Four secondary malignancies, coronary artery disease, aortic atherosclerosis and severe constrictive pericarditis in a survivor of Hodgkin lymphoma treated with radiation therapy: a case report
Автор: Jeri-yabar A., Garazatua-gonzalez J., Montoya-rivera W., Ortuzar-seminario V., Lozada Zingoni C., Massuco V.
Журнал: Сибирский онкологический журнал @siboncoj
Рубрика: Случай из клинической практики
Статья в выпуске: 1 т.22, 2023 года.
Бесплатный доступ
Introduction. Radiation therapy (RT) has been widely used since the 1970s in the treatment of Hodgkin’s lymphoma. RT increases the risk of secondary malignancies and heart disease including coronary artery disease, noncoronary atherosclerotic valvular disease, valvular dysfunction, pericardial disease and radiation induced vasculopathy. Case Presentation. We describe a case of a patient with 4 secondary malignancies due to previous RT including parotid mucoepidermoid carcinoma, breast multicentric infiltrating ducta, thyroid papillary microcarcinoma with follicular pattern and lung adenocarcinoma that later presented with severe constrictive pericarditis, which led to an emergency pericardiectomy - all of these were complications of her previous radiotherapy. She received a prompt diagnosis and treatment. Discussion. Radiation-induced vascular disease (RIVD) occurs due to endothelial injury following RT; patients have up to 3-4 fold increase in risk of myocardial infarction due to CAD, therefore screening of CAD with a CT coronary angiography is recommended to begin 5 years after receiving RT in patients 45 and older and 10 years after RT in patients
Radiation therapy, radiation pericarditis, secondary malignancies
Короткий адрес: https://sciup.org/140297840
IDR: 140297840 | УДК: 616-006.441-08:615.849.1]-06:616.12 | DOI: 10.21294/1814-4861-2023-22-1-159-165
Текст научной статьи Four secondary malignancies, coronary artery disease, aortic atherosclerosis and severe constrictive pericarditis in a survivor of Hodgkin lymphoma treated with radiation therapy: a case report
During the 1970’s, 60Co radiation was the mainstay treatment in Hodgkin’s lymphoma (HL) for its promising results and cure rate [1]. Nevertheless, 10 to 20 years later 60Co radiation concerning side effects were discovered such as secondary cancers and cardiac toxicity and are still being experienced in survivors.
In the field of radiotherapy, radiation dose is measured in Gray units (Gy) where 1 Gy is the absorption of 1J of ionizing radiation energy by 1 Kg of tissue [2]; it’s described that low doses of radiotherapy (<2 Gy) have been shown to be associated with both secondary cancers and a bit of cardiac toxicity, but true heart damage occurs with radiation dose above 30 Gy [2, 3]. In a hybrid phantom Monte Carlo-based method for historical reconstruction of organ doses in patients treated with 60Co for HL, it was shown that out-fielddoses were 38 % on average. Also, distances of 60 cm from the central axis of treatment fields were reported increasing the risk for second malignancies [3].
Among the cardiac toxicities associated with HL treated with radiation therapy (RT) are coronary artery disease, noncoronary atherosclerotic valvular disease, valvular dysfunction, pericardial disease, cardiomyopathy and radiation induced vasculopathy; these are usually observed from 5 to 35 years after therapy on average [2, 4]. Furthermore, the risk of a second malignancy peaks at 35 years after HL radiation treatment. These second malignancies are mostly solid tumors such as cancers of the lung, esophagus, mouth and pharynx, thyroid, stomach and breast [5]. Cardiovascular disease and second malignancies are the leading causes of death in these patients.
Herein, we present a case of a 58-year-old patient who received Cobalt-60 RT for HL at 13 years old and has since battled four different primary neoplasia and now a severe constrictive pericarditis and coronary heart disease.
Case Presentation
A 58-year-old woman from Lima – Perú was admitted to the Internal Medicine ward for presenting a 15-day history of shortness of breath associated with fatigue, palpitations and dry cough.
Her past medical history was significant for Hodgkin lymphoma treated with 60Co radiotherapy in 1977, parotid mucoepidermoid carcinoma treated with parotidectomy in 2000, breast multicentric infiltrating ductal carcinoma treated with mastectomy in 2003, thyroid papillary microcarcinoma with follicular pattern treated with total thyroidectomy in 2010, and lung adenocarcinoma treated with a lobectomy in 2019 with a negative genetic mutation test.
On physical examination, her pulse was 77 bpm, 19 rpm, oxygen saturation was 97 % with 2L of oxygen via nasal cannula. During lung examination, there were diminished breath sounds more prominently in the lower left hemithorax along with diffuse crackles. No intercostal retractions were seen. Cardiac examination was positive for a prominent Kussmaul sign, pericardial friction rub and the cardiac sounds had decreased intensity. The patient also had a bilateral lower limb edema. The rest of the physical exam was within normal limits.
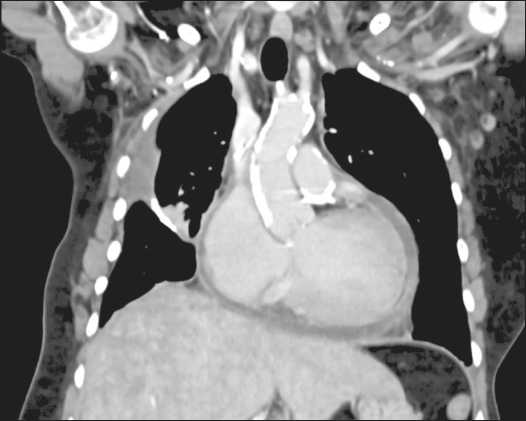
Fig. 1. Chest CT showing cardiomegaly, pleural and pericardial effusion, and atheromatosis of the thoracic and coronary arteries Рис. 1. КТ грудной клетки. Кардиомегалия, плевральный и перикардиальный выпот, атероматоз грудных и коронарных артерий
Due to the shortness of breath, a chest CT was requested and showed cardiomegaly, pericardial effusion, atheromatosis of the thoracic aorta and coronary arteries, alongside with bilateral pleural effusion being more notorious on the left side (Fig. 1). A CT angiography showed no evidence of pulmonary embolism.
A pleural ultrasound showed 500cc of left echogenic pleural effusion and a thoracocentesis was done. The pleural liquid was turbulent and semi-hematic (Table). It was sent for biochemical and pathology testing. Light’s criteria were met, and the fluid was categorized as an exudative effusion. The cytological report later showed no evidence of malignant neoplasia. Laboratory exams showed a Pro-BNP of 1369 pg/ml, D dimer 3.77 ug/ml, moderate anemia (9.4 g/dL).
Oxygen therapy was begun, and she was started on enoxaparin, atorvastatin and furosemide. A cardiology consultation was made, and an echocardiography was done which showed severe pulmonary hypertension (80mmHg) a thickened pericardium, along with mild right atrial enlargement and tricuspid and aortic valve insufficiency (Fig. 2) A cardiac MRI was taken and showed a thickened pericardium with a pericardial effusion (Fig. 3).
A cardiac catheterization finally made the confirmative diagnosis of constrictive pericarditis by showing right atrial hypertension with a sharp X and Y wave decrease (“W” image), the “square root sign” (dip plateau) with increased diastolic pressure “Kussmaul sign” with decrease in systolic LV pressure in inspiration associated with no variation of RA and enhanced ventricular interdependence (Fig. 4); the procedure also showed ostial occlusion (60–70 %) of the circumflex artery and a total occlusive on of the right coronary artery. Besides, severe pulmonary hypertension was confirmed.
The cardiothoracic team was then consulted and recommended an emergency pericardiectomy. The patient then presented with acute kidney injury due probable cardiorenal syndrome and was admitted to the Intensive Care Unit, where she was stabilized. The patient and her family finally accepted the surgical intervention and anterior pericardiectomy was made. After 2 weeks, the patient was discharged without complications.
table/Таблица
Pleural effusion results
Результаты плеврального выпота
|
Test/Тест |
Pleural liquid/ Плевральная жидкость |
Serum/Сыворотка |
|
Protein/Белок |
352 g/dL (NR: 0–3.0) |
8.17 g/dL (NR: 6.40–8.30) |
|
LDH/ЛДГ |
281.6 U/L (NR: 125–333) |
331 U/L (NR: 135-214) |
|
Glucose/Глюкоза |
124 mg/dL (NR: 70–110) |
89 (NR: 70–100) |
|
Red blood cells/Эритроциты |
110,000/mm3 (NR: 0–400) |
– |
|
ADA |
11.67 U/L (NR: 0–45) |
– |
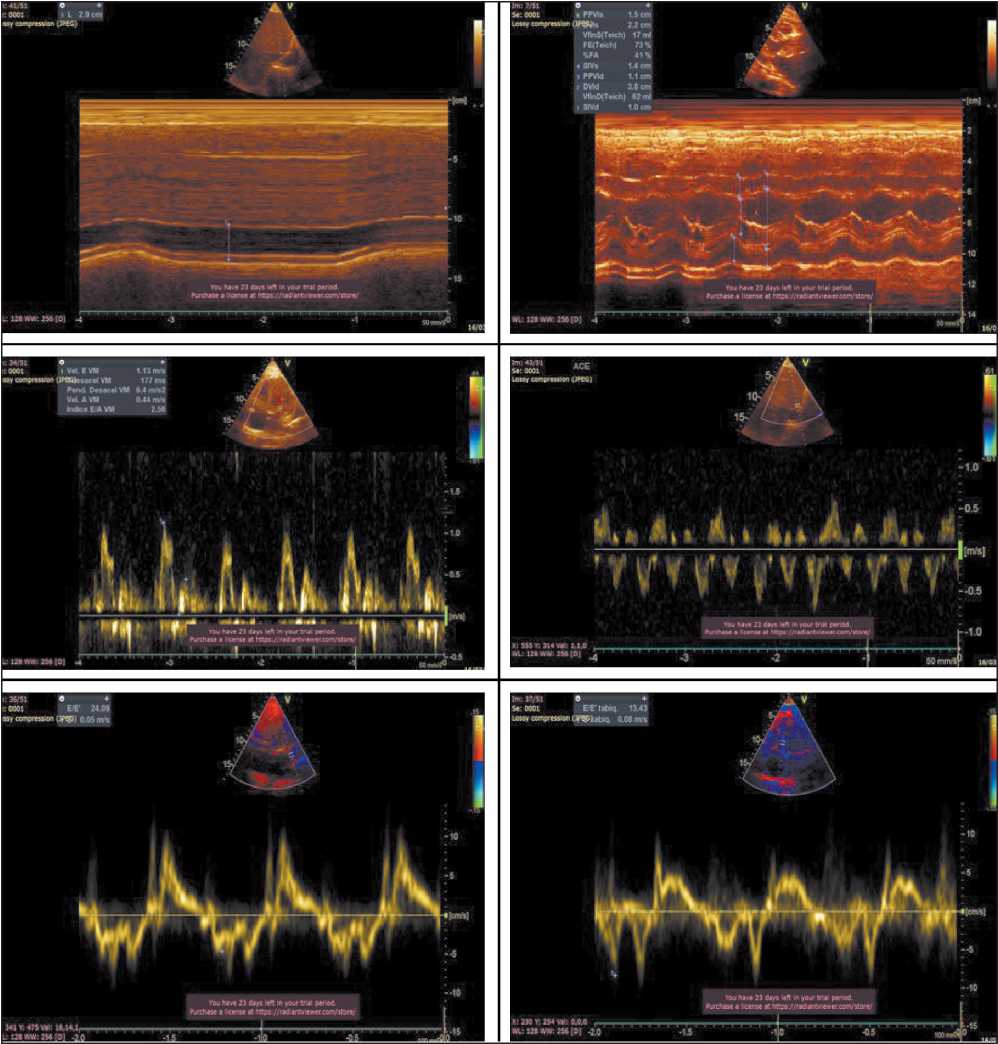
Fig. 2. (A) Dilatated Inferior Vena Cava without inspiratory collapse;
-
(B) interventricular septum with paradoxical movement; (C) Negative flow in pulsed doppler of suprahepatic veins; (D) Variation of mitral diastolic filling rates; (E & F) Lateral tissue doppler with velocity less than medial Рис. 2. (А) Расширенная нижняя полая вена без инспираторного коллапса;
-
(B) Межжелудочковая перегородка с парадоксальным движением;
-
(C) Отрицательный поток в импульсной допплерографии надпеченочных вен; (D) Варьирование скоростей митрального диастолического наполнения;
(E, F) Латеральная допплерография тканей со скоростью меньше медиальной
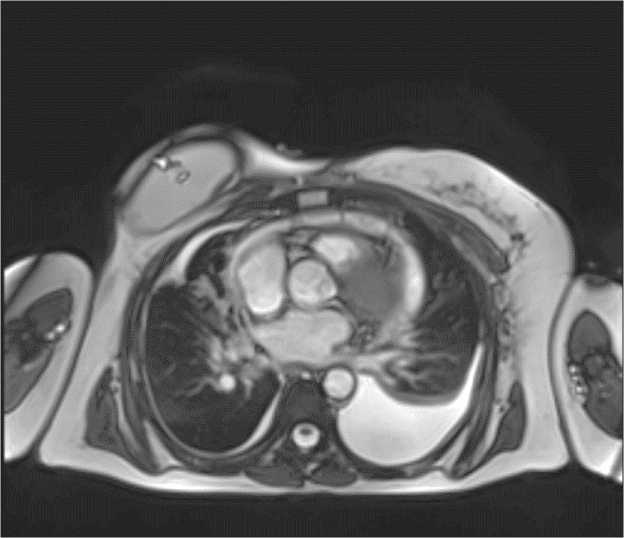
Fig. 3. Cardiac MRI T2 showing increased pericardial thickness, pericardial effusion and bilateral pleural effusion predominantly in left hemithorax
Рис. 3. МРТ сердца Т2. Утолщение перикарда, перикардиальный выпот и двусторонний плеврит, с большим объемом выпота в левом гемитораксе
Discussion
In this patient, three major complications of RT presented simultaneously: radiation-induced vascular disease, four different primary neoplasia, and severe constrictive pericarditis. Radiation-induced vascular disease (RIVD) occurs due to direct endothelial injury following RT. HL survivors that were exposed to RT alone or in combination with chemotherapy, have up to 3–4 fold increase in risk of myocardial infarction due to coronary artery disease (CAD), and this increases if irradiation has been taken before 21 years old [6]. Due to this risk, screening of CAD with a CT coronary angiography is recommended to begin 5 years after receiving RT in patients 45 and older, and 10 years after RT in patients less than 45 years old [7]. Prevention of RIVD consists of a strict control of radiation intensity, breathholding, image guided radiation therapy for minimal radiation to other healthy tissue. Statin therapy during RT has shown promising results in in-vitro studies, due to having anti-inflammatory and anti-thrombotic effects on irradiated endothelial cells [7].
Radiation induced secondary malignancies (RISM) are seen in 17–19 % of cases years after RT and the risk increases by time [8]. Many factors contribute to the risk severity of developing RISM such as age of radiation, dosage and size of the area irradiated, and radiation technique. Lung and breast cancer are the most common forms of second malignancy, as well as thyroid cancer, all of which presented in our patient at different times with different histology. To our knowledge, only a few malignant parotid tumors following RT have been reported and it is most likely due to the mantle field radiation used in the 1970’s, when our patient was treated. As of today, this radiation technique is barely used since more precise techniques have been developed. Fortunately, due to excellent screening and follow ups after RT, the malignant neoplasia were found in early stages where surgery was the only treatment.
The most severe complication found in our patient was constrictive pericarditis, which presented several diagnostic findings in: Echocardiography, Computer Tomography, Cardiac MRI and Hemodynamic catheterization. In the echocardiographic criteria our patient had an inspiration-related ventricular septal shift to the left (best assessed with a combination of 2-dimensional and M mode assessment) which is the most important finding with a sensitivity of 93 % [9], to explain this it’s important to understand that normally during inspiration a negative intrathoracic pressure is created and stimulates the venous return which increases RV filling, but during inspiration in CP the right ventricle can’t expand as usual because of the rigid pericardium, this leads to an interventricular shift to the left because the septum is the only part that is not compromised by the rigid pericardium [10]; the presence of this finding in combination with a medial mitral e’ velocity of ≥9cm/s or a hepatic vein expiratory diastolic flow reversal ratio of ≥ 0.79 is 87 % sensitive and 91 % specific for CP according to the Mayo Clinic Criteria [11].
The CT scan findings that suggest CP are pericardial thickening or calcification with deformation of the cardiac contour or dilatation of the inferior vena cava. Meanwhile the cardiac MRI provides more specific cardiac characterization such as pericardial thickening or peri-myocardial adherence, late gadolinium pericardial enhancement (this occurs because of fibroblast proliferation and neovascularization) and also can be seen the same respiration- related ventricular shift described previously [9].
The gold standard diagnostic test for CP is cardiac catheterism [9], this shows the rise of diastolic pressure in the four cardiac chambers and the pressure between both ventricles was <5 mmHg. Also, once the ventricular volume reaches the limit imposed by the rigid pericardium, suddenly the cardiac chamber’s filling stops and this is presented by the “Dip Plateau” sign. Nevertheless, the most important hemodynamic characteristic in CP is the enhanced ventricular interdependence during breathing [10].
Heart radiation can cause significant pericardial disease which presents as pericardial calcifications, thickening and effusions sometimes found incidentally on imaging. The presentation of constrictive pericarditis decades after RT presents with congestive heart failure and is treated with conventional medications such as diuretics and ACE inhibitors. Furosemide was initiated in our patient which initially decreased her shortness of breath.
The definite treatment for constrictive pericarditis is pericardiectomy, however the operative mortality risk ranges between 5–20 % [12], and when the etiology is secondary to RT, is associated with a poor overall survival even following surgery (about 27 % at 7 years) [2, 13], this is also reported by Tzani et. al. when their meta analysis showed higher mortality rates after peri-cardiectomy in this kind of patients [14].
Minimizing radiation delivery to cardiovascular structures and healthy organs should be prioritized; protocols have been created for new radiation delivery techniques and have reduced ionizing radiation to nontarget structures without the compromise of a state-of-the-art cancer therapy and outcomes regarding cancer care [15]. Although the risk is becoming
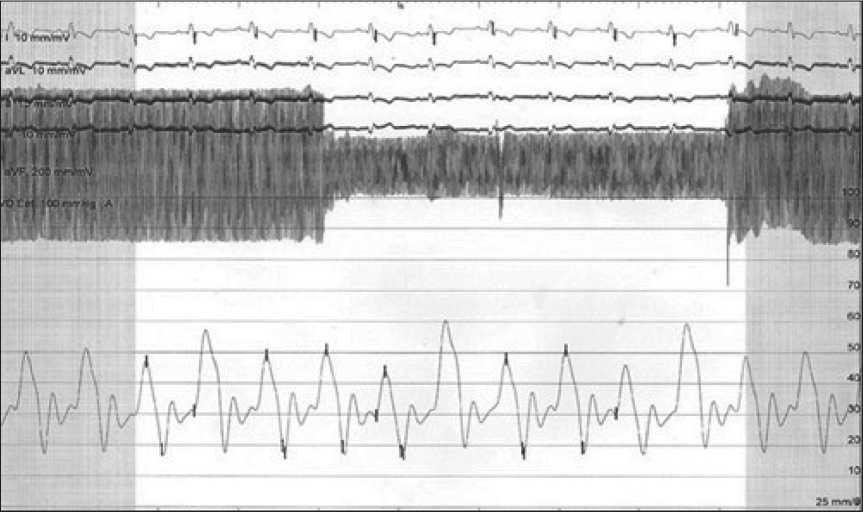
Fig. 4. Right Ventricle. End Diastolic pressure/End systolic pressure Ratio: >⅓ (7/10). RV diastolic curve: “Square root” sign ( Dip Plateau ), diastolic pressures (initial/end) increased Рис. 4. Правый желудочек.
Соотношение конечного диастолического давления/ конечного систолического давления: >⅓ (7/10). Диастолическая кривая ПЖ: признак «квадратный корень» ( Dip Plateau ); диастолическое давление (начальное/конечное) повышено
less prominent because of novel radiation techniques, screening of CV disease should be emphasized as part of the follow-up of cancer patients who have received RT in their lifetime. Furthermore, although pericardial disease is decreasing its incidence following new RT techniques, many patients who were treated between the 1970–1980’s are now facing the devastating side effects of prior RT and should be carefully screened for cardiovascular disease and second malignancies to guarantee a prompt treatment.
Список литературы Four secondary malignancies, coronary artery disease, aortic atherosclerosis and severe constrictive pericarditis in a survivor of Hodgkin lymphoma treated with radiation therapy: a case report
- Svahn-Tapper G., Landberg T. Mantle treatment of Hodgkin’s disease with cobalt 60. Technique and dosimetry. Acta Radiol Ther Phys Biol. 1971; 10(1): 33-55. https://doi.org/10.3109/02841867109129744.
- Groarke J.D., Nguyen P.L., Nohria A., Ferrari R., Cheng S., Moslehi J. Cardiovascular complications of radiation therapy for thoracic malignancies: the role for non-invasive imaging for detection of cardiovascular disease. Eur Heart J. 2014; 35(10): 612-23. https://doi.org/10.1093/eurheartj/eht114.
- Petroccia H., Mendenhall N., Liu C., Hammer C., Culberson W., Thar T., Mitchell T., Li Z., Bolch W. A hybrid phantom Monte Carlo-based method for historical reconstruction of organ doses in patients treated with cobalt-60 for Hodgkin's lymphoma. Phys Med Biol. 2017; 62(15): 6261-89. https://doi.org/10.1088/1361-6560/aa7c2f.
- Hull M.C., Morris C.G., Pepine C.J., Mendenhall N.P. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA. 2003; 290(21): 2831-7. https://doi.org/10.1001/jama.290.21.2831.
- van Leeuwen F.E., Ng A.K. Long-term risk of second malignancy and cardiovascular disease after Hodgkin lymphoma treatment. Hematology Am Soc Hematol Educ Program. 2016; 2016(1): 323-30. https://doi.org/10.1182/asheducation-2016.1.323.
- Charniot J.C., Khaled Z., Kidouche R., Nascimbeni L., Gandjbakhch I., Artigou J.Y. Complications cardiaques tardives de la radiothérapie. Presse Med. Paris. 2006; 35: 239-42.
- Yang E.H., Marmagkiolis K., Balanescu D.V., Hakeem A., Donisan T., Finch W., Virmani R., Herrman J., Cilingiroglu M., Grines C.L., Toutouzas K., Iliescu C. Radiation-Induced Vascular Disease-A Stateof-the-Art Review. Front Cardiovasc Med. 2021; 8. https://doi.org/10.3389/fcvm.2021.652761.
- Dracham C.B., Shankar A., Madan R. Radiation induced secondary malignancies: a review article. Radiat Oncol J. 2018; 36(2): 85-94. https://doi.org/10.3857/roj.2018.00290.
- Welch T.D., Oh J.K. Constrictive Pericarditis. Cardiol Clin. 2017; 35(4): 539-49. https://doi.org/10.1016/j.ccl.2017.07.007.
- Buitrago A.F., Gómez M., Restrepo J.A., Soto M., Díaz J.H. Diagnóstico hemodinámico de pericarditis constrictiva: presentación de un caso y revisión de la literatura. Rev Colomb Cardiol. 2013; 20(6): 397-402. https://doi.org/10.1016/S0120-5633(13)70092-5.
- Welch T.D., Ling L.H., Espinosa R.E., Anavekar N.S., Wiste H.J., Lahr B.D., Schaff H.V., Oh J.K. Echocardiographic diagnosis of constrictive pericarditis: Mayo Clinic criteria. Circ Cardiovasc Imaging. 2014; 7(3): 526-34. https://doi.org/10.1161/CIRCIMAGING.113.001613.
- Bhattad P.B., Jain V. Constrictive Pericarditis: A Commonly Missed Cause of Treatable Diastolic Heart Failure. Cureus. 2020; 12(5). https://doi.org/10.7759/cureus.8024.
- Yusuf S.W., Sami S., Daher I.N. Radiation-induced heart disease: a clinical update. Cardiol Res Pract. 2011. https://doi.org/10.4061/2011/317659.
- Tzani A., Doulamis I.P., Tzoumas A., Avgerinos D.V., Koudoumas D., Siasos G., Vavuranakis M., Klein A., Kampaktsis P.N. Meta-Analysis of Population Characteristics and Outcomes of Patients Undergoing Pericardiectomy for Constrictive Pericarditis. Am J Cardiol. 2021; 146: 120-7. https://doi.org/10.1016/j.amjcard.2021.01.033.
- Mitchell J.D., Cehic D.A., Morgia M., Bergom C., Toohey J., Guerrero P.A., Ferencik M., Kikuchi R., Carver J.R., Zaha V.G., Alvarez-Cardona J.A., Szmit S., Daniele A.J., Lopez-Mattei J., Zhang L., Herrmann J., Nohria A., Lenihan D.J., Dent S.F. Cardiovascular Manifestations From Therapeutic Radiation: A Multidisciplinary Expert Consensus Statement From the International Cardio-Oncology Society. JACC CardioOncol. 2021; 3(3): 360-80. https://doi.org/10.1016/j.jaccao.2021.06.003.


