Influence made by industrial climbing safety equipment on the cardiovascular system performance and thermophysical parameters of limbs in an industrial climber at low ambient temperatures
Автор: Maria A. Goncharova, Ivan Y. Brink
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 20, 2021 года.
Бесплатный доступ
The task of the article is to assess the effect made by an industrial climbing safety system used by an industrial climber, performing his work to provide a harness-based suspended access at low ambient temperatures, on his physiological parameters. The article presents some studies on changes recorded in body surface temperatures, pulse rates, and blood pressure value in an industrial climber depending on the duration of his performance using a harness-based suspended access under ambient air low temperature conditions. The tests have been carried out for various types of thermal protection of the human hip area and the width of the belts of the safety system. The scientific novelty of the study is that it is the first time when such a study has been conducted for a combination of industrial factors, like prolonged suspended condition due to the utilization of the climbing safety system and a low ambient temperature. As a result, it has been found that the physiological parameters are influenced by the width of the safety belts of the safety equipment system and the method of the temperature protection of the hip zone in a climber.
Influence of low ambient temperature, Blood pressure, Pulse, Industrial climber, Industrial climbing safety system
Короткий адрес: https://sciup.org/148322446
IDR: 148322446 | DOI: 10.18137/cardiometry.2021.20.167174
Текст научной статьи Influence made by industrial climbing safety equipment on the cardiovascular system performance and thermophysical parameters of limbs in an industrial climber at low ambient temperatures
Maria A. Goncharova, Ivan Y. Brink. Influence made by industrial climbing safety equipment on the cardiovascular system performance and thermophysical parameters of limbs in an industrial climber at low ambient temperatures. Cardiometry; Issue 20; November 2021; p. 167-174; DOI: 10.18137/cardiome-try.2021.20.167174; Available from: issues/no20-november-2021/influence-made-by-industrial
The stay of a person, a climber or an industrial climber, under low ambient air temperature conditions with the mandatory use of the prescribed industrial safety system, is associated with a negative impact produced on the individual by natural hazards and industrial risk factors, as well as by some changes in the physiological parameters of the body as a result from pressing of the body with belts of the safety system [1] that negatively affects the body as a whole and the systems thereof [2,3,4].
Scientists both in Russia [5] and abroad [6] have already much studied the effect made by low ambient temperatures on the human body as a whole [7] that may cause deviations from the normal values of various organism systems to maintain the proper vital activity of the body [8]. In order to keep the thermal balance with decreasing seasonal temperatures, an individual experiences an elevated load applied to the cardiovascular system performance due to his/her physiological reactions [9,10]. It is known that the cold season is marked with a greater number of cardiovascular diseases and deaths [2,7,9], including the cases provoked due to long-term stays at low temperatures in open air [10,11]. It has been identified that the low ambient temperature exposure applied to the body increases cardiovascular loading [4], intensifies the symptoms of colds [12] and is a forerunner of a great number of heart diseases, such as hypertension [13,14,15], namely angina pectoris [16,17,18], arrhythmia [19], deep vein thrombosis [6,10,11], myocardial infarction [20,21,22], sudden cardiac death [23] etc.
When conducting a cold pressor test [24], it has been found that under the influence of low ambient temperatures, systolic and diastolic blood pressure increases in a human individual; the heart rate become greater, when performing a cold foot pressor test. Cooling of the surface tissues leads to a discomfort that may affect excitation, attention and mental concentration [25]. Cooling of the skin to low tem- peratures causes pain, numbness and, eventually, local freezer burns [26,27].
The industrial safety system and harness permanently used by a climber may also cause harm to human health, due to the compression of the blood vessels of the legs by the straps of the safety system [28] that is manifested by numbness in the lower extremities and a discomfort in the groin area [29]. Industrial climbers, who must use in his work the industrial safety equipment systems, while suspended by their safety harness, may be at risk of rhabdomyolysis [23], loss of consciousness [30] and sudden death [31]. But in this case most often the first line of attack is the performance of the cardiovascular system that is reflected in changes in blood pressure and heart rate [27,32].
Thus, it can be seen that there are no studies available which treat a comprehensive, overall, effect on the body of a climber and an industrial climber produced by a combined action of the factors acting in parallel: both by low ambient temperatures and loading due to the mandatory use of the safety equipment system.
The aim of this study has been to assess the combined effect produced by the industrial safety system loading on the human body and low ambient temperatures affecting an industrial climber organism in parallel. We have assumed that the complex of these factors will have a negative impact on the physiological processes in the human body. We also have expected that the biggest changes would affect the body surface temperature, blood pressure and heart rate. The main data obtained were the recorded values supplied by temperature sensors, a blood pressure monitor and a pulse oximeter. Knowledge of how the industrial safety system and low ambient temperatures influence an industrial climber may be relevant to occupational health care staff involved in the study of cardiovascular diseases of climbers or industrial climbers.
Materials and methods
A man without chronic diseases has participated in our experiments as a test subject with anthropometric data as follows: height 182 cm, weight 88 kg, aged 41.
Our full-scale experiments were carried out at low ambient temperatures, utilizing various combinations of warm protective clothing and industrial safety system versions in order to determine their effect produced on the human body.
168 | Cardiometry | Issue 20. November 2021
Experimental reports
A number of experiments were conducted on February 22, 2021. Before each experiment, the following data were measured and recorded: the air temperature during all experiments was within (3.3 ±4) °C; relative humidity (83.7 ± 6.5)%; wind speed (1.4 ±4) m/s. The data were properly indicated in the test report. After that, the test subject was equipped with an electronic thermometer for measuring body temperature (armpit), a wrist cuff for measuring blood pressure, a pulse oximeter for determining blood oxygen levels and heart rate (see Table 1 herein), temperature sensors placed onto different parts of the body surface; the test subject was dressed using winterized protective clothing (five different combinations).
Time limits have been defined for each experiment as given below: 20 minutes for one experiment and 30 minutes for the recovery of the test subject in a warm room to restore the normal physiological parameters.
After the temperature sensors were fixed onto the body of the test subject, he was dressed in a combination of protective clothes and a safety system specified by the experiment; then the physiological parameters of the test subject were measured and recorded; the test individual was suspended with a rope from a crossbar in such a way that he was positioned free without support for 20 minutes. The data of direct measurements delivered by the temperature sensors were displayed on the digital display of the thermometer and recorded every 2 minutes within 20 minutes for each experiment on the test report. All measurements were carried out during working hours (see Figure 1 herein).
Blood pressure
Shoulder BP was measured using automatic wrist watch (OMRON 2 Basic, China), at intervals of 10 minutes from the beginning of the tests. The arm of the subject was supported, placed onto the knee, and the cuff was positioned at the level of the heart axis.
Heart rate
Heart rate was measured using an automatic fingertip oximeter (Fingertip Pulse Oximeter, SH-01, China), at intervals of 10 minutes from the beginning of the tests. The device was applied to the thumb of the left hand of the test subject. The hand was supported, placed on the knee.
Table 1
Measured physiological data of the test subject in five experiments
|
The test subject wears lightweight textile trousers plus a safety system |
||||
|
Time of measurement |
Body temperature, °C |
Blood pressure, mmHg |
Pulse, beats/min |
Oxygen concentration in blood, % |
|
Beginning of the test |
35 |
122/80 |
56 |
97 |
|
10 minutes after testing start |
36.2 |
130/85 |
98 |
96 |
|
End of the test |
36.6 |
130/90 |
102 |
95 |
|
The test subject wears lightweight textile trousers plus a safety system with downy shorts on top |
||||
|
Beginning of the test |
36 |
122/80 |
95 |
97 |
|
10 minutes after testing start |
36.1 |
125/98 |
96 |
98 |
|
End of the test |
36.3 |
130/90 |
85 |
95 |
|
The belt width of the safety system is 4.3 cm |
||||
|
Beginning of the test |
35.5 |
120/80 |
91 |
98 |
|
10 minutes after testing start |
36.5 |
125/85 |
93 |
96 |
|
End of the test |
36.8 |
125/90 |
100 |
98 |
|
The belt width of the safety system is 7 cm |
||||
|
Beginning of the test |
36.2 |
110/90 |
103 |
97 |
|
10 minutes after testing start |
36.5 |
120/90 |
96 |
97 |
|
End of the test |
36.7 |
120/90 |
95 |
97 |
|
The test subject wearing warm down trousers, equipped with a safety system with a strap width of 4.3 cm as well as lightweight cotton shorts worn over |
||||
|
Beginning of the test |
35.5 |
110/90 |
95 |
96 |
|
10 minutes after testing start |
36.2 |
120/90 |
106 |
97 |
|
End of the test |
36.7 |
120/90 |
108 |
96 |

Figure 1. Points of locations of temperature sensors: sensor No. 1 (on the surface of the hip), sensor No. 2 (on the body surface under the safety system belt), sensor No. 3 on the body surface in the buttock area, sensor No. 4 (on the foot surface) in shoes
Digital data of temperature sensors (skin surface temperature)
The skin temperature was measured by sensors placed at certain points of the skin surface, every 2 minutes for the period of 20 minutes of each test using a small-sized digital thermometer (TCM 1520 (incorporated five remote sensors), Russia), and the data were indicated in the test report.
The sensors were placed as follows: sensor No. 1 on the upper surface of the hip, below the hip strap of the safety system; sensor No. 2 under the strap of the safety system, on the hip; sensor No. 3 on the body surface of the test subject, in the buttock area, above the hip strap of the safety system; sensor No. 4 was placed on the foot surface of the test subject). Heat losses were estimated by the arithmetic mean of 10 measurements for each sensor.
Results
Thermoregulatory reactions
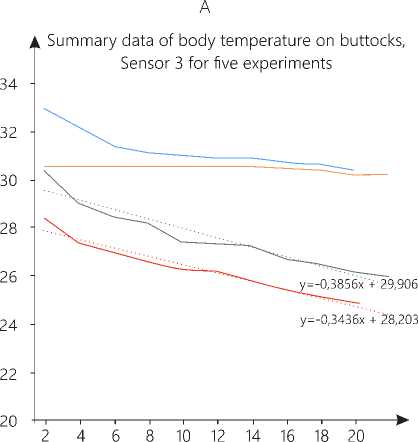
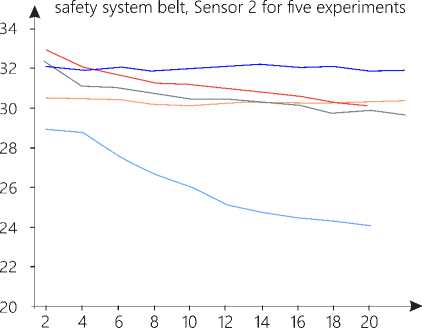
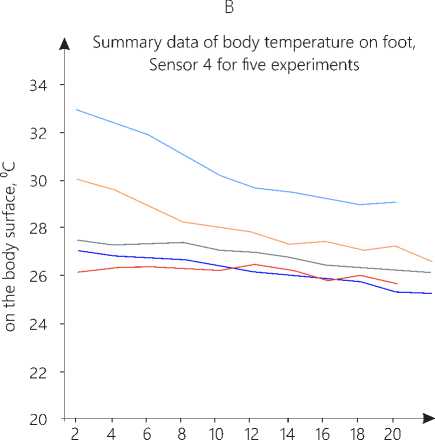
Based on the results of five experiments in various protective clothing configurations and the safety systems with different strap thicknesses, summary diagrams for each temperature sensor have been constructed as given in Figure 2 A, B, C, D herein.
The effect produced by low ambient temperatures on a human individual in all experiments with various combinations of winterized protective clothing has shown, in general, the dynamics of a decrease in the body surface temperature values recorded by all sensors. Thus, sensor No. 1 in the hip area in front has recorded a decrease of 3°C in the skin surface temperature in all experiments; sensor No. 2, fixed under the strap of the safety system on the body surface, has recorded a decrease in the skin surface temperature by 2.2 °C; sensor No. 3, applied to the skin surface in the buttock area, has delivered the measurements decreased by 2.7 ° C, and sensor No. 4, fixed on the foot skin surface, has documented a decrease by 2 °C, respectively. According to the individual feelings of the test subject, numbness of the legs has appeared upon completing half of testing (10 minutes after test starting), and it has been reported that the lower part of the body has begun to freeze after a third of the experiment time (5-6 minutes before the end of the experiment) reaching the state “very cold”.
Blood pressure and heart rate
170 | Cardiometry | Issue 20. November 2021
The effect produced by low ambient temperatures on a human individual, working with the use of industrial climbing safety equipment with a harness-based suspended access has demonstrated that during all the experiments the recorded body temperature has been found to be stable. The exposure to low ambient temperatures has resulted in an increase in the systolic blood pressure by an average of 8 mmHg and in the diastolic pressure value by 5 mmHg. The reported heart rate values in the different experiment configurations (sets of protective clothing used) show highly variable results. For example, when tested in lightweight textile protective trousers with the use of an industrial climbing safety system, the number of heart beats per minute has increased more than 2 times (from 56 to 102 beats/min.). Most likely, this is due to heavy physical load experienced by an individual when working with the use of industrial climbing safety equipment with a harness-based suspended access that is a sort of stress for an untrained organism. It is an important indicator that the cardiac system is under heavy loading, and a rise in the pulse over 100 beats per minute is classified as tachycardia, that is a marker of the incapability of the heart to efficiently deliver blood in the organism. Of course, this unfavorable condition is neutralized as soon as the person returns to his usual environment, and it does not cause serious complications and or a discomfort. But if this load is applied to the human body on a regular basis, then the risk of developing a heart disease becomes greater. So taking into account the individual characteristics of each person, the above indicator may serve as a transitional case towards developing an occupational disease. When wearing warm down shorts in addition to the above set of protective clothing, the difference in the heart rate before the test and after it has been found to be minimized and has become even smaller (from 95 to 85 beats/min) that is probably due to an additional heat insulation of the affected area and a more comfortable condition for the test subject.
Discussion
Our experimental study is the first research designed to assess the physiological parameters of a human body of an individual working with the use of industrial climbing safety equipment with a harness-based suspended access under exposure to low ambient temperatures and other unfavorable atmospheric factors, similar to usual everyday working
Data of temperature sensors Data of temperature sensors on the body surface, °C on the body surface, °C
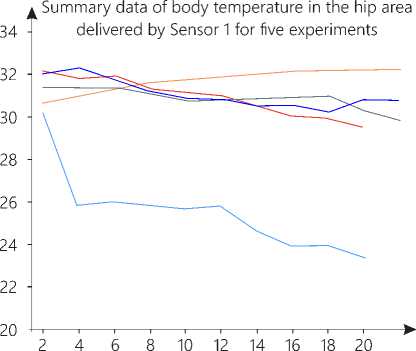
Summary data of body temperature under the
Time intervals of measurements, min.
___ Lightweight textile trousers and safety system,
Sensor 1 in the hip area, °C
Lightweight textile trousers and safety system and down shorts,
Sensor 1 in the hip area, °C
— Down trousers and safety system with stray width 4.3 cm,
Sensor 1 in the hip area, °C
— Down trousers and safety system with stray width 7 cm,
Sensor 1 in the hip area, °C
— Down trousers and safety system with lightweight textile shorts above, Sensor 1 in the hip area, °C
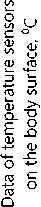
Time intervals of measurements, min.
Lightweight textile trousers and safety system,
Sensor 2 under the safety system belt, °C
Lightweight textile trousers and safety system and down shorts,
Sensor 2 under the safety system belt °C
Down trousers and safety system with stray width 4.3 cm,
Sensor 2 under the safety system belt, °C
Down trousers and safety system with stray width 7 cm,
Sensor 2 under the safety system belt, °C
Down trousers and safety system with lightweight textile shorts above, Sensor 2 under the safety system belt, °C
Time intervals of measurements, min.
Lightweight textile trousers and safety system,
Sensor 3 on buttocks, °C
Lightweight textile trousers and safety system and down shorts,
Sensor 3 on buttocks °C
Down trousers and safety system with stray width 4.3 cm,
Sensor 3 on buttocks, °C
Down trousers and safety system with stray width 7 cm,
Sensor 3 on buttocks, °C
Down trousers and safety system with lightweight textile shorts above,
Sensor 3 on buttocks, °C
Linear (Down trousers and safety system with stray width 4.3 cm,
Sensor 3 on buttocks, °C)
Linear (Down trousers and safety system with stray width 7 cm,
Sensor 3 on buttocks, °C)
Time intervals of measurements, min.
Lightweight textile trousers and safety system,
Sensor 4 on foot °C
Lightweight textile trousers and safety system and down shorts,
Sensor 4 on foot °C
Down trousers and safety system with stray width 4.3 cm,
Sensor 4 on foot °C
Down trousers and safety system with stray width 7 cm,
Sensor 4 on foot °C
Down trousers and safety system with lightweight textile shorts above, Sensor 4 on foot, °C
C
D
Figure 2. Summary diagrams of body temperature data delivered by sensors No. 1, 2, 3, 4 for five experiments conditions. Although the effect made by low ambient temperatures has not been found significant , we have observed that it has resulted in lowering the body surface temperature in the test subject according to the evidence data delivered by all temperature sensors in all sets of our experiments covering all sets of protective clothing that as a consequence may negatively affect the performance of an industrial climber under working conditions and reduce the total time required for the work completion; with regular heat loss when undertaking the regular occupational activity, it may provoke the onset of diseases, with the potential to convert the disease to an occupational one.
According to our results, a short-term exposure to low ambient temperatures (20 minutes) leads to an increase in blood pressure, however not to critical values thereof, that does not affect the overall performance of a person. The observed increase and decrease in the heart rate, depending on the set of protective clothing, may indicate possible frequent problems of the cardiovascular system performance with respect to tachycardia and arrhythmia.
Previous experimental and clinical trials studying the effect produced by low ambient temperatures on the human body [2], including the performance of the cardiovascular system [33] and other systems in the human organism [9,16,14, etc.] were carried out without loading applied to the test subject body due to the use of industrial climbing safety equipment with a harness-based suspended access. Also, some tests conducted with rope-based suspended access [23] did not take into account the effect made by low ambient temperatures on the body of a working person: they were mostly aimed at studying of the industrial climber performance, who used not the industrial climbing safety system, but who employed the rope suspension systems only [32,30].
Conclusions
As a result of the presented sets of tests, it has been found that the systolic and diastolic blood pressure in the test subject has increased by an average of 10 mmHg in all experiments for different protective clothing configurations. At the same time, the heart rate values have demonstrated their instability. Probably, with an increase in blood pressure, the heart rate should also be greater. A detailed analysis has revealed that the complete set of the winterized protective clothing may influence the heart rate values.
The fact is that when a climber applies his industrial climbing safety system onto his trousers, including the winterized version thereof, his protective clothing is pressed by the straps of the safety system, so that some “body heat loss points” appear, which may provoke intensive heat losses, and the climber experiences general discomfort, stress and shows some other changes in his physiological body parameters (the heart rate increase from 56 to 102 beats/min for 20 minutes of the experiment). But when later the same test subject has been experienced some more comfortable conditions, using warm downy shorts over the set of his protecting clothing, we have observed the body’s response: the heart rate reduction (from 95 to 85 beats/min for 20 minutes of the experiment). This is probably due to the fact that the test subject has recovered his comfortable warm state, relaxed, and the stress loading applied to the body has been minimized. The same response has been observed with the use of different versions of the industrial climbing safety systems. When in the first experiment we have utilized a system configuration with a strap width of 4.3 cm for the test subject, the heart rate has increased (from 91 to 100 beats/min for 20 minutes of the experiment). But as soon as in the second experiment we have applied another safety system with straps 7 cm wide, the body has “calmed down”, the test subject has experienced more comfort working with the harness-based suspended access; stress has been eliminated, and the pressure on hips has been minimized; the heart rate has decreased (from 103 to 95 beats /min for 20 minutes of the experiment). By this means it can be concluded that the physiological parameters of the human body exposed to low ambient temperatures depend on the degree of additional thermal protection of the hip area and on the width of the straps of the industrial climbing safety system used by a working person.
The obtained results are the basis for the development of some fresh design concepts for protective clothing and industrial climbing safety systems to improve the working conditions and reduce the physiological load experienced by an industrial climber.
Statement on ethical issues
Research involving people and/or animals is in full compliance with current national and international ethical standards.
Conflict of interest
None declared.
Author contributions
The authors read the ICMJE criteria for authorship and approved the final manuscript.
Список литературы Influence made by industrial climbing safety equipment on the cardiovascular system performance and thermophysical parameters of limbs in an industrial climber at low ambient temperatures
- Brink IY, Goncharova MA. Analysis of the labor activity of industrial mountaineering in conditions of low temperatures. In the collection: Nature, society, technology and thinking: trends and priorities. Collection of scientific papers based on the materials of the I International Scientific and Practical Forum of Young Scientists. 2017. p. 346-354 Available at: http://scipro.ru/wp-content/uploads/2017/04/05042017.pdf [in Russian]
- Fares A. Winter cardiovascular diseases phenomenon. N Am J Med Sci. 2013;5 (4):266–279. doi:10.4103/1947-2714.110430. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3662093/
- Tiina M. Ikäheimo. Cardiovascular diseases, cold exposure and exercise Temperature (Austin) 2018; 5(2): 123–146. Published online 2018 Feb 1. doi: 10.1080/23328940.2017.1414014 PMCID: PMC6204981 Available at: https://pubmed.ncbi.nlm.nih.gov/30377633/
- Abrignani MG, Corrao S, Biondo GB, Lombardo RM, Di Girolamo P, Braschi A. Effects of ambient temperature, humidity, and other meteorological variables on hospital admissions for angina pectoris. Eur J Prev Cardiol. 2012;19:342–8. Available at: https://pubmed.ncbi.nlm.nih.gov/21450571/
- Novikov VS, Soroko SI. Physiological foundations of human life in extreme conditions. SPb: Polytechnic-print, 2017. 476 p. [in Russian]
- Castellani JW, Tipton MJ. Cold stress effects on exposure tolerance and exercise performance. Compr Physiol. 2015;6(1):443–469. doi:10.1002/cphy.c140081. Available at: https://pubmed.ncbi.nlm.nih.gov/26756639/
- Bunker A, Wildenhain J, Vandenbergh A, et al. . Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016; 6: 258–268. Available at: https://pubmed.ncbi.nlm.nih.gov/27211569/
- Hanna JM. Climate, altitude, and blood pressure. Hum Biol. 1999;71:553–82. Available at: https://pubmed.ncbi.nlm.nih.gov/10453102/
- Song X, Wang S, Hu Y, et al. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ. 2017; 586: 241–254. doi:10.1016/j.scitotenv.2017.01.212. Available at: https://pubmed.ncbi.nlm.nih.gov/28187945/
- Ryti NRI, Mäkikyrö EMS, Antikainen H, et al. . Risk of sudden cardiac death in relation to season-specific cold spells: a case-crossover study in Finland. BMJ Open. 2017;7(11):017398. doi:10.1136/bmjopen-2017-017398.
- Gasparrini A, Guo Y, Hashizume M, et al. . Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015; 386(9991):369–375. doi:10.1016/S0140-6736(14)62114-0.
- Ilkka Korhonen (2006) Blood pressure and heart rate responses in men exposed to arm and leg cold pressor tests and whole-body cold exposure, International Journal of Circumpolar Health, 65:2, 178-184, DOI: 10.3402/ijch.v65i2.18090
- Payne RA, Wilkinson IB, Webb DJ. Arterial stiffness and hypertension: emerging concepts.Hypertension. 2010;55(1):9–14. doi:10.1161/HYPERTENSIONAHA. 107.090464.
- Wang Q, Li C, Guo Y, et al. . Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–286. doi: 10.1016/j.scitotenv.2016.10.019.
- Marti-Soler H, Gubelmann C, Aeschbacher S, et al. . Seasonality of cardiovascular risk factors: an analysis including over 230 000 participants in 15 countries. Heart. 2014;100(19):1517–1523. doi:10.1136/heartjnl-2014-305623. Available at: https://heart.bmj.com/content/100/19/1517
- Sun Z. Cardiovascular responses to cold exposure. Front Biosci (Elite Ed). 2010;2:495–503. doi:10.2741/e108. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826836/
- Brown CF, Oldridge NB. Exercise-induced angina in the cold. Med Sci Sports Exerc. 1985;17(5):607–612. doi:10.1249/00005768-198510000-00015 Available at: https://pubmed.ncbi.nlm.nih.gov/4068968/
- Rosengren A, Wennerblom B, Bjurö T, et al. Effects of cold on ST amplitudes and blood pressure during exercise in angina pectoris. Eur Heart J. 1988; 9(10): 1074–1080. doi:10.1093/oxfordjournals.eurheartj.a062402.
- Głuszak A, Kocoń S, Zuk K, Aljabali P, Gluza A, Siwek K. Episodes of atrial fibrillation and meteorological conditions. Kardiol Pol. 2008;66:958–63.
- Abrignani MG, Corrao S, Biondo GB, Renda N, Braschi A, Novo G. Influence of climatic variables on acute myocardial infarction hospital admissions. Int J Cardiol. 2009;137:123–9.
- Wang H, Kakehashi M, Matsumura M, Eboshida A. Association between occurrence of acute myocardial infarction and meteorological factors. J Cardiol. 2007; 49: 31–40.
- Margaret M. Sugg, Scott Stevens, Jennifer D. Runkle. Estimating personal ambient temperature in moderately cold environments for occupationally exposed populations/ Environmental Research:Volume 173, June 2019, Pages 497-507. https://doi.org/10.1016/j.nvres.2019.03.066
- Roger B, MortimerMD. Risks and Management of Prolonged Suspension in an Alpine Harness/ Wilderness & Environmental Medicine Volume 22, Issue 1, March 2011, Pages 77-86. https://doi.org/10.1016/j.wem.2010.10.008
- Enander A. Effects of moderate cold on performance of psychomotor and cognitive tasks. Ergonomics 30, 1987, 1431-45.
- Giesbrecht GG, Bristow GK. Recent advances in hypothermia resrarch. Ann N Y Acad Sci 15, 1997, 633-75. Available at: https://pubmed.ncbi.nlm.nih.gov/9100953/
- Giesbrecht GG, Wilkerson JA. Hypotermia, frostbite and other cold injuries, The Mountaineeers Book, Seattle, 2006.
- Roeggla M, Brunner M, Michalek A, et al. Cardiorespiratory response to free suspension simulating the situation between fall and rescue in a rock climbing accident Wilderness Environ Med, 7 (1996), pp. 109-114
- Physiology of blood circulation: physiology of the vascular system [Text]: a guide to physiology / Ed. B.I. Tkachenko. L .: Science, 1986. [in Russian]
- Gromov AP. Biomechanics of trauma. Moscow: Medicine, 1979. p. 242. [in Russian]
- Mark AL. The Bezold-Jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart J Am Coll Cardiol, 1 (1983), pp. 90-102.
- Mathieu Pasquier MD, Clinical Update: Suspension Trauma. Wilderness & Environmental Medicine Volume 22, Issue 2, June 2011, Pages 167-171. Available at: https://www.sciencedirect.com/science/article/pii/S1080603210004023
- Shamsuzzaman ASM, Sugiyama Y, Kamiya A, Fu Q, Mano T. Head-up suspension in humans: effects on sympathetic vasomotor activity and cardiovascular responses. J Appl Physiol. 1998;84:1513-9.
- Tiina M. Ikäheimo, Heidi Hintsala, Tuomas V. Kenttä. Cardiac Repolarization and Autonomic Regulation during Short-Term Cold Exposure in Hypertensive Men: An Experimental Study. Published: July 1, 2014. Available at: https://doi.org/10.1371/journal.pone.0099973


