Evaluation of proprotein convertase subtilsin /kexin 9(PCSK9) in serum of men hypertensive patients
Автор: Al-mohtaser Y.A.H.M., Al-dujaili A.N.G.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 31, 2024 года.
Бесплатный доступ
High blood pressure is considered a major factor for the development of heart disease and vascular disease in elderly people, due to higher tension in arteries leading to hypertension. PCSK9 is a proprotein convertase that increases circulating LDL levels by directing hepatic LDL receptors into lysosomes for degradation. The effects of PCSK9 on hepatic LDL receptors and contribution to atherosclerosis via the induction of hyperlipidemia are well defined.
Proprotein convertase subtilsin /kexin 9(pcsk9), cholesterol (cho), triglyceride (tg), high density lipoprotein (hdl), & low-density lipoprotein (ldl)
Короткий адрес: https://sciup.org/148328847
IDR: 148328847 | DOI: 10.18137/cardiometry.2024.31.174184
Текст научной статьи Evaluation of proprotein convertase subtilsin /kexin 9(PCSK9) in serum of men hypertensive patients
Yousra Abdul Hussein M Al-mohtaser, Arshad Noori G. Al-Du-jaili. Evaluation of proprotein convertase subtilsin /kexin 9(PCSK9) in serum of men hypertensive patients. Cardiome-try; Issue 31; May 2024; p. 174-184; DOI: 10.18137/cardiome-try.2024.31.174184; Available from: https://www.cardiometry. net/issues/no31-may-2024/evaluation-proprotein-convertase
High blood pressure is considered a major factor for the development of heart disease and vascular disease in elderly people, due to higher tension in arteries leading to hypertension. Elderly is often affected by hypertension caused by stiffness in the arteries so that blood pressure tends to increase. Hypertension is often referred as a silent killer disease, because it is often hypertensive patients for years without feeling any disturbance or symptoms[1]. The PCSK9 site comprised by amino acid residues 367–381 which is situated on the PCSK9/LDLR binding interface, was considered to be targeted by inhibitors.
After the removal of the EGFA domain, [2, 3]. PCSK9 is a proprotein convertase that increases circulating LDL levels by directing hepatic LDL receptors into lysosomes for degradation. The effects of PCSK9 on hepatic LDL receptors and contribution to atherosclerosis via the induction of hyperlipidemia are well defined. Monoclonal PCSK9 antibodies that block the effects of PCSK9 on LDL receptors demonstrated beneficial results in cardiovascular outcome trials[4, 5]. The structure and binding receptors of PCSK9 are shown in Figure (1).
Figure (1) ( A ) The domain structure of human PCSK9 in its zymogen form. The numbering throughout indicates the position of significant amino acid residues including D186, H226 and S386, which form the catalytic triad of PCSK9. D374Y indicates an amino acid substitution that has been characterized as a gain-of-function mutation. ( B )
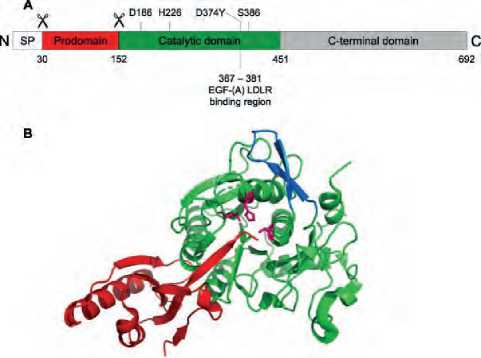
Figure (1) The structure and binding receptors of PCSK9{Evison, 2020 #3
A three-dimensional cartoon representation of the X-ray crystal structure of human PCSK9 lacking its C-terminal domain.
The Prodo main is colored in red, the catalytic domain in green and the catalytic residues D186, H226 and S386 in pink. The region of PCSK9 that directly interacts with the EGF-(A) domain of LDLR is shown in blue. Adapted from PDB file code 4NMX[2, 4].
METHODS
Subject population
The present study was designed to investigate an important biomarker Proprotein Convertase Subtilsin /kexin 9(PCSK9) as a prediction or prognostic biomarker in hypertensive patients and relation with lipid profile (cholesterol, triglyceride, HDL, and LDL)
The following criteria were dependent in a current study:
-
1. Four biomarkers (PCSK9, Cholesterol, TG, and HDL) level in serum
-
2. Ages
-
3. Body mass index
-
4. Hypertensive patients with and without treatment
-
5. Sex (only male)
-
6. Duration of disease
-
7. Smoking or no
-
8. Familial hypertensive or no
Exclusion criteria
The current study excluded many criteria related to diabetic nephropathy, kidney disease, or any complications such as liver disease, heart disease, and anemia, also excluded.
Blood collection
Each patient and control group undergo a drawn of blood samples from venous at 5 milliliters and left at room temperature for 10 minutes for collecting and then centrifuged at 3000 rpm for 15 minutes for given a serum then 1.5 milliliters was transferred to Eppendorf tube for PCSK9and lipid profile measurement.
The serum transported to new Eppendorf tubes and stored at-20 co unlit was used.
Body Mass Index (BMI)
Body mass index was calculated by following formula BMI = kg/m2 where kg is a person›s weight in kilograms and m2 is their height in meters squared
Underweight < 18.5 kg/m2
Normal weight = 18.5–24.9 kg/m2
Overweight = 25–29.9 kg/m2
Obesity = BMI of 30 kg/m2 or greater
DIAGNOSIS
Hypertension is diagnosed if, when it is measured on two different days, the systolic blood pressure readings on both days is ≥140 mmHg and/or the diastolic blood pressure readings on both days is ≥90 mmHg.
Biomarker measurement
The assessment of serum lipid profile of cholesterol, triglyceride and HDL, which uses an automated microtiter plate ELISA reader and an enzyme-linked immunosorbent assay Biotek, USA) is provided by Human Proprotein Convertase Subtilsin /kexin 9(PCSK9) ELISA Kit ( Pars Biochem ).
Statistical analysis
The results were expressed as (Mean ± Standard Error). correlation coefficients were calculated to estimate the correlation between parameters.
The descriptive statistics and correlation coefficients were performed by using IBM SPSS Statistics version 26 .2019.
Unpaired sample t-test was used for the comparison between the patients and control groups and multiple comparison for observed mean test (by Tukey multiple comparison test) was used for the comparison among subdivided groups, while the figures constructed by using excel program. p < 0.001 was used as a level of statically significant.
RESULTS
Blood pressure of hypertensive patients in comparison with control group.
in Figure (2) and Figure (3) show signification increase (p-value<0.01) in hypertensive patients in both Diastolic(10.350±1.0508mmHg) and systolic pres-sure(16.23±1.226358mmg) Comparison with control group (systolic12 mmHg and diastolic 8 mmHg).
I 15
E
£ 10
<
2 5
1 2 m mHg
1 6.23 ± 1 .22 * m mHg

control systolic pateins systolic
S YSTOLI C PRESSUR E FO R CONTRO L AN D P ATIENTS
■ control systolic ■ pateins systolic
12,0
10,0
CD
E 8,0
E 6,0
1 4,0
2,0
0,0
1 0,4 ± 1 .05 * m mHg
8 . 0 m mHg

diastolic(control)
diastolic(patients)
d iastolicfo r contro l an d patiens
diastolic(control) ■ diastolic(patients)
Figure (3) diastolic Blood pressure of hypertensive patients in comparison with control group. N=60 (Patients), N= (Control group). (*) refer to significant differences between patients and control group of p- value < 0.01.
Lipid profile in hypertensive patients in compare with control group.
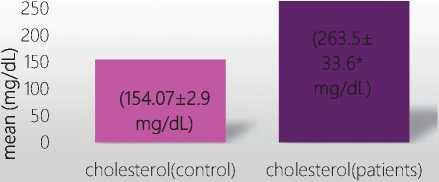
The results of the current study Figure (4) showed that there are significant increase (p<0.01) in cholesterol level between patients (263.53 ±33.693 mg/dL) with high blood pressure and control group (154.067± 2.99 mg/dL),also significant increase (p<0.001) in Triglyceride level of patients(275.67±275.67 mg/dL ) in compare with control group) 112.167±18.456mg/ dL),as in Figure(5) in addition Figure(6) indicate signif-
C holestero l fo r patient s an d c;ntro l grou p i n b lood
■ cholesterol(control) ■ cholesterol(patients)
Figure (4) cholesterol level in hypertensive patients in compare with control group. N=60(patients), N=30(control). (*) refer to significant differences of p- value < 0.01.

(112.17±18.45 mg/dL)
TG(CONTROL)

TG for control and patiens
■ TG(CONTROL) ■ TG(PATIENTS)
Figure (5) Triglyceride level in hypertensive patients in compare with control group. N=60(Patients), N=30(Control). (*) refer to significant differences of p- value < 0.01.
_I 40
^s 30
E
20 D
45.067± 3.41 mg/dL
15.5 ± 7.18* mg/dL
HDL(C0NTROL)
HDL(PATIENTS)
HDL for control and patiens
■ HDL(C0NTROL) ■ HDL(PATIENTS)
Figure (6) Low density lipoprotein level in hypertensive patients and control group. N=60(Patients), N=30(Control). (*) refer to significant differences of p- value < 0.01.
icant decrease(p<0.05) in HDL-level in patients(15.5 ± 7.17 mg/dL ) in compare with control group) 45.067± 3.41mg/dL)as well as Figure (7) revealed a significant
increase in LDL-Level in patients(143.8±12.15mg/dL) in compare with control group) 80.167± 9.24mg/dL).
LDL(CONTROL) LDL(PATIENTS)
Figure (7)
Comparison between Hypertensive patients and control group with PCSK9.
From Figure (7) refer to significant differences of p-value < 0.01 in PCSK9 level in patients(33.16±13.8ng/L) in compare with control group(5.64±0.34ng/L).
35,00
30,00
25,00
20,00
15,00
10,00
5,00
0,00
5,64±0.34 ng/L
PCSK(control)

PCSK9(PATIENTS)
PCSK(control) PCSK9(PATIENTS)
Figure (7) Comparison between Hypertensive patients and control group With PCSK9 level. N=30(control), N=60(patients). (*) refer to significant differences of p- value < 0.01.
Comparison between Hypertensive patients according to age.
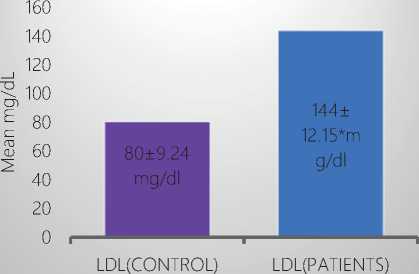
From Figure (8) appear significant increase (p<0.001) in PCSK9 level (48.46±11.9ng/L) In age group (40-49) years higher than age group (50-59) years and age (60-69) with mean (30.76±2.62ng/L) &(20.57±3.43ng/L) respectively .
Comparison between hypertensive patients according to duration of disease.
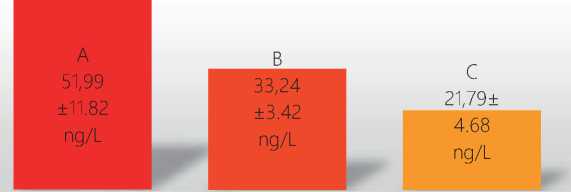
In Figure (9) document that significant increase (p<0.01) in PCSK9 level in duration of disease, duration (one month-one year) in mean (51.99± 11.82ng/L) in compare with duration (1-10) years in mean (33.24± 3.43ng/L) and duration (11-20) years in mean (21.79± 4.68ng/L).
Comparison between hypertensive patients according to treatment.
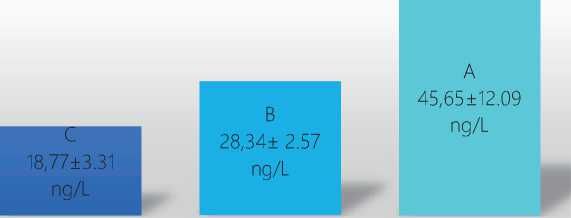
From Figure (10) indicate significant increase (p<0.01) in PCSK9 level indicate significant increase (p<0.01) in PCSK9 level in patients without treatment (45.65±12.09 ng/L) in compare with treatment (24.24± 5.59ng/L).
Comparison according to Smoking.
From Figure (11) show significant increase (p<0.05) in PCSK9 level in Smoking group (41.27± 12.37ng/L) higher than non-Smoking (21.79± 4.68ng/L).
Comparison between hypertensive patients according to body mass index.
From Figure (12 ) appear significant increase (p<0.01) in PCSK9 level in obese hypertensive patients (45.65± 12.09ng/L) in PCSK9 level higher than over-
60,00
50,00
40,00
30,00
20,00
10,00
0,00
age(40-49) age(50-59) age(60-69)
comparision between hypertensive patients according to age
age(40-49) age(50-59) age(60-69)
60,00
50,00
1? 40,00
30,00
20,00
10,00
0,00
duration(one month- duration(1-10 years) duration(11-20 years) one year) duration of disease
■ duration(one month-one year) ■ duration(1-10 years) ■ duration(11-20 years)
50,00
40,00
30,00
20,00
10,00
0,00
50,00

without treatment with treatment
40,00
30,00
20,00
10,00
0,00

smoking non smoking
comparison according to Treatment comparison according to smoking
■ without treatment ■ with treatment
■ smoking ■ non smoking
Figure (10) Comparison between Hypertensive patients according to treatment. N=25(without treatment), N=35(with treatment). (*) refer to significant differences of p- value < 0.01.
Figure (11) Comparison between Hypertensive patients according to Smoking. N=35(Smoking), N=25(non-Smoking). (*) refer to significant differences of p- value < 0.01.
50,00
40,00
30,00
20,00
10,00
0,00
weight(normal)
weight(over)
weight(abese)
■ weight(normal) ■ weight(over) ■ weight(abese)
weight (28.34± 2.57ng/L) and normal weight (18.77± 3.31ng/L).
Comparison between Hypertensive patients according to familial hypertensive.
Results of Figure (13) show significant increase (p<0.01) in PCSK9 level in familial hypertensive patients (43.59± 12.41ng/L) in compare with patients non familial (23.29± 5.19 ng/L).
50,00
40,00
I1 30,00
20,00
10,00
0,00
43,60± 12.41* ng/L
23,29±5.1
9 ng/L

Familial non Familial
-
■ Familial ■ non Familial
Figure (13) Comparison according to familial hypertensive. N=30(familial hypertensive), N=30(non-familial). (*) refer to significant differences of p- value < 0.01.
PCSK9 level and lipid profile.
From figure (15), (16) and (18) indicate a positive significant correlation between PCSK9 and cholesterol, triglyceride and LDL-levels also negative signifi- cant correlate between PCSK9 and HDL-level significant in figure (17).
Correlation between PCSK9 and cholesterol level in hypertensive patients and control group.
The results of correlation and liner regression between PCSK9 level and cholesterol levels are indicated by the person of a significant positive correlation (p< 0.001) between PCSK9 and cholesterol levels of hypertensive patients (R”=0.892), Y=1.5E2+3.22*X, Figure (15).
Correlation between PCSK9 and triglyceride level in hypertensive patients and control group.
The results of correlation and liner regression between PCSK9 level and triglyceride levels are indicated by the person of a significant positive correlation (p< 0.01) between PCSK9 and triglyceride levels of hypertensive patients (R”=0.906), Y=1E2+5.04*X, Figure (16).
Correlation between PCSK9 and High-density lipoprotein level in hypertensive patients and control group.
The results of correlation and liner regression between PCSK9 level and High-density lipoprotein levels are indicated by the person of a significant positive correlation (p< 0.01) between PCSK9 and High-density
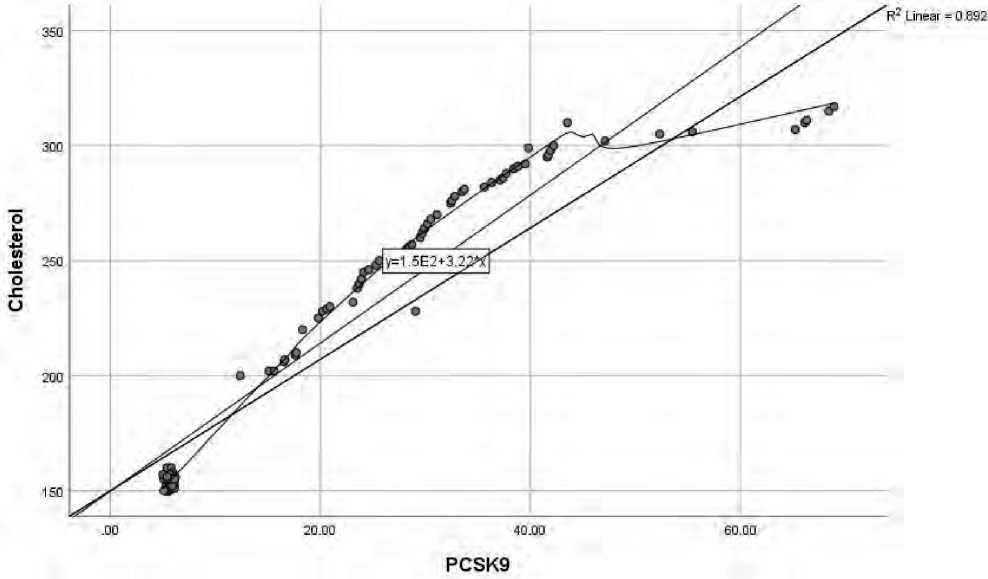
Figure (15) Relation between PCSK9 and cholesterol level in hypertensive patients.
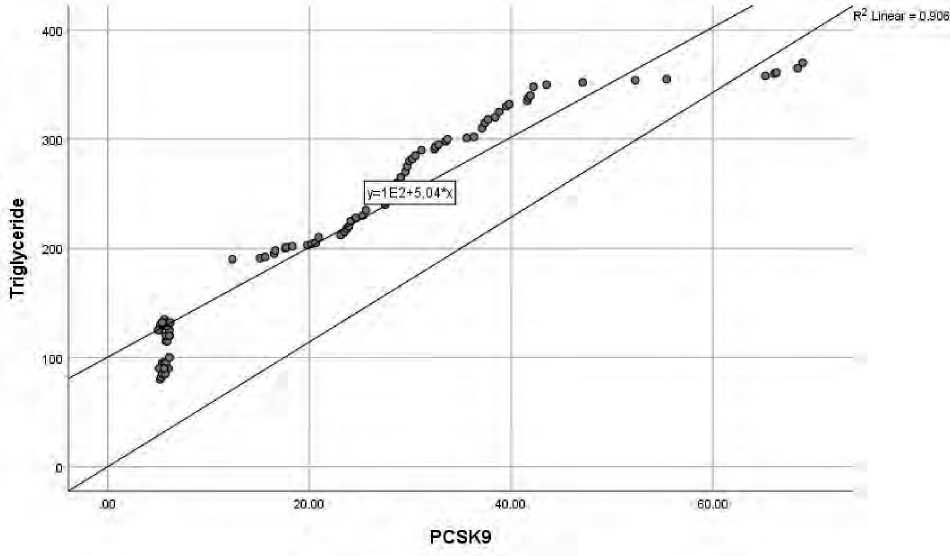
Figure (16) Relation between PCSK9 and triglyceride level in hypertensive patients.
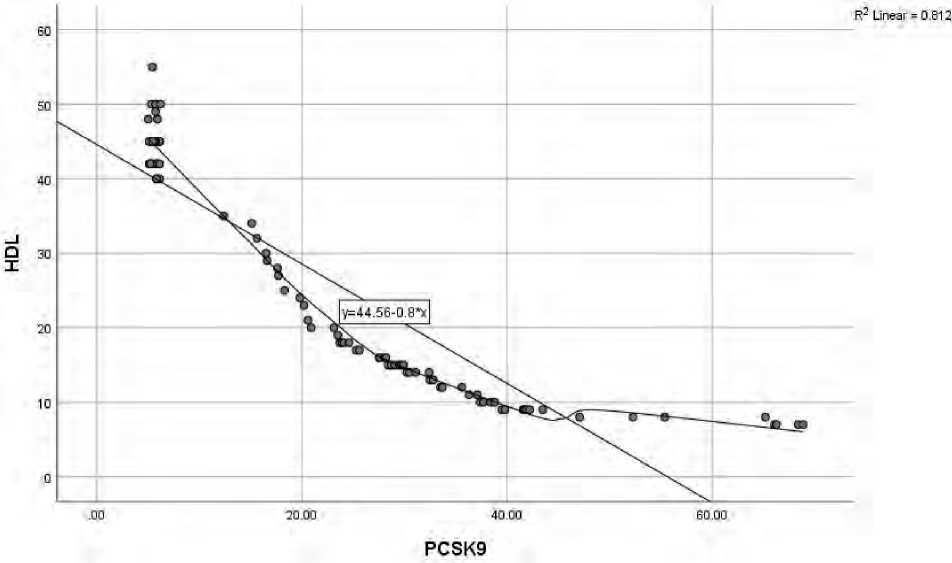
Figure (17) Relation between PCSK9 and HDL-level in hypertensive patients
lipoprotein levels of hypertensive patients (R”=0.812), Y=44.56-0.8*X, Figure (17).
Correlation between PCSK9 and Low-density lipoprotein level in hypertensive patients and control group.
The results of correlation and liner regression between PCSK9 level and low-density lipoprotein levels are indicated by the person of a significant positive correlation (p< 0.01) between PCSK9 and low-density lipoprotein levels of hypertensive patients (R”=0.801), Y=82.49+1.67*X, Figure (18).
DISCUSSION
From the results of Figure (7) found that a significant increase p- value < 0.05 in PCSK9 level
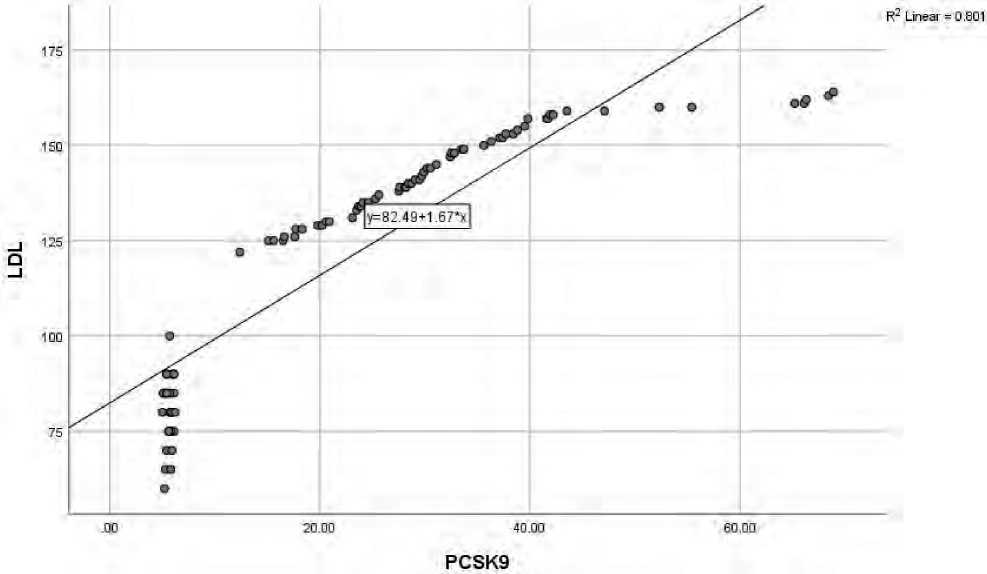
Figure (18) Relation between PCSK9 and LDL-level in hypertensive patients.
in Hypertensive patients in compare with control group.
The present study agree with several studies that has been suggested a relation between PCSK9 level and hypertension (systolic and diastolic) and discuss the relation depend on that decrease (PCSK9) considered as a main regulator of LDL-C by binding with hepatic LDL-receptors which lead to in hance in LDL-degra-dation and promoting LDL-c conception and may effect on develop Wal of hypertension[3, 6, 7].
An important mechanism has been postulated to show a role of PCSK9 in hypertension. Invitro appear that increase level of PCSK9 may result a downregulat-ed epithelial Na+ absorption by reducing the epithelial
Na+ channel expression, and the researchers speculated that PCSK9
could contribute to BP control[8].
The current as in figure (8) indicate a significant increase in PCSK9 level in age (40-49) years as compared with another ages (50-59) and (60-69) years old.
Some studies have been revealed that a level of PCSK9 decrease with age in men but increase in age in women and this result due to effect of testosterone level in men and estrogen level in women in other words increase testosterone associated with high PCSK9level whereas low level at advanced age negatively associated with PCSK9 and considered as a risk factor for initiation hypertension or risk factor [9]. The age (40-
-
49) years in present study has higher PCSK9 level in compare with other ages may result due to that these ages have new diagnosed or and do not administrate to any types of therapy.
From figure (9) also show a significant increase in duration of disease one month to one year in compare with anther duration of diseases and this result may support our view that a hypertensive patients in present study that do not administrated any type of therapy or checking a blood pressure newly after suffering a some of symptoms associated with highly PCSK9 level. also figure (10) proved that a patients of present that newly diagnosed with any treatment has a highly a level of PCSK9 and this may related with high LDL-C,VLDL,TG concentration without any therapy lacking (hypolipidemic or hypertensive drug may result to occurrence of blood pressure in these patients highly in compare with treated patients[10-13].
Figure (11) revealed a significant increase in PCSK9 level in smoker patients in compare with non-smoker.
The current results agreement with several studies that showed that cigarette smoking extract in hance a level of PCSK9 by a mechanism including stimulation of various harmful substances such as high concentrations of oxidant and include Reactive oxygen species production (ROS) which is considered one of the major cause of arterial hypertension and atherosclerosis in carotid arteries also produce a proinflammatory factor such as oxidized LDL, Tumor necrosis factor TNF-α through a signaling ROS/Nuclear factor Kap-pa-β (NFK-β) with high LDL-C level all these may be associated with high PCSK9 level[14, 15].
A present result in figure (12) documented high level of PCSK9 in obese hypertensive patients in compare with overweight and normal weight.
In a previous study has been showed that high level of PCSK9 in obese individuals after exposure to pollution as a result of increase in proinflammatory mediator such as cytokines /adipokines in adipose tissue also over production of ROS therefore obesity it’s a strong risk factor for hypertension atherosclerosis with high LDL-C level [16-19].
Incurrent results as in figure (4-13) indicate a high level of PCSK9 level in familial hypertensive patients in compare with non-familial previous study has been found that defect in the epithelial Na-channel (ENaC) has a crucial role in Na+-homeostasis and control of blood pressure and found that defection a regulation of ENaC lead to form a inherited form of hypertensive and hypotension and show that PCSK9 as a proteases regulate a ENaC gating channel and reduce a hypertension or CVD[20, 21] .
In several research has been suggested that PCSK9 has acritical role in regulation by trafficking ENaC in pathway of synthesis by reducing ENaC channel numbers and Na+ absorption therefore and disruption of PCSK9 lead to high expression of Na + by excessive renal Na+ and these defects known as genetic hypertension forms[22, 23] .
The figure (15), (16), and (18) show a significant positive correlation between PCSK9 and cholesterol, TG and LDL whereas significant negative correlation with HDL as in figure (17).
Previous study Abi faded et al, [24] has been described that cholesterol metabolism and hypercholesterolemia linking with serine protease producing by the liver such as PCSK9 also with LDL-C through
Mediate LDL-R, receptors degradation therefore lowering and fewer LDL-receptors on membrane and decrease clearance from circulation so that high PC-SK9associated with high LDL-C, cholesterol, and triglyceride [25] [26].
In other demographic studies on several metabolic parament has been document a correlation between PCSK9 and other parameters such as LDL-C, HDL-C, Cholesterol, Triglyceride, apolipoprotein n-B, Insulin and glucose [27] [28].
182 | Cardiometry | Issue 31. May 2024
In a study of [29] has been indicated that both secretion and degradation of TG-rich lipoprotein so that hypertriglyceridemia with high PCSK9 linked with multiple mechanism such as increased secretion of APO-B containing lipoprotein in liver and stimulate degradation of LDL-R receptors.
Some former studies have been linked between as present of mature PCSK9 and furin cleaved in circulation with predicts of atherosclerosis and coronary heart disease with high LDL-C and cholesterol [30] [31] [32] [30].
Another studies evident that PCSK9 associated with blood pressure, age, smoking, obesity and correlation with level of apo-B, LDL-C and triglyceride [33] [32] [34].
CONCLUSION
-
1. The present study concluded that PCSK9 considered as a progrestc marker for prediction of hypertension.
-
2. PCSK9 was very related in hypertensive patients with hyperlipidemia (cholesterol, TG, LDL, & HDL)
-
3. High biomarker level associated with ages especially at new diagnosis without treatment and with short duration of disease.
-
4. smoking play important roles with high a level of PCSK9 in hypertensive patients.
-
5. The genetic may play a role in present study by high level of This biomarker in familial hypertensive patients.
-
6. Obesity have a crucial role in in hypertensive patients with high PCSK9 level.
Список литературы Evaluation of proprotein convertase subtilsin /kexin 9(PCSK9) in serum of men hypertensive patients
- Beltrami M, et al. Long-Term Prevalence of Systolic Dysfunction in MYBPC3 Versus MYH7-Related Hypertrophic Cardiomyopathy. Circulation: Genomic and Precision Medicine. 2023;16(4):363-71.
- Kuzmich N, et al. PCSK9 as a Target for Development of a New Generation of Hypolipidemic Drugs. Molecules. 2022;27(2):434.
- Ahamad S, Bhat SA. Recent update on the development of PCSK9 inhibitors for hypercholesterolemia treatment. Journal of Medicinal Chemistry. 2022;65(23):15513-39.
- Seidah NG, Garçon D. Expanding biology of PCSK9: roles in atherosclerosis and beyond. Current atherosclerosis reports. 2022;24(10):821-30.
- Laurent S, Boutouyrie P. Arterial stiffness and hypertension in the elderly. Frontiers in cardiovascular medicine. 2020;7:544302.
- Silla A, et al. Treatment with PCSK9 inhibitor evolocumab improves vascular oxidative stress and arterial stiffness in hypercholesterolemic patients with high cardiovascular risk. Antioxidants. 2023;12(3):578.
- Lupo MG, et al. PCSK9 promotes arterial medial calcification. Atherosclerosis. 2022;346:86-97.
- Schremmer J, et al. Chronic PCSK9 inhibitor therapy leads to sustained improvements in endothelial function, arterial stiffness, and microvascular function. Microvascular research. 2023;148:104513.
- Hwang HS, et al. Circulating PCSK9 level and risk of cardiovascular events and death in hemodialysis patients. Journal of Clinical Medicine. 2020;9(1): 244.
- Parthymos I, et al. Lipoprotein (a) as a treatment target for cardiovascular disease prevention and related therapeutic strategies: a critical overview. European Journal of Preventive Cardiology. 2022;29(5):739-55.
- Wang D, Zhang D. Safety issues associated with the clinical application of Pcsk9 inhibitors: Current findings. Cardiology in Review. 2023;31(3):155-61.
- Merćep I, et al. Present and future of dyslipidaemia treatment—a review. Journal of Clinical Medicine. 2023;12(18):5839.
- Alsayed N, et al. Consensus clinical recommendations for the management of plasma lipid disorders in the Middle East: 2021 update. Atherosclerosis. 2022;343:28-50.
- Afosah DK, RA Al-Horani, Sulfated non-saccharide glycosaminoglycan mimetics as novel drug discovery platform for various pathologies. Current medicinal chemistry. 2020;27(21):3412-47.
- Incalza MA, et al. Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases. Vascular pharmacology, 2018. 100: p. 1-19.
- Roy PK, et al. Prospects of potential adipokines as therapeutic agents in obesity-linked atherogenic dyslipidemia and insulin resistance. The Egyptian Heart Journal. 2023;75(1):1-28.
- Milojević A, et al. Effects of Apnea, Obesity, and Statin Therapy on Proprotein Convertase Subtilisin/ Kexin 9 Levels in Patients with Obstructive Sleep Apnea. Medical Principles and Practice. 2022;31(3):293-300.
- Szudzik M, et al. High-fat diet causes hepatic steatosis, increased plasma low-density lipoprotein levels, and alters the PCSK9-lDLR system more pronouncedly than a high-carbohydrates diet in rats. Atherosclerosis. 2023;379:S101.
- Domingo E, et al. Targeting systemic inflammation in metabolic disorders. A therapeutic candidate for the prevention of cardiovascular diseases? Pharmacological Research. 2024. p. 107058.
- Kiyosue A, et al. Safety and Effectiveness of Alirocumab, a Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Inhibitor, in Patients With Familial or Non-Familial Hypercholesterolemia. A Post-Marketing Survey (J-POSSIBLE). Circulation Journal. 2023; 87(6):834-46.
- Rogula S, et al. Inclisiran—Silencing the Cholesterol, Speaking up the Prognosis. Journal of Clinical Medicine. 2021;10(11):2467.
- Lebeau PF, et al. The emerging roles of intracellular PCSK9 and their implications in endoplasmic reticulum stress and metabolic diseases. Metabolites. 2022;12(3):215.
- Abdelwahed KS. Pseurotin a as a Novel PCSK9 Axis Lead Modulator for the Control of Breast and Prostate Malignancy Recurrences. 2021, University of Louisiana at Monroe.
- Yang SH, et al. Plasma PCSK9 level is unrelated to blood pressure and not associated independently with carotid intima–media thickness in hypertensives. Hypertension Research, 2016;39(8):598-605.
- Fairoozy RH. Genetic functional studies of low density lipoprotein-cholesterol (LDL-C) associated variants and the genetic spectrum of familial hypercholesterolemia in different ethnic groups. 2018, UCL (University College London).
- Schlüter KD, et al. Coming back to physiology: extra hepatic functions of proprotein convertase subtilisin/ kexin type 9. Frontiers in Physiology. 2020; 11:598649.
- Li A, et al. Efficacy of oats for dyslipidemia: a systematic review and meta-analysis. Food & Function, 2024.
- Bhatnagar A. Environmental cardiology: studying mechanistic links between pollution and heart disease. Circulation research. 2006;99(7): p. 692-705.
- Laufs U, et al. Clinical review on triglycerides. European heart journal. 2020;41(1):99-109.
- Sawaguchi J, et al., The circulating furin-cleaved/mature PCSK9 ratio has a potential prognostic significance in statin-naïve patients with acute ST elevation myocardial infarction. Atherosclerosis Plus. 2022; 50:50-6.
- Schulz R, et al. Molecular and cellular function of the proprotein convertase subtilisin/kexin type 9 (PCSK9). Basic research in cardiology. 2015;110:1-19.
- Wichaiyo SP, et al. Functional Roles of Furin in Cardio-Cerebrovascular Diseases. ACS Pharmacology & Translational Science. 2023.
- Puri R, et al. Proposed low-density lipoprotein cholesterol goals for secondary prevention and familial hypercholesterolemia in India with focus on PCSK9 inhibitor monoclonal antibodies: Expert consensus statement from Lipid Association of India. Journal of clinical lipidology. 2020;14(2):e1-e13.
- Nussbaumerova B, H Rosolova. Obesity and Dyslipidemia. Current Atherosclerosis Reports. 2023; 25(12):947-55.


