Features of the course of cardiovascular diseases against the background of COVID-19
Автор: Betuganova A.T., Notov A.A., Ahkubekova Z.A., Aramisova R.M., Kambachokova Z.A., Shereuzhev T.Kh., Aramisov K.E., Kambachokova A.A.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 21, 2022 года.
Бесплатный доступ
Based on the analysis of 308 electronic medical records of patients with a confirmed diagnosis of a new coronavirus infection COVID-19, the features of the course of cardiovascular diseases at the regional level were studied. It was found that in patients with cardiovascular diseases, the severity of the course and mortality are higher than in patients without cardiac pathology.
Covid-19, сardiovascular diseases, features of the course, treatment
Короткий адрес: https://sciup.org/148323980
IDR: 148323980
Текст научной статьи Features of the course of cardiovascular diseases against the background of COVID-19
Imprint
Albina T. Betuganova, Asker A. Notov, Zuhra A. Ahkubekova, Rina M. Aramisova, Zareta A. Kambachokova*, Timerlan Kh. Shereuzhev, Kantemir E. Aramisov, Amina A. Kambachokova. Features of the course of cardiovascular diseases against the background of covid-19. Cardiometry; Issue 21; February 2022; p. 102-106; DOI: 10.18137/cardiometry.2022.21.102106; Available from: features-course-cardiovascular
Relevance of the problem
The results of studies by researches both in Russia and abroad indicate that damage to the cardiovascular system (CVS) is observed in 20-30% of patients with COVID-19 [1, 2, 3]. The combination of CVD and COVID-19 produces additional difficulties in diagnosing, determining priority tactics and choosing therapy. Along with the direct cardiotropic effect of the SARS-CoV-2 virus, pro-arrhythmic effects of 102 | Cardiometry | Issue 21. February 2022
some drugs used to treat COVID-19 are also possible. For example, it is well known that antiviral drugs have a potential arrhythmogenic effect due to their ability to prolong the QT interval, especially in patients with an initial increase in the QT interval, which increases the risk of arrhythmic death [4,5].
In addition, an increase in the incidence of cardiovascular events after recovery from COVID-19 may also play a role in the increase in mortality [6,7,8].
Despite numerous studies by international and Russian scientists, the problem of cardiovascular diseases against the background of COVID-19 has not been fully studied. There are no convincing data on the impact of individual factors on survival and longterm life prognosis. In particular, the extent and nature of the MTR burden in this population is not fully understood and remains open.
The situation is complicated by a lack of information, a significant volume of contradictory publications on this issue, and the importance of information for clinical practice. The available information currently consists of an analysis of small observational studies, speculations about possible mechanisms of the pathological impact of the infection on the cardiovascular system, and prospects for treatment and prevention [9, 10].
Further improving the effectiveness of medical care for patients with COVID-19 at the present stage is one of the important tasks. Therefore, the study of regional features of the course of cardiovascular pathology will contribute to improving the quality and effectiveness of medical care for patients with CVD in the context of SARS-CoV-2 infection, both at the hospital stage and in the post-COVID period.
Material and methods
The study is based on the results of a retrospective analysis of electronic medical records of 308 patients with verified diagnosis of COVID-19 (51.9% men, 48.1% women).
From 14.04.2020 till 31.03.2021, 6 541 people were admitted to the hospital of especially dangerous infections No. 2 in Nalchik, among them 477 people died (7.3%). All patients included in the study were divided into 2 groups: the first group (n=182) consisted of patients with CVD, the second the patients (n=126) without CVD.
SARS-CoV-2 infection was determined by polymerase chain reaction (RT-PCR) using the CoV-2 Test kit. Clinical and laboratory examination was carried out in accordance with medical and economic standards using standard methods by qualified laboratory specialists. In addition, the QT interval was analyzed and monitored, especially in the case of QT-prolonging interval therapy.
Research results
The structure of CVD and COVID in the COVID-19 patients is shown in Figure 1 herein.
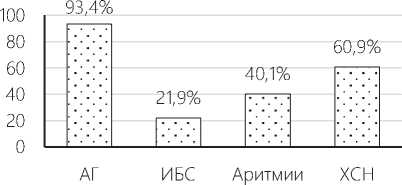
Figure 1. Structure of CVD in COVID patients (n=182)
Arterial hypertension (AH) was most often detected among COVID-19 patients, which was recorded in 93.4% of the patients, and 66.5% had grade 3 hyperten- sion. On the 2nd place there was recorded chronic heart failure (CHF) (60.9%), and on the 3rd reported were cardiac arrhythmias (40.1%). Ischemic heart disease (CHD) was observed in 21.9% of the patients, post-infarction cardiosclerosis was recorded in 10.4% of cases.
Our analysis of the severity of COVID-19 revealed the following: moderate course was observed in 112 (36.4%), severe – in 88 (28.5%) and extremely severe – in 108 (35.1%) patients. There were statistically significant differences in the severity of infection depending on the duration of hospitalization (Table 1).
The table given herein shows that mortality was higher in the group of patients admitted to the hospital (n=112) on day 5-7 of illness (59.8%). The second group in terms of mortality was the group of patients admitted on day 8 or later (n=149) (47.6%). A favorable course was observed among patients admitted at an earlier stage of the disease (63.8%). The structure of patients with complications was dominated by patients hospitalized at a later stage of the disease in 84.8-90.6% of the cases (Table 2).
Table 1
Features of the course depending on the terms of hospitalization
|
Sign |
1-3 days from the day of the disease (n=47) |
5-7 days from the day of the disease (n=112) |
8 or more days from the day of the disease (n=149) |
P1 (1-3 days and 5-7 days) |
P2 (1-3 days and 8 or more days |
P3 (5-7 days and 8 or more days) |
|
Bed-day |
14.7 |
13.3 |
13.3,3 |
|||
|
Recovery |
5 (10,6%) |
9 (8,0%) |
9 (6,0%) |
|||
|
Improvement |
30 (63,8%) |
36 (32,1%) |
68 (45,6%) |
<0.01 |
<0.01 |
<0.01 |
|
Death |
12 (25,5%) |
67 (59,8%) |
71 (47,6%) |
<0.01 |
<0.01 |
<0.01 |
|
Complications |
36 (76,6%) |
95 (84,8%) |
135 (90,6%) |
<0.01 |
<0.01 |
<0.001 |
Table 2
Correlation between the severity of COVID-19 and the presence of cardiovascular pathology
|
Indicators |
of hypertension |
AH+CHD |
CHD |
P1 (AH and AH+CHD) |
P2 (HYPERTENSION and CHD) |
P3 (AH+CHD and CHD) |
|
Age |
group 68.5±1.03 |
72.1±1.7 |
70.4±2.2 |
<0.01 |
||
|
Bed-day |
13.7±0.7 |
12.4±1.7 |
11.7±2.7 |
|||
|
Fever |
37.7±0.3 |
39.4±2.3 |
37.1±0.2 |
<0.05 |
||
|
NPV |
24.2±0.7 |
23.6±0.6 |
23.3±0.7 |
|||
|
SPO2 |
88.5±0.5 |
88.8±1.2 |
91.8±1.3 |
<0.01 |
<0.05 |
|
|
pulse |
88.5±1.2 |
85±2.1 |
86.2±3.9 |
|||
|
CRP |
55.7±2.3 |
85.5±21.7 |
70.3±8.1 |
<0.05 |
||
|
Procalcitonin |
15 (10.6%) |
1 (3.4%) |
3 (25%) |
<0.05 |
||
|
LDH |
342.2±16.1 |
358.1±311.2 |
474±56.8 |
<0.05 |
<0.001 |
<0.05 |
|
Ferritin |
588.2±24.6 |
664.4±65.3 |
831±71.4 |
<0.05 |
<0.01 |
|
|
IL-6 |
179.3±12.5 |
172.1±21.1 |
267.0±12.2 |
<0.05 |
||
|
D-dimer |
260.7±39.6 |
385.2±87.7 |
1182±41.2 |
<0.05 |
<0.01 |
<0.01 |
|
CT scan at admission |
43.9±1.7 |
42.5±3.5 |
38.5±5.0 |
|||
|
Dynamic CT |
61.3±2.2 |
70.0±4.7 |
68.7±6.7 |
|||
|
Complications |
131 (92.9) |
28 (96.6%) |
12 (100%) |
As can be seen from the table, there is a significant correlation between the presence of CVD and the severity of the disease in patients with COVID-19. Moreover, in patients of older age categories, these connections are more pronounced. Particular attention should be drawn to a more pronounced increase in inflammatory markers in patients with AH and AH+CHD (Table 3).
Table 3
Comparative analysis of inflammatory markers and blood coagulation parameters in the study groups
|
indicators |
Group 1 group |
2 |
p |
|
CRP |
61.5±3.9 |
52.2±3.2 |
<0.05 |
|
Procalcitonin |
19 (10.4%) |
5 (3.9%) |
<0.01 |
|
LDH |
353.5±14.1 |
294.5±17.4 |
<0.05 |
|
Ferritin |
616.3±24.7 |
425.6±23.1 |
<0.001 |
|
IL-6 |
183,9±11,9 |
82,8±10,4 |
<0.001 |
|
PTI |
94.5±4.8 |
92.7±1.1 |
|
|
INR |
1.2±0.03 |
3.5±1.4 |
|
|
APTT |
27.4±0.7 |
23.9±0.6 |
|
|
D-dimer |
341.3±45.8 |
80.8±26.1 |
< 0.05 |
|
Fibrinogen |
519.9±24.3 |
526.5±19.3 |
It was found that in patients with CVD, the level of inflammatory markers and the tendency to hypercoagulability were significantly higher.
The results of the comparative analysis of the frequency and structure of complications in the study groups are presented in Table 4 herein.
Table 4
Structure of complications in patients with COVID-19
|
Complication |
Group 1 n=182 |
Group 2 n=126 |
P |
|
Rhythm disorders |
49 (26,9%) |
58 (46,0%) |
<0.001 |
|
Conduction |
59 (32,4%) |
16 (12,7%) |
<0.001 |
|
RF 1 |
15 (8,2%) |
31 (24.6 per cent) |
<0.001 |
|
RF 2 |
33 (18,1%) |
35 (27.8 per cent) |
<0.01 |
|
RF 3 |
89 (48,9%) |
21 (16.7%) are |
<0.001 |
|
tela |
66 (36,3%) |
7 (5.6%)of |
<0.001 |
|
SD |
Card Holder 19 (10,4%) |
8 (6,3%) |
|
|
TO THEM |
13 (7,1%) |
2 (1,6%) |
|
|
ONMK |
9 (4,9%) |
2 (1,6%) |
|
|
Sepsis |
18 (9,9%) |
2 (1,6%) |
<0.05 |
|
Complication |
Group 1 n=182 |
Group 2 n=126 |
P |
|
Emergency call |
center 26 (14,3%) |
7 (5,6%) |
<0.05 |
|
ARDS |
38 (20,9%) |
4 (3,2%) |
<0.05 |
|
Pneumothorax |
7 (3,8%) |
4 (3,2%) |
|
|
Hydropericard |
23 (12,6%) |
3 (2,4%) |
<0.05 |
|
Pneumomediastenum |
0 (0%) |
1 (0,8%) |
|
|
Acute thrombosis of the lower extremities |
2 (1,1%) |
2 (1,6%) |
The table shows that the patients with CVD were significantly more likely to have more severe complications (stage 3 RF (48.9%), PE (36.3%), ARDS (20.9%), DM (10.4%)). compared to those in group 2 of the study. Conduction disturbances and RF of the 3rd degree were observed 3 times more often in patients of the 1st group than in the 2nd, PE more than 5 times, MI 4.5 times, sepsis 8 times, hydropericardia 7 times.
Given that the female sex prevailed in the structure of patients, the gender features of the COVID-19 course were studied. The results are shown in Table 5.
Table 5
Gender features of the COVID-19 course
|
Indicators |
Men (n=143) |
Women (n=165) |
p |
|
Age |
63.6±1.9 |
64.2±1.2 |
|
|
Bed-day |
13.6±0.6 |
13.5±0.7 |
|
|
Temperature |
38.2±0.5 |
38.2±0.5 |
|
|
BPD |
23.5±0.6 |
23.0±0.4 |
|
|
GARDEN |
131.2±23.1 |
133.9±2.4 |
|
|
dad |
79.9±11.9 |
81.3±7.2 |
|
|
SPO2 |
89,3±0,5 |
89,3±0,4 |
|
|
pulse |
of 87.9±1,1 |
89,2±1,1 |
|
|
SRB |
63,9±5,0 |
56,0±2,5 |
0.05 |
|
LDH |
333,9±16,8 |
325±14,6 |
|
|
Ferritin |
585,7±9,5 |
497±21,8 |
<0.01 |
|
IL-6 |
162,9±14,1 |
124,9±10,5 |
<0.02 |
|
D-dimer |
reached 360.3±56,8 |
125,9±23,7 |
<0.01 |
|
Fibrinogen |
508,1±16,6 |
534,9±6,8 |
|
|
CT scan at admission |
39.1±1.5 |
41.9±1.5 |
|
|
Dynamic CT |
59.3±2.3 |
48.7±2.3 |
<0.001 |
|
Complications |
130 (90.9%) |
135 (81.8%) |
<0.05 |
|
Improvement |
of 52 (36.4%) |
83 (50.3%) |
<0.05 |
|
Recovery |
7 (4.9%) |
16 (9.7%) |
|
|
Fatality rate |
84 (58.7%) |
66 (40%) |
<0.05 |
There were no significant differences in age, body temperature, saturation, BMI, and bed days among men and women. However, the indicators of inflammatory markers were higher in men. Significant deterioration in lung CT parameters was also observed among males. Although the number of complications was dominated by women, the outcomes were more severe among men: improvement was observed in 36.4% of the cases among men, and in 50.3% among women. The mortality rate among men was 58.7%, among women-40%.
Our analysis to study hospital mortality from COVID-19 included 150 deaths (66 (44%) women, mean age 50 ± 19.5 years, 84 men (56%), mean age 50 ± 19.4). The age structure of the deceased was dominated by people aged 60-69 years with predominance of males, and in the age group of 70-79 years women. Among people 80 years and older, there were 2 times more men than women. The structure of causes of death is shown in Table 6 herein.
Table 6
Structure of causes of death
|
Complications |
Total patients |
% (n=150) |
|
Pulmonary embolism |
66 |
44 |
|
Acute respiratory distress syndrome |
33 |
22 |
|
Myocarditis |
8 |
5,3 |
|
Hydropericard |
24 |
16 |
|
Acute cerebrovascular |
accident 10 |
6.6 |
|
Myocardial infarction |
12 |
8 |
|
Acute kidney injury |
31 |
20.6 |
|
Diabetes mellitus |
15 |
10 |
|
Sepsis |
16 |
10.6 |
|
Pneumothorax |
8 |
5,3 |
|
Pneumomediastinum |
1 |
0,6 |
As can be seen from the Table, the structure of causes of death was dominated by pulmonary embolism (44%), acute respiratory distress syndrome (22%), acute kidney injury-20.6%, hydropericardia-16%, sepsis-10.6%, pneumothorax-5.3%. These indicators differ from the results of studies by other authors that again confirms the importance of studying the regional features of the course of COVID-19.
Conclusions
-
1. Study of the prevalence of cardiovascular diseases among the studied population of patients with COVID-19 showed: arterial hypertension was re-
- corded in 93.4% of the patients, chronic heart failure in 60.9% of the cases, cardiac arrhythmias-in 40.1% of the cases, coronary heart disease in 21.9% of the patients, post-infarction cardiosclerosis in 10.4% of the cases.
-
2. A clear dependence of the severity of the course and outcome of the disease on the time of hospitalization was revealed: a favorable course was noted among patients admitted at an earlier stage of the disease. Among patients with severe complications, the patients who were hospitalized at a later stage of the disease prevailed.
-
3. In patients with CVD, the level of inflammatory markers and the tendency to hypercoagulability were significantly higher.
-
4. In patients with CVD, an unfavorable course of-COVID-19 was observed with a large number of complications: cardiac arrhythmias and respiratory failure of 3 degrees were observed 3 times more often than in patients without CVD, PE-more than 5 times, MI-4.5 times, sepsis-8 times, hydropericardia-7 times.
-
5. Gender differences in the course and outcomes of-COVID-19 were revealed: the severity of the course and mortality rates were higher among males.
-
6. CVD and its complications, such as hypertension, CHD, CHF, cardiac arrhythmias, PE, and brain strokes, made the greatest contribution to the structure of causes of hospital mortality.
Practical recommendations
-
1. Data on the prevalence of CVD and its complications among patients with COVID-19 were presented to the Practical Healthcare Department of the Kabardino-Balkar Republic. The analysis performed was carried out in one hospital serving most of the urban population and districts of the republic, so the results obtained cannot be extrapolated to patients with COVID-19 throughout the republic.
-
2. The results obtained will allow optimizing the tactics of providing medical care to patients with CVD during the COVID-19 pandemic and can be used in developing prevention programs and improving the rehabilitation of patients in the post-COVID-19 period.
-
3. The high frequency of thromboembolic complications may be related to the low adherence of patients to anticoagulants in the presence of atrial
Issue 21. February 2022 | Cardiometry | 105
-
4. The results obtained, which indicate the presence of regional features of the prevalence and course of CVD in patients with COVID-19, should be taken into account when planning rehabilitation measures both at the hospital stage and at the postcovid rehabilitation stage.
-
5. Further improving the effectiveness of medical care for patients with COVID-19 at the present stage is one of the most important tasks. Therefore, the study of regional features of the course and treatment of cardiovascular pathology will help reduce the mortality of this category of patients.
fibrillation and other indicated cases in the pre-COVID-19 period, and therefore it is necessary to increase the effectiveness of dispensary monitoring of patients with atrial fibrillation (open offices of patients with AF in polyclinics).
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Features of the course of cardiovascular diseases against the background of COVID-19
- Bazdyrev ED. Coronavirus infection - an actual problem of the XXI century. Complex problems of cardiovascular diseases. 2020; 9(2):6-16.
- DOI: 10.17802/2306-1278-2020-9-2-6-16 EDN: PDLBHI
- Barbarash OL, Karetnikova VN, Kashtalap VV, et al. New coronavirus disease (covid-19) and cardiovascular diseases. Complex problems of cardiovascular diseases. 2020;2:17-28.
- Belenkov Yu. N., Snezhitsky V. A., Ardashev A.V. Et al. Recommendations of the Eurasian Arrhythmological Association (EURA) for the diagnosis and treatment of patients with cardiac arrhythmia and conduction disorders during the COVID-19 pandemic. Cardiology. 2020;60(5):4-8.
- EDN: NTZBSG
- Grinevich VB, Gubonina IV, Doschitsin VL, et al. Features of management of comorbid patients during the new coronavirus infection (covid-19) pandemic Cardiovascular therapy and prevention. 2020;19(4):135-72.
- EDN: YFTNJR
- Polonskaya YV, Kashtanova EV, Stakhneva EM, et al. Covid-19 and cardiovascular diseases. Atherosclerosis. 2020;16(2):73-9.
- Chazova IE, Mironova OYu. COVID-19 and cardiovascular diseases. Therapeutic Archive. 2020;9:4-7.
- EDN: FQHMYD
- Shlyakhto EV, Konradi AO, Villevalde SV. Guidelines for the diagnosis and treatment of circulatory system diseases in the context of the COVID-19 pandemic. Russian Journal of Cardiology. 2020, pp. 129-148.
- Yavelov IS. Covid-19 and cardioVascular Diseases. International Journal of Heart and Vascular Diseases. 2020;8(27):4-13.
- Guo T, Fan Y, Chen M, et al. Association of cardiovascular disease and myocardial injury with outcomes of patients hospitalized with 2019-coronavirus disease (COVID-19). JAMA Cardiol. Published online March 27, 2020.
- DOI: 10.1001/jamacardio.2020.1017
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. Published online March 27, 2020. 10.1001/ jamacardio.2020.1286.
- DOI: 10.1001/jamacardio.2020.1286 EDN: AWPXYT


