Методы лечения остеохондральных повреждений таранной кости (рассекающий остеохондрит) на современном этапе (обзор литературы)
Автор: Зейналов В.Т., Шкуро К.В.
Журнал: Кафедра травматологии и ортопедии @jkto
Статья в выпуске: 4 (34), 2018 года.
Бесплатный доступ
Рассекающий остеохондрит голеностопного сустава, асептический некроз блока таранной кости или больше известный в зарубежной литературе как остеохондральное повреждение таранной кости (ОХПТК) впервые описано в 1738 году Alexander Munro на основе замеченных им свободных тел в голеностопном суставе, он предположил, что травма это причина их появления. Не смотря на достаточно длинную историю с момента открытия, ОХПТК остаётся и до нашего времени сложной и запутанной проблемой, как в диагностике так и в лечении. Клиническая картина, чаще всего, представлена симптомами которые на первый взгляд могут быть не ясными и не специфичными.С ежегодным ростом технического прогресса появляются новые возможности и увеличивается их доступность для ранней диагностики и лечении ОХПТК.Целью этой работы является тщательный анализ современных данных по этиологии, патогенезу этой сложной медицинской проблемы, оценка современных методов диагностики и лечении ОХПТК на основе их доказательности и результативности.Выводы: Лечение остеохондральных поражений голеностопного сустава является сложной задачей...
Рассекающий остеохондрит, таранная кость, остохондральные повреждения, остеонекроз
Короткий адрес: https://sciup.org/142221771
IDR: 142221771 | УДК: 616.718.71 | DOI: 10.17238/issn2226-2016.2018.4.24-36
Текст обзорной статьи Методы лечения остеохондральных повреждений таранной кости (рассекающий остеохондрит) на современном этапе (обзор литературы)
Рассекающий остеохондрит голеностопного сустава, асептический некроз блока таранной кости или больше известный в зарубежной литературе как остеохондральное повреждение таранной кости (ОХПТК) впервые описано в 1738 году Alexander Munro на основе замеченных им свободных тел в голеностопном суставе, он предположил, что травма это причина их появления. Не смотря на достаточно длинную историю с момента открытия,
ОХПТК остаётся и до нашего времени сложной проблемой, как в диагностике так и в лечении. Клиническая картина, чаще всего, представлена симптомами которые на первый взгляд могут быть не ясными и не специфичными.
С ежегодным ростом технического прогресса появляются новые возможности и увеличивается их доступность для ранней диагностики и лечении ОХПТК.
Целью этой работы является тщательный анализ современных данных по этиологии, патогенезу этой сложной меди-
цинской проблемы, оценка современных методов диагностики и лечении ОХПТК на основе их доказательности и результативности.
Распространённость ОХПТК
Остеохондральное повреждение в голеностопном суставе принято считать проблемой таранной кости, однако существуют и комбинированные повреждения совместно с суставной поверхностью большой берцовой кости, в любом случае это повреждение не является рядовым и часто сопровождает другую патологию голеностопного сустава и даже может являться случайной находкой. Повреждение связочного аппарата голеностопного сустава одна из самых частых травм. Эта тенденция схожа во всех странах мира, как например только в США в год регистрируется до 2 млн таких случаев [1]. Saxena с соавторами в своей работе определили, что повреждение суставного хряща таранной кости, той или иной локализации может встречайся до 50% у пациентов перенёсших травму голеностопного сустава. Костные повреждения этой локализации представляют собой наиболее высокий риск образования ОХПТК [2]. Hintermann с соавторами обнаружил наличие ОХПТК в 73% у пациентов с переломами в области голеностопного сустава [3]. Так же в литературе встречаются ретроспективные работы по выявлению ОХПТК у солдат, данное исследования продолжалось в течение 10 лет и обнаружило наличие этого повреждения в 27 случаях на 100000 человек [4]. С развитием МРТ и КТ появилась возможность определения повреждений подобного характера, даже самого небольшого размера. ХОПТК может встречаться, как у спортсменов, так и у мало активных людей. Существует высокий процент подобных дефектов у кровных родственников имеющий предположительно наследственный и врожденный характер.
Анатомия и патофизиология
Таранная кость одна из редких костей организма которая имеет достаточно большие размеры, не имея области прикрепления мышц. И в этом аспекте она является уникальной. Кровоснабжение таранной кости осуществляется в основном ретроградно за счёт артерии тарзального синуса. Форма тела таранной кости трапециевидная, в среднем передняя поверхность той части таранной кости которая входит в состав голеностопного сустава на 2,5 мм шире, чем ее задняя часть. Кроме того, около 60% таранной кости покрыто суставным хрящом. По сравнению с другими суставами - голеностопный сустав имеет высокую конгруэнтность и как следствие этого толщина суставного хряща таранной кости значительно ниже, чем у других менее конгруэнтных суставов и в среднем составляет 1,11 мм у женщин и 1,35 мм у мужчин [5].
Это относительно тонкий хрящ и менее эластичный, чем более толстое хрящевое покрытие менее конгруэнтных суставов, например такого, как коленный сустав. Недостаток эластичности во многом определяет чувствительность хрящевого покрытия таранной кости к повреждению, а так же к микропереломам лежащей под ним субхондральной кости. Переломы в области голеностопного сустава, такие как переломы лодыжек, приводят к потере естественного хрящевого покрытия, в том числе из-за увеличения контактного давления на таранную кость.
Thordarson с соавторами, продемонстрировали, что смещения при переломе наружной лодыжки с ее укорочением >2 мм или >5° наружной ротацией значительно увеличивает контактное давление в голеностопном суставе [6]. Ransay и Hamilton нашли, что подвывих таранной кости на 1 мм к наружи сокращает контакт суставных поверхностей на 42%, таким образом смещение таранной кости на 2 мм сокращает этот же контакт до 58% [7]. Формирование посттравматического ассиметричного артроза (-вальус, -варус) так же играет важную роль, увеличивая давления на суставные поверхности так при варус-артро-зе на медиальный край таранной кости, так и на латеральный край кости при вальгус-артрозе соответственно [8]. Пациенты с хронической латеральной нестабильностью голеностопного сустава, также попадают в группу высокого риска по образованию остеохондральных дефектов таранной кости. DiGiovannie с соавторами обнаружили, что 14 из 60 пациентов перенёсших оперативное лечение по поводу хронической латеральной нестабильности имели ХОПТК[9]. Ferkel и Chams отметили, что 95% пациентов перенёсших операцию по Broström по поводу латеральной нестабильности голеностопного сустава имели те или иные признаки внутрисуставной патологии [10]. Gregush и Ferkel выявили, что пациенты с ХОПТК в комплексе с нестабильностью голеностопного сустава имеют результат лечения хуже, чем пациенты только с нестабильностью [11].
Повреждение суставного хряща приводит к появлению непокрытого участка нижележащей субхондральной кости, что в свою очередь приводит к увеличению влияния внутрисуставного давления на обнаженный участок субхондральной кости , и дальнейшему повреждению последней [12]. Длительное воздействие внутрисуставного давления на этот участок может негативно влиять на костную ткань, вызывая развитие склероза, остеолиза, а в конечном итоге крупных дефектов и кистозного перерождения. Выше перечисленные обстоятельства, создают порочный круг, таким образом по мере продолжающегося повреждения субхондральной кости увеличивается её неспособность удерживать хрящевое покрытие приводя к более обширному отслоению суставного хряща, а ввиду хорошей иннервации, пациенты с подобным характером повреждения испытывают выраженный болевой синдром, который становится более интенсивным после образования субхондральной кисты или многочисленных кист в месте повреждения [13].
Наиболее распространенной локализацией остеохондраль-ных повреждений таранной кости является переднелатеральной и заднемедиальной край суставной поверхности таранной кости. Исследование, основанное на изучении МРТ данных, проведенное Hembree с соавт. [14], определило, что большинство выявляемых локализаций остеохондральных повреждений таранной кости располагались медиально и центрально [15]. Независимо от этого, латеральная локализация данных повреждений связана с травмой от 93% до 98% случаев. Однако, было отмечено, что повреждения латеральной локализации в основном имеют меньшую и правильную овальную форму и возникают при эверсионных движениях в максимальном подошвенном сгибании стопы [16]. Медиальные повреждения связаны с острой травмой реже, от 61% до 70% [5]. Считается, что медиальные поврежде- ния, вызваны повторяющейся микротравмой, вызванной соударением медиального края суставной поверхности таранной кости о суставную поверхность большеберцовой кости в момент максимальной супинации стопы. Медиально локализующиеся повреждения глубже, кратерообразной формы, и образуются при максимальном подошвенном сгибании стопы [16]. Остео-хондральные повреждения с центральной локализацией имеют мультифакторный механизм образования и наиболее сложны в плане хирургического лечения (рис. 1).
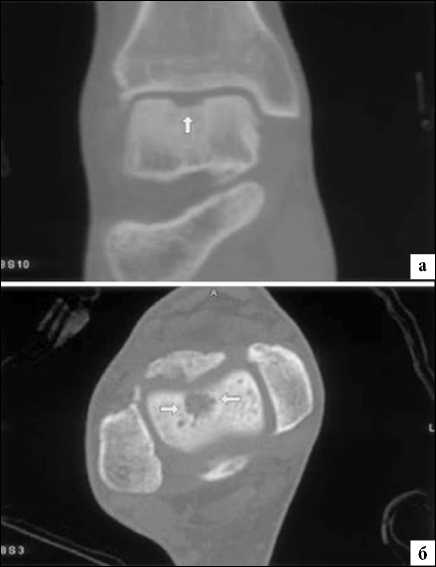
Рис. 1. Центральная локализация ОХДТК
Известно, что атравматическая этиология развития ХОПТК вносит свой вклад развитие и появление этих поражений, но отсутствует какая либо доказательная база данных, четко регламентирующая этот факт.

Рис. 2. Артроскопическая визуализация центрально-медиального повреждения суставной поверхности дистального отела большеберцовой кости, через передне-медиальный артроскопический доступ правого голеностопного сустава
Биполярные остеохондральные поражения - поражения суставных поверхностей дистального отдела большеберцовой и таранной костей
Остеохондральные поражения дистального отдела большеберцовой кости, встречаются гораздо реже, чем подобные поражения таранной кости, а двухполярные поражения большеберцовой и таранной встречаются еще реже. Elias с соавт. оценили МРТ исследование 38 пациентов с остеохондральными поражениями суставной поверхности дистального отдела большеберцовой кости для определения наиболее часто встречающейся локализации последних. Они обнаружили, что центральная, задняя и медиальная локализация встречалась наиболее часто (21%), так же в рамках этого исследования было выявлено, что биполярные поражения имелись в 6 из 38 случаев, и истинные “целующиеся” поражения только в 1 случае [17]. На большом количестве примеров ( 880 процедур) лечебно-диагностических артроскопических оперативных вмешательств голеностопного сустава, Mologne и Ferkel нашли только 23 пациента (2,6%) с остеохондральными поражениями суставной поверхности дистального отдела большеберцовой кости и только 6 пациентов (<1%) с биполярным поражением [18]. Большинство из выявленных ими локализаций располагались задне-центрально [19]. Несмотря на редкую встречаемость, важно знать об этих поражениях и тщательно оценивать большеберцовую кость во время диагностики. Не выявленные поражения большеберцовой кости могут привести к трудностям в реабилитации пациента и, в конечном счете, к неудовлетворительному результату лечения.
Клинические данные
Диагностика остеохондральных поражений таранной кости является трудной задачей и может создать сложности в понимании как для пациента, так и для врача. Большинство пациентов относятся подозрительно к подобному роду медицинских заключений т.к. они, в большинстве случаев, отмечают небольшую травму в анамнезе, последствия которой, по их ощущениям, нивелировались через несколько недель и болевые ощущения в голеностопном суставе появляются только при физической активности. Как правило, пациенты жалуются на боль в голеностопном суставе, только, во время или после физической активности. Loomer с соавт. в своей работе сообщают, что 94% пациентов с ОХПТК у которых были жалобы на боль в голеностопном суставе только при физической активности в 89% имели в анамнезе травму голеностопного сустава, которую они сочли незначительной [20]. При более длительном анамнезе пациенты отмечают постоянный отек и ограничение движений в области голеностопного сустава в сочетании с постоянной болью. В отдельных случаях могут присутствовать механические симптомы: щелчок, блокировка и чувство нестабильности, особенно на стадии фрагментации и дислокации некротизированного фрагмента таранной кости [21]. Этот факт не является общим симптомом, но может свидетельствовать о более серьезной стадии процесса [20].
Клиническое обследование может быть относительно неспецифичным при ОХПТК, но наиболее распространенным является выявление болезненности в проекции передних отделов голеностопного сустава локализующихся по линии сустава. Это тестируется наиболее точно при в положении максимального подошвенного сгибания стопы и голеностопного сустава, в результате чего переднелатеральные и переднемедиальные поверхности суставной поверхности таранной кости оказываются в более доступном положении. Болевые ощущения, проецирующиеся за медиальной лодыжкой при максимальном тыльном сгибании, могут свидетельствовать о заднемедиальной локализации поражения. Многими клиницистами было отмечено, что пациенты, с локализацией ОХПТК у медиального края суставной поверхности, могут предъявлять жалобы на боль только в передне-латеральной области голеностопного сустава. Объяснений этому, не логичному обстоятельству было предложено множество, такие как: отражённая боль или боль в результате неосознанной перегрузки латеральных отделов голеностопного сустава на фоне страдания медиальных отделов и др., однако, не одна из причин до настоящего времени не была убедительно доказана. Пациент с ОХПТК часто испытывает диффузную, неспецифическую болезненность, а локализация болезненности не является надежным индикатором локализации поражения. Стабильность голеностопного сустава следует оценивать с помощью определения симптомов переднего и заднего выдвижного ящика, а также инверсионных и эверсионных тестов. Тестирование стабильности голеностопного сустава, должно быть выполнено при согнутом коленном суставе, для избегания получения не объективной картины диагностики на фоне натяжения икроножной мышцы. Оценка функции подтаранного сустава, является так же обязательной процедурой для исключения патологии со стороны последнего, например, такой, как таранно-пяточная коалиция. При дифференциальном диагнозе всегда следует учитывать другие патологические состояния голеностопного сустава: им-пиджмент синдромы различной локализации, проблемы со стороны дистального межберцового синдесмоза, нестабильность голеностопного сустава, артрит или стресс-перелом.
Лучевая диагностика ОХПТК и классификация
Не смотря на то, что Loomer с соавт. сообщили, что только от 50% до 66% остеохондральных дефектов обнаруживаются при помощи обычной рентгенографии, данный метод является важной отправной точкой и может быть полезен для исключения другой патологии голеностопного сустава [20]. Рентгенологическое исследование голеностопного сустава должно включать переднюю, заднюю и в ¾ внутренней ротации проекции. Все проекции выполняются стоя (под нагрузкой) и называются функциональными. Функциональные рентгенограммы могут быть полезны для выявления сопутствующей нестабильности голеностопного сустава, проекция ¾ во внутренней ротации, помогает в визуализации щели межберцового синдесмоза, а так же отображает передне-внутрений импижмент (таранной и большеберцовой кости) в случае его наличия. Выполненные в положении подошвенного сгибания прямая и ¾ проекция во внутренней ротации могут быть полезны в выявлении заднемедиального поражения таранной кости. Рентгенологические признаки, которые могут быть определены, варьируются от небольших участков сдавления субхондральной кости до крупных отслоенных остеохондральных фрагментов. Радиографическая система классификации была разработана Berndt и Harty в 1959 году и остается золотым стандартом. (Табл. 1) [16]. Loomer с соавторами дополнили имеющуюся классификацию, на основе не только рентгенограмм, а также МРТ (магнитно-резонансная томография) и КТ (компьютерная томография), и добавили стадию V в систему классификации Berndt и Harty [22].
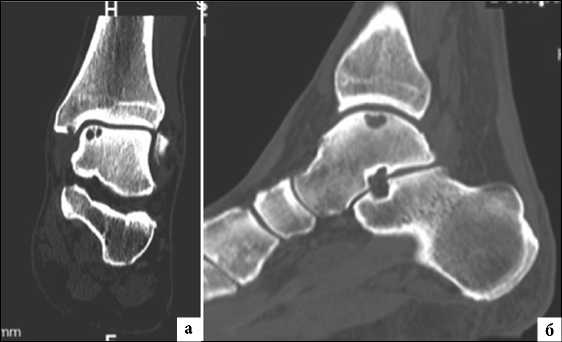
МРТ является ценным инструментом в комплексе диагностики ОХПТК для оценки отека костной ткани, а также выявления скрытых повреждений субхондральной кости и хрящевого покрытия, которые могут быть пропущены при стандартных рентгенограммах или даже КТ. МРТ – самый лучший инструмент оценки для определения стабильности и жизнеспособности фрагмента таранной кости при его отслоении и эта информация может быть решающей в тактике выбора того или иного метода хирургического лечения. Однако, для определения размеров отслоившегося фрагмента таранной кости наилучший метод - КТ, так как данные размеров по МРТ могут не соответствовать действительности в сторону переоценки последних. Hepple с соавторами изучив многочисленные данные МРТ диагностики разработали систему классификации ОХПТК на основе этого метода (Табл. 2) [23]. Однако, наиболее широко принятая система классификации, основанная на КТ-это классификация Ferkel и Sgalione (Табл. 3; Рисунок 4) [24]. Классифицировать ОХПТК также возможно выполнить интраоперационно, на основе артроскопических данных о состоянии остеохондрального поражения. Наиболее широко используется система Ferkel/Cheng (Табл. 4) [25], эта система классификации, в отличие от обычных рентгенограмм, КТ и МРТ, лучше всего взаимосвязана с исходами лечения пациентов.

Рис. 3. Сагитальная проекция магнитно-резонансной томографии голеностопного сустава с визуалзацией биполярного «целующегося» остеохондрального повреждения суставной поверхности дистального отдела большеберцовой кости и суставной поверхности таранной кости
Таблица 1.
Радиографическая классификация по Berndt и Harty
Уровень E
Наличие свободного не дислоцированного костного фрагмента
Таблица 3
Классификация по Ferkel и Sgalione, на основе компьютерной томографии
|
I стадия |
неповрежденный суставной хрящ с наличием субхондральной кисты под ним |
|
IIa стадия |
субхондральная киста имеет связь с полостью сустава |
|
IIб стадия |
открытая субхондральная киста с наличием недислоци-рованного и неотслоившегося костного фрагмента |
|
III стадия |
открытая субхондральная киста с наличием недислоци-рованного полностью отслоившегося костного фраг мента |
|
IV этап |
открытая субхондральная киста с наличием дислоцированного костного фрагмента |
Таблица 4
Ferkel и Cheng предложили артроскопическую классификация костно-хрящевого повреждения голеностопного сустава
|
Уровень A |
Хрящ в месте повреждения гладкий, интактный, но мягкий или баллотирующий |
|
Уровень B |
Поверхность хрящевого покрытия в месте повреждения грубая, шероховатая |
|
Уровень C |
Поверхность хрящевого покрытия в месте повреждения с наличием фибрилляций/трещин |
|
Уровень D |
Поверхность хрящевого покрытия в месте повреждения с наличием отслоения по краю или истончена до костной ткани |
|
I стадия |
субхондральная импрессия (импрессионный перелом) |
|
II стадия |
частичная отслойка остеохондрального фрагмента |
|
III стадия |
полностью отсоединенный фрагмент без смещения от области отслоения |
|
IV стадия |
отрывной и дислоцированный фрагмент |
|
V стадия |
дополнительно к стадии IV присутствует субхондральная киста |
Уровень F
Дислоцированный костный фрагмент
Классификация по Hepple на основе МРТ
Таблица 2
|
I стадия |
повреждение суставного хряща |
|
IIa стадия |
повреждение суставного хряща с импрессией субхондральной кости и отеком костного мозга (острое повреждение) |
|
IIb cтадия |
повреждение суставного хряща с импрессией субхондральной кости без отека костного мозга (хроническое повреждение) |
|
III стадия |
отслоившийся фрагмент субхондральной кости, без его дислокации (суставная жидкость полностью окружает фрагмент) |
|
IV стадия |
дислоцированный фрагмент субхондральной кости, участок дефекта от места дислокации |
|
V стадия |
IV стадия + наличие субхондральной кисты |
Рис. 4. Кистозное ОХПТК медиального края таранной кости. (а) Компьютерная томография (КТ) в коронарной проекции показывает мультикистозный характер поражения.
(б) Сагиттальная проекция КТ показывает глубину кистозной перестройки субхондральной кости и локализацию относительно передне-заднего направления суставной поверхности таранной кости
Лечение
Существует ряд важных условий, которые необходимо учитывать при выборе соответствующего лечения для остеохон-дрального поражения (Табл. 5). Алгоритм принятия решения при лечении остеохондральных дефектов таранной кости, может быть полезен при выборе способа хирургического лечения (Рис. 5).
Таблица 5
Необходимая информация для определения тактики лечения ОХПТК
|
Тип поражения |
|
|
Стабильность поражения |
- Стабильный - Нестабильный |
|
Дислокация костного фрагмента |
- Дислоцированный - Недислоцированный |
|
Активность процесса |
- Острый - Хронический |
|
Размер поражения |
|
|
Местоположение |
|
|
Ограниченность процесса |
|
|
Анамнез лечения |
- Первичное - Ревизионное |
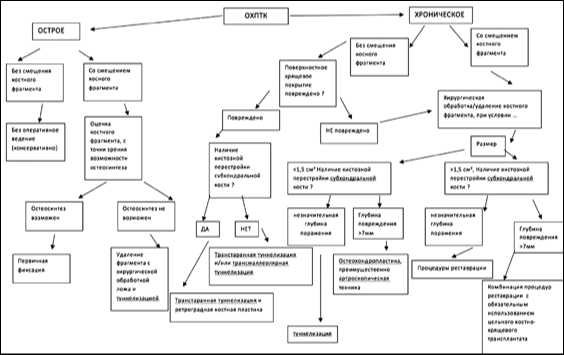
Рис. 5. Алгоритм принятия решения при лечении остеохондральных повреждений таранной кости (ОХПТК). Процедуры реставрации включают Лечение ОХПТК с помощью костной пластики аллотрансплантатом, аутотрансплантатом, имплантация аутологичных хондроцитов (ACI) и пластика фрагментированным, ювенильным аллотрансплантатом хрящевой ткани.
Консервативное лечение
В большинстве случаев этап нехирургического лечения для пациентов с ОХПТК гарантирован, особенно при острых повреждениях. Консервативное лечение в основном заключается в иммобилизации и полной разгрузки конечности на срок от 4 до 6 недель. Консервативное лечение показано для пациентов, имеющих поражение по классификации по Berndt и Harty I и II стадии и начальной стадии III и это лечение, особенно актуально у пациентов в возрасте до 18 лет. Цель лечения – не регенерировать хрящевое поражение, а ликвидировать боль в голеностопном суставе с возвращением обычной для пациента функциональной активности. Изредка, у пациентов молодого возраста, эти повреждения могут восстановится и без применения лечебных мероприятий. И следует не забывать тот факт, что более молодые пациенты всегда будут иметь лучшие результаты лечения при применении нехирургического метода лечения, чем пациенты более старшего возраста.
В своей статье Berndt и Harty сообщили о высоком уровне неудовлетворительных исходов лечения при применении консервативных методов: хорошие в 9%, удовлетворительные 16% и неудовлетворительные в 75% случаев. Zengerink с соавт. в большом системном обзоре нехирургического лечения сообщили 45% успешных исходов у пациентов, получавших лечение с разгрузкой конечности, и 53% успешных исходов у пациентов, получавших разгрузку и иммобилизацию голеностопного сустава [26]. Klammer с соавторами ретроспективно оценили 48 пациентов с МРТ-подтвержденными ОХПТК, получавших консервативное лечение с минимальным сроком наблюдения 2 года. Отмечено, что у 86% пациентов или полностью купирован болевой синдром или уменьшилась интенсивность болевого синдрома. Артрозные изменения не были выявлены в 47%, а в оставшихся 53% ар-трозные изменения не превышали 1 и 2 степень, несмотря на то, что МРТ не выявило существенных изменений по площади поражения на фоне лечения. Интенсивность болевого синдрома и его корреляция, во всех случаях была связана с глубиной поражения таранной кости, выявленным при первичном МРТ, формированием субхондральных кист, а также наличием отека костного мозга [27].
Оперативное лечение
Целью оперативного лечения является восстановление анатомии суставной поверхности таранной кости с целью восстановить амплитуду движений и физическую активность пациента. Артроскопическая хирургия является в настоящее время наиболее распространенным методом лечения ОХПТК, поскольку минимизирует повреждения мягких тканей и костных структур. Это также позволяет хирургу и пациенту избежать осложнений, значительно уменьшает вероятность некроза мягких тканей и инфекционные осложнения, сокращает время госпитализации [10,28]. Артротомия с остеотомией или без нее показана пациентам с ОХПТК имеющих большую площадь и глубину или определенную локализацию. Muir и Amendola обнаружили, что 17% поражений медиальной локализации и 20% латеральной локализации не доступны артроскопически [29]. Однако, с развитием современной артроскопической техники показания к артротомии неуклонно уменьшаются.
Фиксация
Хирургическое лечение с остеосинтезом, применимо только в острых случаях краевых переломов, с хорошо сохраненной суставной поверхностью на поверхности отколовшегося фрагмента суставной поверхности таранной кости, по данным литературы, для этого используют самые разные фиксаторы, так называемые безшляпочные винты, биодеградируемые винты и даже спицы [30]. Kumai с соавт. сообщили об успешном исходе 89% случаев с фиксацией больших, свободных фрагментов суставной поверхности таранной кости [31]. При выполнении подобной манипуляции авторы отмечают необходимость ревизии зоны перелома, для удаления возможного интерпонента и стимуляции «материнской» костной ткани путем хирургической обработки (дебридмента) и туннелизации. Техника фиксации “LIFT” повреждений - отколовшегося и перевернувшегося фрагмента латеральных отделов блока таранной кости (lateral, inverted, fracture, talus), как метод репозиции и ревизии отломков и зоны остеохондральных переломов таранной кости была описана Dunlap и Fenkel в 2013 году (Рисунок 6)[32]. Было отмечено, что эти повреждения хорошо реагируют на раннее открытое оперативное вмешательство и фиксацию, при этом у 6 из 10 пациентов наблюдалась хорошая (близкая к «отличной») функция голеностопного сустава на 9-летнем сроке наблюдении. Kerkhoffs с соавторами описали метод LIFT, DRILL, FILL и FIX (LDFF) (приподнимание, перфорация, заполнение дефекта и фиксация) в тактике лечения острых и хронических ОХПТК с жизнеспособным крупным костным фрагментом удовлетворительного качества [33].

Рис. 6. Техника фиксации LIFT (lateral inverted osteochondral fracture of the talus) ОХПТК переднелатеральной локализации
Методы связанные с удалением фрагмента субхондральной кости и обработкой «материнского» ложа
Небольшой, нежизнеспособный, частично или полностью дислоцированный фрагмент остеохондральной кости может быть удален, нижележащее субхондральное ложе требует при этом хирурургической обработки. В описании 13 случаев удаления фрагмента субхондральной кости Zengerink с соавт. описали 77% успешных результатов [26]. О'Farrell и Costello проведя анализ 24 пациентов с 4-летним наблюдением после открытого удаления субхондального фрагмента таранной кости. Они отметили, что у 15 пациентов были хорошие функциональные результаты, удовлетворительные у 9 пациентов, и не удовлетворительный результат не был отмечен ни в одном случае [34]. Основной целью хирургической обработки области отслоения субхондрального фрагмента состоит в том, чтобы стабилизировать кость и суставной хрящ в границах поражения и создать среду, которая будет способствовать образованию фиброхрящевой ткани (грубо-волокнистый хрящ). Предварительно, необходимо определить точный размер повреждения для последующей оценки качества и эффективности лечения на контрольных исследованиях (Рис. 7).

Рис. 7. Измерение большого ОХПТК левого голеностопного сустава. Визуализация через заднелатеральный артроскопический доступ.
Туннелизация ОХПТК
В редких случаях, когда поверхность суставного хряща интактна и отсутствует костный фрагмент, одним из предпочтительных методов хирургического лечения может быть прямая или ретроградная туннелизация области ОХПТК при помощи спиц (например: Kirschner 0.045 дюймов). Если есть какие-либо признаки разрушения хрящевой поверхности, целью тунне-лизации является, индуцирование кровоснабжения в области ОХПТК, что впоследствии стимулирует образование новой костной ткани. Несколько исследований проведенных с использованием этой методики выявили высокую вероятность успеха при подобном сценарии. В случае переднелатерального поражения туннелизация может осуществляться с помощью одного или двух стандартных передних артроскопических доступов. Для заднемедиальных поражений использование переднего доступа невозможно, чаще всего используют классический трансмаллеолярный открытый доступ, однако в литературе встречается описание артроскопической техники при этой локализации поражения с применением трансмалеолярного (антеградного) или трансталярного (ретроградного) эндоскопического доступа.
Хирургическая обработка и стимуляция регенерации костной ткани для нестабильных ОХПТК
Стимуляция костного мозга включает в себя удаление нестабильных дефектов хрящевого покрытия и любой лежащей в его основе некротической кости с последующей туннелизацией субхондральной кости. Туннелизация, помимо механической стимуляции регенераторных процессов, по средствам исходящей крови из отверстий в субхондральной кости образует кровяной сгусток внутри поражения. Этот сгусток содержит костномозговой детрит, состоящий в том числе и из мезенхимальных стволовых клеток, что приводит к формированию в первую очередь костной ткани и грубоволокнистой хрящевой ткани. Отверстия и костные каналы при тунеллизации располагаются приблизительно на расстоянии 5 мм друг от друга и до 3-4 мм в глубину. Chen с соавт. доказали, что большая глубина туннелизации (до 6 мм), приводит к более хорошим результатам, даже при использовании более тонких средств для туннелизации, чем туннели-зация на меньшую глубину (2 мм). Авторы продемонстрировали лучшее заполнение дефекта хрящевого покрытия, более высокий процент гиалинового хряща в регенерате и увеличенное количество гликозаминогликана в составе хрящевой ткани [35]. Существуют несколько ключевых моментов, которые могут помочь осуществить доступ и обработать поражения заднемедиальной локализации суставной поверхности таранной кости (Табл. 6).
Таблица 6
Некоторые ключевые моменты при хирургическом (артроскопическом) лечении ОХПТК заднемедиальной локализации
|
1. |
Выполняйте переднемедиальный доступ как можно ближе к сухожилию задней большеберцовой мышцы |
|
2. |
Выполняйте переднелатеральный доступ центральнее на сколько это возможно |
|
3. |
Обеспечьте хорошую визуализацию суставных поверхностей для этого разведите их максимально |
|
4. |
Угол заднелатерального доступа к области поражения должен быть выполнен под поперечной межберцовой связкой. |
|
5. |
Оснащение хирургическим оборудованием должно быть адекватным |
Chuckpaiwong с соавт. отметили высокий положительный исход лечения у всех пациентов с поражением размером менее 15 мм, с гораздо более худший результат у тех пациентов у которых размер ОХПТК был более 15 мм. [36]. Choi и соавт. отметили, что 10.5% неудачных результатов, при использовании метода микрофрактурирования при лечении ОХПТК, была связана с площадью ОХПТК. Указанный выше процент наблюдался у пациентов с площадью поражения менее 150 мм2, если дефект был >150 мм², процент неудачных результатов возрастал до 80%. [37, 38]. Choi с соавт. также рассмотрели прогностическое значение ограниченности процесса. Они обнаружили, что ОХПТК неограниченного типа с продолжающейся отслойкой хрящевого покрытия имели значительно худшие исходы, чем более ограниченные поражения. [37, 38]. Shuman с соавт. изучили результаты лечения 38 пациентов с хирургической обработкой и микро-фрактурированием на протяжении, в среднем 4,8 года с момента операции, по результатам исследования они получили хорошие и удовлетворительные результаты при оценке по шкале Ogilvie Harris в 86% случаев при условии первичного оперативного вмешательства. Интересным так же, является то, что они получили 75% хороших результатов у пациентов, перенесших операции вторично при этой патологии [39]. Ferkel с соавт. оценили результаты хирургического лечения пациентов с ОХПТК в сроки наблюдения до 71 месяца и выявили, что у 72% пациентов получены хорошие результаты, однако, они рассмотрели подгруппу из 17 пациентов, оцененных по тем же параметрам 5 лет назад, и обнаружили, что у 35% из них результаты уменьшились на 1 балл (шкала Ogilvie Harris), это наблюдение позволило предположить, что результаты микрофрактурирования при ОХПТК могут ухудшаться при длительном наблюдении в отдельных случаях [40]. Van Bergen и др. обследовали пациентов, которым проводилось микрофрактурирование таранной кости по поводу ОХПТКв течение 12 лет. Они получили хорошие и удовлетворительные результаты по шкале Ogilvie Harris в 78%, средний балл по шкале AOFAS был 88. 94% пациентов вернулись к привычной для них трудовой деятельности и 88% возобновили спортивную нагрузку [41]. Clanton c соавт. оценили результаты лечения пациентов с большими (в среднем 70 мм) размерами поражениями, после выполнения методики микрофрактурирования, срок наблюдения, в среднем составил 26 месяцев, отмечено, что большинство пациентов были удовлетворены результатами лечения (8/10), для тех пациентов, которые остались недовольны результатом, в основной своей массе, данная операция носила ревизионный характер [42].
Хирургическая обработка и стимуляция регенерации костной ткани для ОХПТК с наличием сухондральной кисты
ОХПТК с кистозной перестройкой субхондральной кости могут иметь костный фрагмент, который в основной своей массе нежизнеспособен. Фрагмент должен быть удален, а стенки кистозной перестройки туннелизированы или микрофрактури- рованы с последующей костной пластикой алло- или аутотрансплантатом (Рис. 8).

Рис. 8. Костная аутопластика субхондральной кисты таранной кости левого голеностопного сустава через переднемедиальный артроскопический доступ. Визуализация через заднелатеральный артросопический доступ к голеностопному суставу.
Лечение остеохондральных повреждений суставной поверхности дистального отдела большеберцовой кости — хирургическая обработка, стимуляция регенерации костной ткани и костная пластика.
Большинство остеохондральных повреждений суставной поверхности дистального отдела большеберцовой кости подлежат хирургическому лечению с удалением некротизировано-го участка, туннеллизацией и/или микрофрактурированием. В редких случаях больших дефектов могут быть использованы костные аллотрансплантаты и аутотрансплантаты с ретроградной установкой. Ueblacker с соавторами описали технику и их опыт выполнения этой процедуры [43].
Лечение ОХПТК с помощью костной аутопластики
ОХПТК с большими кистозными подхрящевыми дефектами (по Berndt и Harty стадия V) часто требуют дополнительного костно-пластического материала для заполнения структурного дефекта. Эта тенденция прослеживается в результатах последних научных работ, использовать в этом случае только хирургическую обработку и микрофрактурирование или туннелизацию является недостаточным [44,45]. Кистозная перестройка субхондральной кости с дефицитом костной ткани от 6 до 10 мм может быть заполнена костно-хрящевым трансплантатом одномоментно при использовании любого из известных на сегодняшний день хирургических наборов для остеохондропластики по системе OATS (osteochondral autogaft transplant system), а некоторые из них позволяют замещать дефекты до 15 мм [46]. Донорских зон для взятия аутотрансплантатов несколько, включая бугор пяточной кости, ненагружаемая зона латерального и медиального мыщелка бедренной кости, а так же бугристость большеберцовой кости. Область кистозной перестройки в любом случае должна быть тщательно обработана используя туннелизацию или удалена для создания ложа для трансплантата заранее известной формы и размера. Важным моментом при использовании кост- но-хрящевой аутотрансплантации, является правильное ориентирование аутотрансплантата, поскольку выступающая его хрящевая более 1 мм, приведет к разрушению хрящевого покрытия аутотрансплантата и к травмированнию контактного с ним хряща суставной поверхности большеберцовой кости. Sammarco и Makwana использовали трансплантаты из области задней поверхности таранной кости на пораженной стороне и отследив отдельные клинические наблюдения в сроки до 2-х лет с момента операции отметили улучшение, соответствующее измерениям по шкале AOFAS от 64.4 до 90.8 [47]. Emre и др. изучив 2-х летние исходы лечения 32 пациентов, с использованием техники мозаичной хондропластики, костно-хрящевыми трансплантатами из не нагружаемой зоны наружного и/или внутреннего мыщелка бедренной кости и получили значительное улучшение по шкале AOFAS в этих случаях зафиксировав 59.1 балл до операции, и 87.9 после проведенного лечения. Боль в области забора трансплантата(ов) в сроки более 6 мес. не наблюдалась ни в одном из описанных случаев. [48]. Kennedy и Murawski провели лечение 72 пациентов (средний возраст 34.2 года) с использованием костно-хрящевых трансплантатов из не нагружаемой зоны наружного и/или внутреннего мыщелка бедренной кости с добавлением концентрированного костно-мозгового пунктата (Bone Marrow Aspirate Concentration (BMAC)). При 28-месячном наблюдении этих пациентов результаты лечения были более чем удовлетворительные и доказательно оценены в балах по шкале FAOS и по шкале SF-12, подтверждая хороший результат лечения, и только 3 пациента из этой группы наблюдения, отмечали болевые ощущения в области забора аутотрансплантата(ов) в срок наблюдения через 2 года после операции [49].
Лечение ХОПТК с помощью костной аллопластики
ХОПТК с кистозными подхрящевыми дефектами, имеющие размеры больше, чем 12 мм × 16 мм, для замещения требуют, взятие 2-х и более трансплантатов при условии использования аутопластического материала [46]. Учитывая то, что донорская область при многократных забора аутотрансплантата может иметь осложнённый характер течения в послеоперационном периоде, а использование двух и более донорских зон увеличивает риск осложнений многократно при значительных костных дефектах на фоне ОХПТК рекомендуется использовать аллотрансплантат. Известно что, полученные аллотрансплантаты должны использоваться в течение 21 дня после забора, чтобы увеличить шансы на выживаемость хондроцитов и вероятность успешного результата лечения [19]. Литературные источники использования аллотрансплантатов ХОПТК весьма редки. Raikin и др. описали ряд пациентов с дефектами таранной кости больше, чем 3 см в диаметре, которым выполнялась пластика аллотрансплантатами и фиксация компрессионными каннюлированными винтами. Авторы сообщили, что оценка на основании баллов шкалы AOFAS показала положительную послеоперационную динамику, от 42 до 86 балов в 2-летнем сроке наблюдения [17]. Bugbee с соавторами сообщил о хороших и удовлетворительных результатах у 5 из 12 пациентов с большим остехондральным дефектом таранной кости, которым было проведено лечение с использованием аллотрансплантатов и только у одного из этих пациентов в конечном счете был выполнен артродез голеностопного сустава [24]. В ретроспективном обзоре, Kelikian и др. провели оценку 38 пациентов, которым была проведена аллопластика таранной кости по поводу ОХПТК, срок наблюдения в среднем составил 38 месяцев с момента операции. На основании подсчёта по шкале AOFAS отмечено улучшение в среднем от 52 до 79 баллов, и 28 из 38 пациентов отметили значительное улучшение функции сустава после проведенного лечения. Неудовлетворительный результат был отмечен только у 4 пациентов [50].
Лечение ОХПТК методом имплантации аутологичных хондроцитов
Имплантации аутологичных хондроцитов (ACI) была впервые экспериментально разработана у кроликов, а затем введена медицинскую практику в качестве потенциального решения для хрящевых дефектов коленного сустава [51]. Методика впоследствии была разработана и для остеохондральных поражений таранной кости. В этой процедуре аутологичные хондроциты традиционно забирают из ненагружаемой зоны коленного сустава в области мыщелков бедренной кости, культивируют in vitro и имплантируют в дефект таранной кости через определенное время при повторном вмешательстве. Более современные источники описывают забор хондроцитов с суставной поверхности повреждённой таранной кости, уменьшая частоту послеоперационных осложнений донорской зоны [52, 53]. Первое поколение, или классический ACI, использует аутологичный периостальный лоскут для покрытия имплантированной клеточной субстанции. ACI второго поколения включает клетки хрящевой ткани на несущей матрице. Матрично-индуцированный ACI (MACI) включает размещение клеток на искуственносозданую тканевую мембрану выполняющую роль матричной основы и готовая к имплантации. Показания и противопоказания к применению MACI приведены в таблицах 7 и 8.
Таблица 7
Показания к мплантации аутологичных хондроцитов (ACI) в область голеностопного сустава
|
Общие показания: |
Относительные показания: |
|
Возраст от 15 до 55 лет |
Многочисленые униполярные поражения |
|
Одиночный дефект |
Неотграниченые поражения |
|
Односторонний (униполярный) дефект (затронута только таранная кость) |
|
|
Отграниченный дефект |
|
|
Краевой дефект |
|
|
Рецидив после предыдущей операции |
|
|
Большие поражения с обширными субхондральными кистозными изменениями |
Несмотря на то, что применение этой методики осложняется её высокой стоимостью в отличии от других методов, результаты лечения, на основании последних исследований, весьма обнадеживающие. Kwak с соавт. сообщили о 29 пациентах, которые прошли лечение с применением ACI после неудачной попытки туннеллизации, в среднем срок наблюдения составил 70 месяцев. Авторы выявили улучшение показателей по шкале AOFAS (50.1-85.9), а также увеличение показателя активности по шкале Tegner с 1.6 до 4.3 балов [54].
Таблица 8
Противопоказания для мплантации аутологичных хондроцитов (ACI) в области голеностопного сустава
|
Относительные: |
Абсолютные: |
|
Биполярные («целующиеся») поражения большеберцовой и таранной кости |
Артрозоартрит в стадии активного воспаления |
|
Отсутствие предыдущих операции |
Посттравматическая деформация |
|
Ранние дегенеративные изменения |
Клинически значимые признаки нестабильности голеностопного сустава |
Лечение ОХПТК методом пластики фрагментированным, ювенильным аллотрансплантатом хрящевой ткани
Particulated Juvenile Cartilage Allograft ( DeNovo NT graft; Zimmer, Warsaw, IN) представляет собой специально подготовленный, механически фрагментированый аллотрансплантат ювенильной хрящевой ткни гиалинового хряща с жизнеспособными клетками хондроцитов , фиксация в области ОХПТК осуществляется с помощью фибринового клея (Рис. 9А,Б). Возраст доноров (трупный материал) ювенильной хрящевой ткани должен быть менее 13 лет, исходя из того, что хрящевая ткань в этом возрасте имеет более высокую плотность хондроцитов, что неоднократно доказано, так же как то, что активность хондроцитов в этом возрасте на много выше чем у более старших доноров. Следует отметит еще и тот факт, что тансплантация ювенильной хрящевой ткани из дистального мыщелка бедренной кости, в конечном счете намного дешевле чем применение АСI. Подобное оперативное вмешательство возможно также выполнить полностью артроскопически в одноэтапном оперативном вмешательстве. Подобная возможность позволяет избежать риска послеоперационных осложнений, неоднократных оперативных вмешательств, а также осложнений, связанных с остеотомией лодыжек. Ювенильный аллотрансплантат хрящевой ткани может быть применён для пластики больших по размеру ОХДТК, а так же у пациентов с неудачным исходом оперативного лечения по методике стимуляции регенерации костной ткани (туннелизация). Coetzee и соавт. провели многоцентровое исследование, которое включило 24 голеностопных сустава с последующим послеоперационным наблюдением не менее 16 мес [55]. средний возраст пациентов составил 35 лет, а 14 из 24 пациентов перенесли минимум 1 процедуру стимуляции регенерации костной ткани (туннелизацию). Средний размер ОХПТК составил 125 мм², а средняя глубина - 7 мм. Средний балл AOFAS на заключительном наблюдении составил 85, при этом 18/24 (78%) пациентов сообщили об их удовлетворенности проведённым лечением. Из 24 случаев наблюдений, в срок наблюдения до 16 месяцев только в 1 случае отмечено частичное отслоение трансплантата [59].
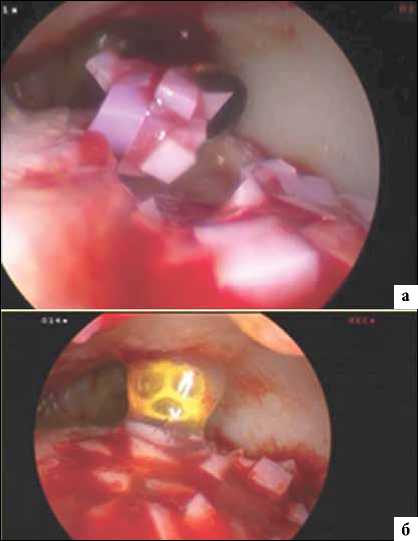
Рис. 9. Пластика ОХПТКс помощью particulated juvenile cartilage (PJC). (A) Этап операции заполнение дефекта таранной кости левого голеностопного сустава препаратом (PJC) , визуализация через заднелатеральный артроскопический доступ. (B) Фиксация препарата (PJC) в необходимом положении при помощи фибринового клея.
Послеоперационное ведение
В раннем послеоперационном периоде конечность требует фиксации в задней гипсовой лонгете от верхней трети голени до кончиков пальцев в средне-физиологическом положении стопы без возможности нагрузки на последнюю и ходьбой при помощи костылей, кожные швы снимаются в стандартные сроки в среднем через 2 недели после операции
Остальная часть послеоперационного ортопедического режима зависит от размера, локализации поражения и метода лечения.
При микрофрактурировании, строгое ограничение по нагрузке на оперированную конечность в течение 4 недель, далее до 8-10 недель в режиме съемной фиксации без нагрузки. Пациент использует съемный ортез и освобождает голеностопный сустав от фиксации 3-4 раза в день на 5-10 мин для лечебной физкультуры и восстановления объёма движений в голеностопном суставе не нагружая последний. Полный спектр движений, без фиксации, должен начинаться не ранее чем через 8-10 недель после операции в комплексе с физиотерапией.
Недавнее исследование под контролем Lee и соавт. показало, что ранняя дозированная нагрузка на конечность через 2 недели после операции, после чего полная нагрузка, как только пациента перестанет беспокоить болевой синдром после операции, имеет похожие результаты относительно шкалы AOFAS, визуальной аналоговой шкалы (ВАШ) и шкалы активности голеностопного сустава (аnkle activity score – AAS), по сравнению с результатами классического послеоперационного ведения с длительной иммобилизацией и периодом без нагрузки на конечность не менее 6-8 недель. Однако, следует отметить, что все пациенты в этом исследовании имели локальное (очаговое) ОХПТК <2,0 см2, хирургическое лечение которым осуществлялось методом микро-фрактурирования [22].
Если для хирургического лечения выполнялась остеотомия лодыжки, то все сроки иммобилизации удлиняются минимум на 1 неделю относительно сроков описанных при микрофрактури-ровании.
При использовании метода пластики фрагментированным ювенильным аллотрансплантатом хрящевой ткани (Particulated Juvenile Cartilage Allograft), авторы метода рекомендуют исключить нагрузку и продлить полную иммобилизацию на 4 недели, после чего перевести в режим съемной фиксации с дозированной разработкой активных движений в течении последующих 2-3 недель с ограничением подошвенного сгибания в процессе разработки до 20 градусов, с целью профилактики излишнего напряжения в зоне пластики. Спустя сроки дозированной разработки, пациент на 2-3 недели приступает к частичной нагрузке на костылях на оперированную конечность с фиксацией последней в туторе или брейсе, а спустя 2,5-3 месяца с момента операции может приступить к полной нагрузке и активной разработке движений в оперированном голеностопном суставе.
В случае использования костно-хрящевого аллотрансплантата, пациентам обычно рекомендуется не нагружать оперированную конечность от 8 до 10 недель.
Было доказано, что использование магнитотерапии (pulse electromagnetic fields - PEMFs) в послеоперационном комплексе лечения пациентов с костно-хрящевым дефектом улучшает функциональное восстановление и сокращает необходимость применения нестероидных противовоспалительных препаратов (НПВП) при лечении остеохондральных поражений коленного сустава [56]. В исследовании на животных было показано, что PEMF стимулирует активность остеобластов в процессе заживления остеохондрального дефекта [57]. Возврат к занятиям спортом и полноценной активности следует начинать не ранее, чем через 4 месяца после операции при условии хорошо локализованного (ограниченного) поражения и до 6 месяцев при более значительном слабо ограниченном поражении.
В работе Van Eekeren с соавторами оценили отдаленные результаты возвращения к спорту после артроскопической хирургической обработки и стимуляции регенерации костной ткани по средством туннелизации [58]. Авторы выявили, что 76% этих пациентов продолжили занимается активными физическими упражнениями и сохранили участие в спортивных мероприятиях, сроки наблюдения при этом в среднем составили 118 месяцев (в диапазоне от 46 до 271 месяцев). Следует так же отметить, что средний бал по шкале AAS ( Ankle Arthritis Score) составляющий перед операцией 8 балов значительно уменьшился до 4 балов в окончательном сроке наблюдения.
Выводы
Лечение остеохондральных поражений голеностопного сустава является сложной задачей. Определенные условия, такие как, возраст, размер дефекта, ограниченность дефекта, вид хирургического вмешательства, использование биопрепаратов и физиотерапии играют определенную роль в благоприятных исходах лечения.
Однако, никакие процедуры поистине не восстанавливают полностью поврежденное хрящевое покрытие. Будущие исследования должны быть выполнены для разработки технологии, отвечающей принципам малоинвазивности, с возможностью более эффективно восстанавливать остеохондральные дефекты голеностопного сустава, с минимальным количеством осложнений и быстрым восстановлением, сохраняющимся на длительный срок.
Список литературы Методы лечения остеохондральных повреждений таранной кости (рассекающий остеохондрит) на современном этапе (обзор литературы)
- Waterman B.R., Belmont P.J., Cameron K.L., Deberardino T.M., Owens B.D. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med, 2010, 38(4), pp. 797-803. DOI: 10.1177/0363546509350757
- Saxena A., Eakin C. Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med, 2007, 35(10), pp. 1680-1687. DOI: 10.1177/0363546507303561
- Hintermann B., Regazzoni P., Lampert C., Stutz G., Gachter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br, 2000, 82-B(3), pp. 345-351
- Hintermann B., Regazzoni P., Lampert C., Stutz G., Gachter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br, 2000, 82-B(3), pp. 345-351
- Orr J.D., Dawson L.K., Garcia E.J., et al. Incidence of osteochondral lesions of the talus in the United States military. Foot Ankle Int, 2011, 32(10), pp. 948-954. DOI: 10.3113/FAI.2011.0948
- Van Dijk C.N., Reilingh M.L., Zengerink M., van Bergen C.J. Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc, 2010, 18(5), pp. 570-580.
- DOI: 10.1007/s00167-010-1064-x
- Thordarson D.B., Motamed S., Hedman T., Ebramzadeh E., Bakshian S. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am, 1997, 79(12), pp. 1809-1815
- Ramsey P.L., Hamilton W. Changes in tibiotalar area contact caused by lateral talar shift. J Bone Joint Surg Am, 1976, 58(3), pp. 356-357
- Bruns J., Rosenbach B. Pressure distribution at the ankle joint. Clin Biomech, 1990, 5(3), pp. 153-161
- DiGiovanni B.F., Fraga C.J., Cohen B.E., et al. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int, 2000, 21(10), pp. 809-815.
- DOI: 10.1177/107110070002101003
- Ferkel R.D., Chams R.N. Chronic lateral instability: arthroscopic findings and long term results. Foot Ankle Int, 2007, 28(1), pp. 24-31.
- DOI: 10.3113/FAI.2007.0005
- Gregush R.V., Ferkel R.D. Treatment of the unstable ankle with an osteochondral lesion: results and longterm followup. Am J Sports Med, 2010, 38(4), pp. 782-790.
- DOI: 10.1177/0363546509351556
- Grimm N.L., Weiss J.M., Kessler J.I., Aoki S.K. Osteochondritis dessicans in the knee: pathoanatomy, epidemiology, and diagnosis. Clin Sports Med, 2014, 33(2), pp. 181-188.
- DOI: 10.1016/j.csm.2013.11.006
- Van Dijk C.N., Reilingh M.L., Zengerink M., van Bergen C.J. The natural history of osteochondral lesions of the ankle. Instr Course Lect, 2010, 59, pp. 375-386
- Hembree W.C., Wittstein J.R., Vinson E.N., et al. Magnetic resonance imaging features of osteochondral lesions of the talus. Foot Ankle Int, 2012, 33(7), pp. 591-597.
- DOI: 10.3113/FAI.2012.0591
- Hannon C.P., Smyth N.A., Murawski C.D., et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J, 2014, 96-B(2), pp. 164-171.
- DOI: 10.1302/0301-620X.96B2.31637
- Berndt A.L., Harty M. Osteochondritis dissecans of the ankle joint; report of a case simulating a fracture of the talus. J Bone Joint Surg Am, 1959, 41-A(4), pp. 988-1020
- Elias I., Zoga A.C., Morrison W.B., Besser M.P., Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid
- Mologne T.S., Ferkel R.D. Arthroscopic treatment of osteochondral lesions of the distal tibia. Foot Ankle Int, 2007, 28(8), pp. 865-872.
- DOI: 10.3113/FAI.2007.0865
- Malinin T., Temple H.T., Buck B.E. Transplantation of osteochondral allografts after cold storage. J Bone Joint Surg Am, 2006, 88(4), pp. 762- 770.
- DOI: 10.2106/JBJS.D.02991
- Loomer R., Fischer C., Lloyd-Smith R., et al. Osteochondral lesions of the talus. Am J Sports Med, 1993, 21(1), pp. 13-19.
- DOI: 10.1177/036354659302100103
- Talusan P.G., Milewski M.D., Toy J.O., Wall E.J. Osteochondritis dissecans of the talus: diagnosis and treatment in athletes. Clin Sports Med, 2014, 33(2), pp. 267-284.
- DOI: 10.1016/j.csm.2014.01.003
- Lee D.H., Lee K.B., Jung S.T., Seon J.K., Kim M.S., Sung I.H. Comparison of early versus delayed weightbearing outcomes after microfracture for small to midsized osteochondral lesions of the talus. Am J Sports Med, 2012, 40(9), pp. 2023-2028.
- DOI: 10.1177/0363546512455316
- Hepple S., Winson I.G., Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int, 1999, 20(12), pp. 789-793.
- DOI: 10.1177/107110079902001206
- Gortz S., De Young A.J., Bugbee W.D. Fresh osteochondral allografting for osteochondral lesions of the talus. Foot Ankle Int, 2010, 31(4), pp. 283-290.
- DOI: 10.3113/FAI.2010.0283
- Zengerink M., Struijs P.A., Tol J.L., van Dijk C.N. Treatment of osteochondral lesion of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc, 2010, 18(2), pp. 238-246. 10.1007/s00167-009- 0942-6
- DOI: 10.1007/s00167-009-0942-6
- Klammer G., Maquiera G., Spahn S., Vigfusson V., Zanetti M., Espinosa N. Natural history of nonoperatively treated osteochondral lesions of the talus. Foot Ankle Int, 2015, 36(1), pp. 24-31.
- DOI: 10.1177/1071100714552480
- Van Buecken K., Barrack R.L., Alexander A.H., et al. Arthroscopic treatment of transchondral talar dome fractures. Am J Sports Med, 1989, 17(3), pp. 350-355.
- DOI: 10.1177/036354658901700307
- Muir D., Saltzman C.L., Tochigi Y., Amendola N. Talar dome access for osteochondral lesions. Am J Sports Med, 2006, 34(9), pp. 1457-1463.
- DOI: 10.1177/0363546506287296
- Zengerink M., Szerb I., Hangody L., et al. Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin, 2006, 11(2), pp. 331- 359.
- DOI: 10.1016/j.fcl.2006.03.008
- Kumai T., Takakura Y., Kitada C., et al. Fixation of osteochondral lesions of the talus using cortical bone pegs. J Bone Joint Surg Br, 2002, 84(3), pp. 369-374
- Dunlap B.J., Ferkel R.D., Applegate G.R. The "LIFT" lesion: lateral inverted osteochondral fracture of the talus. Arthroscopy, 2013, 29(11), pp. 1826-1833.
- DOI: 10.1016/j.arthro.2013.08.012
- Kerkhoffs G., Reilingh M., Gerards R., de Leeuw P. Lift, drill, fill and fix (LDFF): a new arthroscopic treatment for talar osteochondral defects. Knee Surg Sports Traumatol Arthrosc, 2016, 24(4), pp. 1265-1271.
- DOI: 10.1007/s00167-014-3057-7
- O’Farell T., Costello B. Osteochondritis dissecans of the talus. The late results of surgical treatment. J Bone Joint Surg Br, 1982, 64(4), pp. 494-497
- Chen H., Hoemann C.D., Sun J., et al. Depth of subchondral perforation influences the outcome of bone marrow stimulation cartilage repair. J Orthop Res, 2011, 29(8), pp. 1178-1184.
- DOI: 10.1002/jor.21386
- Chuckpaiwong B., Berkson E.M., Theodore G.H. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy, 2008, 24(1), pp. 106-112. 10.1016/ j.arthro.2007.07.022
- DOI: 10.1016/j.arthro.2007.07.022
- Choi W., Choi G., Kim J., Lee J. Prognostic significance of the containment and location of osteochondral lesions of the talus. Am J Sports Med, 2014, 41(1), pp. 126-133.
- DOI: 10.1177/0363546512453302
- Choi W., Park K., Kim B., Lee J. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med, 2009, 37(10), pp. 1974-1980.
- DOI: 10.1177/0363546509335765
- Schuman L., Struijs P.A., van Dijk C.N. Arthroscopic treatment for osteochondral defects of the talus: Results at follow-up at 2 to 11 years. J Bone Joint Surg Br, 2002, 84-B(3), pp. 364-368
- Ferkel R.D., Zanotti R.M., Komenda G.A., et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long term results. Am J Sports Med, 2008, 36(9), pp. 1750-1762.
- DOI: 10.1177/0363546508316773
- Van Bergen C.J., Kox L., Maas M., Sierevelt I.N., Kerkhoffs G., van Dijk C.N. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow up. J Bone Joint Surg Am, 2013, 95(6), pp. 519-525.
- DOI: 10.2106/JBJS.L.00675
- Clanton T.O., Johnson N.S., Matheny L.M. Outcomes following microfracture in grade 3 and 4 articular cartilage lesions of the ankle. Foot Ankle Int, 2014, 35(8), pp. 764-770.
- DOI: 10.1177/1071100714539656
- Ueblacker P., Burkart A., Imhoff A.B. Retrograde cartilage transplantation on the proximal and distal tibia. Arthroscopy, 2004, 20(1), pp. 73- 78.
- DOI: 10.1016/j.arthro.2003.11.016
- Kolker D., Murray M., Wilson M. Osteochondral defects of the talus treated with autologous bone grafting. J Bone Joint Surg Br, 2004, 86(4), pp. 521-526
- Robinson D.E., Winson I.G., Harries W.J., Kelly A.J. Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Br, 2003, 85(7), pp. 989-993
- Ferkel R.D., Scranton P.E., Stone J.W., Kern B.S. Surgical treatment of osteochondral lesions of the talus. Instr Course Lect, 2010, 59, pp. 387- 404
- Sammarco G.J., Makwana N.K. Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int, 2002, 23(8), pp. 693-698.
- DOI: 10.1177/107110070202300803
- Emre T.Y, Ege T., Cift H.T., et al. Open mosaicplasty in osteochondral lesions of the talus: a prospective study. J Foot Ankle Surg, 2012, 51(5), pp. 556-560.
- DOI: 10.1053/j.jfas.2012.05.006
- Kennedy J.G., Murawski C.D. The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate: surgical technique. Cartilage, 2011, 2(4), pp. 327-336.
- DOI: 10.1177/1947603511400726
- El-Rashidy H., Villacis D., Omar I., Kelikian A.S. Fresh osteochondral allograft for the treatment of cartilage defects of the talus; a retrospective review. J Bone Joint Surg Am, 2011, 93(17), pp. 1634-1640.
- DOI: 10.2106/JBJS.J.00900
- Brittberg M., Lindahl A., Nilsson A., Ohlsson C., Isaksson O., Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med, 1994, 331(14), pp. 889-895.
- DOI: 10.1056/NEJM199410063311401
- Kreulen C., Giza E., Kim J., Campanelli V., Sullivan M. Viability of talus osteochondral defect cartilage for chondrocyte harvesting: results of 151 patients. Foot Ankle Int, 2014, 35(4), pp. 341-345.
- DOI: 10.1177/1071100714523272
- Niemeyer P., Salzman G., Schmal H., Mayr H., Sudkamp N. Autologous chondrocyte implantation for the treatment of chondral and osteochondral defects of the talus: a meta analysis of available evidence. Knee Surg Sports Traumatol Arthosc, 2012, 20(9), pp. 1696-1703. 10.1007/ s00167-011-1729-0
- DOI: 10.1007/s00167-011-1729-0
- Kwak S.K., Kern B.S., Ferkel R.D., Chan K.W., Kasraeian S, Applegate G.R. Autologous chondrocyte implantation of the ankle: 2-10 year results. Am J Sports Med, 2014, 42(9), p. 2156
- Coetzee J.C., Giza E., Schon L.C., et al. Treatment of osteochondral lesions of the talus with particulated juvenile cartilage. Foot Ankle Int, 2013, 34(9), pp. 1205-1211.
- DOI: 10.1177/1071100713485739
- Zorzi C., Dall’Oca C., Cadossi R., Setti S. Effects of pulsed electromagnetic fields on patients’ recovery after arthroscopic surgery: prospective, randomized and double-blind study. Knee Surg Sports Traumatol Arthrosc, 2007, 15(7), pp. 830-834.
- DOI: 10.1007/s00167-007-0298-8
- Cane V., Botti P., Soana S. Pulsed magnetic fields improve osteoblast activity during the repair of an experimental osseous defect. J Orthop Res, 1993, 11(5), pp. 664-670.
- DOI: 10.1002/jor.1100110508
- Van Eekeren I.C., van Bergen C.J., Sierevelt I.N., Reilingh M.L., van Dijk C.N. Return to sports after arthroscopic debridement and bone marrow stimulation of osteochondral talar defects: a 5- to 24-year follow-up study. Knee Surg Sports Traumatol Arthrosc, 2016, 24(4), pp. 1311-1315.
- DOI: 10.1007/s00167-016-3992-6
- Мо Ц., Ригин Н.В., Бобров Д.С., Слиняков Л.Ю., АНКЕТЫ И ШКАЛЫ ДЛЯ ОЦЕНКИ СОСТОЯНИЯ СТОПЫ И ГОЛЕНОСТОПНОГО СУСТАВА // Кафедра травматологии и ортопедии. 2016. №4(20). C. 5-11 [Mo J., Rigin N.V., Bobrov D.S., Slinyakov L.Y., OUTCOME RATING SCALES FOR CLINICAL EVALUATION OF FOOT AND ANKLE. The Department of Traumatology and Orthopedics, 2016, no. 4(20), pp. 5-11. [in Russ]


