Effects of total table salt restriction on blood pressure
Автор: Chacon-Lozsan Francisco Jose, Peinado-Acevedo Juan Sebastian
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 6, 2015 года.
Бесплатный доступ
Aims. The aim of the study was to evaluate the effect of total omission of dietary salt intake on BP. Material and methods. The effects of total omission on the consumption of dietary salt over the BP, were evaluated for this study in a group of 30 hypertensive patients between 40-60 years old, uncontrolled, with monotherapy with angiotensin converting enzyme inhibitors or angiotensin II receptor antagonists. BP was recorded over three days at the same time, according to the guidelines of the American Heart Association for correct BP measurement in humans. The average of the three registers measurement was taken as baseline for comparison of the data. The only intervention was the total restriction of table salt and sauces with salt. The patients were followed monthly during the first five months recording BP under the same conditions that basal measurement, after this, were indicated to all the patients the consumption of salt 5g/day (provided by the researchers) and were followed for another five months in the same measurement conditions above...
Hypertension, sodium chloride, blood pressure, diet, sodium dietary
Короткий адрес: https://sciup.org/148308803
IDR: 148308803 | DOI: 10.12710/cardiometry.2015.6.96103
Текст научной статьи Effects of total table salt restriction on blood pressure
Aims The aim of the study was to evaluate the effect of total omission of dietary salt intake on BP. Material and methods The effects of total omission on the consumption of dietary salt over the BP, were evaluated for this study in a group of 30 hypertensive patients between 40-60 years old, uncontrolled, with monotherapy with angiotensin converting enzyme inhibitors or angiotensin II receptor antagonists. BP was recorded over three days at the same time, according to the guidelines of the American Heart Association for correct BP measurement in humans. The average of the three registers measurement was taken as baseline for comparison of the data. The only intervention was the total restriction of table salt and sauces with salt. The patients were followed monthly during the first five months recording BP under the same conditions that basal measurement, after this, were indicated to all the patients the consumption of salt 5g/day (provided by the researchers) and were followed for another five months in the same measurement conditions above. Results Total restriction of consumption of dietary salt caused highly significant reduction (P<0.0001) of SBP, which was progressive and was evident from the first week of follow up. In addition, caused a decrease in DBP during the first week of monitoring, but that effect was not continuous, and no significant decrease in DBP was observed during follow-up (P 0.0662) Discussion and сonclusions We recommend that a minimum restriction to 5g/day would be ideal in this population group. Keywords Hypertension • Sodium chloride • Blood pressure • Diet • Sodium dietary Imprint Francisco Jose Chacon-Lozsan, Juan Sebastian Peinado-Acevedo. Effects of total table salt restriction on blood pressure; Cardiometry; No.6; May 2015; p.96-103; doi: 10.12710/cardiometry.2015.6.96103 Available from:
The cardiovascular diseases are the main cause of death worldwide; the risk of developing cardiovascular diseases is significantly higher in patients with hypertension (HT), and getting it increases the number of adverse outcomes including mortality [1,2]. Similarly, there is a direct relationship between salt intake, elevated blood pressure and cardiovascular outcomes [3,4]. There is evidence that reducing dietary salt intake lowers blood pressure (BP), therefore, a reduction in salt intake would decrease the BP and cardiovascular risk [5,6].
As estimated for 2010, 1 in 10 cardiovascular deaths were attributable to the consumption of more than 2 g/day sodium, the majority secondary coronary heart disease and stroke; also the 40% of those deaths were recorded in people younger than 70 years [7]. HT is diagnosed more often in regions with average sodium intakes greater than 2.3g/day (100 mEq); however, it is less common in regions with an average sodium intake of less than 1.2g/day (50 mEq) [8]. For this reason various organizations worldwide including the United Nations Organization, the United States Department of Health and Human Services, the World Health Organization and Centers for Disease Control and Prevention, emphasize the reduction of daily salt consumption for all adults [9-12]. European Guidelines on cardiovascular disease prevention and management of hypertension currently recommend the restriction of salt intake of 5-6g/day, with a level of evidence and grade of recommendation 1-A, respectively [13,14].
The mechanisms that explain the relationship between salt intake and HT are unclear, it is known that not only sodium, if not also the chlorine, which is the companion anion in salt (NaCl), play an important role in the increased intravascular volume by their osmotic activity [15]. In addition, some individuals are more sensitive to salt (BP changes to salt intake), as by various mechanisms such as: the higher retention and absorption of sodium, abnormal vascular tone with endothelial damage (higher tendency to vasoconstriction and alteration in normal vasodilation), and others are still not well understood, are more likely to develop HT [16-19].
Recent studies worldwide [20-22] and meta-analysis [3] have been conducted to evaluate the effect of reduced salt intake on BP, their results support the efforts of doctors and patients to reduce sodium intake due their beneficial effects. Therefore it is important to conduct further studies in diverse populations in order to generalize and generate recommendations. The aim of the study was to evaluate the effect of total omission of dietary salt intake on BP.
Materials and methods
Patients
The effects of total omission on the consumption of dietary salt on the BP were evaluated for the study in a group of 30 hypertensive patients between 40 and 60 years old, over two years of diagnosis, uncontrolled, with monotherapy with angiotensin converting enzyme inhibitors (ACEi) or angiotensin II receptor antagonists (ARBs). The 50% were men, and the rest of the patients were women. All patients had mild exercise habits related to moderate daily work activities. No patients were included pregnant, diabetic, with neoplastic, neurological or immunological diseases. The daily consumption of salt pre-study was 15-20g (See Table 1).
Table 1. Population characteristics
|
Characteristic |
n |
% |
|
Gender |
||
|
Male |
15 |
50 |
|
Female |
15 |
50 |
|
Age |
||
|
40-50 |
13 |
43 |
|
51-60 |
17 |
57 |
|
Antihypertensive agents |
||
|
Enalapril |
12 |
40 |
|
Lisinopril |
2 |
7 |
|
Losartan |
4 |
13 |
|
Olmersatan |
12 |
40 |
|
Mean |
Std. deviation |
|
|
Baseline systolic blood pressure |
158,3 |
10,3 |
|
Baseline diastolic blood pressure |
79,6 |
9,2 |
Design
The study protocol was approved by the Ethics Committee of Centroccidental University Lisandro Alvarado. All patients got their written informed consent before entering in the study. BP was recorded over three days at the same time (15:00 hours), three hours postprandial; according to the guidelines of the American Heart Association for correct BP measurement in humans [23]. The average of the three registers measurement was taken as baseline for comparison of the data. The only intervention was the total restriction of table salt and sauces with salt. Neither other changes in the lifestyle or adjustments to the antihypertensive treatment were recorded. The patients were followed monthly during the first five months by recording BP under the same conditions that basal measurement, after that, indicated was to all the patients the consumption of salt 5g/day (provided by the researchers), and they were followed for another five months under the same measurement conditions as above.
Statistical analysis
The data were collected in EXCEL spreadsheet firsthand and processed in GraphPAD PRISM 5.0 for Windows. The data were analyzed with ANOVA, comparing each month tracking your basal previous month and the results are presented in graphs with the average +/- standard deviation taking significant difference as a value of P <0.05.
Results
Changes in systolic blood pressure (SBP)
Restriction total of consumption of dietary salt caused highly significant reduction (P <0.0001) of SBP, which was progressive and was evident from the first week of follow up. However, after the start use of the salt administered by the researchers, the SBP increased progressively during follow up to 5 months without significant statistical difference when compared with restart the fifth month of salt intake with the value of the fifth month of salt restricted without reaching its basal level of BP (see Fig. 1).
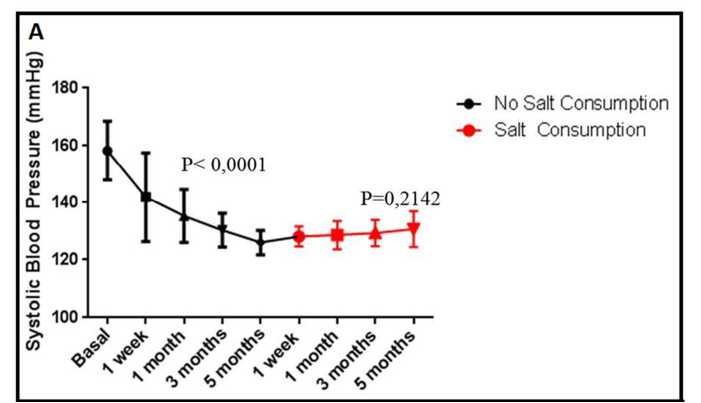
Figure 1. Effects of salt consumption on Systolic Blood Pressure
Changes in diastolic blood pressure (DBP)
Restriction total of consumption of dietary salt caused a decrease in DBP during the first week of monitoring, but this effect was not continuous and no significant decrease in DBP was observed during follow-up (P 0.0662), after the first use of the salt administered by the researchers, the DBP was increased up to similar to the baseline measurement values (Fig 2).
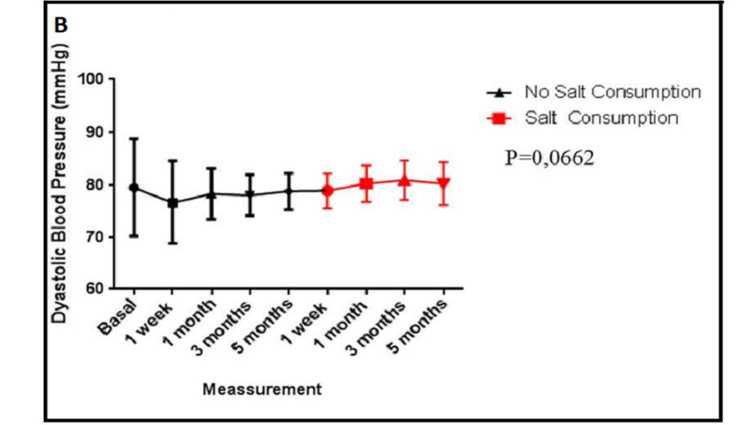
Figure 2. Effects of salt consumption on Dyastolic Blood Pressure
Discussion and сonclusions
The present study shows that the total omission of salt intake causes a significant immediate and progressive decrease in SBP, and the effect was not observed for the DBP. The decrease in SBP in following for five months was greater than 20 mmHg, and it might deduce that patients who were out of targets (>140 or 150 mmHg) reached goals only with that simple, economic and accessible intervention to all hypertensive patients. The mechanism that could intervene in the marked and immediate decrease in SBP may be mediated by a decrease in the concentration of sodium in the blood; eating a meal that containing salt raises the levels of serum sodium at 120 minutes, while a food without salt decreases concentration and in its turn the osmolality, this phenomenon decreases significantly the SBP, but the same effect for DBP is not observed. The high concentration of sodium in plasma, and therefore osmolality causes three responses that seek to increase blood volume: 1. Movement of fluid from the intracellular to the extracellular space; 2. It stimulates thirst, and 3. It increases secretion of antidiuretic hormone, which is evidenced clinically with an increase of 1.91mmHg in SBP with increasing the concentration of serum sodium in 1 mmol/L [28,29]. In addition, the patients that are more sensitive to salt, with the salt intake may have a greater increase in SBP and proteinuria, this may be due to an alteration in renal hemodynamics in this patients group [30].
The absence of significant reduction in DBP may be due to the hypertensive mechanism inducing by the salt is mainly mediated by changes in blood volume rather than changes at peripheral vascular resistance, which is the main modulator of PAD. In addition, vascular resistance also can be increased in response to the decrease in blood volume induced by low sodium intake. An increased activity of aldosterone renin-angiotensin-axis with the less consumption of salt has been already described. This may increase vascular resistance; activation axis in response to the absence of salt intake is not evident in black, elderly and / or chronic renal failure patients. It explains a greater reduction in BP with this intervention in this group of patients [31,32]. This divergence between the reduction in SBP and DBP had already been demonstrated in other studies [21,29]. This is an important finding since it is proven that the PAS is more associated with cardiovascular disease and predicts risk more accurately than the PAD [30-32].
The subsequent progressive increase of SBP with the consumption of salt administered by the researchers, which did not exceed the 10 mmHg, may be due to basal consumption levels in patients on average were 15-20g/day compared with 5g/day given by the researchers, this SBP would be within the targets set for hypertensive patients, so it would appear that a minimum restriction to 5g/day would be ideal in this population group.
List of abbreviations
HT - hypertension
BP - blood pressure
ACEi - angiotensin converting enzyme inhibitors
ARBs - angiotensin II receptor antagonists
SBP - systolic blood pressure
DBP - diastolic blood pressure
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
All authors coordinated and helped to draft the manuscript. All authors read and approved the final manuscript.
Список литературы Effects of total table salt restriction on blood pressure
- Global status report on noncommunicable diseases 2010. Geneva, World Health Organization, 2011.
- Rapsomaniki E1, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1•25 million people. Lancet. 2014 May 31;383(9932):1899-911.
- He FJ, Li J, MacGregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database of Systematic Reviews 2013, Issue 4. Art. No.: CD004937 DOI: 10.1002/14651858.CD004937.pub2
- Qin Y, Li T, Lou P, Chang G, Zhang P, Chen P. Salt intake, knowledge of salt intake, and blood pressure control in Chinese hypertensive patients. J Am Soc Hypertens. 2014 Dec;8(12):909-14. Epub 2014 Sep 28. http://www.ncbi.nlm.nih.gov/pubmed/25492834 DOI: 10.1016/j.jash.2014.09.018
- He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet. 2011 Jul 30;378(9789):380-2. http://www.ncbi.nlm.nih.gov/pubmed/21803192 DOI: 10.1016/S0140-6736(11)61174-4
- Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2011 Nov 9;(11):CD004022. http://www.ncbi.nlm.nih.gov/pubmed/22071811 DOI: 10.1002/14651858.CD004022.pub3
- Mozaffarian D1, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014 Aug 14;371(7):624-34 DOI: 10.1056/NEJMoa1304127
- Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007 May 10;356(19):1966-78.
- WHO guideline: sodium intake for adults and children. Geneva: World Health Organization, 2012.
- General Assembly of the United Nations. High-level meeting on non-communicable diseases, September 19-20, 2011
- Food and Nutrition Board, Institute of Medicine. Strategies to reduce sodium intake in the United States. Washington, DC: National Academies Press, 2010.
- US Dept of Agriculture and US Dept Health and Human Services. Dietary Guidelines for Americans 2010. US Govt Printing Office; US Dept of Agriculture and US Dept Health and Human Services, Washington, DC, 2010.
- Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012 Jul;33(13):1635-701. Epub 2012 May 3 DOI: 10.1093/eurheartj/ehs092
- Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013 Jul;34(28):2159-219. Epub 2013 Jun 14 DOI: 10.1093/eurheartj/eht151
- Kurtz TW, Al-Bander HA, Morris RC Jr. "Salt-sensitive" essential hypertension in men. Is the sodium ion alone important? N Engl J Med 1987; 317:1043.
- Barba G, Galletti F, Cappuccio FP, Siani A, Venezia A, Versiero M, et al. Incidence of hypertension in individuals with different blood pressure salt-sensitivity: results of a 15-year follow-up study. J Hypertens. 2007 Jul;25(7):1465-71.
- Capasso G, Cantone A, Evangelista C, Zacchia M, Trepiccione F, Acone D, et al. Channels, carriers, and pumps in the pathogenesis of sodium-sensitive hypertension. Semin Nephrol. 2005 Nov;25(6):419-24.
- Schmidlin O, Sebastian AF, Morris RC Jr. What initiates the pressor effect of salt in salt-sensitive humans? Observations in normotensive blacks. Hypertension 2007; 49:1032.
- Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT. Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation. 2012 Jun 26;125(25):3108-16. Epub 2012 Jun 18 DOI: 10.1161/CIRCULATIONAHA.112.096115
- Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014 Aug 14;371(7):601-11 DOI: 10.1056/NEJMoa1311989
- Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007 Apr 28;334(7599):885-8.
- Slagman MC, Waanders F, Hemmelder MH, Woittiez AJ, Janssen WM, Lambers Heerspink HJ, et al. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: randomised controlled trial. BMJ. 2011 Jul 26;343:d4366 DOI: 10.1136/bmj.d4366
- Pickering TH, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142-61.
- De Wardener HE, He FJ, MacGregor GA. Plasma sodium and hypertension. Kidney Int. 2004 Dec;66(6):2454-66.
- Suckling RJ, He FJ, Markandu ND, MacGregor GA. Dietary salt influences postprandial plasma sodium concentration and systolic blood pressure. Kidney Int. 2012 Feb;81(4):407-11. Epub 2011 Nov 2 DOI: 10.1038/ki.2011.369
- Weir MR, Dengel DR, Behrens MT, Goldberg AP. Salt-induced increases in systolic blood pressure affect renal hemodynamics and proteinuria. Hypertension. 1995 Jun;25(6):1339-44.
- Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. WNK1 kinase polymorphism and blood pressure response to a thiazide diuretic. Hypertension 2005; 46:758.
- Siffert W, Düsing R. Sodium-proton exchange and primary hypertension. An update. Hypertension. 1995; 26:649.
- Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009 Sep;54(3):475-81. Epub 2009 Jul 20 DOI: 10.1161/HYPERTENSIONAHA.109.131235
- Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001; 103: 1245-1249.
- Kannel WB. Elevated systolic blood pressure as a cardiovascular risk factor. Am J Cardiol. 2000; 85: 251-255.
- He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure in isolated systolic hypertension and combined hypertension. Hypertension. 2005 Jul;46(1):66-70. Epub 2005 Jun 13.


