Impact on student behavior due to COVID-19 lockdown in India
Автор: Singh J., Chitranshi J.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 22, 2022 года.
Бесплатный доступ
This paper aims to comprehend the change & impact on students’ behavior during the COVID-19 Lockdown in India. The research is conducted by surveying to assess the different behavioral changes due to the COVID-19 spread. Novel coronavirus pandemic started from Wuhan, China, on 31/12/19. It spread across the globe affecting 1,00 000 people within the span of two to three months. People across the globe were affected not just in terms of physical health but also mental & psychological health, resulting in major changes in their behavior. The digital questionnaire assessed the status of pupils’ mental and psychical nature while the COVID-19 lockdown was on. The questions were framed to answer how students felt about the pandemic and how it has affected their day-today life. The results of the survey revealed the measure of the anxiety level of the students. The survey results are analyzed on SPSS, and Pearson Coefficient is the method used for statistical analysis. The survey results revealed that 74.2% of the respondents favored cleaning their hands more often due to the COCID-19 pandemic. In the same way, an overwhelming number of student respondents have become aware that wearing masks is crucial to prevent the spread, and 95.9% of student respondents have favored wearing masks if they decide to step outside of their house. Student respondents are more worried about the possibility that their family members will catch the COVID-19 virus than the concern of themselves catching the virus. The student respondents showed clear signs of worry and unpredictability due to the COVID-19 spread. More than have 37.6% have responded that they are in a constant state of worry during the lockdown. The paper states varied responses from the students on the anxiety levels and that they have been experiencing high anxiety levels during the lockdown. The measurement and correlation between emotional & preventive behavior can provide viable options to reduce the outbreak and further control it.
Students behavior, covid-19, lockdown, mental health, physical health
Короткий адрес: https://sciup.org/148324597
IDR: 148324597 | DOI: 10.18137/cardiometry.2022.22.207214
Текст научной статьи Impact on student behavior due to COVID-19 lockdown in India
Jyoti Singh, Jaya Chitranshi. Impact on student behavior due to Covid-19 lockdown in India. Cardiometry; Issue 22; May 2022; p. 207-214; DOI: 10.18137/cardiometry.2022.22.207214; Available from: impact_student_behavior
The new coronavirus, first identified in China, Wuhan, in December 2019, is set to become the worst pandemic threat humanity collectively faces. Within a span of three to four months, the novel coronavirus has spread across the globe. The virus continues to spread, affecting and disrupting the lives of millions adversely [1].The initial incident in India was announced on 30 January 2020 in the state of Kerala (India, Indian Council of Medical Research-CMR).
As the cases continue to rise with every passing day, the pandemic has brought significant changes in people’s lives. The effect of lockdown has caused harm to the economies and the mental and psychological behavior of the populations [2]. People have become aware of the preventive behavior to protect themselves from the virus and build a protective attitude towards their well-being throughout the crisis of the COVID-19 upsurge. The right information at the right time must be provided to restrain the extent of the infection and manage mental stress and uncertainty during the lockdown [3]. Additionally the perception of the society of being affected by the virus has a significant effect on the protective behavior and the steps taken to minimize the risk of catching the disease. People feel safe when they know what to do, and their beliefs are enhanced by knowing that they can take meaningful steps to prevent the spread. Pandemics are known to create an adverse impact on people’s anxiety levels and increase psychological issues due to raised concerns about their well-being. Protective/ preservative factors for mental health are signified by heavy use of face masks and following other notions of protective measures [4]. OCD and PST are few disorders related to anxiety. They result from the tense and stressed environment around us, which eventu- ally are rampant, devitalizing, and expensive (Davies MR, 2020). The novel coronavirus pandemic has been reported to cause evident mental/psychological health issues across countries like China and Japan [5].
The COVID-19 outbreak is sudden and unpredictable. With the strong infectious nature of the virus, people usually show signs of stress and other related psychological problems. Control and contain the COVID-19 virus rules and regulations are set up through measures like avoiding physical contact with each other, restricting travel/movement, social distancing in public places, and quarantine or self-isolation [6]. Such prohibitions and precautions affect a human being’s social life, emotional well-being, and psychological status. During such turbulent times, it is imperative to probe and observe people’s mental health status. Suitably, it is important to measure and evaluate behavioral and psychological aspects [7]. Conducting psychological tests help in identifying specific disorders, tracking disease, and forecasting in such a manner that variables in human behavior can be reflected.
Additionally, these tests taken through web/on-line-based surveys render a quick and coherent method of recognizing difficulties, structuring and tracking a flow of treatment, and further evaluating the aftereffect of interference [8]. Specifically in the grave COVID-19 outbreak, data received by such methods offer useful information regarding human emotions, attitude, and behavior and provides immediate insight to researchers. The type and diagnosis of prevalent psychological disorders or how they are distributed throughout the population cannot be identified. Hence it is imperative to provide a quick estimation and analysis of Pandemic-associated psychological disorders to the population [9].
2 Materials and methods 2.1 Design and respondents
A net-oriented online poll was carried on for the study, and respondents were students living in India.
2.2 Measure
Respondents answered questions about Name, Age, and Gender.
2.3 Protective and preventive behavior towards covid-19 lockdown
To measure responses related to epidemiology and behavior about epidemiology during the COVID-19 outbreak, respondents answered yes and No questions related to precautionary steps to be taken during the lockdown [13]. The questions directed towards the respondents were “Washing or cleaning their hands frequently with soap-based cleansers for twenty seconds,” “wear masks in public places,” “refraining from touching face and eyes with hands,” “Proper ventilation of the residence” and “Maintaining social distancing.” The medical practitioners endorse these precautionary steps to prevent the virus spread [14].
2.4 Psychological behavior and levels of anxiety due to covid-19 lockdown
To measure the impact of COVID 19 Lockdown on the Student respondent’s emotional state of mind and change in levels of anxiety experienced during the ongoing crisis, they were presented with two important epidemiological questions:
“How fearful are you of being infected by the virus COVID-19?”
“How fearful are you of a family member getting infected by virus COVID-19?”
The questions have been answered on a Five-point (ordinal) Likert Scale with the level of agreement varying from (1) “Strongly Disagree,” (2) “Disagree,” (3)
“Neutral,” (4) “Agree,” (5) “Strongly Agree.” These two questions were compared with each other for the frequency distribution of estimated risk and fear factor of the COVID 19 pandemic [15].
To evaluate the emotional state of the student respondents in the survey, they were asked to answer questions: “What are your thoughts and emotions related to the COVID-19 Lockdown?” Respondents were given five choices to choose from, namely “Scared,” “Sad,” “Indifferent,” “worried,” and “afraid.” To measure the Anxiety level of respondents during the COVID-19 outbreak, they were asked to answer the question: “Experiencing increased Anxiety during Lockdown?” The question was answered on 5-point Likert Scale [16].
2.5 Exposure to news during the covid-19 lockdown
2.6 Statistical analysis
3 Results
Indian students consisting of 49% females and 50% males and 1% others (preferred not to say) with age ranging from Eighteen years to Thirty years participated in the survey and filled the Web-Based Survey Named “Impact on Student behavior During COVID-19 Lockdown” is shown in Figure 1.
|
VARIABLE |
RESPONDENTS (%) |
|
Gender |
|
|
Male |
49 % |
|
Female |
50% |
|
Prefer not to say |
1% |
|
Age (Years) Below 18 |
3.6 % |
|
18-24 |
53.6 % |
|
25-29 |
35.6 % |
|
30 & Above |
7.2 % |
Fig. 1. Depicts the demographic data of the student respondents
Content on Figure- 2 depicts the frequency Distribution of Preventive Behavior (Protective) Student respondents have shown to pay attention to keeping their hands clean and washing them more frequently (74.2 %), social distancing and isolation practices (93.3%), maintaining residence ventilation (82.5%), wearing masks (95.9%). [19].

Fig. 2. Frequency distribution of preventive behavior
Figure 3 and Figure 4 depict the frequency distribution to understand the COVID-19 fear and risk amid the respondents and their family members regarding catching the virus. In Figure 3, respondents answer the question “Scared of catching the Coronavirus?” and 69% of the respondents have a high fear of catching the infection, out of which 36% are extremely scared of picking the infection. However, 16.5% have a moderate fear of catching the disease, and the others do not fear the infection. When compared to the data of Figure 4, “Scared that a Family Member will catch _ 100 * 80 у 60 2 40 —
Q 20
g 0 -----—--■--■--■-
5 Never Somewhat Moderately Very Extremely
* FEAR OF BEING INFECTED BY THE NOVEL CORONAVIRUS
Fig. 3. Frequency distribution

Never Somewhat Moderately Very Extremely
FEAR OF BEING INFECTED BY THE NOVEL CORONAVIRUS
As shown in Figure 5, respondents have answered the question “My Emotions around the COVID-19 Pandemic during Lockdown?” Most of the respondents feel worried (37.6%) about the COVID-19 crises; while the second-highest section feels indifferent towards it (20.6%) followed by feelings and emotions of sadness (15.5%), anger (15.5%), and being afraid (10.8%).
Figure 6 and Figure 7 depict the extent of anxiety experienced with fear for the near future due to the widespread COVID-19 Pandemic situation.
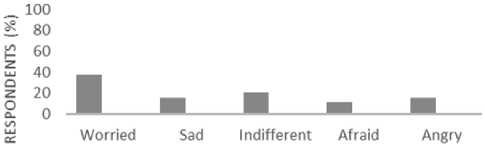
EMOTIONS (%) CAUSED DUETOCOVIDD-19 SPREAD
Fig. 5. Respondents have answered the question ж so
^ 60

cl Never Somewhat Moderately Very Extremely к Anxiety Levels and Fear of Future
Fig. 6. Extent of anxiety experienced

tr Career in Post Repaying Completing Not Being able
COVID Worli Student Loans . Education ■ students constant thoughts during COVID-19 Pandemic
Fig. 7. Extent of anxiety experienced
Almost 57% of the respondents feel very high and extremely high levels of anxiety and 22.7% have moderate anxiety levels
A major part of the respondents (75.3%) has constant thoughts about “career in post COVID world”; they are worried about “completing education” (33%) and “repaying Education loans” (19.6%). 31.4% of the respondents feel they face difficulties in Adapting to the new normal and are consistently have thoughts about the same.
Table 1 depicts a major correlation between exposure to media TV and information related to 210 | Cardiometry | Issue 22. May 2022
On the other hand, in Table 2, exposure to Media and News shows a correlation with Disruption in sleeping patterns. All the correlations are summarized in Table 1 and Table 2.
The present study aims to discover the spread of anxiety and its effect on the emotional state, preventive behavior of the young Indian population, and understand their connection with each other. Additionally, examine the interconnection of media and news exposure during the COVID-19 crisis on student behavior [21].
4 Discussions
This paper demonstrates the behavior change during the COVID-19 Lockdown in India. Each passing day situation across the world is being contained. Medical institutes are working to find a vaccine for the novel coronavirus disease. In this study, a web (online) -the based survey was taken to examine the responses of behavioral questions as it is efficient and faster. It has been found that the behavior of the respondents varies in accordance to age, gender, exposure to media, emotional state. The regular variation corresponds to the demographic, psychological, and epidemiological behavior [22].
It has been found that the protective or preventive behaviors of people in the country have changed due to the COVID-19 crisis. Moreover, people are becoming aware of the crisis by taking more precautions due to fear and uncertainty of the pandemic. Respondents are in constant fear that a family member might catch the novel coronavirus. This fear is even more when compared to them being infected [23].
Additionally, the use of masks is extremely high in the protective behavior section even though it has not been made legal by the government. However, people are following guidelines, and hence the use of masks is quite high than expected. Few studies have shown that individuals with pulmonary respiratory disease
Table 1
Major correlation between exposures to media TV
|
Pearson Correlation |
Hand Wash |
Wearing Mask |
Social Distancing |
Contact Face & Eyes |
Residence ventilation |
Exposure to Media about COVID-19 on TV |
|
Hand Wash |
1 |
.237** |
.128 |
.191** |
.082 |
.104 |
|
Wearing Mask |
.237** |
1 |
.463** |
.400** |
.250** |
.038 |
|
Social Distancing |
.128 |
.463** |
1 |
.315** |
.372** |
.116 |
|
Contact Face & Eyes |
.191** |
.400** |
.315** |
1 |
.234** |
.164* |
|
Residence ventilation |
.082 |
.250** |
.372** |
.234** |
1 |
.176* |
|
Exposure to Media about COVID-19 on TV |
.104 |
.038 |
.116 |
.164* |
.176* |
1 |
Correlation is significant at the *0.05 level (2-tailed) and **0.01 level (2-tailed)
Table 2
Major correlation between exposure to media TV
|
Pearson Correlation |
Exposure to news and information related to COVID-19 on TV? |
Fear of infection |
Fear Family Infection |
No control of future |
Anxiety experienced |
Sleep Disruptions |
Preference to Online Interaction |
Physical Activity adversely affected |
|
Exposure to news and information related to COVID-19 on TV |
1 |
-.183* |
-.058 |
.027 |
-.106 |
.120 |
-.011 |
-.020 |
|
Fear of infection |
-.183* |
1 |
.358** |
.225** |
.308** |
.204** |
.177* |
.232** |
|
Fear Family Infection |
-.058 |
.358** |
1 |
.150* |
.084 |
-.026 |
-.003 |
.145* |
|
No control of future |
-.058 |
.358** |
1 |
.150* |
.084 |
-.026 |
-.003 |
.145* |
|
Anxiety experienced |
-.106 |
.308** |
.084 |
.471** |
1 |
.369** |
.129 |
.350** |
|
Sleep Disruptions |
.120 |
.204** |
-.026 |
.400** |
.369** |
1 |
.036 |
.352** |
|
Preference to Online Interaction |
-.011 |
.177* |
-.003 |
.132 |
.129 |
.036 |
1 |
-.007 |
|
Physical Activity adversely affected |
-.020 |
.232** |
.145* |
.412** |
.350** |
.352** |
-.007 |
1 |
Correlation is significant at the *0.05 level (2-tailed) and **0.01 level (2-tailed)
The responses that the survey has received regards to the same it has been observed that the rate of washing hands by the student respondents is fairly high, but it is less than the rate of wearing masks, which is a surprising outcome [26].
The majority of the Respondents have answered the question “Your Emotions on COVID-19 Pandemic?” in favor of being “Worried” at 37.6%. This survey outcome can be considered normal because it is only natural to worry about one’s health in a pandemic. It can be concluded that it is a positive outcome that students or young people have an encouraging message and positive information. It is observed in another study that “worry” can increase as an emotion due to misinformation and perception in society. Moreover, in the right amount, worry has previously been effective in containing pandemics like SARS and Ebola. However, on the other hand, excessive worry may lead to negative outcomes and context to the novel coronavirus disease spread [27].
Respondents have answered the question,” How fearful are you of being infected by the virus (COVID-19)?” and 36.1% have said that they are ex- tremely scared of catching the virus, with another 33% saying that they are highly scared of catching the virus. However, when the data is compared to the response of the question, “How fearful are you of a family member getting infected by a virus (COVID-19)?” the results were unusual and prominent, and 60% of the respondents have confirmed, “Extremely fearful.” These results can be interpreted due to the quick and untraceable rate of the transmission of the disease and the mortality rates associated with it. Another interpretation is derived from the nature of humans that they believe it to be their moral responsibility to protect their family members, and hence they depict unconventional behavior. Therefore, increased fear and misinterpretation regarding novel coronavirus COVID-19 can lead to a disorder with a high emotional state [28].
The survey conducted has a few public health inferences. The responses received show that student’s preventive behavior constantly changes with exposure to news TV or Media. Due to firm social distancing regulations and policies, people have to remain connected through digital platforms now even more than ever to provide a similar experience of people interactions and data sharing related to COVID-19. The respondents have reacted highly to the social distancing protective/preventive behavior in the COVID-19 lockdown. An earlier study shows that people had no idea that the novel coronavirus can be transmitted through droplets. In return may decrease the effectiveness of a few precautionary measures. On the contrary, this paper shows that people are more inclined towards protective and preventive behavior. Digital platforms consistently stream videos from highly influential people during the COVID-19 pandemic outbreak. Therefore, it has resulted in effective and correct information transfer to the public regarding the COVID-19 outbreak [29].
A suggestion can be made in this context that by imparting simple and continuous information through digital media platforms, these preventive and protective behaviors can be encouraged.
The survey’s outcome has emphasized that the correlation between exposure to news TV media and sleep pattern disruption is significant. Earlier studies concur with the results that increased screen time on social media, and the internet leads to poor sleep quality [30].
On comparing the anxiety experienced due to the COVID-19 outbreak, the highest level of seriousness 212 | Cardiometry | Issue 22. May 2022
was observed due to fear of losing a family member due to the disease and about the career in the future with constant thoughts of worry and uncertainty associated with it. As a result, the anxiety experienced by the respondents is extremely high and emotions reflected are fear of a career in the post-COVID-19 world, not being able to adapt to new normal, and feeling of sadness. Since more than 50% of respondents have responded negatively to the switch from face-to-face interaction to online interactions, and sleep pattern being adversely affected due to increased social media and digital media exposure and social distancing and other restrictions, the high levels of anxiety are visible in the results. The students have not responded positively to the online medium of classes and would rather prefer classroom education. Following the same emotion, studies have shown that the delay in educa-tional/academic year is related to the increase of anxiety indicators in the universities of China. In another research, it has been found that the increased levels of anxiety in the students are due to fear of future career prospects and completion of education. Our study confirmed these results, with 74.3% of respondents saying they are constantly thinking about their career in the future, 33.5% saying they are worried about completing education, and 19.6% are thinking about repaying student loans. Lockdown has led to a negative impact on the mental health of the student respondents, and they are showing signs and symptoms of high psychological effects due to the COVID-19 outbreak in China as well. In response to the crisis, medical institutes worldwide are working on a vaccine, but no cure has been found. The same is that the COVID-19 crisis has resulted in very high anxiety levels due to its uncertainty about the cure [31].
In the survey results, it has been predicted that the protective and anxious nature of people, the adaptation to the new normal, and their protective/preven-tive behavior may have impacted by the COVID-19 crisis. Hence, this study is imperative for scientifically proving that widespread information and its connection to anxiety level and change in behavior due to a pandemic crisis is evident [32].
5 Limitations
In the current study, a few limitations are required to be noted. There is no investigative proof of exposure to news, media, TV-related to COVID-19 lockdown. Additionally, Meng et al. have stated that in the protection and cure of COVID-19 treatments, gender must be taken as a biological factor/variable.
Irrespective of their age, men have been found to have a higher risk than women of dying due to the COVID-19 virus in a study. Considering all these studies, a major limitation of the current study is that 50% of the respondents are females and only young adult students whose financial status has not been examined.
6 Conclusions
This study provides effective and efficient insight into creating a compassionate individual and more supportive society that would respond appropriately to the turbulent outbreak. The behavioral and psychological study like this sheds light on the uncertain future, and finding can help in paying a more structured process for the time ahead. Given that the survey was filled online, it still has a partial limit in context to the general population; its quick execution, the discovery of new and critical data may increase the extent of public awareness and consequently may provide life-saving measures. Educational programs in the Public Health domain can enhance and encourage a positive approach in dealing with COVID-19.
Further cognitive behavior therapy may help in calming down stress levels and provide coherent coping mechanisms. This study has implications for student’s public health provisions amidst the pandemic of infectious crisis, combined with improvements in preventive behavior.
Post COVID-19 crisis, studies on behavior and psychological effects of an outbreak can be conducted. The data that the current study provides can be referred by the researchers for critical processes and beyond.
Data Availability Statement
The paper consists of all the datasets presented in this study.
Ethics Statement
The name, age, gender of the respondents is taken with due written consent and will not be made public. According to the World Health Organization guidelines (WHO) on Ethical Issues in Public Health Surveillance, a study during an outbreak is exempted from ethical review and oversight. The web-based survey is taken in August 2020 in India, where the lockdown is ongoing. Respondents participated voluntarily in the complete report survey.
Conflict of Interest
The study was conducted without any financial or commercial relationship that may lead to any potential conflict of interest. It is completely for academic purposes.
Список литературы Impact on student behavior due to COVID-19 lockdown in India
- Y. Meng, P. W, Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PloS Pathog, 16(4), e1008520, (2020).
- A, C, Reducing Nursing Student Anxiety in the Clinical Setting: An Integrative Review. Nurs Educ Perspect, 41(4), 229–34, (2020).
- S. P. Adhikari, S. M, Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty, 9:1–12, (2020).
- D. K. Ahorsu, C. L, The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict, 27:1–9, (2020).
- A. Asnaani, J. T. Anxiety sensitivity and emotion regulation are mechanisms of successful CBT outcomes for anxiety-related disorders in a naturalistic treatment setting. In Journal of Affective Disorders 267, 86–95, (2020).
- B. L. Brown, J. M, TreaTment for emerging viruses: Convalescent plasma and COVID-19. Transfus Apher Sci, 59(3):102790 (2020).
- W. H. Chen, U. S, The SARS-CoV-2 vaccine pipeline: an overview. Curr Trop Med Rep, 3, 1–4, (2020).
- K. Choi, H. S, Internet overuse and excessive daytime sleepiness in adolescents. Psychiatry Clin Neurosci, 63(4), 455–62, (2009).
- C. Y. L, Social reaction toward the 2019 novel coronavirus (COVID-19). Soc Health Behav, 3, 1–2, (2020).
- M. R. Davies, G. K, The Genetic Links to Anxiety and Depression (GLAD) Study: Online recruitment into the largest contactable study of depression and anxiety. In Behav Res Ther 123, 103503, (2020).
- J. Greene, M. D, Learning to use statistical tests in psychology. UK: McGraw-Hill. Education (2005).
- C. S. Ho, C. C, Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann Acad Med Singapore, 49(3), 155–60, (2020).
- J. V. d, Television viewing, computer game playing, and Internet use and self-reported time to bed and time out of bed in secondary-school children. Sleep, 27(1), 101–4, (2004).
- J. M, Coronavirus and Mental Health: Taking Care of Ourselves During Infectious Disease Outbreaks. American Psychiatry Association, APA Coronavirus Resources (2020).
- J. Jin, P. B, Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front Public Health, 8, 152, (2020).
- J. H. Jones, M. S. Early Assessment of Anxiety and Behavioral Response to Novel Swine-Origin Influenza A(H1N1. PloS One , 4(12), e8032, (2009).
- L. Kang Y. L, The mental health of medical workers in Wuhan, China, is dealing with the 2019 novel coronavirus. Lancet Psychiatry, 7(3), e14, (2020).
- J. C. Levenson, A. S, The association between social media use and sleep disturbance among young adults. Prev Med, 85, 36–41, (2016).
- Y. H. Lin, C. L, Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. In Brain Behav Immun, 87, 30–2, (2020).
- R. Maunder, J. H, The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ, 168(10), 1245–51, (2013).
- M. ME, The use of psychological testing for treatment planning and outcomes assessment: General considerations. Lawrence Erlbaum Associates Publishers 3rd ed (2004).
- B. Person, F. S, Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis, 10, 358–63, (2004).
- E. Sallard, F. L, Type 1 interferons as a potential treatment against COVID-19. Antiviral Res, 178, 104791, (2020).
- J. Shigemura, R. U. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci, 74(4), 281–2, (2020).
- J. M. Shultz, F. B, The 2014 Ebola Outbreak and Mental Health: Current Status and Recommended Response. JAMA, 313, 567–8, (2015).
- W. Tan, F. H, Is Returning to Work during the COVID-19 Pandemic Stressful? A Study on Immediate Mental Health Status and Psychoneuroimmunity Prevention Measures of Chinese Workforce. In Brain, Behavior, and Immunity, 87, 84–92, (2020).
- S. Thomée, A. H, Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults—a prospective cohort study. BMC Public Health, 11(1), 66–76, (2011).
- C. Wang, R. P, Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health, 17, 1729, (2020).
- C, Wang, R. P, A Longitudinal Study on the Mental Health of General Population during the COVID-19 Epidemic in China. In Brain Behav 87, 40–8, (2020).
- A. Wilder-Smith, D. F, Isolation, quarantine, social distancing and community containment: a pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med, 27, 1–4, (2020).
- H. C. Woods, H. S, Sleepy teens: social media use in adolescence is associated with poor sleep quality, anxiety, depression, and low self-esteem. J Adolesc, 51, 41–9, (2016).
- N. Zhou, H. C, A four-wave, cross-lagged model of problematic internet use and mental health among Chinese college students: Disaggregation of within-person and between-person effects. Dev Psycho, 56, 1009–21, (2020).


