Expansion Capacity of Drug-Eluting Stents in Patients with Left Main Coronary Artery Disease: An Intravascular Ultrasound Guided Study
Автор: Mohamed Mahrous Ali, Basheer Hafez Mohamed, Metwally Hasan El Emary,Ashraf Ahmed Abd Al Mageed
Журнал: Cardiometry @cardiometry
Статья в выпуске: 19, 2021 года.
Бесплатный доступ
Aims: The aim of this study was to assess the expansion capacity of current commercially available Drug Eluting Stents (DES) with nominal diameters of 3.5-4.0mm in patients with Left Main disease. Materials and Methods: This study was conducted on 50 Patients who underwent percutaneous coronary intervention (PCI)for Left Main disease at Benha university hospitals and National Heart Institute. PCI was done with Drug Eluting Stents (DES) with large diameters of 3.5-4mm and post dilatation was done with non-compliant (NC) balloons with diameters of 4.5- 5mm. Intravascular ultrasound (IVUS) was used to measure maximal stent diameter and area. Results: Three commercially available DESs were used in our study; XIENCE Xpeditionᵀᴹ, Ultimasterᵀᴹ and Onyxᵀᴹ. Maximal stent diameter was 4.5±0.3mm and diameter expansion index was 0.96±0.05. Maximal stent area was 14.67±2.06mm² and area expansion index was 0.86±0.07mm². On IVUS images, significantly more calcification< 90 ̊ was detected in the group with expansion index - 0.85 (68.4 percent versus 25.8%, P=0.003) compared to the group with expansion index - 0.85. We found that DESs with diameters of 3.5-4.0mm can be expanded up to diameter of 5.3mm after post-dilation. No complications were reported in the studied patients, including perforation or stent fracture. Conclusion: Current DESs with nominal diameters of 3.5-4.0mm can be safely and effectively over-expanded to reach the predicted diameters in the left main, but the presence of calcification -90 may affect the achievement of the predicted area.
Left Main, Intravascular Ultrasound, Expansion Capacity, Drug Eluting Stents.
Короткий адрес: https://sciup.org/148320560
IDR: 148320560 | DOI: 10.18137/cardiometry.2021.19.117122
Текст научной статьи Expansion Capacity of Drug-Eluting Stents in Patients with Left Main Coronary Artery Disease: An Intravascular Ultrasound Guided Study
Mohamed Mahrous Ali, Basheer Hafez Mohamed,Metwally Hasan El Emary,Ashraf Ahmed Abd Al Mageed. Expansion Capacity of Drug-Eluting Stents in Patients with Left Main Coronary Artery Disease: An Intravascular Ultrasound Guided Study. Cardi-ometry; Issue 19; August 2021; p. 117-122; DOI: 10.18137/cardiom-etry.2021.19.117122; Available from: issues/no19-august-2021/expansion-capacity-of-drug-eluting
Left main disease carries more risk in comparison to other anatomical subtypes of coronary artery disease, it also has a poor prognosis when compared to non-left main disease. [1] . PCI for left main disease were linked to increased rates of acute complications, early mortality and long-term restenosis before the introduction of drug-eluting stents [2-4]. As a result, coronary artery bypass grafting (CABG) was the mainstay revascularization option for Left Main lesions for decades. In patients with Left main disease, when comparing CABG with PCI with DESs, randomized controlled trials and meta-analyses show that the safety composite of myocardial infarction, stroke and death is equal in both groups after five years of follow-up. [5]. PCI is now recommended as an alternate revascularization technique for LMCA lesions with low to intermediate SYNTAX score, according to current European Society of Cardiology guidelines [6]. The large reference diameter of the left main coronary artery in comparison to commercially available DESs, as well as the caliber difference between the LMCA and both left circumflex (LCX) and left anterior descending (LAD) arteries, pose a significant challenge during PCI to the LMCA. Overexpansion of the stent with larger post-dilation balloons is the most effective way to decrease the chance of incomplete stent apposition [7]. Several bench testing and in vitro studies had evaluated the overexpansion capacity of current DES platforms, but in vivo data on this issue is still scarce [8].
Aim of the work:
The aim of this study was to assess the expansion capacity of current commercially available DESs with nominal diameters of 3.5-4.0mm in patients with Left Main disease.
Material and Method:
This was a two-center retrospective study that was conducted at both Benha University hospitals and the National Heart Institute (NHI). All PCIs performed in the period from January 2019 to December 2020 were reviewed to detect Interventions with the following inclusion criteria; Unprotected Left Main Interventions, Interventions in which drug eluting stents with a nominal diameter of 3.5 and 4.0 mm was used, Interventions in which post-dilation was done using noncompliant balloons with a nominal diameter of 4.5 and 5.0 mm and Interventions involving IVUS assessment before stent deployment and after the final post-dilation. Exclusion criteria in this study were; patients presented with STEMI, hemodynamic Instability, angiographically visible thrombus or slow flow.
IVUS Measurements:
IVUS images were obtained using Eagle Eye® Platinum RX Digital IVUS catheter (Philips, San Diego, USA). After injection of 0.1 mg of intracoronary nitroglycerin, images were recorded from LAD or LCX back to LM ostium. Experienced interventional cardiologists reviewed the recorded images. They were blinded to the data of the post-dilation process, including balloon diameter and inflation pressure. Minimal lumen diameter (mm), plaque burden, minimal lumen area (mm2), maximal stent diameter (mm), and maximal stent area (mm2) were all measured. Calcification was quantitatively described according to arc and measured in degrees and expressed as 2 main categories; >90 o and <90 o . The diameter expansion index was calculated by dividing the maximal stent diameter by the predicted post-dilation stent diameter . The area expansion index was calculated by dividing the maximal stent area by the predicted post-dilation stent area. Predicted stent diameter was calculated based on post-dilation balloon diameter and inflation pressure, according to the manufacturers’ information, and predicted stent area was calculated subsequently from predicted stent diameter.
Study End Points:
The Primary End Points: Post intervention diameter expansion index and area expansion index.
The secondary End Points: Post procedural complications and in-hospital death, myocardial infarction or need for revascularization.
Statistical analysis:
SPSS version 25. (IBM, Armonk, New York, United States) was used for data management and statistical. Quantitative data were assessed for normality using Kolmogorov–Smirnov test and direct data visualization methods. Means and standard deviations were used to summarize numerical data. Categorical data were summarized as numbers and percentages. Quantitative data were compared according to the expansion index using independent t-test. The Chi-square test was used to compare categorical data. Correlations were done using Pearson’s correlation. Stepwise logistic regression analysis was done for the prediction of a low expansion index. The odds ratio and the 95% confidence interval were calculated. P values less than 0.05 were considered significant. All statistical tests were two-sided.
Results
This study was conducted on 50 Patients, the mean age of the studied patients was 61±5 years, more than half of the patients (56%) were males, 62.0% were hypertensives, and 30.0% were diabetics. Table 1, describes the demographic data and risk factors of studied patients.
Table 1
Demographic data and risk factors studied patients
|
Age |
Mean ±SD |
61 ±5 |
|
Gender |
Males n (%) |
28 (56.0) |
|
Females n (%) |
22 (44.0) |
|
|
Hypertension |
n (%) |
31 (62.0) |
|
Diabetes mellitus |
n (%) |
15 (30.0) |
|
Smoking |
n (%) |
13 (26.0) |
|
Dyslipidemia |
n (%) |
11 (22.0) |
|
Family history |
n (%) |
10 (20.0) |
Angiography and procedural characteristics:
Most patients underwent angiography due to ACS (82.0%), and majority of patients (82%) showed bifurcation lesions. Table 2, describes angiographic and procedural data in the studied patients.
IVUS characteristics
Minimal Lumen Diameter (MLD) mean was 2.31, Minimal Lumen Area (MLA) mean was 4.27, the mean plaque burden was 70.2% and 42.0% of the studied patients showed calcification > 90%. Maximal stent diameter mean was 4.5mm and maximal stent area mean was and 14.67mm². The mean values of diameter expansion index and area expansion index were 0.96 and 0.86, respectively (Table 3). There was
Table 3
IVUS characteristics in the studied patients
|
MLD |
Mean ±SD |
2.31 ±0.14 |
|
MLA |
Mean ±SD |
4.27 ±0.52 |
|
Plaque burden % |
Mean ±SD |
70.2 ±6.6 |
|
Calcification > 90% |
n (%) |
21 (42.0) |
|
Max stent diameter |
Mean ±SD |
4.5 ±0.3 |
|
Max stent area |
Mean ±SD |
14.67 ±2.06 |
|
Diameter expansion index |
Mean ±SD |
0.96 ±0.05 |
|
Area expansion index |
Mean ±SD |
0.86 ±0.07 |
Table 2
Angiographic and procedural characteristics in the studied patients
|
Indication |
ACS |
n (%) |
41 (82.0) |
|
CCS |
n (%) |
9 (18.0) |
|
|
Lesion site |
Ostium or shaft |
n (%) |
9 (18.0) |
|
Bifurcation |
n (%) |
41 (82.0) |
|
|
Stent length |
Mean ±SD |
29 ±6 |
|
|
DES type |
ONYX |
n (%) |
18 (36.0) |
|
ULTIMASTER |
n (%) |
15 (30.0) |
|
|
EPEDITION |
n (%) |
17 (34.0) |
|
|
Deployment pressure |
Mean ±SD |
14 ±2 |
|
|
Post-dilation balloon diameter |
Mean ±SD |
4.63 ±0.22 |
|
|
Post-dilation balloon inflation pressure |
Mean ±SD |
14 ±2 |
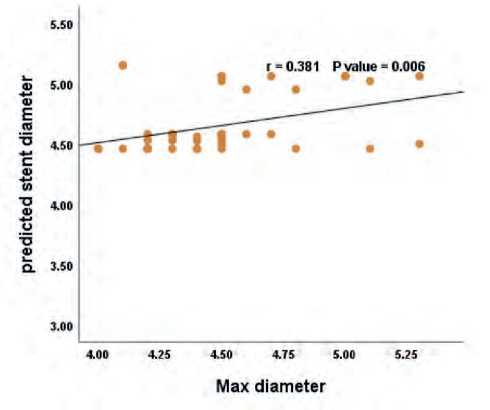
Figure 1. Relationship between predicted stent diameter and maximal stent diameter.
MLD; minimum lumen diameter
There was no significant difference between 3 used DESs types (XIENCE XpeditionTM, UltimasterTM and OnyxTM) as regard maximal stent diameter, maximal stent area, diameter expansion index and area expansion index (Table 4). The 3 used DESs with nominal diameters of 3.5-4.0 mm can be expanded up to diameter of 5.3mm after post-dilation (Figure 3).
Demographic data and risk factors according to area expansion index:
Smoking was significantly higher (42.1%) in those with expansion index < 0.85 than those with expansion in-
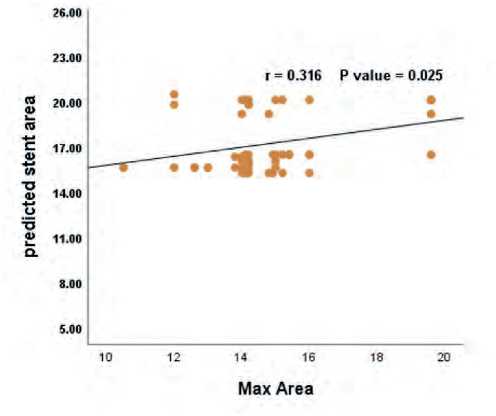
Figure 2. Relationship between predicted stent area and maximal stent area.
Table 4
IVUS measured parameters of 3 different Drug Eluting Stents
|
Stent type |
P-value |
||||
|
Onyx |
Ulti-master |
Xpedi-tion |
|||
|
Max diameter |
Mean ±SD |
4.4 ±0.3 |
4.5 ±0.4 |
4.5 ±0.3 |
0.874 |
|
Max Area |
Mean ±SD |
14.2 ±1.74 |
14.61 ±1.92 |
15.22 ±2.45 |
0.343 |
|
Diameter expansion index |
Mean ±SD |
0.96 ±0.06 |
0.96 ±0.06 |
0.97 ±0.04 |
0.963 |
|
Area expansion index |
Mean ±SD |
0.86 ±0.06 |
0.85 ±0.08 |
0.86 ±0.09 |
0.868 |
One-way ANOVA was used
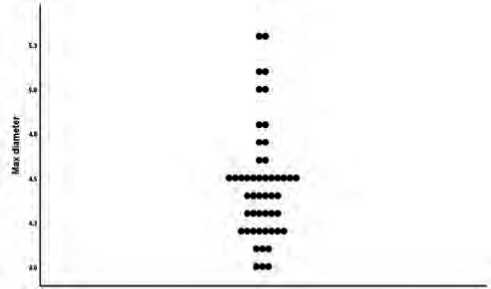
Figure 3. Maximal Stent Diameter as measured by IVUS after post-dilation.
The patients were then categorized into two groups based on their area expansion indices: ≥ 0.85 (n = 31) and ˂ 0.85 (n = 19).
dex ≥ 0.85 (16.1%); P-value was 0.042. No significant differences were observed regarding age, gender, hypertension, diabetes, dyslipidemia and family history (Table 5).
Angiographic and procedural according to area expansion index.
No significant differences were reported regarding indication, lesion site, stent length, DES type, stent deployment pressure, diameter of post-dilation balloon and inflation pressure of post-dilation balloon (Table 6).
IVUS characteristics according to area expansion index
Calcification > 90% was significantly higher (68.4%) in those with expansion index < 0.85 than those with expansion index ≥ 0.85 (25.8%); P-value was 0.003. No significant differences were reported regarding plaque burden, minimal lumen diameter (MLD) and minimal lumen area (MLA) (Table 7).
Predictors of expansion index < 0.85
Stepwise multivariate logistic regression analysis revealed that MLA (OR = 0.138, 95% CI = 0.026-0.725, P-value = 0.019) and calcification > 90% (OR=14.726, 95% CI = 2.789-77.761, P-value = 0.002) were significant predictors for expansion index < 0.85.
Procedural complications and in-hospital outcomes:
No procedural complications, including perforation or stent fracture, no in-hospital death, myocardial infarction, or need for revascularization were reported in the studied patients.
120 | Cardiometry | Issue 19. August 2021
Table 5
Demographic data and risk factors according to expansion index
|
Expansion index |
P-value |
|||
|
≥ 0.85 (n = 31) |
<0.85 (n = 19) |
|||
|
Age |
Mean ±SD |
60 ±5 |
61 ±5 |
0.894 |
|
Gender |
Males n (%) |
17 (54.8) |
11 (57.9) |
0.833 |
|
Females n (%) |
14 (45.2) |
8 (42.1) |
||
|
Hypertension |
n (%) |
21 (67.7) |
10 (52.6) |
0.285 |
|
Diabetes mellitus |
n (%) |
11 (35.5) |
4 (21.1) |
0.28 |
|
Smoking |
n (%) |
5 (16.1) |
8 (42.1) |
0.042 |
|
Dyslipidemia |
n (%) |
8 (25.8) |
3 (15.8) |
0.407 |
|
Family history |
n (%) |
6 (19.4) |
4 (21.1) |
0.884 |
Table 6
Angiographic characteristics according to expansion index
|
Expansion index |
P-value |
||||
|
≥ 0.85 (n = 31) |
<0.85 (n = 19) |
||||
|
Indication |
ACS |
n (%) |
26 (83.9) |
15 (78.9) |
0.66 |
|
CCS |
n (%) |
5 (16.1) |
4 (21.1) |
||
|
Lesion site |
Ostium or shaft |
n (%) |
6 (19.4) |
3 (15.8) |
0.75 |
|
Bifurcation |
n (%) |
25 (80.6) |
16 (84.2) |
||
|
Stent length |
Mean ±SD |
29 ±6 |
28 ±6 |
0.539 |
|
|
DES type |
Onyx |
n (%) |
10 (32.3) |
8 (42.1) |
0.646 |
|
Ulti-master |
n (%) |
9 (29.0) |
6 (31.6) |
||
|
XPEDI-TION |
n (%) |
12 (38.7) |
5 (26.3) |
||
|
Deployment pressure |
Mean ±SD |
14 ±2 |
13 ±1 |
0.075 |
|
|
Post-dilation balloon diameter |
Mean ±SD |
4.65 ±0.23 |
4.61 ±0.21 |
0.529 |
|
|
Post-dilation balloon inflation pressure |
Mean ±SD |
14 ±2 |
13 ±2 |
0.54 |
|
Table 7
IVUS characteristics according to expansion index
|
Expansion index |
P-value |
|||
|
≥ 0.85 (n = 31) |
<0.85 (n = 19) |
|||
|
MLD |
Mean ±SD |
2.33 ±0.12 |
2.29 ±0.16 |
0.338 |
|
MLA |
Mean ±SD |
4.35 ±0.46 |
4.13 ±0.6 |
0.138 |
|
plaque burden (%) |
Mean ±SD |
70.1 ±6.9 |
70.5 ±6.2 |
0.842 |
|
Calcification > 90% |
n (%) |
8 (25.8) |
13 (68.4) |
0.003 |
Independent t-test was used for numerical data. Chi-square test was used for categorical data
MLD; minimum lumen diameter
MLA; minimum lumen area
Discussion
In our study, we aimed to assess the expansion capacity of current commercially available DESs with nominal diameters of 3.5-4.0 mm in patients with Left Main disease. This study revealed that currently available DESs with nominal diameters of 3.5-4.0 mm can be safely and effectively expanded above their nominal diameters to achieve predicted diameters and can be expanded up to diameter of 5.3mm after post-dilation using 5.0 mm non-compliant balloon.
This was in agreement with Jaryl et al., who showed that current DESs can be expanded above their nominal diameters to achieve maximal diameters of up to 5.8mm using a 6.0mm semi-compliant balloon. But this was tested in vitro and did not take into account the interaction between stent and vessel wall nor the plaque composition. Furthermore, the sample size was very small as only one stent of each platform was tested. [9].
This was in agreement with Ye et al. who showed that there was a significant positive correlation between maximal stent diameter and calculated stent diameter (r = 0.718 & P-value = <0.001) and predicted stent area showed a significant positive correlation with maximal stent area (r = 0.562 & P-value = <0.001) [7].
In this study Calcification > 90% was significantly higher (68.4%) in those with expansion index <0.85 than those with expansion index ≥0.85 (25.8%); P-val-ue was 0.003.
This was in agreement with Ye et al. who showed that Calcification > 90% was significantly higher in those with expansion index <0.85 than those with expansion index ≥0.85(72.7%versus 16.7%, P-value = 0.007) [7].
In this study no complications were reported in the studied patients, including perforation or stent fracture. This was in agreement with Ye et al. who reported only one adverse event in the form of acute stent fracture [7].
Conclusion
Current DESs with nominal diameters of 3.54.0mm can be safely and effectively over-expanded to reach the predicted diameters in the left main, but the presence of calcification >90 may affect the achievement of the predicted area.
Limitations:
-
• Small sample size of the study.
-
• Lack of follow up IVUS data of studied patients.
-
• Only 3 current DESs type were tested in this study.
Financial support and sponsorship
Nil
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Expansion Capacity of Drug-Eluting Stents in Patients with Left Main Coronary Artery Disease: An Intravascular Ultrasound Guided Study
- Lee PH, Ahn JM, Chang M, et al. Left main coronary artery disease: Secular trends in patient characteristics, treatments, and outcomes. J Am Coll Cardiol 2016; 68:1233–1246.
- Park SJ, Hong MK, Lee CW, et al. Elective stenting of unprotected left main coronary artery stenosis: Effect of debulking before stenting and intravascular ultrasound guidance. J Am Coll Cardiol 2001; 38: 1054–1060.
- Tan WA, Tamai H, Park SJ, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation 2001; 104: 1609–1614.
- Black A, Cortina R, Bossi I, et al. Unprotected left main coronary artery stenting: Correlates of midterm survival and impact of patient selection. J Am Coll Cardiol 2001; 37: 832–838.
- Giacoppo D, et al. Percutaneous coronary intervention vs coronaryartery bypass grafting in patients with left main coronary artery stenosis: A systematic review and meta-analysis. JAMA Cardiol 2017;2:1079–1088.
- Franz-Josef, Neumann Miguel, Sousa-Uva et al 2018. ESC/EACTS Guidelines on myocardial revascu122 larization. European Heart Journal, Volume 40, Issue 2, 07 January 2019, Pages 87–165.
- Ye Y, Qian H, Yang M, Zhu X, Gan T, Zhang S, Zeng Y. Over-expansion of drug-eluting stents in patients with left main coronary artery disease: An in vivo study. J Int Med Res. 2017 Aug;45(4):1406-1416. doi: 10.1177/0300060517708515. Epub 2017 Jun 12. PMID: 28606023; PMCID: PMC5625525.
- Foin N, Alegria E, Sen S, et al. Importance of knowing stent design threshold diameters and post-dilatation capacities to optimize stent selection and prevent stent overexpansion/incomplete apposition during PCI. Int J Cardiol 2013; 166: 755–758.
- Ng J, Foin N, Ang HY, et al. Overexpansion capacity and stent design model: an update with contemporary des platforms.Int J Cardiol 2016; 221: 171–179.


