Evaluation of general repolarization of cardiomyocites with biphasic pulses of different shapes
Автор: Chernov Nikolay N., Bezverkhii Aleksandr A., Timoshenko Vladimir I.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 16, 2020 года.
Бесплатный доступ
According to data provided by the European Resuscitation Council (ERC), 76% of sudden cardiac arrests should be attributed to ventricular fibrillation [1-3]. The main treatment of this disease is an immediate cardiopulmonary resuscitation, one of the components of which is a defibrillation of abnormal rhythms. The paper presents an analysis of advanced shapes of biphasic pulses, which have found a widespread application and have been clinically tested. The aim is to study the main parameters of the impact of different shapes of the existing pulses and their due consideration in a development of a defibrillator. An evaluation has been performed using defibrillators Fluke Impulse 7000DP and device Impulse 7010 designed to simulate different loads. Evaluated has been the shape of each of 7 biphasic pulses, the amplitude and exposure time of each of different signal phases. Upon results of the conducted analysis, some recommendations on cardiopulmonary resuscitation have been prepared; in particular, the necessity to maintain a constant current density of 14 -16 A, delivered for 4 -5 ms, is proposed. The maintenance of these parameters can be provided using the current stabilization technology (CST).
Biphasic pulse, defibrillation, cardiomyocytes repolarization, ventricular fibrillation, current-controlled defibrillation
Короткий адрес: https://sciup.org/148311466
IDR: 148311466 | DOI: 10.12710/cardiometry.2020.16.8084
Текст научной статьи Evaluation of general repolarization of cardiomyocites with biphasic pulses of different shapes
р.80-84; DOI: 10.12710/cardiometry.2020.16.8084; Available from:
Sudden cardiac arrest (SCA) is one of the leading causes of death in developed countries. According to data provided by the European Resuscitation Council (ERC), in 2015, 76% of sudden cardiac arrests should be attributed to ventricular fibrillation (VF) [1-3]. A marked increase in the VF share has been identified after taking active measures to apply automated external defibrillators (AED) [4-5] available at all the important public places. The main treatment of SCA is an immediate cardiopulmonary resuscitation (CPR) and defibrillation of abnormal rhythms, such as VF and ventricular tachycardia (VT). The AED availability and an early, within 3-5 minutes, defibrillation can raise a survival rate up to 50-70% [3,5,6].
The basic characteristics of defibrillators operating in manual and automated modes are the range of energies that the defibrillator is capable to produce, their pulse shape and their charging/discharging time. The first discharge shock energy for adults is 150 J with a possible further increase in case of inefficacy [7-9]. For adolescents aged 1 to 8 years in case of using manual defibrillators, it is necessary to use energy from 4 to 9 J / kg in the range of 50 -75 J [10-13]. As to the shape of the pulse used, they are biphasic in all modern defibrillators. A higher efficiency of the bipolar pulse in comparison to the monopolar one is supported by a large number both of theoretical and practical works [14-16]. The basic concept of the time requirement is to minimize it from the beginning of the rhythm detection to the readiness to discharge. Based on the duration of the proper defibrillation it is found that the time and amplitude of the second pulse phase should be lower. This parameter varies from one manufacturer to another, and each of them submits its own justifications of why to produce its own type of circuitry.
The pulse energy, its shape and the time should be optimal and serve two purposes. The first purpose is to provide a complete and simultaneous repolarization of all cardiomyocytes, and the second one is to reduce damaging negative effects made on cardiomyocytes. The major damage is done to mitochondria of cardiomyocytes, cristae of which are destroyed due to the action of high level energy. According to studies conducted in mice, the restoration of the above damaged structures takes longer than a week and may be irreparable [17]. The above mentioned purposes can be achieved using the current stabilization technology (CST), which provides constant current strength throughout the entire discharge, that makes the pulse almost rectangular and eliminates peak current fluctuations damaging the myocardium, which are typical to other pulse shapes (exponential, trapezoidal, sinusoidal type, etc. ). Based on the above, a development of a defibrillator requires a careful analysis of electropulse therapy (EPT) technologies and mathematical modeling of an impact produced by shapes of defibrillating.
The aim herein is to analyze and develop the optimal shape of an acting pulse for an external defibrillator.
Materials and methods
We have studied different pulse shapes, which have been clinically tested and used in automated and manual defibrillators. Our analysis is based on the impact of a biphasic pulse on cardiomyocytes. The following main energy characteristics of the defibrillator are compared: the shape, the duration and the amplitude of a pulse, as well as dependencies of these parameters on the load resistance magnitude, charging voltage and capacitance characteristics of a capacitor.
The study has been conducted with the Fluke Impulse 7000DP analyzer of defibrillators in transdermal pacemaker, with the use of an additional device Impulse 7010 for the selection of a defibrillator load.
Results and discussion
-
7 different types of pulses used in defibrillators for electropulse therapy have been investigated. Results of our studies are given below.
“The smart biphasic pulse” widely used in electropulse therapy practice is based on the 95 μF capacitor, which is charged up to 1625 V (energy 115 J) or 1800 V (energy 130 J), employing the 120 μF capacitor with a charge of 1800 V at a nominal pulse having an energy of 180 J.
At the onset of each pulse, a chest impedance has been assessed with serially connected resistors having a resistance of 22 ohms for 50 µs. During this period of time the patient’s impedance is determined, which should be at least 22 ohms. Based on the measured impedance, the time is specified in such a way that the nominal energy would be delivered in full. During our studies the pulses with an energy of 200 J and an impedance of 25, 50, 100 and 125 ohms have been applied. The measurement results are shown in Figure 1 herein.
Figure 1 shows that the pulse duration and its amplitude are highly dependent on the chest impedance. The ratio between the first and second phase current strengths is relatively constant in the pulse [18].
As opposed to the smart biphasic system, the "adaptive biphasic pulse” protocol is implemented with a possibility to adjust the delivered energy up to 360 J. To deliver this energy, in the circuit used is a capacitor of 210 μF that makes the pulse more prolonged. The results of measuring the pulses with an energy of 200 J at an impedance of 25, 50, 100 and 125 ohms are shown in Figure 2 herein.
As seen from the diagram in Figure 2, the feature of an adaptive pulse is a constant ratio between the second phase and the first one, which is always 2/3 of the first phase, regardless of the impedance. This compensates for internal losses, especially in patients with a low resistance, and slightly shortens the pulse duration in patients with a high resistance, so that with these changes make possible to maintain the rated output power always at the same level.
A self-compensating output signal of envelope-type pulse SCOPE (Self-Compensating Output Pulse Envelope Waveform) is widely used in the EPT practice. The feature of the circuitry of the defibrillators employing this type of pulses is the following sequence: capacitor - resistor - patient. It is just in this area where an evaluation of the patient impedance occurs. The pulse is provided with a capacitor of 120 μF. According to the studies conducted by the pulse technique developers, even in patients with a high resistance (> 100 ohms), the defibrillation is carried out successfully with a pulse energy of 100 J. A protocol of use of the defibrillators with this signal type has been adapted to circuit 150 J - 150 J - 200 J according to ERC2015. The diagram of studies on SCOPE pulses with an energy of 200 J at a load of 25, 50 and 100 ohms is shown in Figure 3 herein.
The diagrams show that both phases always have the same duration. In general, this sort of pulses is very similar to the "smart pulse", which shortens the second phase in case of longer pulses.
"Orbital biphasic pulses" illustrated by Figure 4 herein are positioned as low voltage (maximum voltage of 1350 V) defibrillation pulses. They are provided by capacitors of a high capacity of 500 µF.
Issue 16. May 2020 | Cardiometry | 81
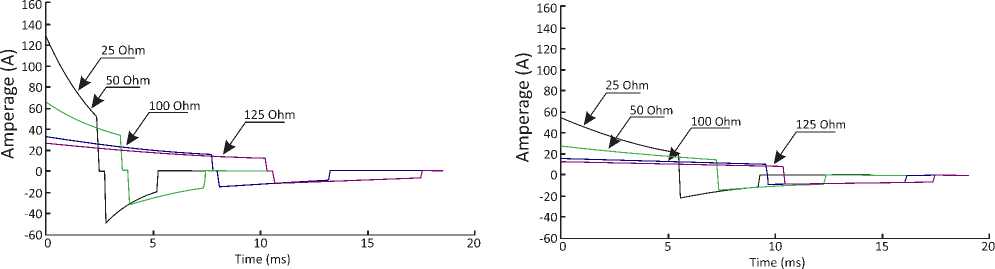
Figure 1. Pulse shape in “smart biphasic pulse» at a load of 25, 50, 100 and 125 ohms
Figure 2. Diagram of "an adaptive biphasic pulse" at a load of 25, 50, 100, 125 ohms
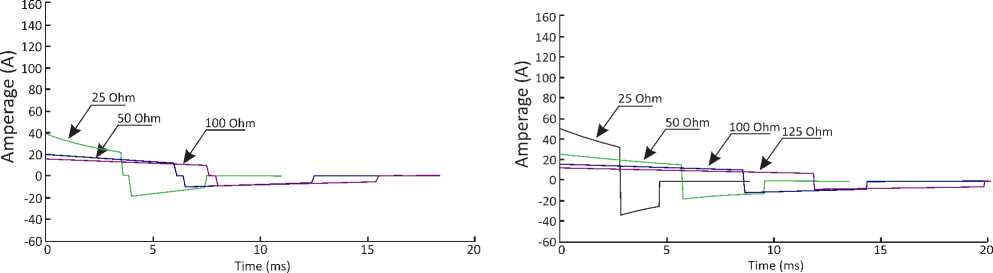
Figure 3. Diagram of the SCOPE pulse at a load of 25, 50 and 100 ohms
Figure 4. Diagram of “an orbital” pulse with an energy of 200 J at a load of 25, 50, 100, 125 ohms
Figure 4 shows that the signals are characterized by a prolonged pulse duration (up to 35 ms with a high resistance). Previously it was assumed that it was impossible to efficiently use the technology in patients having a high resistance. However, some studies in animals have demonstrated the opposite. Studied were 6 dogs weighing 21.6 to 34.5 kg, and it was found that the defibrillation threshold was from 20 to 30 J, which was comparable with the biphasic defibrillator with a voltage of 2 kV. Patients with a high resistance were modeled with an additional resistor of 32 ohms, the threshold defibrillation rose to 34.3 J. Despite the obtained results, which are not typical to humans, developers believe that the orbital biphasic pulses may be applicable to humans.
Figure 5 gives a "multipulse" discharge type, which demonstrates a feature to represent each phase in the form of pulses with a frequency of 5 kHz and a pulse/ pause ratio of 1: 1. Finally, the single-phase pulse studies have shown that such pulses behave as a closed signal of a medium current strength [19,20]. As is known, the pulse energy depends on the square of the current, and a pulse interruption leads to an increase in energy requirements. This is compensated by the fact that the declared pulse duration is closer to the minimum nec- 82 | Cardiometry | Issue 16. May 2020
essary for the cardiomyocytes excitation, in comparison with the biphasic pulse shapes as discussed above.
Figure 5 gives an illustration of fundamental differences between the "multipulse" discharge from the previously described discharge techniques, but in fact this is a standard bipolar exponentially truncated signal. The protocol of the energy increase recommended by the developers implies starting with 90 J and maximizing up to 180 J. The energy of 180 J is positioned as a "threefold energy margin”.
Used is the so-called STAR discharge which represents a biphasic pulse. It has long been considered to be optimal from the standpoint of the structure of the second phase, which consequently implements the theory of "a charge balance". The patents describe a debatable discrete equivalent circuit diagram and some findings associated therewith [21,22]. Impedance is mentioned as an additional feature, although its importance cannot be underestimated [23]. These facts do not allow us considering the "STAR pulse” as a relevant pulse circuitry.
As a “linear” pulse described is a pulse, which in the first phase is close to a rectangular pulse with a constant current of 15A. It is emphasized that the time is constant for any allowable resistance. This is sup-
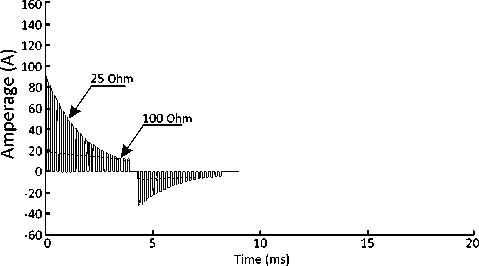
Figure 5. Diagram of “a multipulse” signal with an energy of 200 J at a load of 25 and 100 ohms
The "biphasic" pulse peculiarity is a programmable switch, which allows changing the ratios of the delivered energy. In the design settings, the developers preset the ratio of energies as 90% in the first and the remaining 10% in the second phase. When testing the signal, the first pulse duration always is 4 ms, which is the optimal time to complete repolarization according to numerous studies [15]. As it is the case with the previous signal, this can be realized at high voltage charging only. Diagrams of pulse with an energy of 200 J at a load of 25, 50, 100 and 125 ohms are given in Figure 7 herein.
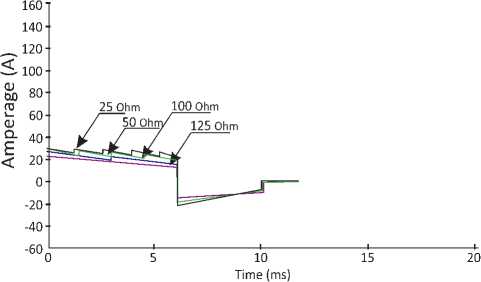
Figure 6. Diagram of “a linear” pulse with an energy of 200 J at a load of 25, 50, 100 and 125 ohms
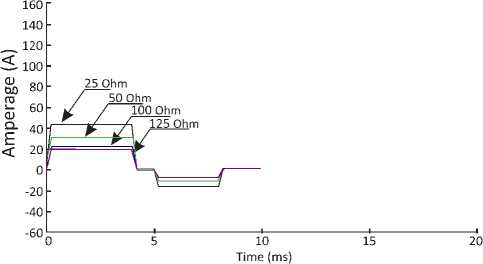
Figure 7. Diagram of “a biphasic” pulse at a load of 25, 50, 100 and 125 ohms ported by the results of the pulse test, presented in Figure 6 herein.
Thanks to the constant current density the efficacy considerably increases, especially in the patients with a low resistance. The patients with a high resistance, in their turn, are exposed to a standard bipolar pulse, which is relatively shorter than the above one. From the standpoint of engineering, the pulse shaping is provided with the use of serially connected resistors, the required set of which is switched depending on the patient’s actual impedance [24]. An imperfection of this circuit is a high voltage, when discharging to low resistance, despite the stated CCT system.
Conclusions
Considering the conducted analysis of the existing developments in the field of external defibrillation, the applicable recommendations on cardiopulmonary resuscitation, and the results of the theoretical research, we may arrive at conclusions as follows:
-
1. Optimal is the biphasic pulse of rectangular shape, that provides a constant current density of 14 -16 A, delivered in 4 -5 ms. The maintenance of these parameters can be achieved using the current stabilization technology.
-
2. According to the recommendations, the starting charge for adults is 150 J, with a possibility of increasing it up to 360J. The conducted studies on the presented biphasic pulses demonstrate the possibility of achieving general repolarization with lower values of energy, but it is necessary to have an engineering solution to deliver the maximum energy of 360J.
-
3. The ratios between the first phase and the second phase of the pulses in external biphasic defibrillators under consideration show significant differences, but all of them have been implemented in clinically approved defibrillators. So, we can conclude that the issue on the ratio between the phases remains on the agenda as a subject for further research.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Evaluation of general repolarization of cardiomyocites with biphasic pulses of different shapes
- Ringh M, Herlitz J, Hollenberg J, Rosenqvist M, Svensson L. Out of hospital cardiac arrest outside home in Sweden, change in characteristics, outcome and availability for public access defibrillation. Scan-dinavian journal of trauma, resuscitation and emer¬gency medicine 2009; 17: 18.
- Hulleman M, Berdowski J, de Groot JR, et al. Im¬plantable cardioverter defibrillators have reduced the incidence of resuscitation for out of hospital cardiac arrest caused by lethal arrhythmias. Circulation 2012; 126: 815–21.
- Blom MT, Beesems SG, Homma PC, et al. Improved survival after outofhospital car diac arrest and use of automated external defibrillators. Circulation 2014; 130: 1868–75.
- Weisfeldt ML, Sitlani CM, Ornato JP, et al. Surviv¬al after application of automatic external defibrillators before arrival of the emergency medical system: evalua¬tion in the resuscitation outcomes consortium popula¬tion of 21 million. J Am Coll Cardiol 2010; 55: 1713–20.
- Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out_of_hos¬pital cardiac arrest. Circulation 2011; 124: 2225–32.
- Ringh M, Rosenqvist M, Hollenberg J, et al. Mobile_phone dispatch of laypersons for CPR in out_of_hos¬pital cardiac arrest. The New England journal of med¬icine 2015; 372: 2316–25.
- Deakin CD, Nolan JP, Sunde K, Koster RW. Europe¬an Resuscitation Council Guidelines for Resuscitation 2010 Section 3. Electrical therapies: automated ex¬ternal defibrillators, defibrillation, cardioversion and pacing. Resuscitation 2010; 81: 1293–304.
- Koster RW, Walker RG, Chapman FW. Recurrent ventricular fibrillation during advanced life support care of patients with prehospital cardiac arrest. Resus¬citation 2008; 78: 252–7.
- Morrison LJ, Henry RM, Ku V, Nolan JP, Morley P, Deakin CD. Single_shock defibrillation success in adult cardiac arrest: a systematic review. Resuscitation 2013; 84: 1480–6
- Gurnett CA, Atkins DL. Successful use of a biphasic waveform automated external defibrillator in a high_risk child. The American journal of cardiology 2000; 86: 1051–3.
- Rossano J, Quan L, Schiff M, MA K, DL A. Survival is not correlated with defibrillation dosing in pediat¬ric out of hospital ventricular fibrillation. Circulation 2003; 108: IV–320–1.
- Samson R, Berg R, Bingham R, Pediatric Advanced Life Support Task Force ILCoR. Use of automated ex-ternal defibrillators for children: an update. An advi¬sory statement from the Pediatric Advanced Life Sup¬port Task Force, International Liaison Committee on Resuscitation. Resuscitation 2003; 57: 237–43.
- Berg RA, Samson RA, Berg MD, et al. Better out¬come after pediatric defibrillation dosage than adult dosage in a swine model of pediatric ventricular fibril¬lation. J Am Coll Cardiol 2005; 45: 786–9.
- Bett GCL, Rasmusson RL: Computer Models of Ion Channels. In Quantitative Cardiac Electrophysi¬ology Edited by: Cabo C, Rosenbaum DS. New York: Marcel Dekker, Inc; 2002:1-60.
- Priebe L, Beuckelmann DI: Simulation Study of Cellular Electric Properties in Heart Failure. Circ Res 1998, 82:1206-1223.
- Carpenter J, Rea T, Murray JA, Kudenchuk PJ, Eisenberg MS: Deflbrillation waveform and post-shock rhythm in out-ofhospital ventricular fibrillation cardiac arrest. Resuscitation 2003, 59:189-96.
- Ferreira M, Ferreira C, de Abreu LC, et al. Myocar¬dium tissue changes caused by electrical transthoracic discharges in rats. Int Arch Med. 2009;2(1):31. Pub¬lished 2009 Oct 23. doi:10.1186/1755-7682-2-31
- J. Malmivuo and R. Plonsey, Bioelectromagnetism. Oxfort University Press, 1995.
- A. Valance, «La défibrillation semi-automatique par les Sapeurs-Pompiers de Meurthe-et-Moselle». Master's thesis, Nancy, (F), 2002.
- R. Sweeney, R. Gill, J. Jones, and P. Reid, «Defibril¬lation using a high-frequency series of monophasic rectangular pulses: observations and model predic¬tions», Journal of cardiovascular Electrophysiology, vol. 7, pp. 134-143, 1996.
- J. E. Brewer, K. F. Olson, B. L. Gilman, and R. E. Bosler, «Continual waveform shape reforming meth¬od and apparatus for transchest resistance dynamics». US 6,198,967 B1, 06. März 2001.
- Brewer JE, Stendahl GB, and Olson KF. “Method and Apparatus for delivering a Defibrillation Pulse with variable Energy”. WO 02/28479 A1, 11. April 2002.
- A. Cansell and I. Daskalov, “Defibrillation Signal, Method and Device for adjusting Defibrillation En¬ergy relative to a Patientt's transthoracic Resistence". WO 03/055557 A1, 10.07.2003.
- S. Ayati and M. L. Lopin, “Electrotherapy Current Waveform". WO 98/26841, 25.06.1998.


