Мочеточниково-влагалищные свищи: от этиологии к тактике лечения
Автор: Елисеев Денис Эдуардович, Гурбанов Шамиль Шукурович, Огай Дмитрий Сергеевич
Журнал: Экспериментальная и клиническая урология @ecuro
Рубрика: Реконструктивная урология
Статья в выпуске: 2, 2020 года.
Бесплатный доступ
Введение. Мочеточниково-влагалищные свищи являются следствием нераспознанной травмы мочеточника преимущественно при гинекологических операциях. Внедрение различных хирургических энергий в гинекологии и онкогинекологии привело к тому, что коагуляционный некроз стал частой разновидностью травмы мочеточника. Первым шагом в лечении поздно диагностированных повреждений мочеточника является использование миниинвазивного эндоурологического подхода и стентирования мочеточника.
Мочеточниково-влагалищный свищ, уретероскопия, стентирование мочеточника, уретероцистоанастомоз
Короткий адрес: https://sciup.org/142225666
IDR: 142225666 | DOI: 10.29188/2222-8543-2020-12-2-150-157
Текст научной статьи Мочеточниково-влагалищные свищи: от этиологии к тактике лечения
экспериментальная и клиническая урология № 2 2 0 2 0
Мочеточниково-влагалищные свищи являются следствием нераспознанной травмы мочеточника преимущественно при гинекологических операциях [1]. Травма мочеточника встречается в 0,5 – 1 % случаев всех операций на органах таза, при этом 75% травм мочеточников случаются во время гинекологических операций [2,3]. Радикальная гистерэктомия, выполняемая по поводу рака шейки матки, наиболее часто осложняется формированием мочеточниково-влагалищных свищей [1,4-7]. Частота мочеточниково-влагалищных свищей после радикальной гистерэктомии составляет 1,3 – 2,43 % [7- 9]. Гистерэктомии по поводу доброкачественных гинекологических заболеваний значительно реже ведут к формированию мочеточникововлагалищных свищей. Так, по данным T.H. Brummer и соавт., проанализировавших 5279 гистерэктомий, выполненных по поводу доброкачественной патологии, частота травмы мочеточников составила 0,2% [10]. Кроме гистерэктомии образование мочеточниково-влагалищных свищей возможно после других гинекологических операций (передняя кольпоррафия, операции на придатках матки) [1,11]. Акушерские мочеточниково-влагалищные свищи встречаются сравнительно редко, обычно связаны с травмой мочеточника при кесаревом сечении и гистерэктомии в послеродовом периоде [1,12,13]. Лучевая терапия сама по себе или в сочетании с хирургическим вмешательством может быть потенциально опасна в плане повреждения мочеточника и последующего формирования мочеточниково-влагалищного свища [11,14].
По данным A. Kiran и соавт., анализировавших риск травмы мочеточника у 377 073 женщин, которым была выполнена гистерэктомия в клиниках Великобритании в период с 2001 по 2010 год, наиболее типичные виды травмы мочеточника в порядке уменьшения частоты следующие: лигирование, перегиб швом, пересечение/отрыв частичное пересечение, сдавление и деваскуляризация [5]. В связи с увеличением количества вмешательств в гинекологии и онкогинекологии, выполняющихся лапароскопическим доступом, эффективный гемостаз становится одной из центральных проблем лапароскопической хи-рургии[15]. Например, такие методы гемостаза, как прошивание и лигирование, которые традиционно используются в открытой хирургии, являются технически сложным и трудоемкими в лапароскопической хирургии. Кроме того, могут быть трудности при лапароскопическом контроле кровотечения [15]. Поэтому столь распространен в лапароскопической хирургии превентивный гемостаз с использованием различных хирургических энергий. Также внедрение электрохирургии по мнению ряда авторов, привнесло большой вклад в модернизацию техники радикальной гистерэктомии и улучшило ее исходы [15,16]. Тревожная особенность лапароскопических операций состоит в том, что ранения мочеточника распознают интраоперационно менее чем в 7% случаев [17]. Со- гласно данным проспективного исследования FINHYST в ходе которого были проанализированы осложнения 5279 гистерэктомий, выполненных в 2006 году в клиниках Финляндии, 9 из 10 повреждений мочеточника были диагностированы в послеоперационном периоде, что указывает на коагуляционный некроз мочеточника [10]. Внедрение различных хирургических энергий в гинекологии и онкогинекологии привело к тому, что коагуляционный некроз стал частой разновидностью травмы мочеточника.
В 2010 году P.A. Sutton и соавт. опубликовали результаты первого исследования, сравнивающего боковое распространение тепловой энергии при использовании монополярной и биполярной диатермии, Harmonic ScalpelTM и LigasureTM. Степень бокового распространения тепловой энергии изменялась в зависимости от типа инструмента, мощности установки и времени воздействия. Монополярная диатермия приводила к самым высоким температурам и наибольшей степени теплового распространения в тканях [18].
Чтобы определить, насколько безопасным является воздействие ультразвукового скальпеля для окружающих тканей, K.M. Kadesky и соавт. использовали ультразвуковой скальпель на молодых свиньях для диссекции воротной вены из поджелудочной железы, почечной артерии и вены из ворот почки, мочеточника из забрюшинного пространства, аорты от нижней полой вены и общего желчного протока из окружающих тканей. Гистологическое исследование показало повреждение адвентиции и медии сосудистых структур, продемонстрировано выраженное повреждение с участками трансмуральной коагуляции мочеточника и общего желчного протока. Это исследование показало, что хотя ультразвуковой скальпель может облегчить рассечение при хорошем гемостазе, необходимо соблюдать осторожность, чтобы избежать повреждения соседних структур. Хотя его боковая энергетическая дисперсия может быть меньше, чем при диатермокоагуляции, он все же может вызывать трансмуральный некроз важных структур [19].
Изменение механизма травмы мочеточника привело и к изменению клиническая картина заболевания. По данным А.А. Попова и соавт. клинические проявления данного осложнения весьма разнообразны и отличаются от таковых при выполнении гистерэктомии открытым доступом. Свободному поступлению мочи через перфорационное отверстие в стенке мочеточника в брюшную полость без формирования мочевого затека, развитию мочеточниково-влагалищного свища или мочевого перитонита способствует то, что большинство хирургов не производят перитонизацию при лапароскопической гистерэктомии [20,21]. При этом может не наблюдаться нарушения пассажа мочи из почки [20].
Вопрос классификации мочеточниково-влагалищных свищей остается открытым. Д.В. Кан разделял мочеточниково-влагалищные свищи на полные и неполные
урогинекология
экспериментальная и клиническая урология № 2 2 0 2 0
-
[1 ]. N. Rajamaheswari и соавт. провели ретроспективный анализ данных 17 пациенток с мочеточниково-влагалищными свищами, в результате которого обосновали целесообразность разделения мочеточниково-влагалищных свищей на высокие и низкие, а также ранние и поздние.
Стентирование мочеточника было более эффективно у пациенток с низкими мочеточниково-влагалищными свищами, которые образовались в ранние сроки после перенесенного оперативного вмешательства [22].
Согласно рекомендациям Европейского общества урологов, первым шагом в лечении поздно диагностированных повреждений мочеточника являет использование миниинвазивного эндоурологического подхода стентирования мочеточника с дилатацией или без нее. Вмешательство может быть выполнено либо ретроградно, либо антеградно после выполнения перкутанной нефростомии. В случае неудачи показано открытая или робот-ассистированная лапароскопическая реконструктивная операция [23,24].
N.T.Schmeller и соавт. сообщили об опыте лечения 11 пациенток с мочеточниково-влагалищными свищами с использованием перкутанной нефростомии. У 6 (55%) больных отмечена стойкая персистенция свища, потребовавшая выполнения уретероцистоанастомоза с использованием техники «psoas hitch». У 2 (18%) пациенток сформировались стриктуры мочеточника, одна из которых была успешно устранена дилатацией мочеточника в сочетании с использованием системных кортикостероидов. Второй случай стриктуры мочеточника потребовал выполнения его реимплантации [25].
В 5-м издании руководства «Incontinence» приведен обзор об использовании стентирования мочеточников у пациенток с мочеточниково-влагалищными свищами в 11 исследованиях. Общее количество пациенток составило 126. Стентирование мочеточника было эффективно и привело к закрытию свища в 63 случаях [25–37].
В 2016 году C. Arasu с соавт. сообщили об опыте лечения 30 пациенток с мочеточниково-влагалищными свищами, возникшими после гистерэктомии (18 пациенток – после лапароскопическая гистерэктомии, 11 пациенток – после операции открытой абдоминальной гистерэктомии и 1 пациентка – после влагалищной гистерэктомии). Ретроградная уретерография, уретероскопия и стентирование JJ-стентом было эффективно у 29 женщин. 1 больной была выполнена перкутанная нефростомия с последующим ретроградным стентированием JJ-стентом. Только у 1 (7,1%) пациентки развилась стриктура мочеточника после удаления стента, потребовавшая открытой операции.
МАТЕРИАЛЫ И МЕТОДЫ
С 2016 по 2019 год нами пролечено 11 пациенток с мочеточниково-влагалищными свищами. Возраст паци- ентов колебался от 36 до 74 лет (средний возраст – 49,4 года). 3 пациентки обратились более чем через 2 месяца после формирования свища, остальные – ранее этого срока. У всех больных мочеточниково-влагалищные свищи были односторонними: у 6 – левосторонние, у 5 – правосторонние. У 10 пациенток свищи образовались после перенесенной гистерэктомии. 10 пациенткам была выполнена лапароскопическая экстрафасциальная гистерэктомия, 1 пациентке – радикальная гистерэктомия III типа по Piver открытым абдоминальным досупом у 1 пациентки – после иссечение ретроцервикального эндометриоидного инфильтрата, уретролиза, резекции заднего свода влагалища и шейвинга прямой кишки.
Всем пациенткам на догоспитальном этапе было выполнено ультразвуковое исследование почек, а также экскреторная урография или компьютерная томография органов брюшной полости и малого таза с внутривенным контрастированием (рис. 1).
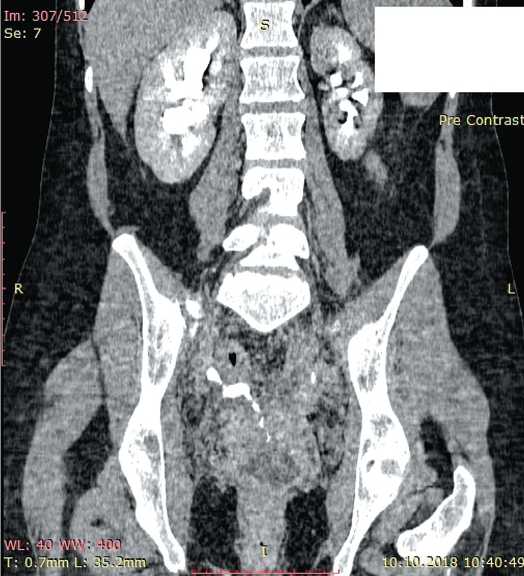
Рис. 1.Экскреторная фаза компьютерной томографии больной Ч., 38 лет (фронтальная проекция).Визуализируется мочеточниково-влагалищный свищ
Fig.1. Excretory phase of computed tomography of patient Ch., 38 years old (frontal projection). The ureteral-vaginal fistula is visualized
У 2 из 3 пациенток, обратившихся позже 2 месяцев после формирования свищей, не было обнаружено нарушения уродинамики верхних мочевых путей на стороне поражения, и им не проводилось дренирование почки на предоперационном этапе. У 1 больной из этой группы по данным экскреторной урографии и ультразвукового исследования обнаружен правосторонний уретерогидро-нефроз, потребовавший выполнения перкутанной нефростомии на предоперационном этапе. У остальных 8 пациенток мы придерживались описанной ниже тактики: лечение начинали с выполнения ретроградной уре- мочеточниково-влагалищные свищи
экспериментальная и клиническая урология № 2 2 0 2 0 теропиелографии и уретероскопии с попыткой дренирования почки внутренним мочеточниковым стентом. Уре-теропиелография и уретероскопия позволяли точно установить уровень мочеточникового свища, оценить распространенность травмы, выполнить визуальный контроль эффективности бужирования стриктуры. Если удавалось провести стент проксимальнее зоны свища мочеточника, то дренирование продолжали в течение 2 месяцев. Если же ретроградное проведение внутреннего мочеточникового стента не удавалось (при IV степени травмы мочеточника по AAST и полных мочеточникововлагалищных свищах), а у пациентки имелись признаки нарушения уродинамики верхних мочевых путей на стороне поражения, то выполняли перкутанную нефростомию. Через 2 месяца проводили оценку эффективности лечения. Пациенткам, которым была выполнена перкутанная нефростомия, выполняли антеградную пиелоуре-терографию. Больным, которым выполнялось стентирование мочеточника, удаляли внутренний стент и проводили контрольное обследование (уретероскопия, ретроградная уретеропиелография) под анестезией. Уретеро-пиелография позволяла исключить персистенцию свища и формирование стриктуры мочеточника, а уретероско-пия – провести визуальный контроль репарации в зоне внутреннего отверстия свища. При персистенции мочеточниково-влагалищного свища или формировании стриктуры мочеточника мы склонялись к выполнению уретероцистоанастомоза без повторных попыток стентирования мочеточника и бужирования стриктуры. В такой ситуации мы заканчивали операцию стентированием мочеточника для дренирования почки до момента выполнения реконструкции мочеточника. В случае эффективности стентирования (заживление свища и отсутствие стриктуры мочеточника) на следующие сутки после удаления внутреннего мочеточникового стента выполняли экскреторную урографию и ультразвуковое исследование почек для оценки уродинамики в естественных условиях. При отсутствии признаков нарушения уродинамики больных выписывали из стационара с рекомендациями динамического наблюдения. В случае невозможности ретроградного стентирования почки и отсутствия уре-терогидронефроза на стороне поражения пациенткам с функционирующим мочеточниково-влагалищным свищом выполнялась реконструктивная операция в объеме уретероцистоанастомоза или операции Боари спустя 2 – 3 месяца после рассасывания мочевых затеков, купирования воспаления и формирования рубцового процесса.
РЕЗУЛЬТАТЫ
У всех пациенток травма мочеточника имела коагуляционный генез. Зона травмы мочеточника располагалась в его тазовом отделе, на уровне 4 – 6 см от устья мочеточника, что соответствовало уровню перекреста мочеточника с маточной артерией.
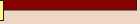
Двум женщинам, с полными мочеточниково-влагалищными свищами обратившимся позже 2 месяцев после формирования свища, не имевшим признаков нарушения оттока мочи из почки, на ипсилатеральной стороне в плановом порядке были выполнены реконструктивные операции (одной пациентке выполнена операция Боари открытым абдоминальным доступом, второй – лапароскопический уретероцистоанастомоз). Еще 1 пациентке с неполным мочеточниково-влагалищным свищом, у которой по данным экскреторной урографии и ультразвукового исследования обнаружен правосторонний уретеро-гидронефроз, потребовавший выполнения перкутанной нефростомии на предоперационном этапе, впоследствие в плановом порядке выполнен уретероцистоанастомоз открытым абдоминальным доступом (рис. 2,3).
5 пациенткам удалось выполнить стентирование мочеточника, у 3 из них потребовалось выполнение бужирования стриктуры, располагавшейся сразу дистальнее внутреннего отверстия свища. Все стриктуры были короткие (менее 1 см), имели рыхлую структуру. У всех пациенток диагностированы неполные мочеточникововлагалищные свищи, как следствие травмы мочеточника II степени у 4 пациенток и III степени у 1 пациентки (согласно классификации AAST). Бужирование стриктур

Рис. 2.Экскреторная урограмма больной С., 36 лет
Fig. 2. Excretory urogram of patient S., 36 years old

Рис. 3.Ретроградная уретерограмма больной С.
Fig. 3. Retrograde ureterogram of patient C.
урогинекология

экспериментальная и клиническая урология № 2 2 0 2 0
выполняли нефростомическими бужами по стандартной технологии. При контрольном обследовании, проведенном спустя 3 месяца, у 1 больной отмечена персистенция свища. Ей был выполнен уретероцистоанастомоз открытым абдоминальным доступом. У остальных 4 пациенток при контрольном обследовании нарушения уродинамики не были обнаружены (рис. 4,5).
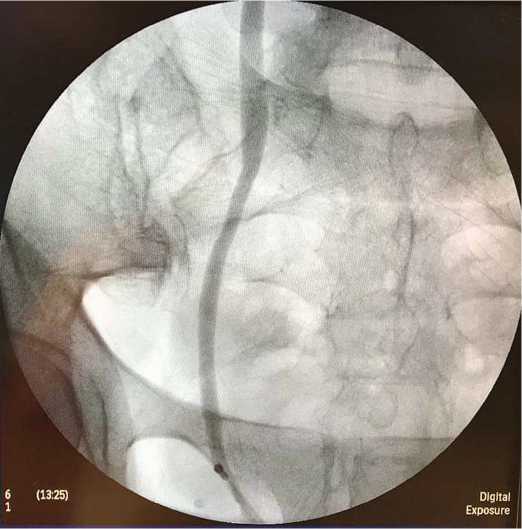
Рис. 4. Контрольная ретроградная уретерограмма после удаления внутреннего мочеточникового стента у больной Т., 50 лет
Fig. 4. Control retrograde ureterogram after removal of the internal ureteric stent in patient T., 50 years old
У 3 пациенток при уретероскопии диагностирована IV степень травмы мочеточника и полные мочеточниково-влагалищные свищи. Этим пациенткам при урете-

Рис. 5. Контрольная экскреторная урограмма на 1 сутки после удаления внутреннего мочеточникового стента больной Т., 50 лет. Отсутствие нарушения уродинамики верхних мочевых путей
Fig. 5. Control excretory urogram for 1 day after removal of the internal ureteral stent of patient T., 50 years old. The absence of impaired urodynamics of the upper urinary tract роскопии не удалось визуализировать проксимальный конец мочеточника в зоне травмы и мочевого затека и выполнить стентирование (рис. 6). Двум пациенткам вы-

Рис.6.Уретероскопия у больной Р.,49 лет. Уретероскоп проведен до зоны облитерации мочеточника. Визуализируются 2 клипсы на маточных сосудах (уровень травмы мочеточника)
Fig. 6. Ureteroscopy in patient R., 49 years old. A ureteroscope is held up to the ureter obliteration zone. 2 clips on the uterine vessels (level of ureteral injury) are visualized

никово-влагалищные свищи
экспериментальная и клиническая урология № 2 2 0 2 0
полнена перкутанная нефростомия для дренирования почки. У 1 пациентки нефростомия не выполнялась, учитывая наличие полного мочеточниково-влагалищного свища и отсутствие нарушений уродинамики на стороне поражения. Всем 3 женщинам впоследствии в плановом порядке выполнен уретероцистоанастомоз (1 пациентке открытым абдоминальным доступом, 2 – лапароскопическим).
Таким образом, все пациентки были избавлены от мочеточниково-влагалищных свищей. Попытка уретроскопии и ретроградного стентирования мочеточника предпринята у 8 пациенток. У 5 пациенток удалось выполнить стентирование, у 3 – не удалось. Стентирование мочеточника оказалось эффективно у 4 пациенток. 7 пациенткам (64%) выполнена реконструкция тазового отдела мочеточника: 1 пациентке – операция Боари, 6 пациенткам – уретероцистоанастомоз. Реконструкция мочеточника выполнена открытым абдоминальным доступом у 4 пациенток, лапароскопическим – у 3 пациенток. Во всех случаях реимплантация мочеточника выполнена интравезикальным способом по методике Н.А. Лопаткина.
ОБСУЖДЕНИЕ
Гистерэктомия является одной из наиболее часто выполняемых «больших» гинекологических операций. Техника лапароскопической гистерэктомия обладает некоторыми явными преимуществами перед открытой абдоминальной гистерэктомией. Лапароскопическая гистерэктомия сопровождается меньшей интраоперационной кровопотерей, лучшим косметическим эффектом, меньшей частотой инфекционных осложнений, меньшей интенсивностью послеоперационной боли,более коротким сроком стационарного лечения быстрым возвращением к нормальной жизнедеятельности. Также лапароскопический доступ более выгоден с экономической точки зрения. Тем не менее, лапароскопическая гистерэктомия ассоциируется с более длительным операционным временем и большим риском травмы мочевого пузыря или мочеточников по сравнению с открытой абдоминальной гистерэктомией [39,40].
В настоящее время только 10% травм мочеточников диагностируются интраоперационно [10]. Возможно, причина такого явления – увеличение количества коагуляционных повреждений мочеточника. При изучении этой причины травмы мочеточника необходимо учитывать два аспекта: тип используемого электрохирургического инструмента и соблюдение методологии его использования, а также место лигирования маточной артерии при гистерэктомии. По данным нескольких сравнительных исследований биполярная коагуляция и ультразвуковая энергия и большой размер сосуда коррелировали с увеличением термического повреждения. Термическое воздействие биполярной коагуляции рас- пространялось до 3,2 мм в сосудах диаметром 6 – 7 мм что говорит о безопасном запасе в 5 мм между инструментом и окружающей тканью. Биполярная коагуляция широко используется из-за удобства, экономии времени и снижения кровопотери, но требует осторожности при использовании для лигирования сосудов большого размера [41,42]. Известно, что по мере опущения вглубь таза мочеточники смещаются медиальнее.На уровне матки они находятся менее чем в 1 см от крестцово-маточных связок. Мочеточники входят в ткань кардинальных связок в точке, где маточные сосуды пересекают их сверху, а влагалищные сосуды снизу, в это время мочеточники делают поворот к мочевому пузырю [43]. Попытка лигирования основного ствола маточной артерии в толще параметрия в зоне перекреста с мочеточником является причиной коагуляционной травмы мочеточника. Исходя из этого, базовым принципом безопасной гистерэктомии, как в открытом, так и в лапароскопическом варианте, является пересечение восходящей ветви маточной артерии на уровне перешейка матки с последующим отсечение кардинальных и крестцово-маточных связок вдоль ребра матки [44- 45].
Открытым остается вопрос классификации мочеточниково-влагалищных свищей. В 2017 г. Д.Э. Елисеев в статье, посвященной влагалищному доступу в хирургии мочеточниково-влагалищных свищей, уже поднимал вопрос о необходимости классификации этих свищей [46]. Интересна публикация N. Rajamaheswari и соавт., в которой на основании серии наблюдений обосновывается необходимость выделения новых классификационных категорий («высокие» и «низкие», «ранние» и «поздние») мочеточниково-влагалищных свищей [22]. И.А. Ерюхин и С.А. Шляпников считают, что клиническая классификация должна быть краткой, удобной в использовании и ориентированной на решение вполне конкретной клинической задачи: обеспечение дифференцированного подхода к лечебно-диагностической тактике. Пусть не идеальная, но согласованная и общепринятая классификация всегда имеет преимущество перед прочими, не получившими широкого признания классификационными вариантами [47]. Учитывая данные, полученные N. Rajamaheswari и соавт., мы выбрали максимальный временной интервал 2 месяца от момента формирования мочеточниково-влагалищного свища,в течение которого считали оправданным попытку выполнения уретероскопии,уретерографии и ретроградного стентирования мочеточника [22]. Всем пациенткам, обратившимся позже 2 месяцев после образования свища, попытки миниинвазивного лечения не предпринимались, им была выполнена реимплантация мочеточника в мочевой пузырь. Вопрос о целесообразности выполнения уретероскопии и попытки стентирования мочеточника при мочеточниково-влагалищном свище остается спорным. Интересна дискуссия Д.Ю. Пушкаря и Г.Р. Касяна в книге
урогинекология
экспериментальная и клиническая урология № 2 2 0 2 0
«Ошибки и осложнения в урогинекологии», посвященная срокам и целесообразности выполнения уретероскопии при повреждении мочеточника. Мнение Г.Р. Касяна: «Думаю, что здесь нужны разграничения по времени. Потому что если делать это через несколько дней после травмы – это одна ситуация. Через несколько месяцев после травмы – другая ситуация» [48]. И ответ Д.Ю. Пушкаря: «Согласен, уретероскопия должна быть. И, наверное, как первый шаг, если мы считаем это возможным» [48]. В то же время А.Г. Мартов и соавт. в 2007 году описали опыт лечения 7 пациенток с мочеточниково-влагалищными и мочеточниково-маточными свищами, у которых срок выполнения рентгеноэндоскопической операции от момента повреждения мочеточника составил от 2 месяцев до 1,5 года. Всем пациенткам выполняли филь-гурацию свища со стороны мочеточника через уретеро-скоп с помощью шарикового или крючковидного электрода, операции заканчивались установкой внутреннего стента диаметром 6–8 Ch на 6–18 недель. С первой попытки удалось ликвидировать свищ и восстановить уродинамику у 4 пациенток, со второй попытки – еще у 2 пациенток, 1 пациентке выполнен уретероцистоанасто-моз после второй неудачной попытки рентгеноэндоскопического лечения [49].
Еще одним обоснованием необходимости дифференцированного подхода к лечебно тактике при мочеточниково-влагалищных свищах является клиническое наблюдение персистенции неполного мочеточниково-влагалищного свища после уретероцистоанастомоза за счет рефлюкса мочи из мочевого пузыря в культю пораженного мочеточника [6]. При выполнении уретероцистоа-настомоза или операции Боари обычно мочеточник отсекают над зоной рубцового инфильтрата, не выполняя разобщение мочеточниково-влагалищного свища. По мнению Д.Э. Елисеева, если мочеточниково-влагалищный свищ полный, то это не имеет практического значения, а если неполный, то возможна персистенция свища за счет рефлюкса в культю мочеточника [46]. С целью профилактики персистенции свища у всех пациенток с неполными мочеточниково-влагалищными свищами, которым мы выполняем реконструкцию нижней трети мочеточника мы также выполняем трансвезикальную резекцию мочеточникового устья и интрамутального отдела пораженного мочеточника. Мы используем технику интравези-кального уретероцистоанастомоза по методике Н.А. Лопаткина [50]. После создания перфорационного отверстия в заднебоковой стенке мочевого пузыря, соответствующего диаметру мочеточника, последний проводим в полость мочевого пузыря, спатулируем на протяжении 1,5 см. Далее рассекаем слизистую оболочку мочевого пузыря от перфорационного отверстия на протяжении 1,5 см и выполняем уретероцистоанастомоз рассасывающимся шовным материалом 4/0 на внутреннем мочеточниковом стенте. При выполнении операции Боари мы также не формируем подслизистый тоннель, не использует «open end technicue», а применяем аналогичную технику Н.А. Лопаткина с формированием перфорации для мочеточника в выкроенном лоскуте.
ЗАКЛЮЧЕНИЕ
Развитие реконструктивной урологии и урогинекологии происходит параллельно внедрению новых медицинских технологий. Еще в 1986 году Д.В. Кан в своей книге «Руководство по акушерской и гинекологической урологии» писал: «Таким образом, устранить недержание мочи при мочеточниково-влагалищных свищах можно посредством удаления почки или с помощью пластической операции на мочеточнике» [1]. В настоящее время нефрэктомия допустима только в случае необратимой утраты функции почки на фоне свища, а современные возможности реконструктивной урологии и использование миниинзвазивных технологий позволяют устранить свищ и восстановить уродинамику верхних мочевых путей у большинства пациенток. Но изменение этиологической структуры и клинической картины современной травмы мочеточника и ее последствий требуют оптимизации классификации мочеточниково-влагалищных свищей для дифференцированного лечебного подхода и улучшения его результатов.
ЛИТЕ РАТУPA/REFERENCE S
мочеточниково-влагалищные свищи
экспериментальная и клиническая урология № 2 2 0 2 0
Список литературы Мочеточниково-влагалищные свищи: от этиологии к тактике лечения
- Кан Д.В. Руководство по акушерской и гинекологической урологии. - М.: Медицина, 1986. - 488 с. [Kan D.V. Guide to obstetric and gynecological urology. - M.: Medicine, 1986. 488 p. (In Russian)].
- Mattingly RF, Borkowf HI. Acute operative injury to the lower urinary tract. Clin Obstet Gynaecol 1978; 5(1):123-49.
- Gorchev G, Kornovski IA. Anatomical and surgical meaning of the ureters during the performance of radical hysterectomy. Akush Ginekol 2006;45:28-32
- Symmonds RE. Ureteral injuries associated with gynecologic surgery: prevention and management. Clin Obstet Gynecol 1976; 19(3): 623-44. DOI: 10.1097/00003081-197609000-00012
- Kiran A, Hilton P, Cromwel DA. The risk of ureteric injury associated with hysterectomy: a 10-year retrospective cohort study. BJOG 2016;123(7):1184-91. DOI: 10.1111/1471-0528.13576
- Hwang JH, Lim MC, Joung JY, Seo SS, Kang S, Seo HK, et al Urologic complications of laparoscopic radical hysterectomy and lymphadenectomy. Int Urogynecol J 2012; 23(11):1605-11.
- Likic IS, Kadija S, Ladjevic NG, Stefanovic A, Jeremic K, Petkovic S, et al. Analysis of urologic complications after radical hysterectomy. Am J Obstet Gynecol 2008;199(6):644.e1-3.
- Torres-Lobaton A, Rueda-Mesias M, Román-Bassaure E, Guadaluperojo-Herrera, Barra-Martínez R. Complications of radical hysterectomy during management of stage Ib and IIa cervix uteri cancer. Experience with 145 patients. Ginecol Obstet Mex 1996;(64):265-71.
- Hatch KD, Parham G, Shingleton HM, Orr JW Jr, Austin JM Jr. Ureteral strictures and fistulae following radical hysterectomy. Gynecol Oncol 1984;19(1):17-23.
- DOI: 10.1016/0090-8258(84)90152-5
- Brummer TH, Jalkanen J, Fraser J, Heikkinen AM, Kauko M, Mäkinen J, et al. FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Hum Reprod 2011;26(7):1741-51.
- DOI: 10.1093/humrep/der116
- Ginsberg D. Ureterovaginal fistula. In: Raz S, Rodriguez LV (edit.) Female Urology, 3rd ed. W. B. Saunders, Philadelphia, Pa., p. 821-24.
- Meirow D, Moriel EZ, Zilberman M, Farkas A. Evaluation and treatment of iatrogenic ureteral injuries during obstetric and gynecologic operations for nonmalignant conditions. J Am Coll Surg 1994;178(2):144-8. Hosseini SY, Roshan YM, Safarinejad MR. Ureterovaginal fistula after vaginal delivery. J Urol 1998;160(3 Pt 1):829.
- DOI: 10.1097/00005392-199809010-00055
- Goodwin WE, Scardino PT. Vesicovaginal and ureterovaginal fistulas: a summary of 25 years of experience. J Urol 1980;123(3):370-4.
- DOI: 10.1016/s0022-5347(17)55941-8
- Fagotti A, Vizzielli G, Fanfani F, Gallotta V, Rossitto C, Costantini B, et al. Randomized study comparing use of THUNDERBEAT technology vs standardelectrosurgery during laparoscopic radical hysterectomy and pelvic lymphadenectomy for gynecologic cancer. J Minim Invasive Gynecol 2014;21(3):447-53.
- DOI: 10.1016/j.jmig.2013.12.001
- Kimio Ushijima, Shuji Takemoto, Kouichiro Kawano, Shin Nishio, Atsumu Terada, Naotake Tsuda, et al. Controversies surrounding type III radical abdominal hysterectomy and its procedure using new instruments. Korean J Obstet Gynecol 2012;55 (4):225-229.
- Федоров И.В., Дубровин В.Н. Урологические осложнения лапароскопической хирургии: учеб. пособие. Казан. гос. мед. акад; Казань: КГМА, 2010. 24 c. [Fedorov I.V., Dubrovin V.N. Urological complications of laparoscopic surgery: textbook. allowance. Kazan. state med. acad; Kazan: KSMA, 2010. 24 p. (In russian)].
- Sutton PA, Awad S, Perkins AC, Lobo DN. Comparison of lateral thermal spread using monopolar and bipolar diathermy, the Harmonic Scalpel and the Ligasure. Br J Surg 2010;97(3):428-33.
- DOI: 10.1002/bjs.6901
- Kadesky KM, Schopf B, Magee JF, Blair GK. Proximity injury by the ultrasonically activated scalpel during dissection. J Pediatr Surg 1997;32(6):878-9.
- DOI: 10.1016/s0022-3468(97)90641-2
- Попов А.А., Шагинян Г.Г., Мананникова Т.Н., Мачанските О.В., Рамазанов М.Р. Урогенитальные осложнения при лапароскопической гистерэктомии. Материалы сборника «Актуальные проблемы акушерства и гинекологии и перспективы их решения в Московской области». - М.: МЕДпресс-информ, 2003. С. 203-207. [Popov A.A., Shaginyan G.G., Manannikova T.N., Machanskite O.V., Ramazanov M.R. Urogenital complications of laparoscopic hysterectomy. Materials of the collection "Actual problems of obstetrics and gynecology and the prospects for their solution in the Moscow region". - M.: MEDpress-inform, 2003. P. 203-207. (In russian)].
- Selli C, Turri FM, Gabellieri C, Manassero F, De Maria M, Mogorovich A. Delayed-onset ureteral lesions due to thermal energy: An emerging condition. Arch Ital Urol Androl 2014;86(2):152-3.
- DOI: 10.4081/aiua.2014.2.152
- Rajamaheswari N, Chhikara AB, Seethalakshmi K. Management of ureterovaginal fistulae: an audit. Int Urogynecol J 2013;24(6):959-62.
- DOI: 10.1007/s00192-012-1959-9
- EAU Guidelines Office, Arnhem, The Netherlands. URL: http://uroweb.org/guidelines/compilations-of-all-guidelines
- Tracey AT, Eun DD, Stifelman MD, Hemal AK, Stein RJ, Mottrie A. Robotic-assisted laparoscopic repair of ureteral injury: an evidence-based review of techniques and outcomes. Minerva Urol Nefrol 2018;70(3):231-41.
- DOI: 10.23736/S0393-2249.18.03137-5
- Schmeller NT, Gottinger H, Schuller J, Marx FJ. Percutaneous nephrostomy as primary therapy of ureterovaginal fistula. Urologe A 1983;22(2):108-12.
- Ridder D, Abrams P, Vries C, Elnei S, Alice Emasu A, Esegbono G., et al. Fistula. In: Abrams P, Cardozo L. Khouy S, Wein A, eds: Incontinence, 5th ed. 2013. Committee 4, 1527-1580.
- Andriole GL, Bettmann MA, Garnick MB, Richie JP. Indwelling double-J ureteral stents for temporary and permanent urinary drainage: experience with 87 patients. J Urol 1984;131(2):239-41.
- DOI: 10.1016/s0022-5347(17)50324-9
- Barton DP, Morse SS, Fiorica JV, Hoffman MS, Roberts WS, Cavanagh D. Percutaneous nephrostomy and ureteral stenting in gynecologic malignancies. Obstet Gynecol 1992;80(5):805-11.
- Beaghler MA, Taylor FC, McLaughlin KP. A combined antegrade and retrograde technique for reestablishing ureteral continuity. Tech Urol 1997;3(1):44-8.
- Campbell SC, Streem SB, Zelch M, Hodge E, Novick AC. Percutaneous management of transplant ureteral fistulas: patient selection and long-term results. J Urol 1993;150(4):1115-7.
- DOI: 10.1016/s0022-
- Dowling RA, Corriere JN, Jr., Sandler CM. Iatrogenic ureteral injury. J Urol 1986;135(5):912-5.
- DOI: 10.1016/s0022-5347(17)45921-0
- Koonings PP, Huffman JL, Schlaerth JB. Ureteroscopy: A new asset in the management of postoperative ureterovaginal fistulas. Obstet Gynecol 1992;80 (3 Pt 2):548-9.
- Lang EK. Antegrade ureteral stenting for dehiscence, strictures, and fistulae. AJR Am J Roentgenol 1984;143(4):795-801.
- DOI: 10.2214/ajr.143.4.795
- Lingeman JE, Wong MYC, Newmark JR. Endoscopic management of total ureteral occlusion and ureterovaginal fistula. J Endourol 1995;9(5):391-6.
- DOI: 10.1089/end.1995.9.391
- Mandal AK, Sharma SK, Vaidyanathan S, Goswami AK. Ureterovaginal fistula: Summary of 18 years' experience. Br J Urol 1990;65(5):453-6.
- DOI: 10.1111/j.1464-410x.1990.tb14785.x
- Narang V, Sinha T, Karan SC, Sandhu AS, Sethi GS, Srivastava A, et al. Ureteroscopy: savior to the gynecologist? Ureteroscopic management of post laparoscopic-assisted vaginal hysterectomy ureterovaginal fistulas. J Minim Invasive Gynecol 2007;14(3):345-7.
- DOI: 10.1016/j.jmig.2006.10.013
- Ustunsoz B, Ugurel S, Duru NK, Ozgok Y, Ustunsoz A. Percutaneous management of ureteral injuries that are diagnosed late after cesarean section. Korean J Radiol 2008;9(4):348-53.
- DOI: 10.3348/kjr.2008.9.4.348
- Arasu C, Ramasamy N, Kumaresan N. Early Endoscopic Management of Ureterovaginal Fistula: A Prospective Study. Int J Sci Stud 2016;4(2):191-193.
- Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2009; 8(3): CD003677
- Allam IS, Makled AK, Gomaa IA, El Bishry GM, Bayoumy HA, Ali DF. Total laparoscopic hysterectomy, vaginal hysterectomy and total abdominal hysterectomy using electrosurgical bipolar vessel sealing technique: a randomized controlled trial. Arch Gynecol Obstet 2015;291(6):1341-5.
- DOI: 10.1007/s00404-014-3571-3
- Seehofer D, Mogl M, Boas-Knoop S, Unger J, Schirmeier A, Chopra S, et al. Safety and efficacy of new integrated bipolar and ultrasonic scissors compared to conventional laparoscopic 5-mm sealing and cutting instruments. Surg Endosc 2012;26(9):2541-9.
- DOI: 10.1007/s00464-012-2229-0
- Carbonell AM, Joels CS, Kercher KW, Matthews BD, Sing RF, Heniford BT. A comparison of laparoscopic bipolar ves¬sel sealing devices in the hemostasis of small-, medium-, and large-sized arteries. J Laparoendosc Adv Surg Tech A 2003;13:377-80.
- DOI: 10.1089/109264203322656441
- Лоран О.Б., Касян Г.Р., Пушкарь Д.Ю. Экстренная урогинекология. М., ГЭОТАР-Медиа, 2020. 160 с. [Loran O.B., Kasyan G.R., Pushkar D.Yu. Emergency urogynecology. M., GEOTARMedia, 2020.160 p. (In Russian]
- Hiramatsu Y. Basic Standard Procedure of Abdominal Hysterectomy: Part 1. Surg J (N Y) 2019;5(Suppl 1):S2-S10.
- DOI: 10.1055/s-0039-1678575
- Konishi I. Basic Principle and Step-by-Step Procedure of Abdominal Hysterectomy: Part 2. Surg J (N Y) 2018;5(Suppl 1):S11-S21.
- DOI: 10.1055/s-0038-1676467
- Кулаков В.И., Адамян Л.В., Аскольская С.И. Гистерэктомия и здоровье женщины. М.: Медицина, 1999. 321 c.
- Kulakov V.I., Adamyan L.V., Askolskaya S.I. Hysterectomy and women's health. M.: Medicine, 1999.321 p.
- Елисеев Д.Э. Влагалищный доступ в хирургии мочеточниково-влагалищных свищей: обзор литературы и клинический случай. Экспериментальная и клиническая урология 2017;(1):120- 125. [Eliseev D.E. Surgical treatment of ureterovaginal fistulae using vaginal access: literature review and a clinical case. Eksperimental'naya i klinicheskaya urologiya = Experimental and clinical urology. 2017;(1):120-125. (In Russian)].
- Ерохин И.А., Шляпников С.А. Перитонит. Руководство по неотложной хирургии органов брюшной полости. [ Под ред. Савельева В.С.] ред. М.; «Триада-Х». 2004. С. 461-494 [Erokhin I.A., Shliapnikov S.A. Peritonitis. Guidelines for emergency abdominal surgery. [Edit. Saveliev V.S.]. M.; "Triad-X".2004. 461-494 p. (In Russian)].
- Пушкарь Д.Ю., Касян Г.Р. Ошибки и осложнения в урогинекологии. М., ГЭОТАР-Медиа, 2017. 384 с.
- Мартов А.Г., Меринов Д.С., Гурбанов Ш.Ш., Маслов С.А. Рентгеноэндоскопическое лечение мочеточниково-влагалищных и мочеточниково-маточных свищей. Consilium medicum 2007;9(4):42-46.
- Martov A.G., Merinov D.S., Gurbanov Sh.Sh., Maslov S.A. X-ray endoscopic treatment of the ureter-vaginal and ureter-uterine fistulas. Consilium medicum 2007; 9 (4): 42-46.
- Лопаткин Н.А., Шевцов И.П. Оперативная урология. Л.: Медицина, 1986. 480 c.
- Lopatkin N.A., Shevtsov I.P. Operative urology. - L.: Medicine, 1986.480 p.