Level of delirium and its contributing factor among patients in ICU
Автор: Amzad S., Barathi S.K., Karpagam K.
Журнал: Cardiometry @cardiometry
Рубрика: Original research
Статья в выпуске: 23, 2022 года.
Бесплатный доступ
Background: Delirium is an acute state of confusion characterized by a rapid onset, usually within hours to days, with changes in consciousness and cognitive changes. Delirium may also present as a form of agitation in intensive care patients. Delirium can affect up to 80% of patients in intensive care units and increase their length of stay and cost of hospitalization. Objectives: The main aim of the study is to evaluate the level of Delirium and its contributing factors among patients in intensive care unit. Methods: A descriptive study design was adopted for the study with 60 samples that met the inclusion criteria and were selected using convenience sampling technique. Data for demographic variables were collected using multiple-choice questionnaires, followed by assessment of delirium using the Confusion Assessment Method (CAM) scale. Results: 20%) had mild delirium, 13 samples (21.7%) of moderate delirium and 13 samples (21.7%) of severe delirium. Regarding the demographic variables of delirium, diabetes rapidly had a statistically significant association with the degree of delirium in ICU patients at p
Delirium, confusion, confusion assessment method (cam) scale, cam-icu and dementia
Короткий адрес: https://sciup.org/148326573
IDR: 148326573 | DOI: 10.18137/cardiometry.2022.23.8993
Текст научной статьи Level of delirium and its contributing factor among patients in ICU
Shaik Amzad, S. Kala Barathi, Karpagam K. Level of Delirium and its Contributing Factor among Patients in ICU. Cardiom- etry; Issue 23; August 2022; p. 89-93; DOI: 10.18137/cardiom-etry.2022.23.8993; Available from: issues/no23-august-2022/level-delirium-contributing
Delirium is an acute state of confusion characterized by rapid onset, usually hours to days, with alterations in consciousness and change in cognition. Delirium also can be manifested as a form of agitation in the critical care patient. [1] Delirium can impact up to 80% of critical care unit care patients and increases their length of stay and cost of hospitalization. Delirium is characterized by rapid onset confusion, depression, as a mood state, can be normal or a symptom of a psychopathologic syndrome or a general medical disorder. Depression is indicated by feelings of sadness, despair, anxiety, emptiness, discouragement, or hopelessness; apathy; or appearing tearful. Unlike delirium, dementia follows an insidious onset and a slow progression, with dementia accompanied by disturbed sleep patterns, memory impairment, and various mood disorders. [2]
The American Psychiatric Association’s Diagnostic and Statistical Manual, 5th Edition (DSMV), delirium, distraction (decreased ability to direct, focus, maintain, and shift) and five key functions that characterize consciousness, these Failures are short-term, usually hours to days, and represent a change from baseline. This also tends to change throughout the day and has additional cognitive impairment. [3]
Nejla TiloucheS et. al., (2018) conducted a study in which a total of 206 patients were enrolled, 167 were not delirium, and 39 (19%) were analyzed for delirium. Patients with delirium had significantly longer duration of mechanical ventilation or stay in the ICU without affecting mortality [4]. Delirium was associated with high incidence of unintentional removal of catheters, Endotracheal tubes and urinary catheters. In multivariable risk regression analysis, age, hypertension, COPD, steroids and sedation were independent risk factors for delirium. Not find a relationship between delirium and mortality. [5] Delirium is frequent in the ICU and is associated with poor outcome. Several risk factors for delirium are linked to intensive care environment. [6]
critically ill patients in the ICU at the Burn, Trauma and Critical Care Research Center at the University of Queensland, Australia. The data collection tool used was a behavioral pain scale for assessing pain and assessing the level of sedation using the Richmond Agitation Scale, and delirium was also screened using the CAM method. The results showed that pain is a contributing factor to the development of delirium, and that dexmedetomidine as a sedative is relatively more effective in preventing delirium than benzodiazepines. [7]
MATERIALS AND METHODS
A total of 60 samples that met the selection criteria were selected for the study using expedient sampling techniques. After sample selection, the researchers introduced themselves and explained the purpose of the study to the patient participants. We obtained the consent after ensuring the trust. Each patient was examined at the bedside. [9] Demographic and clinical variables were collected using a multiple-choice questionnaire and the Confusion Assessment Method (CAM) scale. The data was tabulated and analyzed by descriptive and inference statistics .
RESULTS AND DISCUSSION
The Table 1 shows that, most of the patients in ICU 46(76.7%) had no diabetes mellitus, 59(98.3%) had no liver disease, 43(71.7%) had no hypertension, 47(783%) had no alcoholic history and 46(76.7%) had no present surgical history and shows that, most of the patients in ICU 52(86.7%) had no previous experience of psychosis or seizures, 56(93.3%) had no previous history of head injury, 49(81.7%) of patients were not on sedation, 33(55%) of patients had depression, 31(51.7%) had no metabolic changes, 46(76.7%) had no infection and 48(80%) had the presence of malnutrition.
Table 1
Frequency and percentage distribution of contributing factors of patients in ICU N = 60
|
Contributing Factors |
No. |
% |
|
Comorbidity Factor |
||
|
Diabetes Mellitus |
||
|
Yes |
14 |
23.3 |
|
No |
46 |
76.7 |
|
Liver Disease |
||
|
Yes |
1 |
1.7 |
|
No |
59 |
98.3 |
|
Hypertension |
||
|
Yes |
17 |
28.3 |
|
No |
43 |
71.7 |
|
Alcoholic history |
||
|
1 – 5 years |
6 |
10.0 |
|
6 – 10 years |
5 |
8.3 |
|
11 – 15 years |
2 |
3.3 |
|
No |
47 |
78.3 |
|
Present surgical history |
||
|
Yes |
14 |
23.3 |
|
No |
46 |
76.7 |
|
Previous experience of psychosis or seizures |
||
|
Yes |
8 |
13.3 |
|
No |
52 |
86.7 |
|
Previous history of head injury |
||
|
Yes |
4 |
6.7 |
|
No |
56 |
93.3 |
|
Patient on sedation |
||
|
Yes |
11 |
18.3 |
|
No |
49 |
81.7 |
|
Patient depression |
||
|
Yes |
33 |
55.0 |
|
No |
27 |
45.0 |
|
Presence of metabolic changes |
||
|
Yes |
29 |
48.3 |
|
No |
31 |
51.7 |
|
Presence of infection |
||
|
Yes |
46 |
76.7 |
|
No |
14 |
23.3 |
|
Presence of malnutrition |
||
|
Yes |
48 |
80.0 |
|
No |
12 |
20.0 |
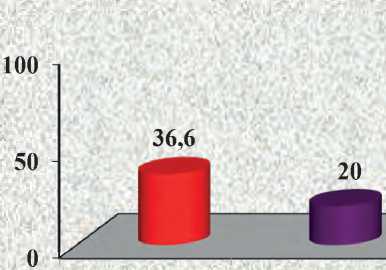
The Table 2 shows that 22(36.6%) had no symptoms, 13(21.7%) had moderate and severe delirium and 12(20%) had mild delirium.
Table 2
Frequency and percentage distribution of level of delirium among patients in ICU.N = 60
|
Level of Delirium |
No. |
% |
|
No symptoms (0) |
22 |
36.6 |
|
Mild Delirium (1) |
12 |
20.0 |
|
Moderate Delirium (2) |
13 |
21.7 |
|
Severe Delirium (3 – 7) |
13 |
21.7 |
The Table 3 shows that none of the contributing factors diabetes mellitus P<0.05 level and the other demographic variables had not shown statistically significant association with level of delirium among patients in ICU.
The present study findings revealed regarding delirium level, none of the demographic variables had shown statistically significant association with level of delirium among patients in ICU. [9]
The present study findings supported by Nejla Ti-louche S. et al. , (2018) reported a study in which a total of 206 patients were enrolled, 167 were not delirium, and 39 (19%) were analyzed for delirium. Patients with delirium had significantly longer duration of mechanical ventilation or stay in the ICU without affecting mortality. [10] Delirium is associated with a high incidence of inadvertent removal of catheters, endotracheal tubes, and urinary catheters. In multivariate risk regression analysis, age, hypertension, COPD, steroids, and sedation were independent risk factors for delirium. [11] There is no link between delirium and mortality. Delirium is frequent in the ICU and is associated with poor outcome. Several risk factors for delirium are linked to intensive care environment. [12]
The present study findings revealed, none of the contributing factors of diabetes mellitus (χ2=10256, p=0.017) had shown statistically significant association with level of delirium among patients in ICU at P<0.05. The present study findings revealed regarding delirium level, none of the contributing factors diabetes mellitus P<0.05 level and the other demographic variables had not shown statistically significant association with level of delirium among patients in ICU. [13]
The present study findings supported by Rodrigo B. Serafim, et.al., (2016) who reported a study which describes subsyndromal delirium (SSD) is a frequent condition and has been commonly described as an intermediate stage between delirium and normal cognition. [14] However, the impact on ICU outcomes that are clinically related to the actual incidence of SSDs
Table 3
Association of level of delirium among patients in ICU with their contributing factors. N = 60
|
Contributing Factors |
No Symptoms |
Mild |
Moderate |
Severe |
Chi-Square Value |
||||
|
No. |
% |
No. |
% |
No. |
% |
No. |
% |
||
|
Comorbidity Facto r |
|||||||||
|
Diabetes Mellitus |
χ2=10.256 d.f=3 p = 0.017 S* |
||||||||
|
Yes |
3 |
5.0 |
0 |
0 |
5 |
8.3 |
6 |
10.0 |
|
|
No |
19 |
31.7 |
12 |
20.0 |
8 |
13.3 |
7 |
11.7 |
|
|
Liver Disease |
χ2=4.068 d.f=3 p = 0.254 N.S |
||||||||
|
Yes |
0 |
0 |
1 |
1.7 |
0 |
0 |
0 |
0 |
|
|
No |
22 |
36.7 |
11 |
18.3 |
13 |
21.7 |
13 |
21.7 |
|
|
Hypertension |
χ2=6.376 d.f=3 p = 0.095 N.S |
||||||||
|
Yes |
2 |
3.3 |
5 |
8.3 |
5 |
8.3 |
5 |
8.3 |
|
|
No |
20 |
33.3 |
7 |
11.7 |
8 |
13.3 |
8 |
13.3 |
|
|
Alcoholic history |
χ2=7.623 d.f=9 p = 0.573 N.S |
||||||||
|
1 – 5 years |
2 |
3.3 |
1 |
1.7 |
1 |
1.7 |
2 |
3.3 |
|
|
6 – 10 years |
0 |
0 |
1 |
1.7 |
2 |
3.3 |
2 |
3.3 |
|
|
11 – 15 years |
0 |
0 |
1 |
1.7 |
0 |
0 |
1 |
1.7 |
|
|
No |
20 |
33.3 |
9 |
15.0 |
10 |
16.7 |
8 |
13.3 |
|
|
Present surgical history |
χ2=1.428 d.f=3 p = 0.699 N.S |
||||||||
|
Yes |
4 |
6.7 |
2 |
3.3 |
4 |
6.7 |
4 |
6.7 |
|
|
No |
18 |
30.0 |
10 |
16.7 |
9 |
15.0 |
9 |
15.0 |
|
S* - Significant N.S – Not Significant
remains unclear. Six eligible studies were evaluated. SSDs were present in 950 (36%) patients. The four studies included only surgical patients. [15] Four studies used the Intensive Care Delirium Screening Checklist (ICDSC) and two confusion assessment (CAM) scores to diagnose SSDs. The use of antipsychotics in
SSD patients to prevent delirium was evaluated in two studies but it did not modify ICU LOS. [16]
Association of level of delirium among patients in ICU with their confusion assessment is shown in Table 4. Percentage distribution of level of delirium among Patients in ICU is shown in Figure 1.
Table 4
Association of level of delirium among patients in ICU with their confusion assessment N= 60
|
Confusion Assessment |
No Symptoms |
Mild |
Moderate |
Severe |
Chi-Square Value |
||||
|
No. |
% |
No. |
% |
No. |
% |
No. |
% |
||
|
Previous experience of psychosis or seizures |
χ2=5.197 d.f=3 p = 0.158 N.S |
||||||||
|
Yes |
1 |
1.7 |
1 |
1.7 |
2 |
3.3 |
4 |
6.7 |
|
|
No |
21 |
35.0 |
11 |
18.3 |
11 |
18.3 |
9 |
15.0 |
|
|
Previous history of head injury |
χ2=8.180 d.f=3 p = 0.042 S* |
||||||||
|
Yes |
0 |
0 |
1 |
1.7 |
0 |
0 |
3 |
5.0 |
|
|
No |
22 |
36.7 |
11 |
18.3 |
13 |
21.7 |
10 |
16.7 |
|
|
Patient on sedation |
χ2=6.529 d.f=3 p = 0.089 N.S |
||||||||
|
Yes |
1 |
1.7 |
2 |
3.3 |
3 |
5.0 |
5 |
8.3 |
|
|
No |
21 |
35.0 |
10 |
16.7 |
10 |
16.7 |
8 |
13.3 |
|
|
Patient depression |
χ2=6.286 d.f=3 p = 0.099 N.S |
||||||||
|
Yes |
10 |
16.7 |
5 |
8.3 |
7 |
11.7 |
11 |
18.3 |
|
|
No |
12 |
20.0 |
7 |
11.7 |
6 |
10.0 |
2 |
3.3 |
|
|
Presence of metabolic changes |
χ2=5.525 d.f=3 p = 0.137 N.S |
||||||||
|
Yes |
8 |
13.3 |
4 |
6.7 |
8 |
13.3 |
9 |
15.0 |
|
|
No |
14 |
23.3 |
8 |
13.3 |
5 |
8.3 |
4 |
6.7 |
|
|
Presence of infection |
χ2=1.858 d.f=3 p = 0.602 N.S |
||||||||
|
Yes |
18 |
30.0 |
8 |
13.3 |
11 |
18.3 |
9 |
15.0 |
|
|
No |
4 |
6.7 |
4 |
6.7 |
2 |
3.3 |
4 |
6.7 |
|
|
Presence of malnutrition |
χ2=2.839 d.f=3 p = 0.417 N.S |
||||||||
|
Yes |
17 |
28.3 |
8 |
13.3 |
12 |
20.0 |
11 |
18.3 |
|
|
No |
5 |
8.3 |
4 |
6.7 |
1 |
1.7 |
2 |
3.3 |
|
N.S – Not Significant

-
■ No symptoms (0)
-
■ Mild Delirium (1)
-
■ Moderate Delirium (2)
-
■ Severe Delirium (3 – 7)
21,7 21,7
No symptoms Mild Delirium Moderate Severe
(0) (1) Delirium (2) Delirium (3 –7)
Level of Delirium
Figure 1. Percentage distribution of level of delirium among Patients in ICU 92 | Cardiometry | Issue 23. August 2022
CONCLUSION
ICU delirium is now becoming a major threat to the health care professionals because many of the studies reveals that the percentage of patients suffering from ICU delirium is being increasing day by day amidst this technological developments. It has really become a challenge for the health professionals to detect ICU delirium at the earliest so that they can prevent the cognitive impairment.Delirium resulted in longer ICU stay, prolonged mechanical ventilation, and exposed our patients to adverse events. Mortality in the ICU was unchanged by delirium.The confusion assessment method (CAM) score is effective in to assess the level of delirium in intensive care unit patients.Delirium resulted in longer ICU stay, prolonged mechanical ventilation, and exposed our patients to adverse events. Thus, nurses shall strengthen the monitoring of delirium, regularly access the patient’s level of calmness, and limit the use of physical restraint.Both critical care physicians and nurses should pay greater attention to the quality of the ICU stay experienced by their older patients.
ACKNOWLEDGEMENT
Список литературы Level of delirium and its contributing factor among patients in ICU
- Nejla Tilouche, S. Souheil El Atrous et al. (2018). Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) clinical care. Journal of Intensive Critical Care Nursing, (2).
- Haozhang. (2017).Delirium prevention post operatively .Journal of Intensive Critical Care Nursing, (2).
- Karthick, S. (2018). Effectiveness of delirium prevention bundle among critically ill patients admitted in intensive care unit at KMCH, Coimbatore (Doctoral dissertation, KMCH College of Nursing, Coimbatore).
- Claudia Disabatino Smith & Petra Grami (2016) Bundles in Delirium Prevention –American Journal Of Nursing research.volume-63.
- Ouimet, S., Kavanagh, B. P., Gottfried, S. B., &Skrobik, Y. (2007). Incidence, risk factors and consequences of ICU delirium. Intensive care medicine, 33(1), 66-73.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-III-R. 3rd ed., rev.Washington, DC: The Association; 1987.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed., text revision. Washington, DC: The Association; 2016.
- Inouye, S. K. (2015). The Confusion Assessment Method (CAM): training manual and coding guide. Boston: Hospital Elder Life Program; 2014.
- Inouye, S. K., van Dyck, C. H., Alessi, C. A., Balkin, S., Siegal, A. P., &Horwitz, R. I. (1990). Clarifying confusion: the confusion assessment method: a new method for detection of delirium. Annals of internal medicine, 113(12), 941-948.
- Bruce, A. J., Ritchie, C. W., Blizard, R., Lai, R., & Raven, P. (2007). The incidence of delirium associated with orthopedic surgery: a meta-analytic review. International psychogeriatrics, 19(2), 197-214.
- Élie, M., Rousseau, F., Cole, M., Primeau, F., Mc- Cusker, J., &Bellavance, F. (2000). Prevalence and detection of delirium in elderly emergency department patients. Cmaj, 163(8), 977-981.
- Inouye, S. K., & Charpentier, P. A. (1996). Precipitating factors for delirium in hospitalized elderly persons: predictive model and interrelationship with baseline vulnerability. Jama, 275(11), 852-857.
- Smith, R. J., Rabinstein, A. A., Cartin-Ceba, R., Singh, V. P., Lachner, C., Khatua, B., ... & Gajic, O. (2022). Chemokines in ICU Delirium: An Exploratory Study. Critical Care Explorations, 4(7).
- Zhu, X., Feng, X., Lin, J., & Ding, Y. (2022). Risk factors of delirium in paediatric intensive care units: A meta-analysis. PloS one, 17(7), e0270639.
- Ishii, K., Kuroda, K., Tokura, C., Michida, M., Sugimoto, K., Sato, T., ... & Morimatsu, H. (2022). Current status of delirium assessment tools in the intensive care unit: a prospective multicenter observational survey. Scientific reports, 12(1), 1-9.
- Mu-Hsing, H. O., Chang, H. C. R., Kee-Hsin, C. H. E. N., HSIAO, S. T. S., & TRAYNOR, V. (2022). Recognizing Intensive Care Unit Delirium: Are Critical Care Nurses Ready? Journal of Nursing Research, 30(3), e214.


