Клинический случай: формирование абсцесса в области имплантации коронарного голометаллического стента
Автор: Бережной К.Ю., Ванюков А.Е., Зомбковская Л.С.
Журнал: Московский хирургический журнал @mossj
Рубрика: Клинические исследования
Статья в выпуске: 3 (49), 2016 года.
Бесплатный доступ
В данной статье представлен клинический случай одного из самых редких осложнений коронарного стентирования - формирования абсцесса в области имплантации коронарного голометаллического стента.
Чрескожное коронарное вмешательство, инфекция, абсцесс, колоректальнй рак
Короткий адрес: https://sciup.org/142211262
IDR: 142211262 | УДК: 616.12-089
Текст научной статьи Клинический случай: формирование абсцесса в области имплантации коронарного голометаллического стента
В связи с бурным развитием интервенционной кардиологии, в последние годы «золотым стандартом» лечения острого коронарного синдрома стало чрескожное коронарное вмешательство [1 – 3]. В связи с этим нам стоит помнить о редких, но, тем не менее, драматичных осложнениях.
Довольно часто, в 7 % случаев в области коронарного стентирования возникает гематома, в 74% случаев это осложнение протекает бессимптомно и в 29% случаев даже не выявляется при выполнении КАГ [4, 5]. Случаи возникновения абсцесса в области гематомы встречаются крайне редко.
Впервые стентирование коронарных артерий было выполнено в 1987 году [6]. Однако первый случай инфекционного воспаления в месте имплантации коронарного стента был зарегистрирован только спустя 6 лет. При этом за все прошедшее время до настоящего момента в англоязычной литературе описано всего около 17 случаев инфекционного поражения связанного с коронарным стентированием. Большинство случаев зарегистрированы после 2000 года, когда количество черескожных коронарных вмешательств заметно возросла. Довольно часто (около 30% случаев) после проведения ЧКВ возникает бессимптомная бактериемия, однако клинические проявления возникают редко [7, 8]. Несмотря на низкую частоту встречаемости данного осложнения, инфекция в месте имплантации стента сопровождается крайне высокой летальностью.
В настоящее время, чаще всего, при постановке диагноза «инфекция стента» используются критерии Diter [9]. Окончательный диагноз ставится на основании данных аутопсии или после экспертизы хирургического материала. Для постановки предварительного диагноза должны присутствовать 3 из представленных критериев: имплантация коронарного стента в течение предыдущих 4 недель, наличие бактериемии, повышение температуры или лейкоцитоз без другой возможной причины, острый коронарный синдром, несколько процедур выполняемых через один и тот же ин-традюссер или данные инструментальной диагностики. Принято выделять раннее начало инфекции – в сроки до 10 дней после имплантации стента и позднее – в сроки превышающие 10 дней.
Инфекционные осложнения, связанные с имплантацией стента, в первую очередь сопровождаются развитием местного абсцесса и перикардита. Также возможно развитие более тяжелых осложнений таких как гнойный перикардит, перфорация сосуда, тромбоз стента, разрыв миокарда, эмпиема перикарда.
Del Pace S, ретроспективно проанализировав 41 случай тромбоза стента, предположил, что возникновение этого осложнения связано с острой инфекцией [10].
Elieson [11], в 2012 году представил обзор случаев, связанных с инфекцией коронарных стентов представленных в англоязычной литературе. Эти данные помогли определить ряд закономерностей в данной группе пациентов. У всех
представленных пациентов не было иммунодефицита. При выявлении данного осложнения у всех больных была схожая клиническая картина – загрудинные боли, повышение температуры.
У всех пациентов был высеяны патогенные бактерии – в 14 случаях - стафилококк и в 2 случаях синегнойная палочка. После высева патогенного штамма, следующим этапом определяли локализацию очага инфекции. Источник инфекции диагностировали различными методами. 10 пациентам была выполнена чреспищеводная ЭХОКГ, однако только у 4 пациентов исследование показало положительный результат [12 – 15]. Так же еще у одного пациента выполнение ЭХОКГ показало отрицательный результат, одна при повторном исследовании была выявлена аневризма коронарной артерии [16]. При выполнении ангиографической процедуры во всех случаях была выявлена аневризма или ложная аневризма коронарной артерии. Таким образом, Elieson, установил, что выполнение коронарографии нужно считать золотым стандартом в сочетании с выполнением ЭХОКГ для первичной постановки диагноза при подозрении на возникновение инфекционных осложнений коронарного стентирования.
Также данный обзор показал, что сроки возникновения осложнения и применяемая тактика существенно влияют на исход заболевания. 10 пациентов имели серьезные осложнения и 5 умерли [16 – 19]. Ранее начало инфекции связанной с имплантацией стента поддается медикаментозной терапии, так 2 пациента из 4 выжили при проведении консервативной терапии. Из 6 пациентов, также получавших консервативную терапию и перенесших хирургическое вмешательство, 4 пациента выжили. Возникновение инфекции в более поздние сроки требует хирургического вмешательства, так как все пациенты получавшие только консервативную терапию погибли, а все 4 пациента перенесших оперативное вмешательство выжили. В последующем выжившие больные получали курс антибиотикотерапии как минимум 4 недели.
Клиническое наблюдение
Пациент С. 87 лет поступил в ГКБ №52 23.09.15 с жалобами на одышку и возникновение загрудинных болей при минимальной физической нагрузке. Из анамнеза известно, что пациент на протяжении года страдает хронической железодефицитной анемией, хроническим геморроем, МКБ, хроническим пиелонефритом, ДГПЖ, гипертонической болезнью 3 ст. Также известно, что пациент около 4 лет назад перенес резекцию полипа толстой кишки. При поступлении Hb 79 г/л, мочевина 11 ммоль/л, креатинин 145 мкмоль/л. При дообследовании пациенту был выставлен диагноз ИБС: стенокардия напряжения III Ф.К. В связи с чем получал консервативную терапию: ингибиторы АПФ, бета-адреноблокаторы, препараты железа, противоязвенные препараты. Однако, через 3 суток с затяжным приступом загрудинных болей пациент был переведен в отделение кардиореанимации. На ЭКГ депрессия ST в II,III, V 2–6 отведениях, тропонин – 460 нг/л, по данным ЭХОКГ – зоны акинеза апикального, среднего, сегментов боковой и передней стенки, акинез апикального сегмента задней стенки в связи с чем пациенту был выставлен диагноз ИМ без подъема сегмента ST в связи с чем пациенту была выполнена экстренная коронарография. По данным коронарографии выявлен тандемный протяженный стеноз проксимального и среднего сегмента ПМЖВ с участками стенозирования до 95%, стеноз устья ДВ 85%, стеноз среднего сегмента ОВ 80%, хроническая окклюзия ВТК. Дистальное русло заполняется по интра- и межсистемным коллатералям, хроническая окклюзия среднего сегмента ПКА, дистальное русло заполняется по интра- и межсистемным коллатералям преимущественно из системы ЛКА. Учитывая степень и локализацию поражения коронарного русла, методы лабораторных и инструментальных методов обследования выполнена баллонная ангиопластика и стентирование стеноза проксимально-

Рис. 1. Ангиограмма коронарных артерий: выявлен тандемный протяженный стеноз проксимального и среднего сегмента ПМЖВ с участками стенозирования до 95%
го и среднего сегмента ПМЖВ двумя голометаллическими стентами 3,0×38 и 3,5×28 с хорошим ангиографическим эффектом. После проведения процедуры состояние пациента стабилизировалось, на ЭКГ сегмент ST на изолинии, боли не рецидивировали. К назначенным препаратам была добавлена двойная антитромбоцитарная терапия.

Рис. 2 Результат коронарного стентирования проксимального и среднего сегмента ПМЖВ
Пациент был переведен в отделение кардиологии. 28.09.15 в анализе мочи у пациента лейкоциты, бактерии, значительное количество белка, креатинин 221 мкмоль/л. 29.09.15 пациента беспокоит слабость, гипотония. В анализе крови Hb 69г/л, лейкоциты 5,2×109/л, СОЭ 45 мм/час. Больному выполнена ЭГДС при которой выявлен эрозивный гастрит с признаками состоявшегося кровотечения. При осмотре нефрологом выставлен диагноз контраст-индуцированная нефропатия. 02.10.15 продолжает беспокоить слабость, температура 37,3. 04.10.15 ухудшение состояния, одышка до 30 в мин, гипотония, тахикардия, спутанное сознание. В анализах крови лейкоцитоз 19,7 тыс. с левым сдвигом. Пациент был переведен на ИВЛ и в тот же день скончался.
По результатам секции с последующим гистологическим исследованием у больного за основное заболевание принято сочетание распадающегося рака толстой кишки, осложнившегося развитием тяжелой анемии. А также, как второе основное заболевание коронарокардиоскле-роз, осложнившейся острым коронарным синдромом без подъема сегмента ST, что потребовало выполнения ЧКВ, которое осложнилось периваскулярной гематомой с нагноением и формированием абсцесса в зоне имплантации стента, тромбозом стента, а так же фибринозно-гнойным перикардитом и сепсисом: метастатическим гнойным миокардитом, метастатическим гнойным нефритом, гиперплазией и миелоидной метаплазией костного мозга и селезенки.
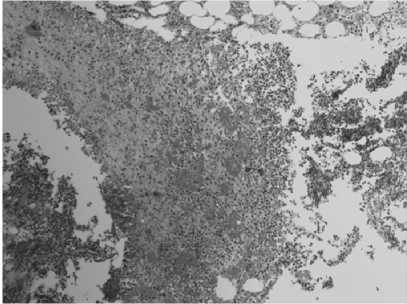
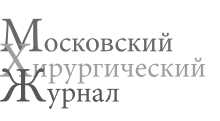
Рис. 3. В зоне имплантированного стента абсцесс, стенками которого является некротизированный миокард с лейкоцитарной инфильтрацией. В полости абсцесса скопление гнойно-некротических масс
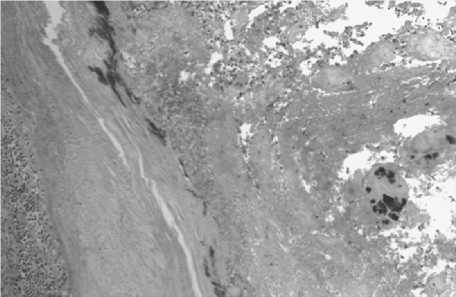
Рис. 4. Стенка аорты в области устья левой коронарной артерии с колониями бактерий и гнойно-некротическим расплавлением стенки, на которой также отмечается наложение гнойно-некротических масс с колониями бактерий
Рис. 5. Гнойный миокардит. Некрозы с густой лейкоцитарной инфильтрацией и колониями микробов
Обсуждение
Учитывая результаты аутопсии можно предположить, что источником инфекции и развития сепсиса с последую-
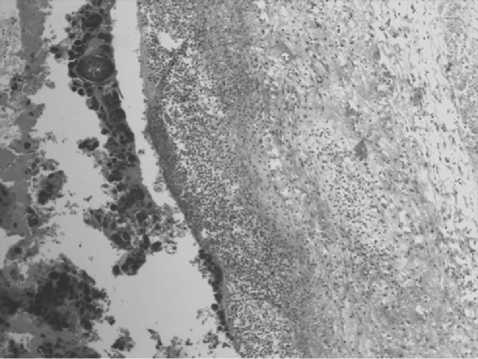
Рис. 6. Диффузная лейкоцитарная инфильтрация эпикарда с наложениями фибринозно-гнойных масс с колониями микробов
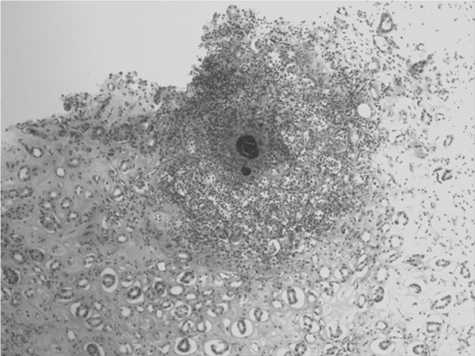
Рис. 7. Почка. Некрозы с густой лейкоцитарной инфильтрацией с колониями кокковой флоры
щим абсцедированием гематомы в области имплантации стента мог послужить рак толстой кишки с распадом. В пользу этого говорят исследования показавшие статистически значимую связь между развитием бактериемии, сепсиса и гнойными метастатическими очагами Streptococcus Bovis у больных колоректальным раком. По различным данным заболеваемость эндокардитом S. Bovis на фоне колоректального рака достигает от 18 до 62% [20 – 26]. Tjalsma H. доказал что колоректальный рак с распадом служит входными воротами инфекции и ассоциируется с бактериемией и инфекция проявляет себя при иммунодефиците [27]. Возможно, что в нашем приведенном случае аденокарцинома толстой кишки с распадом послужила причиной иммунодефицита у пациента и/или являлась входными воротами инфекции и привела к развитию бактериемии что в свою очередь привело к формированию абсцесса на фоне периваскулярной гематомы в области имплантации стента. К сожалению, посевы крови у больного не были взяты и говорить абсолютно уверено об источнике инфекции и виде патогенного штамма мы не можем.
Заключение
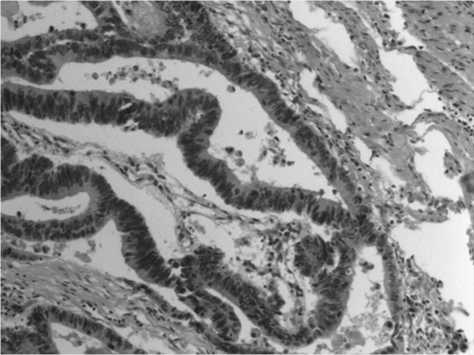
Рис. 8. Аденокарцинома толстой кишки с очагами распада
Коронарная ангиопластика как и любое другое хирургическое вмешательство сопряжено с риском развития инфекционных осложнений, но поиск литературы показал крайне малое количество подобных случаев. Основываясь на анализе 16 случаев инфекционного поражения стента Elieson M. вывел ряд алгоритмов: во всех случаях при возникновении загрудинных болей и повышения температуры у пациентов перенесших стентирование стоит заподозрить инфекционное осложнение связанное с имплантацией стента. После посева крови необходимо начать антибио-тикотерапию препаратами широкого спектра действия для перекрытия MRSA, MSSA и грамотрицательных микроорганизмов. При возникновении инфекции в ранние сроки консервативная терапия может быть эффективна. Однако наилучшие результаты показывает хирургический подход с извлечением или без извлечения имплантированного стента. Лечение антибиотиками должно проводиться парентерально в течение не менее 4 недель. Возможно при подозрении на наличие входных ворот для инфекции целесообразно ограничиваться баллонной ангиопластикой, однако этот вопрос требует более тщательного изучения.
Список литературы Клинический случай: формирование абсцесса в области имплантации коронарного голометаллического стента
- Keeley E.C., Boura J.A., Grines C.L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
- Zijlstra F., Hoorntje J.C., de Boer M.J. et al. Longterm benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl j Med. 1999;341:1413-9. Substudy Investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. N Engl j Med. 1997;336:1621-8. Erratum in: N Engl j Med. 1997;337:287.
- Maehara A., Mintz G.S., Bui A.B. Incidence, morphology, angiographic findings, and outcomes of intramural hematomas after percutaneous coronary interventions: an intravascular ultrasound study. Circulation. 105 2002:2037-2042.
- Mintz G.S., Nissen S.E., Anderson W.D. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement, and reporting of intravascular ultrasound studies (IVUS): a report of the American College of Cardiology task force on clinical expert consensus documents. j Am Coll Cardiol. 37 2001:1478-1492.
- Sigwart U., Puel J., Mirkovitch V., Joffre F., Kappenberger L. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl j Med.1987; 316: 701-706.
- Ramsdale D.R., Aziz S., Newall N., Palmer N., Jackson M. Bacteremia following complex percutaneous coronary intervention. j Invasive Cardiol 2004;16:632-4.
- Cleveland K.O., Gelfand M.S. Invasive staphylococcal infections complicating percutaneous transluminal coronary angioplasty: three cases and review. Clin Infect Dis 1995;21: 93-6.
- Dieter R.S. Coronary artery stent infection. Clin Cardiol 2000; 23(11):808-10.
- Del Pace S. Acute infection-inflammation and coronary stent thrombosis: an observational study. Intern Emerg Med. 2010 Apr;5(2):121-6. Epub 2010 Feb 19 DOI: 10.1007/s11739-010-0350-4
- Marc Elieson. Coronary Stent Infections. Tex Heart Inst j. 2012; 39(6): 884-889.
- Bangher M., Liva P., Baccaro J. Coronary stent infection: case report and definition . Rev Esp Cardiol 2003;56 (3):325-6.
- Golubev N., Schwammenthal E., Di Segni E., Pudil R., Hay I., Feinberg M.S. Echocardiographic imaging of coronary artery abscess following stent implantation. Echocardiography 2004;21(1):87-8.
- Alfonso F., Moreno R., Vergas J. Fatal infection after rapamycin eluting coronary stent implantation. Heart 2005;91(6):e51.
- Gunther H.U., Strupp G., Volmar J., von Korn H., Bonzel T., Stegmann T. Coronary stent implantation: infection and abscess with fatal outcome . Z Kardiol 1993;82(8): 521-5.
- Alfonso F., Moreno R., Vergas J. Fatal infection after rapamycin eluting coronary stent implantation. Heart 2005;91(6):e51
- Grewe P.H., Machraoui A., Deneke T., Muller K.M. Suppurative pancarditis: a lethal complication of coronary stent implantation. Heart 1999;81(5):559.
- Schoenkerman A.B., Lundstrom R.J. Coronary stent infections: a case series. Catheter Cardiovasc Interv 2009;73(1):74-6.
- Garg R.K., Sear J.E., Hockstad E.S. Spontaneous coronary artery perforation secondary to a sirolimus-eluting stent infection. j Invasive Cardiol 2007;19(10):E303-6.
- Wilson W.R, Thompson R.L., Wilkowske C.J., Washington J.A., Giuliani E.R., Geraci J.E. Short-term therapy for streptococcal infective endocarditis. Combined intramuscular administration of penicillin and streptomycin. jAMA. 1981;245:360-363. doi: 10.1001/jama.1981.03310290028017.
- Reynolds J.G., Silva E., McCormack WM. Association of Streptococcus bovis bacteremia with bowel disease. j Clin Microbiol. 1983;17:696-697.
- Leport C, Bure A, Leport J, Vilde JL. Incidence of colonic lesions in Streptococcus bovis and enterococcal endocarditis. Lancet. 1987;1:748.
- Zarkin B.A., Lillemoe K.D., Cameron J.L., Effron P.N., Magnuson T.H., Pitt H.A. The triad of Streptococcus bovis bacteremia, colonic pathology, and liver disease. Ann Surg. 1990;211:786-791. discussion 791-782 DOI: 10.1097/00000658-199006000-00019
- Kok H., Jureen R., Soon C.Y., Tey B.H. Colon cancer presenting as Streptococcus gallolyticus infective endocarditis. Singapore Med j. 2007;48:43-45.
- Malkin J., Kimmitt P.T., Ou H.Y., Bhasker P.S., Khare M., Deng Z., Stephenson i., Sosnowski A.W., Perera N., Rajakumar K. Identification of Streptococcus gallolyticus subsp. macedonicus as the etiological agent in a case of culture-negative multivalve infective endocarditis by 16S rDNA PCR analysis of resected valvular tissue. j Heart Valve Dis. 2008;17:589-592.
- Gupta A., Madani R., Mukhtar H. Streptococcus bovis endocarditis; a silent sign for colonic tumour.Colorectal Dis. 2010;12:164-171 DOI: 10.1111/j.1463-1318.2009.01814
- Tjalsma H., Scholler-Guinard M., Lasonder E., Ruers T.J., Willems H.L., Swinkels D.W. Profiling the humoral immune response in colon cancer patients: diagnostic antigens from Streptococcus Bovis. Int j Cancer. 2006;119:2127-2135 DOI: 10.1002/ijc.22116


