Distal humerus fractures: closed reduction and percutaneous pinning versus open reduction and internal fixation
Автор: Gupta Pranav, Garg Shipra, Garg Keerty, Jindal Mohit
Журнал: Гений ортопедии @geniy-ortopedii
Рубрика: Оригинальные статьи
Статья в выпуске: 3 т.28, 2022 года.
Бесплатный доступ
Introduction Distal humerus fractures are relatively rare and being intra-articular are difficult to manage. As the number of elderly people grows steadily and also with increasing use of motor vehicles in the developing countries, it can be said that the frequency of intraarticular fractures of the distal humerus will increase similar to the fractures of the distal end of the radius, hip, and spine. There are several treatment plans for managing intraarticular fractures of the distal humerus depending on fracture anatomy. We conducted this study to assess which approach is superior, closed percutaneous reduction with K-wires or ORIF. Methods A total of 30 patients who satisfied the inclusion criteria were included, out of which 16 patients underwent ORIF and 14 patients underwent closed reduction and percutaneous pinning (СRPP). Patients included were between 21-50 years of age with intraarticular nonpathological closed distal humerus fractures without preoperative neurovascular deficit and presented less than 10 days between the fracture event and treatment. Results In our study, mean age of patients undergoing CRPP was 28.1 years while the mean age of patients undergoing ORIF was 30.1 years. This study showed that distal humerus fractures are more common in younger age groups. In our study, mean arc of motion at 6 months postoperatively in patients which underwent CRPP was 106.07 degrees while the mean arc of motion in patients which underwent ORIF was 80.94 degrees. In patients who underwent ORIF, only 6.2 % (1/16) had excellent outcome, 56.3 % (9/16) patients had good outcomes, 31.3 % (5/16) patients had fair outcomes, and 6.2 % (1/16) had poor outcome. It was found that out of a total of 14 patients which underwent CRPP, only 7.1 % (1/14) had cutaneous impingement. Fracture union occurred in 100 % of patients except 3 patients in ORIF group; however, they had partial union up till 6 months of follow-up. Conclusion Our study concludes that even displaced intra-articular fractures of the distal humerus can be satisfactorily treated with closed reductions and percutaneous pinning.
Closed reduction, percutaneous pinning, distal humerus, k-wires
Короткий адрес: https://sciup.org/142235327
IDR: 142235327 | УДК: 616.717.46-001.5-089.227.84 | DOI: 10.18019/1028-4427-2022-28-3-315-321
Текст научной статьи Distal humerus fractures: closed reduction and percutaneous pinning versus open reduction and internal fixation
Original article
Intercondylar fractures of the distal humerus are intraarticular comminuted fractures of the elbow joint that involve soft tissue injury [1]. These types of fractures are relatively rare and, being intraarticular, are difficult to manage [2]. They encompass 2 % of all fractures and around 30 % of all humeral injuries in adults [3–5]. As more and more people belong to the older age group and also with increasing use of motor vehicles in the developing countries, it can be said that the frequency of intraarticular fractures of the distal humerus will increase similar to the fractures of the distal end of the radius, hip, and spine [6–8].
These fractures have bimodal distribution according to age [9]. Mainly two mechanisms of fractures are seen: low-energy trauma in the older age group where there is either a direct impact on the elbow or an indirect impact resulting from a fall on the outstretched hand, and high-energy trauma in a younger patient group resulting from road traffic collisions or sport injuries [10]. Forces of these mechanisms cause the proximal end of the ulna hitting the articular part (trochlea, capitellum) of the distal humerus, no matter whether the elbow is flexed or extended at the moment of impact resulting in intra-articular distal humerus fractures [2].
There are various classification systems for these fractures. Internationally, the AO classification is most commonly used, which divides these fractures into three main groups: extra-articular, partial articular, and articular fractures. Further comminution and specific fracture patterns is defined by numbers 1–3 [11].
There are several treatment options for managing intraarticular fractures of the distal humerus depending on fracture anatomy. The goal is to start early motion at the elbow joint to avoid joint stiffness [12, 13]. Immobilization is acceptable only when fractures are non-displaced or as temporary treatment when immediate fixation is not possible [2, 13]. Non-surgical treatment can also be performed in the situations like hemiplegia sequelae that involve the ipsilateral upper limb, severe osteoporosis, fractures where there is bone loss [12] in low-demanding patients, or in patients being declared unfit for the surgical intervention, or as a short-term measure in the older age group prior to arthroplasty [13]. Other cases of non-surgical management include fractures with less soft-tissue stripping and vascular disruption, resulting in a lower likelihood of loss of bone vascularity and disturbances in growth [14]. However, functional results are typically less than optimal [12, 15]. Currently, conservative treatment has been playing only a minor role in the management of these fracture types [16].
Many surgeons recommend percutaneous Kirschner wires (K-wire) for treatment of this category of fractures in younger age group with minimal displacement [17]. The decision to use this technique depends on the skill and confidence of the surgeon in achieving the desired reduction. Some studies report the use of a percutaneous technique, even in displaced fractures, recognizing the decreased risk of iatrogenic nerve palsy, stiffness and infection with comparable functional results [18]. Requirement of another surgery is also low with this technique, as wires can be removed on outpatient basis. This treatment averts many complications by avoiding the need to open the elbow posteriorly, possibly preserving the elbow joint motion and also decreasing the chances of osteonecrosis of the distal humerus [19]. This procedure is mostly used in young children who have thick periosteum and fracture is not much displaced. However, surgeons must be prepared to open the fracture as backup if closed reduction and percutaneous pinning (CRPP) fails to achieve acceptable reduction and stability. Therefore, when taking consent for this procedure, one should inform the patient that the fracture may require being opened and fixed, if necessary. Preoperative documentation of the neurovascular status is necessary as there is always a risk of injury to the ulnar nerve. Frequency of ulnar nerve injury during pin placement from the medial side has been reported to range from 1.4 % to 15.6 % [20].
The primary goal of surgical treatment is to obtain fixation with sufficient stability so that the elbow can be mobilized immediately following surgery [21, 22]. Open fixation is currently the most preferred method as it allows requisite bone healing, early ROM exercises, and prevents future cartilage degeneration [23–25]. The available literature narrates a lateral approach for this type of fractures but their results were unsatisfactory with inability to visualize the ulnar nerve and the cases of developing flexion contractures and disturbances in growth. Therefore, most surgeons started using a posterior approach, and the present-day literature also supports this approach [26]. Currently, osteotomy of the olecranon process to visualise the articular reduction is considered “gold standard” treatment for these fractures [21, 27]. Fixation for complex fractures consist of application of precontoured locking compression plates or reconstruction plates on each column with the two plates perpendicular to each other to neutralize deforming forces, especially the rotational ones [23]. Disadvantage of ORIF is that it frequently requires another surgery for removal of implants if there is impingement [28].
Problems that may occur following surgery include loss of reduction, implant failure, nonunion, malunion, nerve involvement and elbow stiffness [29]. Complication rate in conservatively treated patients has been shown to be up to 60 % [30]. Cause for poor results may be a higher-energy accident by sustaining these fractures in adults compared with a classic elbow fracture in children.
To prevent complications, preoperative planning and additional diagnostic imaging is mandatory to know the extent of the injury using CT scans and to check bone quality [30]. Even so, fixation failure is seen in up to 7–27 % of cases [30].
Postoperatively, most surgeons advise early mobilisation within the first week post-surgery whereas others apply POP casts for several weeks to give rest to the part. Early mobilisation is believed to help patients gain more functional range of motion at the elbow and sooner than in the cases where joint is immobilized [31].
We conducted this study to assess whether percutaneous fixation with K-wires can be a better fixation method compared to ORIF wherever possible.
MATERIALS AND METHODS
This study is a prospective study comprising patients who referred to a tertiary care hospital with closed intraarticular fractures of the distal humerus. Thirty patients with an average age 29.2 years were included in the study. The inclusion criteria were:
-
1) age between 21 and 50 years;
-
2) close fractures;
-
3) intra-articular non-pathological distal humerus fractures;
-
4) no preoperative neurovascular deficit;
-
5) fewer than 10 days between the fracture event and treatment.
Exclusion criteria were:
-
1) multi-comminuted non-reconstructible distal humerus fractures with bone loss;
-
2) pathological fractures;
-
3) open fractures;
-
4) age <= 20 and > 50 years;
-
5) metabolic bone diseases;
-
6) prolonged steroid intake.
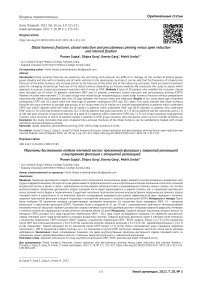
All the patients presented within three days (range, 0–3 days) after the injury. Proper history was taken at the time of admission to rule out trivial trauma. Thorough clinical examination was done, with particular emphasis on the distal neurovascular status. Serum calcium, phosphate and alkaline phosphatase and vitamin D tests were done to rule out any metabolic condition. For every patient, standard AP and lateral elbow X-rays were taken followed by CT to view a complete fracture pattern. In accordance with the AO classification, all were type C1–C2 fractures. CRPP was done in supine position while ORIF was done in lateral decubitus position. In CRPP, 2-mm K-wires with smooth-tip were used. Extended fragments were reduced with one assistant applying anterior force on the olecranon while the other person simultaneously applied longitudinal traction and flexion at the elbow. When the distal fragment was in a flexed position, a posteriorly directed force was applied to the forearm with the arm at 90 degrees of flexion. K-wires were inserted from lateral to medial direction to avoid damage to the ulnar nerve. Configuration of the pins was such that they diverge at the fracture site to improve stability. Medial to lateral pins were placed with the elbow in slight extension to avoid injury to the ulnar nerve to improve stability of reconstruction. In all the cases of CRPP, the K-wires were bent and left protruding outside the skin. Following the surgery, the elbow was immobilized in an above elbow slab. All the patients were discharged from the hospital after the first X–ray check was taken on the second post-op day. Thereafter, the patients were followed up at one week after the surgery by taking X-rays of the operated elbow to check the reduction. The second follow-up was done three weeks after the surgery to check the reduction and callus formation. The third follow-up was done at 6 weeks when the pop splints were removed and the cuff and collar slings were given to all the patients along with instructions to do gentle elbow range of motion exercises. The fourth follow-up was 12 weeks after the surgery. If a radiological evidence of bridging callus formation was seen, K-wires were removed and ROM exercises were started. At 6-month follow-up, the following clinical and radiological parameters were assessed in every patient: joint range of motion, QuickDASH score and fracture union visible on AP or lateral views. In patients who underwent CRPP, fracture union was defined as a radiological evidence of bridging callus formation, which was attained in all of our patients except one after the average time of 10 weeks (range 8–12 weeks).
In cases of ORIF, the posterior approach was used; the ulnar nerve was explored and secured and fractures were generally well reconstructed using plates on both columns. Clinical and radiological follow-up was done for all patients up to at least six month. DASH scoring was done to evaluate the outcome.
Continuous and normally distributed data were written in the form of its mean and standard deviation. Student’s T-test was used to compare the mean arc of motion and mean DASH score at 6 months postoperatively. Qualitative data were compared using the chi-square test, i.e., the number of patients undergoing CRPP and ORIF in different age group, DASH score of patients undergoing CRPP and ORIF in different age groups, cutaneous impingement experienced by patients undergoing CRPP and ORIF and number of cases having union and nonunion in those undergoing CRPP and ORIF.
Ethical Statement Ethical clearance was done vide institutional ethical committee.
RESULTS
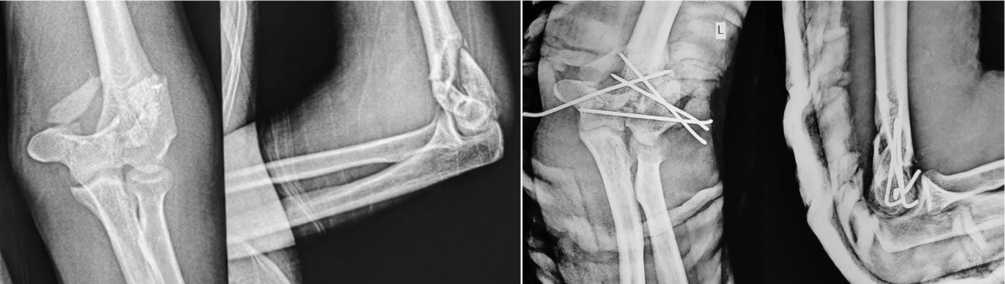
Fig. 1. Preoperative and immediate postoperative images

Fig. 2. Postoperative images at 3 months just before and after removal of K-wires
A total of 30 patients who satisfied the inclusion criteria were included, out of which 16 patients underwent ORIF and 14 patients underwent closed reduction and percutaneous pinning. The male and female patients which underwent surgery were also compared to observe sex distribution. It was not found to be statistically significant. The mean age and male to female ratio, and decade-wise distribution of patients is highlighted in Table 1.
Table 1
|
Variable |
CRPP |
ORIF |
P value |
|
Mean age |
28.1 |
30.1 |
0.47 |
|
Male |
12:2 |
12:4 |
|
|
Female |
2 |
4 |
The patients were divided into 3 groups based on their age (Table 2).
Table 2
Distribution of patients according to different age groups
|
Age Groups |
CRPP |
ORIF |
P value |
|
21-30 years |
9 |
10 |
0.9 |
|
31-40 years |
4 |
3 |
0.5 |
|
41-50 years |
1 |
3 |
0.3 |
In our study, mean age of patients undergoing CRPP was 28.1 yrs while the mean age of patients undergoing ORIF was 30.1 years. The overall sex distribution showed that such fracture is relatively more common in male population. A non–dominant extremity was involved in 22 (73 %) cases and a dominant extremity was injured in 8 (27 %) patient. Out of 30 patients, 19 patients belonged to 21–30 year age group, 7 patients belonged to 31– 40 year age group while 4 patients belonged to 41–50 year age group. This shows that this fracture pattern is more common in younger age groups. Out of 19 patients who belonged to 21 to 30- year age group, 9 patients underwent CRPP, while 10 patients underwent ORIF. In 31–40 year age group, 4 patients underwent CRPP and 3 underwent ORIF. In 41–50 year age group, 1 underwent CRPP and 4 underwent ORIF. Difference in the three groups was not found to be statistically significant (p > 0.05).
Mild elbow stiffness was seen in three (42 %) patients at 5 weeks of follow–up, which was dealt with by planning vigorous physiotherapy schedules after the K-wire removal. All patients who underwent CRPP achieved almost complete ROM at 6 months postoperatively. Patients who underwent ORIF started their ROM exercises immediately. However at 6 months, ROM achieved was less as compared to that achieved by the patients who underwent CRPP. In our study, mean arc of motion at 6 months postoperatively in CRPP patients was 106.07 degrees while the mean arc of motion in ORIF patients was 80.94 degrees (Table 3). On applying Student’s t-test, difference in the two groups was found to be statistically significant (р < 0.05).
Table 3
Distribution of patients according to mean arc of motion and mean DASH score
|
Variable |
CRPP |
ORIF |
p-value |
|
Mean arc of motion |
106.07 |
80.94 |
0.00001 |
|
Mean DASH score |
90.36 |
74.69 |
0.0001 |
Quick DASH score was assessed in all patients at 6 months postoperatively, and it was seen the DASH score was either good or excellent in most CRPP patients while the scores were mostly fair and good in ORIF patients. In patients who underwent CRPP, 42.9 % (6/14) patients had excellent outcomes, 50 % (7/14) had good outcomes while 7.1 % (1/14) patients had fair outcome, but no patient had poor outcome. In patients who underwent ORIF, only 6.2 % (1/16) patients had excellent outcomes, 56.3 % (9/16) patients had good outcomes, 31.3 % (5/16) patients had fair outcomes, and 6.2 % (1/16) had poor outcome. In comparing the DASH score of 2 groups in terms of patients with excellent outcome and patients with less favourable outcomes, the difference was statistically significant (p < 0.05) (Table 4).
Table 4
Distribution of patients according to DASH score
|
DASH SCORE |
CRPP |
ORIF |
p-value |
|
Poor |
0 |
1 |
|
|
Fair |
1 |
5 |
0.09 |
|
Good |
7 |
9 |
0.7 |
|
Excellent |
6 |
1 |
0.02 |
Another parameter evaluated was cutaneous impingement. It was found that out of a total of 14 CRPP patients only 7.1 % (1/14) had cutaneous impingement. This can be due to the fact that wires were left outside and were removed later on OPD basis. In case of ORIF, 37.5 % (6/16) had cutaneous impingement mainly due to tension band wiring of the olecranon (Table 5). By comparing the 2 groups, difference was found to be statistically significant (p < 0.05) what suggested that a significant number of
ORIF patients had cutaneous impingement compared to those who underwent CRPP.
Table 5
Distribution of patients according to presence or absence of cutaneous impingement
|
Cutaneous impingement |
CRPP |
ORIF |
|
YES |
1 |
6 |
|
NO |
13 |
10 |
A consolidated fracture union was seen at an average interval of 3 months after the surgery. Slabs were removed at 2 months, wires were removed at 3 months, and joint motion exercises were started. Fractures united in all CRPP patients; however, the time of fracture consolidation was different. In ORIF group, 18.8 % (3/16) of patients had nonunion, and all these patients had nonunion of olecranon osteotomy. Fracture union occurred in 100 % of patients, including 3 patients in ORIF category who showed partial union at 6 months of follow-up (Table 6).
Table 6
Distribution of patients according to presence or absence of union
|
Non union |
CRPP |
ORIF |
|
YES |
0 |
3 |
|
NO |
14 |
14 |
In CRPP patients, pin tract infection was seen in 7.1 % (1/14) patients and was treated successfully conservatively with daily pin-site dressing and antibiotic course. Complications like an early fixation failure, an iatrogenic neurovascular injury, deep infection and instability at the elbow joint were not seen in any of the patients who underwent CRPP. However, 2 patients who underwent ORIF had surgical site infection for which cultures were sent and appropriate antibiotics were started. Ulnar nerve was explored and preserved in all ORIF cases. However, transient ulnar neuropathy was seen in 3 cases which resolved after 6 weeks. No implant failure was seen.
DISCUSSION
Distal humerus fractures are complex because of joint involvement and comminution. These fractures are relatively rare. Therefore, there is dearth of literature to guide treatment and specific management scheme for them is not clear. Several approaches have been used to treat this type of fracture with the aim of treatment being to restore elbow joint function. The treatment strategy seems crucial. The chosen approach must allow the fracture to be reduced adequately without causing neurovascular injury and injury to other soft tissue structures as well. High-quality fixation is essential for good results. The success or failure of fracture fixation is based on patient-associated factors, the surgical procedure undertaken and the postoperative period. Fracture type is an important prognostic factor [32]. The ideal treatment for adult intra-articular fracture of the distal humerus is open reduction and internal fixation with plates and screws, to allow an early mobilization of the elbow to prevent elbow stiffness. However, the treatment options may vary, depending upon the amount of displacement of the condylar pillars, the extent of the comminution and the integrity of the articular surfaces.
In non-operative treatment, the rate of nonunion one year after injury has been as high as 47 % [33]. Therefore, conservative treatment is considered only for patients with a low activity level and patients for whom surgery would be more harmful due to comorbidities.
The study conducted by Calvert et al. showed that olecranon osteotomy is associated with a significant nonunion rate, which negatively affected the results of their study [32]. However, the study conducted by Chen et al. reported that ORIF with olecranon osteotomy, compared with triceps-sparing, resulted in better function outcomes in patients > 60 years of age. Although the olecranon osteotomy approach is commonly used, it has potential complications related to hardware prominence/ migration, displacement/nonunion of osteotomy, and triceps weakness [34].
In our study, CRPP group showed 6.2 % of nonunion (1/14) while in patients which underwent ORIF, 18.8 % (3/16) had nonunion. However, the difference in the two groups was not found to be statistically significant.
Another approach that can be tried in these types of fractures is closed reduction and percutaneous pinning. With this approach, there is no damage to the surrounding soft tissues, particularly the extensor mechanism at the elbow joint, which could lead to subsequent elbow stiffness. There is no complication which is related to bulky hardware like impingement and pain in the soft tissues and skin necrosis [18]. Elbow stiffness and nerve injury are more common after open reduction and internal fixation than with closed reduction and percutaneous pinning [35].
In our study, pin tract infection was seen in 7.1 % (1/14) of CRPP patients, who was treated successfully conservatively with daily pin-site dressing and antibiotic course. Complications like an early fixation failure, an iatrogenic neurovascular injury, deep infection and instability at the elbow joint were not seen in any of the patients who underwent CRPP. However, two patients who underwent ORIF had surgical site infection for which cultures were sent and appropriate antibiotics were started. The ulnar nerve was explored and preserved in all ORIF cases; however transient ulnar neuropathy was seen in 3 cases which resolved in 6 weeks. No implant failure was seen.
We did CRPP in 46.7 % patients (14/30). It was found that in CRPP patients, only 7.1 % (1/14) had cutaneous impingement while in case of ORIF, 37.5 % (6/16) had cutaneous impingement. On comparing the 2 groups, difference was found to be statistically significant (p < 0.05) which suggested that chances of cutaneous impingement is significantly more in patients undergoing ORIF compared to those undergoing CRPP. Cutaneous impingement in one case also resolved upon K-wires removal.
Another complication commonly seen in distal humerus fractures posteoperatively is elbow stiffness. There are very few studies which compare elbow range of motion in patients who underwent ORIF versus those who underwent CRPP. The study conducted by Re et al. showed that regardless of the approach, the biggest indicator for loss of range of motion postoperatively was the degree of preoperative articular damage [35]. The study conducted by Beck et al. showed that the duration of immobilization did not seem to affect ROM at the 1-year follow-up [31]. The study conducted by Bell et al. in 2015 also showed that closed reduction and pinning of extra-articular distal humerus fractures in adolescents resulted in predictable clinical and radiographic outcomes and allowed for earlier return of motion and fewer complications when compared with open treatment [17]. However, all of the above studies were done in the adolescent age group.
In CRPP patients, mild elbow stiffness was seen in 21.4 % (3/14) patients at 5 weeks of follow–up, which was dealt with by planning vigorous physiotherapy schedules after the K-wire removal. All patients who underwent CRPP achieved almost complete ROM at 6 postoperative months. ROM exercises were started immediately in the patients who underwent ORIF. However at 6 months, they could not achieve the ROM that was achieved by the patients who underwent CRPP. In our study, mean arc of motion at 6 months postoperatively in the patients of CRPP group was 106.07 degrees while the mean arc of motion in ORIF patients was 80.94 degrees. The application of the Student’s t-test found that the difference between the two groups was statistically significant (p < 0.05).
We also calculated mean DASH score for all patients in our study. Mean DASH score was 90.36 in CRPP patients while it was 74.69 in patients who underwent ORIF. The application of the Student’s t-test found that the difference between the two groups was statistically significant (p = 0.0001) thus showing that function of the elbow is preserved more with the closed procedure rather than the open one.
Because of the rare incidence of this injury, no consensus exists on an ideal treatment option yet. Further research is needed to optimize its management and rehabilitation recommendations and to minimize complications.
CONCLUSION
Our study concludes that even displaced intra-articular fractures of the distal humerus can be satisfactorily treated with closed reduction and percutaneous pinning. Thereby, there is no need of another surgical procedure to remove the pins, because these can be removed very easily as an outdoor procedure. It decreases the risk of surgical and anaesthetic risks to the patient and it is also very cost effective. Moreover, the surgical time is much less as compared to that of the open surgical reduction of the fracture. However, this study did not allow us to paint a picture of the ideal fracture that should be treated by internal fixation or by CRPP. The major limitation of the present study was that the sample size was small indicating the need for more RCTs to further investigate what might be the optimal method(s) for treating this type of fracture. In addition, heterogeneity existed across the studies with respect to the type of fracture, the criteria used to evaluate the severity of the fracture, and the assessment tool used to evaluate joint function following surgery.
Список литературы Distal humerus fractures: closed reduction and percutaneous pinning versus open reduction and internal fixation
- Sanchez-Sotelo J., Torchia M.E., O'Driscoll S.W. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique // I. Bone Joint Surg. Am. 2007. Vol. 89, No 5. P. 961-969. DOI: 10.2106/JBJS.E.01311.
- Begue T. Articular fractures of the distal humerus // Orthop. Traumatol. Surg. Res. 2014. Vol. 100, No 1 Suppl. P. S55-S63. DOI: 10.1016/j. otsr.2013.11.002.
- Epidemiologic features of humeral fractures / S.H. Rose, L.J. Melton 3rd, B.F. Morrey, D.M. Ilstrup, B.L. Riggs // Clin. Orthop. Relat. Res. 1982. No 168. P. 24-30.
- Anglen J. Distal humerus fractures // J. Am. Acad. Orthop. Surg. 2005. Vol. 13, No 5. P. 291-297. DOI: 10.5435/00124635-200509000-00001.
- Jupiter J.B., Mehne D.K. Fractures of the distal humerus // Orthopedics. 1992. Vol. 15, No 7. P. 825-833. DOI: 10.3928/0147-7447-19920701-07.
- Osteoporotic fractures of the distal humerus in elderly women / M. Palvanen, S. Niemi, J. Parkkari, P. Kannus // Ann. Intern. Med. 2003. Vol. 139, No 3. P. W-W61. DOI: 10.7326/0003-4819-139-3-200308050-00021-w2.
- Secular trends in the osteoporotic fractures of the distal humerus in elderly women / M. Palvanen, P. Kannus, S. Niemi, J. Parkkari // Eur. J. Epidemiol. 1998. Vol. 14, No 2. P. 159-164. DOI: 10.1023/a:1007496318884.
- Why is the age-standardized incidence of low-trauma fractures rising in many elderly populations? / P. Kannus, S. Niemi, J. Parkkari, M. Palvanen, A. Heinonen, H. Sievänen, T. Järvinen, K. Khan, M. Järvinen // J. Bone Miner Res. 2002. Vol. 17, No 8. P. 1363-1367. DOI: 10.1359/ jbmr.2002.17.8.1363.
- Adult distal humeral metaphyseal fractures: epidemiology and results of treatment / C.M. Robinson, R.M. Hill, N. Jacobs, G. Dall, C.M. Court-Brown // J. Orthop. Trauma. 2003. Vol. 17, No 1. P. 38-47. DOI: 10.1097/00005131-200301000-00006.
- Egol K.A., Koval K.J., Zuckerman J.D. Handbook of Fractures. 4th Ed. Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo: Lippincott Williams & Wilkins. 2010. 812 p.
- Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification // J. Orthop. Trauma. 1996. Vol. 10, No Suppl. 1, v-ix. P. 1-154.
- Miller A.N., Beingessner D.M. Intra-articular distal humerus fractures // Orthop. Clin. North Am. 2013. Vol. 44, No 1. P. 35-45. DOI: 10.1016/j. ocl.2012.08.010.
- Hausman M., Panozzo A. Treatment of distal humerus fractures in the elderly // Clin. Orthop. Relat. Res. 2004. No 425. P. 55-63. DOI: 10.1097/01. blo.0000131485.47685.8c.
- Mok C.Y., Lui T.H. T-condylar fractures of the distal humerus in children: report on three cases // BMJ Case Rep. 2013. Vol. 2013. bcr2013009685. DOI: 10.1136/bcr-2013-009685.
- Triangular fixation technique for bicolumn restoration in treatment of distal humerus intercondylar fracture / S.W. Jung, S.H. Kang, M. Jeong, H.S. Lim // Clin. Orthop. Surg. 2016. Vol. 8, No1. P. 9-18. DOI: 10.4055/cios.2016.8.1.9.
- Geddes J.R. The Cochrane database of systematic reviews // Journal of Psychosomatic Research. 1996. Vol. 40. P. 438-439. DOI: 10.1016/S0022-3999(96)90063-X.
- Adolescent distal humerus fractures: ORIF versus CRPP / P. Bell, B.P. Scannell, B.J. Loeffler, B.K. Brighton, R.G. Gaston, V. Casey, M.E. Peters, S. Frick, L. Cannada, K.L. Vanderhave // J. Pediatr. Orthop. 2015. Vol. 37, No 8. P. 511-520. DOI: 10.1097/BPO.0000000000000715.
- Closed reductions and percutaneus "k" wire fixation for adolescent intercondylar fractures of the distal humerus / Julfiqar, A. Pant, N. Huda, W. Ahmed // J. Clin. Diagn. Res. 2013. Vol. 7, No 8. P. 1666-1668. DOI: 10.7860/JCDR/2013/5695.3227.
- Fractures of the lateral condyle of the humerus in children / J.A. Hardacre, S.H. Nahigian, A.I. Froimson, J.E. Brown // J. Bone Joint Surg. Am. 1971. Vol. 53, No 6. P. 1083-1095.
- A comparative study of two percutaneous pinning techniques (lateral vs medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus / K. Prashant, D. Lakhotia, T.D. Bhattacharyya, A.K. Mahanta, A. Ravoof // J. Orthop. Traumatol. 2016. Vol. 17, No 3. Р. 223-229. DOI: 10.1007/s10195-016-0410-2.
- Beghin J.L., Bucholz R.W., Wenger D.R. Intercondylar fractures of the humerus in young children. A report of two cases // J. Bone Joint Surg. Am. 1982. Vol. 64, No 7. P. 1083-1087.
- Dreyfuss D., Eidelman M. Treatment of complex intercondylar humeral fractures in adolescents by open reduction and internal fixation through the transolecranon approach // J. Pediatr. Orthop. B. 2014. Vol. 23, No. 4. P. 364-368. DOI: 10.1097/BPB.0000000000000048.
- Is ulnar nerve transposition beneficial during open reduction internal fixation of distal humerus fractures? / R.C. Chen, D.J. Harris, S. Leduc, J.J Borrelli Jr., P. Tornetta 3rd, W.M. Ricci // J. Orthop. Trauma. 2010. Vol. 24, No 7. P. 391-394. DOI: 10.1097/BOT.0b013e3181c99246.
- Incidence, management, and prognosis of early ulnar nerve dysfunction in type C fractures of distal humerus / H.J. Ruan, J.J. Liu, C.Y. Fan, J. Jiang, B.F. Zeng // J. Trauma. 2009. Vol. 67, No 6. P. 1397-1401. DOI: 10.1097/TA.0b013e3181968176.
- Intraarticular distal humerus fractures. Factors affecting functional outcome / K. Kundel, W. Braun, J. Wieberneit, A. Ruter // Clin. Orthop. Relat. Res. 1996. No 332. Р. 200-208.
- Pediatric T-Condylar Humerus Fractures: A Systematic Review / J.B. Anari, A.L. Neuwirth, N.M. Carducci, D.J. Donegan, K.D. Baldwin // J. Pediatr. Orthop. 2017. Vol. 37, No 1. P. 36-40. DOI: 10.1097/BPO.0000000000000588.
- Re P.R., Waters P.M., Hresko T. T-condylar fractures of the distal humerus in children and adolescents // J. Pediatr. Orthop. 1999. Vol. 19, No 3. P. 313-318.
- Outcomes after surgical treatment of adolescent intraarticular distal humerus fractures / J.B. Cook, AI. Riccio, T. Anderson, W. Chen, S.H. Shaha, R.L. Wimberly // J. Pediatr. Orthop. 2016. Vol. 36, No 8. P. 773-779. DOI: 10.1097/BPO.0000000000000555.
- Osteosynthesis of intercondylar humerus fracture using Bryan and Morrey approach / S. Lakhey, S. Sharma, R.L. Pradhan, R.R. Manandhar, K.P. Rijal // Kathmandu Univ. Med. J. (KUMJ). 2010. Vol. 8, No 30. P. 154-157. DOI: 10.3126/kumj.v8i2.3549.
- Amir S., Jannis S., Daniel R. Distal humerus fractures: a review of current therapy concepts // Curr. Rev. Musculoskelet. Med. 2016. Vol. 9, No 2. P. 199-206. DOI: 10.1007/s12178-016-9341-z.
- T-condylar fractures of the distal humerus in children: does early motion affect final range of motion? / N.A. Beck, T.J. Ganley, S. McKay, L. Tomlinson, J. Ahn, J.M. Flynn, K. Baldwin // J. Child. Orthop. 2014. Vol. 8, No 2. P. 161-165. DOI: 10.1007/s11832-014-0576-1.
- Outcomes of distal humerus fractures in patients above 65 years of age treated by plate fixation / P. Clavert, G. Ducrot, F. Sirveaux, T. Fabre, P. Mansat; SOFCOT // Orthop. Traumatol. Surg. Res. 2013. Vol. 99, No 7. P. 771-777. DOI: 10.1016/j.otsr.2013.08.001.
- Aitken S.A., Jenkins P.J., Rymaszewski L. Revisiting the 'bag of bones': functional outcome after the conservative management of a fracture of the distal humerus // Bone Joint J. 2015. Vol. 97-B, No 8. Р. 1132-1138. DOI: 10.1302/0301-620X.97B8.35410.
- Comparison of treatments in patients with distal humerus intercondylar fracture: a systematic review and meta-analysis / H. Chen, D. Li, J. Zhang, X. Xiong // Ann. Med. 2017. Vol. 49, No 7. P. 613-625. DOI: 10.1080/07853890.2017.1335429.
- Popkin C.A., Rosenwasser K.A., Ellis Jr. H.B. Pediatric and Adolescent T-type Distal Humerus Fractures // J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2017. Vol. 1, No 8. P. e040. DOI: 10.5435/JAAOSGlobal-D-17-00040.