Depression: a predictor of coronary heart disease in Saudi Arabia
Автор: Alshahrani S., Korairi H., Sharifi A.Y., Alqahtani M.A.M., Qahtani S.a.Al., Ahamed K.M.A., Kaabi A., Alzahrani O.M., Abouelyazid A.Y.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 22, 2022 года.
Бесплатный доступ
Aims and Objectives: This research study mainly deals to evaluate the effect of depression in coronary heart disease patients. Background: Depression is one of the common comorbidity among patients presented with acute coronary syndrome or those with major cardiovascular event. Depression has been independently associated or lead to acute cardiac events in patients. Method: The study was conducted from three months followed-up patients with recent diagnosed coronary heart disease and they getting treatment from cardiac centres “Armed Forces Hospitals. Depression was evaluated by using 17-item Hamilton Rating Scale and the cardiac outcome was assessed clinically by echo parameters and cardiac biomarkers such as C-reactive Protein. The data were analysis by SPSS version 23. Results: In this study 83 patients were part of this research. The patients had been picked up from range 18-65 year in which mostly patients were male (75%) than female (25%). Among 83 coronary heart disease patients 29.5% were suffering from depression while 19.5% were on severity. The deterioration factor was significantly influence by depression and smoking. Conclusion: Depression has a great impact on deterioration of the cardiac outcomes. It can serve as a predictive variable for future cardiological morbidity and mortality.
Hamilton depression rating scale, coronary disease
Короткий адрес: https://sciup.org/148324588
IDR: 148324588 | DOI: 10.18137/cardiometry.2022.22.147153
Текст научной статьи Depression: a predictor of coronary heart disease in Saudi Arabia
The term “depression” can refer to anything from a passing feeling of sadness to serious clinical or mental manifestations that can be mild to severe, recurring, and cause disability. Depression is a prevalent illness that affects over million people globally [1]. It is a condition that is interconnected with physical health such as coronary heart disease (CHD). It is reported that depression show about 3 times more regular pattern in patients suffering from an acute myocardial infarction (AMI) than in the general population [2]. Hu Y 2020 reported that myocardial infarction patients admitted to hospital after their treatment some behavioural changes lead to major depression symptoms [3]. Furthermore, CHD young women patients suffer more with depression followed by AMI condition [6]. Literature showed that the severe emotional activity was observed in first four months of their cardiac arrest patients. Furthermore, with the aid of Hospital Anxiety and Depression Scale (HADS), 7.3% of post-AMI patients showed moderate to severe depression at the three-month mark [20]. Similarly, Mavrides 2022 reported that 17-47 % depression were observed in CVD patients during his research work [4]. Women have high prevalence rate of depression after menopause as compare to general population [5]. Poor prognosis in CHD patients enhance the grade of depression [7]. Additionally, Depression is also reported after MI, it is nearly increased the risk of cardiac attack [8]. The link between depression and CHD can be explained by both biological and behavioural mechanisms. Depressed CHD patients when compared to normal individuals found to frequently prone to cardiac events or that induce atherosclerosis. Several studies have reported that lower heart rate variability [8, 9], hypothalamic-pituitary-adrenal axis impairment [10], increased platelet activation [11], impaired vascular function [12], and an increased inflammatory response [13]. Additionally, due to the pathophysiological effect on the heart, depression is associated with poor medication adherence and triples the risk of noncompliance with medical treatment regimens due to the pathophysiological impact on the heart [14]. It has been noted that depression can reduce the likelihood of modifications of other cardiac predictors and rehabilitation. [15, 16] It is also related to greater associated costs, healthcare service utilisation [17] and reduced life quality [18]. Many studies have reported that individuals with CHD are likely to suffer from mood changes resulting in depression [19]. The exact pathophysiology linking depression to enhanced CHD risk are highly complicated, and remain unknown. However, traditional risk factors and life style may contribute in this context. Therefore, the aim of this study is to evaluate the prevalence of depression among CHD patients reported to our centre and its correlation with associated factors.
Methods
In this descriptive prospective study, patients with coronary artery disease were referred to Armed Forces Hospitals in the Southern Region from 2019 to 2020. This was a two-phase study conducted among coronary heart disease patients aged between 18-65 years, not previously diagnosed with depression or any psychiatric complaints. Written consent was obtained from all the patients before participation in the study. The exclusion criteria were patients aged <18 years, those who did not attend the cardiac clinic for follow up for three consecutive months, those with the history of psychological disorders and patients who refused to participate. The sample size was calculated using the EpiCalc 2000 program for sample size calculation with a power of 80% and a CI of 95%. Assuming that the prevalence of CHD was 5.5% based on Al-Baghli NA et al. study, the minimum sample was 73 and was raised to 83 over the three months [21]. Depression was assessed by one of the most extensively used clinician-administered depression evaluation tools namely, the 17-item Hamilton Rating Scale for Depression (HAM-D). This version is compatible for 17 items (HDRS17) to analysed the symptoms of depression in a week. Although the scale based on computation of questionnaire related to clinical interview with semi-structured guideline also emphasizing on emotional and physical symptoms of depression [22]. Cardiac outcomes were assessed clinically by echocardiography and biochemical analysis of cardiac biomarkers.
STATISTICAL ANALYSIS: The data obtained was computerized and statistically analysed using SPSS v23. Descriptive tests were used to describe and mea- sure the frequency and percentage of each variable. Comparative analysis was performed to measure the difference between the prevalence of depression and statistical differences between the groups. An independent t-test was used for the comparison of Socio-demographic study group while the chi-square was used for depression. Normality test (Kolmogorov-Smirnov and Shapiro-Wilk) was performed with Wilcoxon signed-rank test. Binary logistic regression was used to determine the most predictable variables (diabetes and smoking) for cardiac improvement. The considered significant value of was P0.05.
Results
The data set was designed on the bases of age of patients ranging from 18 to 65 years. It was observed that male’s participants are most prevalent than females. Most of the participants were literate, married and retired. It was also observed that 50 patients were currently not working or retired. Among the 20 working participants, most had a sufficient income. It is found from results that majority of patients were non-smokers (Figure 1). The mean Body mass index (BMI) of patients was found to be 29.33±3.67 that falls in normal weight category. The Binary logistic regression test was performed to analysed the difference between BMI and depression and smoking in male and female. It was observed that depression was the single most predictable variable as it can exhibit 0.24 times more likely to cause CHD. Other variables related to the outcome could be smoking and gender Figure 2. The depression status of CHD patients was assessed and presented in grade of depression scale. It was observed that the prevalence of depression among CHD patients was 27.7%. The grades of depression showed that most of the CHD patients were depressed as compared to moderately and severely depressed. The mean Hamilton score was found to be 6.02±8.4, with minimum range of 0 to maximum of 28 (Table 1, Figure 3). The cardiac outcome of studied group was analysed in the second phase of study and indicated in It was observed that after a follow-up period, of three months, 39.8% of patients were deteriorated based on their echo parameters and cardiac biomarkers. It was observed that age of deteriorated patients was significantly higher as compared to improved patients (p=0.002). Moreover, the Hamilton score for deteriorated patients were significantly higher compared to improve one (p<0.001). Chi square test was used to analysed the association of depression
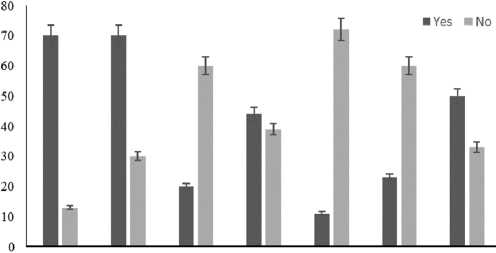
Table 1
The depression status of CHD patients was assessed and presented in grade of depression scale
|
Grade of depression |
GROUP STUDY |
HDRS score |
|
|
n |
% |
||
|
Normal |
60 |
72.30% |
8- 12 |
|
Moderate |
9 |
10.80% |
13-17 |
|
Sever |
3 |
3.70% |
18-29 |
|
Acute |
11 |
13.20% |
> 30 |
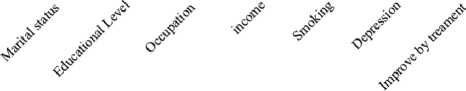
Figure.1: The sociodemographic characteristics of the studied group are represented in mean+ SD the survey based under the yes and no section.
status and smoker between deteriorated and improve patients. It was found that depression (p=0.003) and smoking (p=0.002) were significantly associated with deteriorated patients with the risk ratio score indicated that both variables have harmful effect on deteriorated CHD patients (RR=4.3, RR=9) (Table 2).
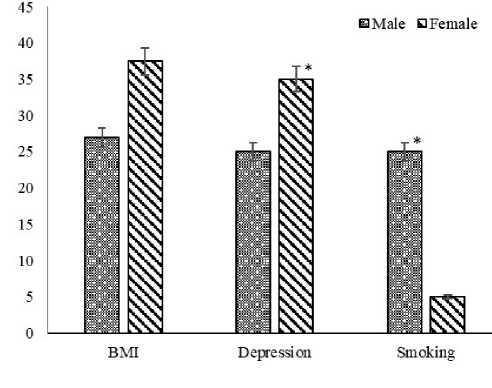
Figure2:Regression test was performed to analysed the difference between BMI and depression and smoking in male and female. The values are represented in percentage. The regression was analysed by Binary Logistic test carried out by SPSS V23.
Figure.3: The depression status of CHD patients was assessed and presented in grade of depression scale
Table 2
Cardiac outcome observed after3 months treatment of studied group
|
Cardiac outcome (after 3 weeks) |
No. |
% |
|
Deteriorate |
33 |
39.8% |
|
Improve |
50 |
60.2% |
Discussion
After a baseline assessment of the patients’ depression using the 17-item (HAM-D) scale, the population was allocated into two groups, i.e., those with depression and Normal. The cardiac functions for both groups were assessed again after the three-month follow-up period, and a comparison between both groups was conducted. Males constituted 75% of cases, and this predominance of male participants was similar to findings in most of the previous studies. Bai et al. explained that the lower rates among females may be due to the exposure to endogenous oestrogens during the fertile period of life, which delays the manifestation of atherosclerotic disease in women [23]. Thus, before menopause, the CHD event rate in women is low and is predominantly attributed to lower smoking rates. Similarly, Möller et al. [24] also reported that male had a 3 times greater CHD incidence and a 5 times higher mortality rate than female. Conversely, a study conducted in Palestine showed that symptoms of depression were more common in females (84.9%) than males (76.4%) [25]. The majority of the risk variables favoured women, however the gender gap in risk factor levels narrowed with ageing.
Smokers constituted 13.3% of the participants. Smoking is a well-established predictor for cardiovas- cular disease as It affects both coronary and peripheral circulation in a long term. This finding is consistent with those of Jalali Z et al. [26], who reported that cigarette smoke contains a large number of oxidants. It has been explained that the adverse effects of smoking may result from oxidative damage to the vascular endothelium. In long-term smokers, and even in passive smokers, endothelial dysfunction in the brachial and coronary arteries has been demonstrated.
The mean age for presentation of CHD in our sample was 58.15±14.67 years, which is in accordance with CDC that reported 27.8% of adults diagnosed with CHD aged 45-64 years felt mentally unhealthy (CDC, 2019) [3]. It is also found in a study that female CHD patients with age >60 years were also found to be an independent risk factor for 2-year depression (P 0.05). The findings of Barbera M et al., suggested that the CHD incidence and mortality increased in the 50–59 year and 60–64 year of age groups. They explained that the individuals in the respective age groups demonstrated that CHD risk increases significantly with age [27].
CHD can be a product of high BMI. I current study the mean BMI was 29.33±3.67 kg/m2. which is considered as overweight. Most of the CHD patients in studied group were obese range showed the upper limit by 37.46 kg/m2. This finding is in agreement with that of Jahangir E. et al, who explained the relationship of obesity to coronary artery disease (CAD) by the major health implications associated with obesity, including diabetes mellitus type 2, hypertension, metabolic syndrome, and dyslipidaemia, all of which are independent risk factors for CAD [28]. A study demonstrated that increase in body mass can induce the release of certain pro-inflammatory from adipose tissue that are responsible for cardiac dysfunction by causing systemic inflammation [29]. However, A UK based study reported that there was no association found between BMI and depression in CHD patients [30]. The prevalence of depression in studied CHD patients was observed to be 27.7%. This finding is close to the results of Agency for Healthcare Research and Quality systematic review. According to the review report up to 20% of CHD patients fulfil the criteria for severe depressive illness. Patients reported major depression symptoms in up to 47% of cases, and the diagnoses/ symptoms persisted long after they were discharged [3]. In 2020, Dai WS et al., reported that music therapy helpful after CAD bypass grafting in depression [31]. The outcome of CHD after the follow-up period 150 | Cardiometry | Issue 22. May 2022
revealed that almost 40% of patients with depression suffered from deteriorated health and that 60% had improved based on their cardiac parameters by echo and enzyme measurements. This finding is slightly lower than that of Willems R. et al., who reported that following their initial CHD-related admittance, 79% of people with CHD continued to go labour market with improved health [32]. The difference may be in the follow-up period; the follow-up was 3 months in our study and one year in the comparative study. We presumed that these differences may also due to the diverse culture context and the different diagnostic criteria used in the included study. However, according to NHANES III data, a history of major depression was linked with a 64% increase in the risk of having an elevated high-sensitivity C-reactive protein (hs-CRP) that may cause health deterioration [33]. More deterioration occurred among males, with a p-value of 0.057 [non-significant] and Relative Risk (RR) 2.88 [0.94: 8.8]. This finding may be explained by the occurrence of CVD and increased risk factors, especially smoking. This result is in contrast with that of Khamis RT et al. (2016), who reported that gender difference such as women have worse outcomes in chronic stable angina as well as acute coronary syndrome related to a worse co morbid outline under treatment as compared with men [34]. The difference may come from their inclusion in a different community or the research design. Education and income played no role in the outcomes and had a non-significant P-value. Smoking showed a significant difference of P=0.002 with a high RR 9 [1.8: 44.9]. This is in agreement with the findings of Lu C et al., who found a great association between smoking and a worse outcome in relation to CHD [35]. Older age showed a statistically significant association with a worse outcome due to the accumulation of risk factors. Mosley JD et al., reported the same result; that is, age is a predictable variable for a worse outcome in relation to CHD [36]. There is no doubt that among depressed individuals a variety of behavioural and lifestyle factors may have role in causing recurrent CHD. Smoking, alcohol consumption, lack of physical activity, and obesity are all on the rise [37]. Major depression, like with other medical illnesses, predicts poorer adherence to drugs [38], and rehabilitation programmes in CHD patients [39]. The Hamilton score, as an indication of depression status, showed a highly significant difference among the worsened outcomes between the groups, which is in agreement with Davidson KW, who reported in prospective observational studies that in patients with coronary heart disease, depression is linked to a very high risk of recurring acute coronary syndrome or death. They discovered that among ACS patients, the hazard ratio for all-cause death was 1.80 (95% CI= 1.46–2.51), and the hazard ratio for MI recurrence was 1.95 (95% CI= 1.33–2.85). These findings are explained by the biological mechanisms proposed to clarify the prognosis of depression-CHD [40]. The depression occurrence showed a highly significant association (P=0.003 with RR 4.3 [1.5: 12.3]) with the development of worsened CHD outcomes. This is in agreement with Rumsfeld JS et al., who report depression in patients with angina were more likely to develop cardiac problems such as recurrent infarction, ischemia, or CHF after studied their early hospitalization records [41]. No introduction of anti-depressant drugs was observed during the acute phase or follow-up period. The third objective of studying the effect of anti-depressant drugs on cardiac outcomes could not be assessed.
Learning points
This prospective study concluded that the prevalence of depression among CHD patients was 27.7%. This has a great impact on the deterioration of cardiac outcomes. The study recommends that an assessment of depression status should be mandatory among all cardiac patients, with the introduction of anti-depressant treatment in cases of depression. In order to improve a patient’s quality of life and to prevent a recurrent coronary attack, early detection and treatment of depression in heart patients is critical. Additionally, further multidisciplinary research studies involving epidemiology are needed. A longitudinal study design involving a large sample and a long follow-up period must be conducted for more accurate results for reviewing the effect of depression on cardiac outcomes.
Acknowledgements
All authors are thankful to Saudi Arabian “Armed Forces Hospitals Southern Region” along with Ministry of Health, Saudi Arabia for support towards this study. This study was equally contributed by all authors.
Ethics approval and consent to participate
The ethics approval was attained by the ethical committee of research “Armed Forces Hospitals South- ern Region, Saudi Arabia having registration number H-06-KM-001. The consent was already filled by all participants before conducting the research and their confidentiality and privacy were guaranteed. They had an option to withdraw at any time if accepted to participate, and they all signed the informed consent form.
Availability of data and materials
The author confirm that the supporting data is related to this study are available with in this article.
Competing interests
The authors have declared that they have no competing interests.
Funding
No funding was received in this account.
Список литературы Depression: a predictor of coronary heart disease in Saudi Arabia
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019 permalink/d780dffbe8a381b25e1416884959e88b
- Trajanovska AS, Kostov J, Perevska Z. Depression in survivors of acute myocardial infarction. Materia socio-medica. 2019 Jun;31(2):110.
- Hu Y, et al. Behavioral and biochemical effects of KXS on postmyocardial infarction depression. Frontiers in Pharmacology. 2020:1359.
- Mavrides N, Nemeroff CB. Treatment of affective disorders in cardiac disease. Dialogues in clinical neuroscience. 2022 Apr 1.
- Zeng LN, et al. The prevalence of depression in menopausal women in China: a meta-analysis of observational studies. Journal of affective disorders. 2019 Sep 1;256:337-43.
- Agarwala A, et al. The use of sex-specific factors in the assessment of women’s cardiovascular risk. Circulation. 2020 Feb 18;141(7):592-9.
- Khandaker GM, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Molecular psychiatry. 2020 Jul;25(7):1477-86.
- Gold SM, et al. Comorbid depression in medical diseases. Nature Reviews Disease Primers. 2020 Aug 20; 6(1):1-22.
- Doyle, F. et al. Systematic review and individual patient data meta-analysis of sex differences in depression and prognosis in persons with myocardial infarction. Psychosom. Med. (2015).77, 419–428
- Wilkowska A, Rynkiewicz A, Wdowczyk J, Landowski J. Morning and afternoon serum cortisol level in patients with post-myocardial infarction depression. Cardiology Journal. 2019;26(5):550-4.
- Vassiliou AG, Kotanidou A, Dimopoulou I, Orfanos SE. Endothelial damage in acute respiratory distress syndrome. International Journal of Molecular Sciences. 2020 Jan;21(22):8793.
- Alexopoulos GS, Bruce ML, Silbersweig D, Kalayam B, Stern E. Vascular depression: a new view of late-onset depression. Dialogues in clinical neuroscience. 2022 Apr 1..
- Müller N. The role of intercellular adhesion molecule- 1 in the pathogenesis of psychiatric disorders. Frontiers in Pharmacology. 2019:1251.
- Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, Leung J, Ravindran AV, Chen WQ, Qiao YL, Shi J. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Molecular psychiatry. 2020 Jul; 25(7): 1487-99.
- Dhar AK, Barton DA. Depression and the link with cardiovascular disease. Frontiers in psychiatry. 2016 Mar 21; 7:33.
- Glazer KM, et al. Psychological predictors of adherence and outcomes among patients in cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention. 2002 Jan 1; 22(1):40-6.
- Stein MB, et al. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population- based perspective. Psychological medicine. 2006 May; 36(5):587-96.
- Wu Y, et al. New insights into the comorbidity of coronary heart disease and depression. Current problems in cardiology. 2021 Mar 1;46(3):100413.
- Januzzi JL, et al. The influence of anxiety and depression on outcomes of patients with coronary artery disease. Archives of internal medicine. 2000 Jul 10; 160(13):1913-21.
- Dixon T, et al. Psychosocial experiences of cardiac patients in early recovery: a community‐based study. Journal of advanced nursing. 2000 Jun 1; 31(6):1368-75.
- Al-Baghli NA, et al. Awareness of cardiovascular disease in eastern Saudi Arabia. Journal of Family and Community Medicine. 2010 Jan; 17(1):15.
- Hamilton M. A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry. 1960 Feb; 23(1): 56.
- Bai MF, Wang X. Risk factors associated with coronary heart disease in women: a systematic review. Herz. 2020 Dec;45(1):52-7.
- Möller-Leimkühler AM. Gender differences in cardiovascular disease and comorbid depression. Dialogues in clinical neuroscience. 2022 Apr 1.
- Allabadi H, et al. Depression and anxiety symptoms in cardiac patients: a cross-sectional hospital-based study in a Palestinian population. BMC Public Health 19, 232 (2019). https://doi.org/10.1186/s12889-019-6561-3
- Jalali Z, Khademalhosseini M, Soltani N, Esmaeili Nadimi A. Smoking, alcohol and opioids effect on coronary microcirculation: an update overview. BMC Cardiovascular Disorders. 2021 Dec;21(1):1-7.
- Barbera M, et al. Third follow-up of the Cardiovascular Risk Factors, Aging and Dementia (CAIDE) cohort investigating determinants of cognitive, physical, and psychosocial wellbeing among the oldest old: the CAIDE85+ study protocol. BMC geriatrics. 2020 Dec; 20(1): 1-9.
- Powell-Wiley TM, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021 May 25; 143(21): e984-1010.
- IL-1 family members in the pathogenesis and treatment of metabolic disease: Focus on adipose tissue inflammation and insulin resistance. Ballak DB, Stienstra R, Tack CJ, Dinarello CA, van Diepen JA Cytokine. 2015 Oct; 75(2):280-90.
- Khandaker GM, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol Psychiatry 25, 1477–1486 (2020). https://doi.org/10.1038/s41380-019-0395-3
- Dai WS, Huang ST, Xu N, Chen Q, Cao H. The effect of music therapy on pain, anxiety and depression in patients after coronary artery bypass grafting. Journal of cardiothoracic surgery. 2020 Dec;15(1):1-5.
- Willems R, et al. Long-term healthcare utilization, medical cost, and societal cost in adult congenital heart disease. Congenital Heart Disease. 2020;15(6):399-429.
- Persons JE, Pierce GL, Fiedorowicz JG. Anxiety, C-reactive protein, and obesity in NHANES 1999–2004. Heliyon. 2019 Aug 1;5(8):e02267..
- Khamis RY, Ammari T, Mikhail GW. Gender differences in coronary heart disease. Heart. 2016 Jul 15; 102(14):1142-9.
- Lu C, Jia H, Wang Z. Association between epicardial adipose tissue and adverse outcomes in coronary heart disease patients with percutaneous coronary intervention. Bioscience reports. 2019 May 1;39(5).
- Mosley JD, et al. Predictive accuracy of a polygenic risk score compared with a clinical risk score for incident coronary heart disease. Jama. 2020 Feb 18; 323(7): 627-35.
- Stapelberg NJ, Neumann DL, Shum DH, et al. A topographical map of the causal network of mechanisms underlying the relationship between major depressive disorder and coronary heart disease. Aust N Z J Psychiatry (2011) 45:351–69.10.3109/00048674.2011.570427
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med (2005) 165:2508–13.10.1001/archinte.165.21.2508
- Brouwers RW, Houben VJ, Kraal JJ, Spee RF, Kemps HM. Predictors of cardiac rehabilitation referral, enrolment and completion after acute myocardial infarction: an exploratory study. Netherlands Heart Journal. 2021 Mar; 29(3): 151-7.
- Davidson KW. Depression and coronary heart disease. ISRN cardiology. 2012 Nov 22.
- Rumsfeld JS, et al. Depression predicts mortality and hospitalization in patients with myocardial infarction complicated by heart failure. American heart journal. 2005 Nov 1; 150(5): 961-7.


