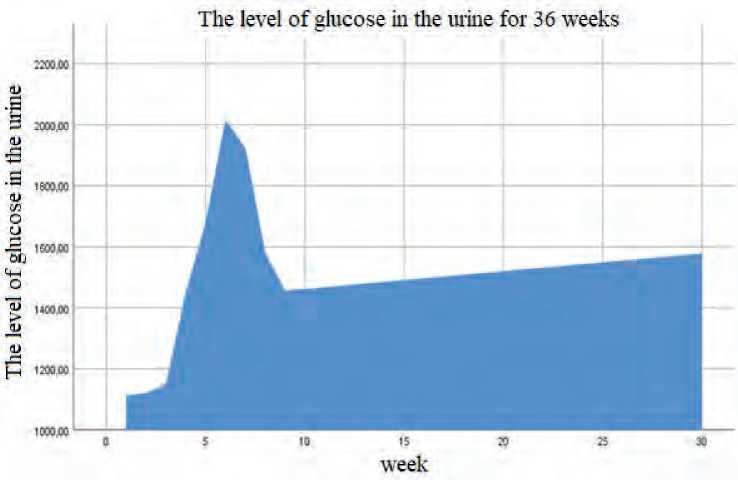
Figure 4. The level of glucose in the urine (glucosuria) for 36 weeks in a patient with a combination of MODY-2 and DM 1.
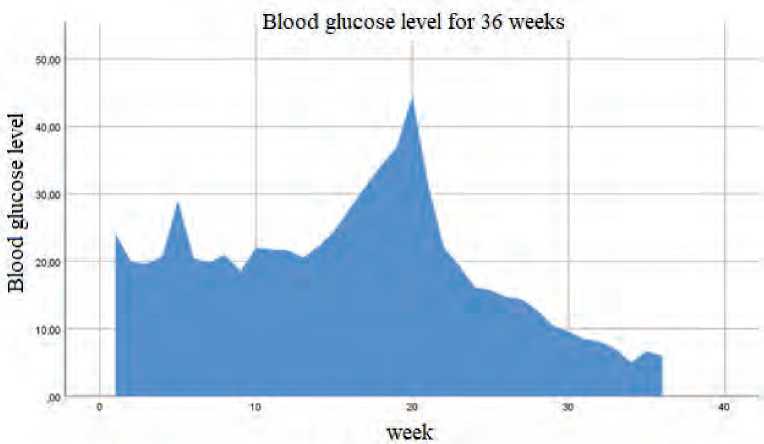
Figure 5. Blood glucose level for 36 weeks in a patient with a combination of MODY-2 and DM 1
Results and Discussion
Type I diabetes becomes severe in combination with MODY 2. In adolescence, an increase in glycemia in patients with combined MODY 2 is often regarded as a typical exacerbation of DM I and standard insulin therapy is prescribed, which does not give a positive effect. It is this situation of late diagnosis of MODY 2 that is described in the presented clinical case, when the course of DM I against the background of changes in hormonal levels in the puberty period and a decrease in the effectiveness of endogenous insulin action is aggravated by MODY 2. In addition, diabetes mellitus often affects target organs, causing the development of acute and chronic complications. In the proposed clinical case, the complications recorded in the registry [1] as the most common were noted, such as diabetic polyneuropathy, retinopathy, hypertension. The specificity of the course of diabetes mellitus, especially when several types are combined, requires molecular genetic diagnostics to verify the diagnosis and clarify the MODY subtype, followed by the choice of treatment tactics and reducing the risk of complications [1, 15, 16].
Conclusions
Any clinical case of type I diabetes mellitus in children and adolescents should be considered individually, taking into account the variety of clinical manifestations and the possibility of combination with diabetes associated with a GCK gene mutation. The presented clinical case clearly indicates the need for mandatory implementation of molecular genetic testing in children and adolescents to verify differential diagnostic criteria.
Compliance with ethical standards: voluntary informed consent for treatment and processing of personal data was obtained from the patient’s legal representatives.
Funding
None
Acknowledgements
We would like to express our gratitude to the Director of the Tambov State University named after G.R. Derzhavin, Mr. Voronin Nikita Igorevich, for assistance in research work and support at all stages of publication.
Список литературы Combination of type I diabetes mellitus and diabetes associated with GCK gene mutation: features of the clinical course in puberty
- Dedov II, et al. Diabetes mellitus in the Russian Federation: prevalence, morbidity, mortality, parameters of carbohydrate metabolism and the structure of hypoglycemic therapy according to the Federal DM Registry, status 2017. Diabetes mellitus. 2018; 21(3): 144-159. [in Russian]
- Sultanaliva RB, et al. Epidemiological aspects of diabetes mellitus in Kyrgyzstan. Bulletin of KRSU. 2016; vol. 16 (11): 140-144.
- Sharofova MU, Sagdieva ShS, Yusufi SD. Diabetes mellitus: current state of the art. Avicenna Bulletin. 2019; 1:502-12. [in Russian]
- Brunerova L, et al. Use of oral antidiabetic drugs in the treatment of Maturity-Onset Diabetes of the Young (MODY): a minireview. Diabetes Metab Res Rev. 2018; 34(1):2940.
- Urbanová J, Brunerová L, Brož J (2018) Hidden MODY – looking for a Needle in a Haystack. Front Endocrinol (Lausanne). 2018; 9:355.
- Ken Munene Nkonge, Dennis Karani Nkonge, Teresa Njeri Nkonge The epidemiology, molecular pathogenesis, diagnosis, and treatment of maturity- onset diabetes of the young (MODY) Clin Diabetes Endocrinol. 2020 Nov 4; 6(1):20.
- Kuraeva TL, et al. Molecular genetic and clinical variants of MODY2 and MODY3 in children in Russia. Problems of endocrinology. 2015; 5:14-25. [in Russian]
- Cherkasova YuB, et al. The combination of type I diabetes mellitus and diabetes associated with a mutation in the GCK gene. Issues of history. 2022; 8-2:280-7. EDN AENSBB. [in Russian]
- Zubkova NA, et al. Clinical and molecular genetic characteristics of MODY1-3 cases in the Russian Federation identified by NGS results. Problems of endocrinology. 2017; 63(6): 369-78. [in Russian]
- Ovsyannikova AK, et al. MODY in Siberia - molecular genetics and clinical manifestations. Diabetes. 2017; 20(1): 5-12. [in Russian]
- Kononenko IV, et al. Difficulties in diagnosing diabetes mellitus type MODY2 in adults. Diabetes. 2019; 22(4): 384-91. [in Russian]
- Kitao N, et al. The role of glucokinase and insulin receptor substrate-2 in the proliferation of pancreatic beta cells induced by short-term high-fat diet feeding in mice. Metabolism. 2018; 85: 48-58. [in Russian]
- Jun Shirakawa, Yasuo Terauchi. Newer perspective on the coupling between glucose-mediated signaling and β-cell functionality. Endocr J. 2020; Jan 28; 67(1):1-8.
- Vella A, et al. Targeting hepatic glucokinase to treat diabetes with TTP399, a hepatoselective glucokinase activator. Science translational medicine. 2019; 11(475): eaau3441. [in Russian]
- Carlsson A, et al. Absence of islet autoantibodies and modestly raised glucose values at diabetes diagnosis should lead to testing for MODY: lessons from a 5-year pediatric Swedish National Cohort Study. Diabetes Care.2020; 43(1): 82–89. [in Russian]
- Steele AM, et al. Prevalence of vascular complications among patients with glucokinase mutations and prolonged, mild hyperglycemia. JAMA. 2014; 311(3): 279-286. [in Russian]
- Voevoda MI, et al. Molekuljarnaja genetika MODY. Terapevticheskij arhiv. 2016; 88(4): 117-124. [in Russian]


